Abstract
Objectives
To investigate the effects of cholecalciferol supplementation on the progression of motor disability in a cohort of amyotrophic lateral sclerosis (ALS) patients with low blood 25-hydroxyvitamin D3 [25(OH)D] levels, on the basis of the hypothesis of potential neuroprotective effects of vitamin D supplementation.
Methods
Forty-eight ALS patients, 34 with deficient (<20 ng/mL) and 14 with insufficient (20–29 ng/mL) serum levels of 25(OH)D, were randomized and treated by 3 different doses of cholecalciferol [50.000, 75.000 and 100.000 international units (IU) /month] and evaluated after 6-months. Assessment of motor dysfunction at baseline and after 6 months included ALS Functional Rating Scale-Revised (ALFRS-R) and upper motor neuron (UMN) scores and blood samples for 25(OH)D levels.
Results
Clinical data of 33 patients were available after 6 months. Analysis of Covariance (ANCOVA), with pre-treatment measurements included as covariate, did not show statistically significant differences in the ALSFRS-R (p > 0.05) and UMN (p > 0.05) among the patient groups who underwent 3 different doses of cholecalciferol. Conversely, the treatment with 75.000 IU/month or 100.000 IU/month induced a significant increase in serum levels of 25(OH)D in comparison with the supplementation with 50.000 IU/month; no significant differences were found between 75.000 IU/month and 100.000 IU/month.
Conclusions
Our findings highlighted that 6-month supplementation of vitamin D in ALS patients had no significant effects on motor dysfunction. However, it is recommended to prevent medical complications of vitamin D deficiency in ALS patients as well as in other populations of neurodegenerative patients, characterized by low mobility and decreased sun exposure.
Similar content being viewed by others
Introduction
Increasing evidence suggests that vitamin D3, in its active form 1α, 25-dihydroxyvitamin D3 [1,25(OH)2D3], may exert a neuroprotective role in several pathophysiologic pathways, such as oxidative stress, inflammation, mitochondrial dysregulation, and apoptosis, which have been demonstrated to play a crucial role in several neurodegenerative disorders, including Alzheimer’s disease (AD), Parkinson’s disease, and amyotrophic lateral sclerosis (ALS) [1,2,3,4,5]. However, further research is required to elucidate the potential neuroprotective effects of vitamin D and if they may be dependent on route of administration, combining endogenously sourced vitamin D from ultraviolet (UV) exposure to exogenously derived vitamin D through synthetic supplementation [6].
As for ALS, a fatal neurodegenerative disease affecting both upper and lower motor neurons, strong evidence of neuroprotective effects of vitamin D are derived from pre-clinical studies. Particularly, several investigations, using the G93A mouse model, have shown that high-dose vitamin D3 supplementation improves motor performances in the affected mice [3, 4]. Moreover, in the same transgenic mouse model vitamin D3 deficiency has been related to increased levels of markers of oxidative damage, apoptosis and inflammation in the cerebrospinal fluid [7] and impaired performances in functional disease outcomes [8].
From the pathophysiologic point of view, genetic studies have contributed to identify the proteins that potentially link vitamin D to ALS pathology, such as major histocompatibility complex (MHC) class II molecules, toll-like receptors, poly(ADP-ribose) polymerase-1, heme oxygenase-1, and calcium-binding proteins, as well as the reduced form of nicotinamide adenine dinucleotide phosphate [9]. Moreover, vitamin D may exert its effect on ALS modulating several pathophysiologic mechanisms, such as: (i) glutamate-induced excitotoxic neuronal injury; [10] (ii) increased levels of reactive oxygen species and apoptosis;[11] (iii) and regulation of intracellular signaling pathways, implicated in determining the balance between neuronal survival and death [12].
On the basis of this pre-clinical background, in the last decades, several observational studies have been drawn to verify the potential effects of vitamin D status on the disease course. In this regard, the abnormalities of the calcium-parathyroid hormone (PTH)-vitamin D axis and the decrease of the serum concentration of 25-hydroxyvitamin D3 [25(OH)D] have been reported in a number of cohorts of ALS patients [13,14,15,16]. Moreover, significant correlations have been shown between low serum 25(OH)D levels and impairment of gross motor function [14], assessed by the ALS Functional Rating Scale-Revised (ALSFRS-R) [17], and these results were interpreted as a consequence of poor mobility, of the less sun exposure, and of malnutrition frequently observed in ALS patients [14, 16].
From the prognostic point of view, diverging results were reported about potential correlations between serum 25(OH)D levels and disease progression or survival in a number of cohorts of ALS patients [14, 16, 18]. In particular, a retrospective study by Camu et al. [16]. revealed that low plasma 25(OH)D levels were associated with higher rate of decline and shorter survival of ALS patients. Conversely, a recent study by Blasco et al. [18] demonstrated that high levels of serum 25(OH)D were related to a worse prognosis in a cohort of ALS patients. Finally, baseline levels of 25(OH)D were not predictive of disease progression over the next 12 months in another population of ALS patients [14].
With regard to the effects on disease progression of vitamin D supplementation in ALS, Karam et al. [15] revealed that the daily administration of 2000 international units (IU) of vitamin D significantly reduced the decline in the ALSFRS-R score after 9 months in the treated patients versus non-supplemented patients. However, Libonati et al. [19] did not replicate this result, reporting that supplementation with high doses of cholecalciferol (i.e., 100.000 IU/week for a month and, then, 25.000 IU/15 days) did not modify the clinical progression of ALS after 6 months in treated patients compared to the untreated ones. Notably, in both studies high-dose vitamin D supplementation did not cause any side effect, considering that another debated point is related to the uncertainty about the appropriate use of low-dose (e.g., 800 IU/daily) versus high-dose vitamin D supplementation (e.g., >2000 IU/daily) in clinical practice [20]. However, according to the United Kingdom National Osteoporosis Society guidelines [21], neuromuscular diseases have been recognized as clinical features suggestive of osteomalacia, thereby to be tested for 25(OH)D and, consequently, supplemented, although the recommended doses to use in these conditions have not clearly established.
Taking these findings all together, in this pilot study, we aimed at evaluating the potential effects of vitamin D supplementation in a population of ALS patients with low levels of serum 25(OH)D: the enrolled patients were randomized in 3 groups for receiving 3 different doses of cholecalciferol (i.e., 50.000, 75.000, and 100.000 IU/month), as yet performed in clinical practice [15, 19, 20], and underwent the clinical examination after 6 months of vitamin D supplementation. We expected to clarify the effects of this treatment on motor dysfunction and clinical progression in the studied cohort of ALS patients.
Materials and methods
Case selection
This study was prospective in design and included patients diagnosed with either definite or clinically or laboratory-supported probable ALS according to the El Escorial revised criteria [22], consecutively hospitalized in our referral ALS center, from January to December 2016. The patients with nephropathy (serum creatinine level >1.5 mg/dl), use of tube feeding, gastrostomy, and receiving drugs that are known to affect calcium and bone metabolisms (e.g., bisphosphonate, estrogen, calcium, vitamin D, anabolic steroids, or other hormones) were not included in the study.
Initially, 48 patients with sporadic ALS were enrolled; after 3 months 15 patients dropped out because of discontinuity in vitamin D supplementation (i.e., 4 patients were hospitalized for tracheostomy, 6 patients died, and 5 patients were not compliant to the supplementation according to our protocol) (flow chart in Fig. 1). The baseline characteristics of the excluded patients did not differ from the remaining sample (for details see Supplementary Table 1). Overall, 33 ALS patients were included in the final data analysis, of whom 22 with deficient (<20 ng/mL) and 11 with insufficient (20–29 ng/mL) serum levels of 25(OH)D. To avoid seasonal effects, 25(OH)D levels measured at the baseline and month 6 visit were seasonally synchronous.
The enrolled patients were randomized and treated by 3 different doses of cholecalciferol (i.e., group A: 50.000 IU/month; group B: 75.000 IU/month; group C: 100.000 IU/month), also used in clinical practice [20], and clinically evaluated at baseline and after 6-months (5.97 ± 1.13 months).
Demographic (sex, age) and clinical data were collected for all the patients, such as age at onset; disease duration (defined as the time, in months, between ALS onset and clinical observation); total scores and subscores of ALSFRS-R [17], which evaluates 4 domains (i.e., bulbar, fine motor, gross motor and respiratory) by 12 items, attributing a maximum score of 4 to each item (maximum total ALSFRS-R score: 48; maximum subscore for each domain: 12); upper motor neuron (UMN) score, index of pyramidal dysfunction through the evaluation of the number of pathologic reflexes elicited from 15 body sites (score range: 0–16) [23]; body mass index (BMI); and serum 25(OH)D concentration, measured as a part of the routine biochemical workup of patients at our center, using chemiluminescent immunoassay on an ARCHITECT i1000SR analyzer (Abbott, Abbott Park, Illinois, US). Among the bone turnover parameters, at baseline we assessed the serum levels of intact-parathyroid hormone (33.41 pg/mL ± 8.22) and total (9.71 mg/dL ± 0.76) and ionized calcium (1.21 mmol/L ± 0.24) to exclude abnormalities of the bone metabolism. However, their monitoring was not included in the study design. We also investigated the occurrence of side effects related to hypercalcemia (calcium serum levels >10.5 mg/dL) every three months. All patients were treated with riluzole (100 mg/daily) from the date of diagnosis.
Genetic analysis was performed in all patients, exploring C9orf72 repeat expansion and mutations of SOD1, TARDBP, and FUS/TLS. No mutations of the explored genes were reported.
The study was conducted according to the principles expressed in the Declaration of Helsinki. Ethics approval was obtained from the Ethics Committee of our Institution. Patient or family written consent was obtained from each participant.
Statistical analysis
Differences in demographic and clinical characteristics among the ALS patient groups who underwent different vitamin D supplementation doses were assessed using Pearson chi-square test (χ2) and one-way analysis of variance (ANOVA), when appropriate.
To test the post-treatment effects of different vitamin D supplementation doses on functional measures (i.e., ALSFRS-R and UMN score) and blood levels of 25(OH)D, we employed an analysis of covariance (ANCOVA) model, with pre-treatment measurements included as covariate [24].
All analyses were performed using IBM Statistical Package for Social Science (SPSS) version 20, with p-value < .05 considered statistically significant.
Results
Pre-treatment demographic and clinical characteristics did not differ among the three treatment groups (Table 1).
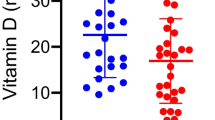
ANCOVA did not show statistically significant differences among the treatment groups in the ALSFRS-R total and domain scores (Fig. 2a–e) and UMN scores (Fig. 2f). Conversely, we found statistically significant differences in post-treatment measures of serum 25(OH)D levels (Fig. 3). In detail, Bonferroni post-hoc analyses showed that treatment with 75.000 IU/month or 100.000 IU/month induced a significant increase of serum 25(OH)D levels after 6 months in comparison to the effects of supplementation with 50.000 IU/month. Moreover, no significant differences were found between the treatment groups underwent 75.000 IU/month and 100.000 IU/month (Table 2).
Discussion
This pilot study revealed, for the first time, that the supplementation of vitamin D at different doses had no effect on modification of functional outcome measures in a cohort of ALS patients after a 6 months follow-up period. Moreover, treatment with 75.000 IU/month or 100.000 IU/month induced a similar increase of serum 25(OH)D levels in comparison to the supplementation with 50.000 IU/month.
Our findings are in line with previous results by Karam et al. [15], who monitored the disability status in a cohort of ALS patients, revealing that the decline in the ALSFRS-R score was not significantly different between patients receiving and those not receiving vitamin D after a 6-month follow-up period. However, only after a nine-month follow-up period, a significantly smaller decrease of the ALSFRS-R score in the supplemented group was observed. Of note, our results were original with regard to the different effects of the supplementation with 3 different doses of cholecalciferol on increase of 25(OH)D serum levels, suggesting a similar effect of the treatment with 75.000 IU/month and 100.000 IU/month after 6 months. However, although previously performed in other studies on patients with ALS [14, 15, 19] or other neurodegenerative diseases [25, 26], the assessment and monitoring of the serum 25(OH)D levels across time may not be able to completely address the role of oral supplementation of vitamin D, in that the serum 25(OH)D levels also derive from vitamin D synthesized in the skin from UV exposure, thereby needing the use of season-averaged 25(OH)D levels [14, 27].
On the basis of our findings, similarly to previous results by Paganoni et al. [14], the oral supplementation of vitamin D revealed no effects on slowing ALS disease progression. In particular, Paganoni et al. [14] found that participants taking supplementary vitamin D experienced a faster rate of decline, although serum 25(OH)D levels were not predictive of decline. Moreover, lower (season-averaged) 25(OH)D levels were associated with lower motor scores at baseline, but did not predict the occurrence of altered motor or total function. These results, together with our findings, support the evidence that, although lower 25(OH)D levels may reflect the motor disability status in ALS, the disease progression is not influenced by the biological activity of the supplementary vitamin D.
With regard to the neuroprotective effect of vitamin D supplementation in other neurodegenerative diseases than ALS, conflicting results were also revealed by prospective randomized controlled trials that investigated if vitamin D treatment improved cognitive scores in patients with mild-moderate dementia [26, 28]. Stein et al. [26] administered to mild-moderate AD patients low doses of vitamin D2 (1000 IU/day) for a period of 8 weeks, then randomly allocated to high dose (6000 IU/day) vitamin D2 or placebo for a subsequent 8 weeks. No significant differences were observed in the mini-mental state examination scores between the treatment groups, suggesting that supplementary high dose of vitamin D has no protective benefit compared to low dose on disease progression in AD. Conversely, another randomized controlled trial by Gangwar et al. [28] revealed that, after 6 months of supplementation with vitamin D3 (4000 IU/day) in a population of elderly patients with mild-moderate dementia, cognitive performances were significantly improved in the treatment group compared to controls, supporting that vitamin D3 may have a beneficial effect on cognitive functions in an elderly population. To note, most pre-clinical [29, 30] and observational data [31, 32] in support of neuroprotective/therapeutic benefits from vitamin D have been reported in multiple sclerosis (MS), revealing evidence on the immunomodulatory effects of the high-dose vitamin D supplementation on MS patients [5, 33]. However, these positive results have not been confirmed by findings from most prospective clinical trials [6]. In particular, in several populations of patients affected by highly inflammatory conditions, also including MS, inflammation has been shown to lower serum 25(OH)D levels via oxidative stress, while increasing vitamin D status has been hypothesized to reduce inflammation [34]. In this regard, in highly inflammatory diseases, baseline 25(OH)D concentration must be low [mean baseline 25(OH)D concentration <45 nmol/L] to see an anti-inflammatory effect linked to vitamin D supplementation, at least when using physiological doses of vitamin D. In fact, in these conditions, vitamin D supplementation has been shown to modestly lower markers of inflammation, when the baseline 25(OH)D levels were low and when the achieved 25(OH)D levels were higher. Similarly to what reported in highly inflammatory conditions, Camu et al. [16] revealed that also in ALS the clinical course of the disease worsened in the patients with severe vitamin D deficiency at baseline (<25 nmol/L) compared to the patients with normal 25(OH)D levels (>75 nmol/L). Moreover, taking these results all together, the impact of vitamin D deficiency on disease progression in several inflammatory and neurodegenerative conditions may not be considered as disease-specific. Notably, Camu et al. [16] did not provide evidence that vitamin D supplementation would be beneficial to individuals with ALS, while Karam et al. [15] suggested that the daily administration of 2000 UI of cholecalciferol might provide therapeutic benefits in ALS patients after 9 months. However, Karam et al. [15] accounted some limitations of their study, especially related to the small number of patients, the retrospective design of the study, and the fact that the supplemented group was younger and had lower vitamin D levels to begin with, thereby hindering conclusions regarding the role of supplementing ALS patients with vitamin D. Finally, some negative evidence regarding the potential relationships between serum 25(OH)D concentrations and survival in ALS patients was reported in a retrospective analysis by Yang et al. [35], who revealed that serum 25(OH)D levels were not correlated to other bone markers and survival time in a clinic population of ALS patients.
Another controversial point concerns the optimal doses of vitamin D3 supplementation to reach for clinical and research purposes, particularly in the light of the proven beneficial effects of high-dose vitamin D3 supplementation (i.e., using 10 and 50 times the adequate intake of cholecalciferol) carried out in G93A mouse model of ALS [3, 4], that may resemble recent evidence of the beneficial effects of high-dose vitamin D3 treatment (i.e., 35.000 IU/day) in autoimmune disorders of the skin [36]. Although universal supplementation guidelines do not exist, the doses of vitamin D3 supplementation applied in our observational study met the clinical recommendations proposed in patients at risk of osteomalacia [21], in whom cholecalciferol supplementation has been recommended at a daily dose of at least 1000–2000 IU given intermittently [20, 37]. We did not design to use higher doses of vitamin D3 (i.e., >2000 UI/day), although revealed to be safe [38], taking into consideration previous evidence showing that short-term high-dose and more regular low dose supplementation of vitamin D3 seem to offer similar efficacy [39]. Future clinical studies exploring the safety and the therapeutic efficacy of administration of very high doses of vitamin D3 might be designed also in neurological disorders, especially in those with autoimmune or neuroinflammatory pathogenesis, including MS and ALS, in line with the promising results revealed in autoimmune disorders of the skin [36].
Although further research is required to better understand the potential neuroprotective role of vitamin D on disease progression in neurodegenerative disorders through the “non-calcemic” effects of vitamin D metabolites (i.e., genomic and non-genomic actions) [5], a consistent evidence in several populations of neurodegenerative patients, including those investigated in this study, is the detection of low serum 25(OH)D levels [14, 40, 41], frequently below the recommended level of 30 ng/ml. A potential explanation for these observations is that serum 25(OH)D levels in neurodegenerative diseases may reflect less mobility and sun exposure of these patients, as also reported in the elderly, characterized by decline of physical performances [42]. This evidence supports the recommendation to screen individuals with ALS or other neurodegenerative diseases for vitamin D deficiency and, when this deficit is found, to supplement vitamin D to prevent the medical complications of this deficiency, such as bone loss and, possibly, secondary musculoskeletal pain and bone fractures.
Although evidence from the pre-clinical research supported the neuroprotective effect of vitamin D in either delaying onset or reducing symptoms in neurodegenerative diseases, our findings of lacking association between vitamin D supplementation and progression of motor disability in a small cohort of ALS patients argues against the role for vitamin D as a modifier of ALS outcome. However, major limitations of our pilot study are related to the small sample size studied and to the short follow-up period. Moreover, 1,25-dihydroxyvitamin D levels were not assessed and monitored and this may represent a weak point of the study design, considering that 1,25-dihydroxyvitamin D have been demonstrated to play a crucial neuroprotective role in animal models of several neurodegenerative disorders [1,2,3,4]. However, the concentration of total 1,25-dihydroxyvitamin D is not routinely used as a clinical marker of vitamin D status because of its short half-life and the low serum concentrations of the final metabolite [43], thereby causing that previous population-based and cohort studies mainly explored the correlations between serum 25(OH)D concentrations and clinical features in several neurological disorders [14, 15, 19, 35, 44]. Another criticism is related to the fact that serum 25(OH)D concentration is the total circulating form, but much of both 25(OH)D and 1,25-dihydroxyvitamin D is bound to the vitamin D-binding protein (DBP) and albumin and, therefore, the percentage of free vitamin D, which is bioavailable, should be more indicative of the actual vitamin D status [45]. Further studies, including the assessment of bioavailable 25(OH)D, DBP, and vitamin D receptor polymorphism, will be needed to elucidate the potential benefits of supplementary vitamin D intake on both motor and extra-motor symptoms reported in ALS, such as cognitive and behavioral dysfunctions, as also previously evaluated in AD patients. However, the investigation of vitamin D status and its supplementation, when needed, are recommended in ALS, as well as in other neurodegenerative diseases, to prevent the medical complications of vitamin D deficiency.
References
Lin AM, Chen KB, Chao PL. Antioxidative effect of vitamin D3 on zinc-induced oxidative stress in CNS. Ann N Y Acad Sci. 2005;1053:319–29.
Durk MR, Han K, Chow EC, Ahrens R, Henderson JT, Fraser PE, et al. 1α,25-Dihydroxyvitamin D3 reduces cerebral amyloid-β accumulation and improves cognition in mouse models of Alzheimer’s disease. J Neurosci. 2014;34:7091–101.
Gianforcaro A, Hamadeh MJ. Dietary vitamin D(3) supplementation at 10x the adequate intake improves functional capacity in the G93A transgenic mouse model of ALS, a pilot study. CNS Neurosci Ther. 2012;18:547–57.
Gianforcaro A, Solomon JA, Hamadeh MJ. Vitamin D3 at 50x the adequate intake attenuates functional decline in the G93A mouse model of amyotrophic lateral sclerosis, but is toxic in females. PLoS ONE. 2013;8:e30243.
Di Somma C, Scarano E, Barrea L, Zhukouskaya VV, Savastano S, Mele C, et al. Vitamin D and Neurological Diseases: An Endocrine View. Int J Mol Sci. 2017;18:E2482.
Iacopetta K, Collins-Praino LE, Buisman-Pijlman FTA, Liu J, Hutchinson AD, Hutchinson MR. Are the protective benefits of vitamin D in neurodegenerative disease dependent on route of administration? A systematic review. Nutr Neuroscience. 2018; e-pub ahead of print 9 July 2018; https://doi.org/10.1080/1028415X.2018.1493807
Moghimi E, Solomon JA, Gianforcaro A, Hamadeh MJ. Dietary vitamin D3 restriction exacerbates disease pathophysiology in the spinal cord of the G93A mouse model of amyotrophic lateral sclerosis. PLoS ONE. 2015;10:e0126355.
Solomon JA, Gianforcaro A, Hamadeh MJ. Vitamin D3 deficiency differentially affects functional and disease outcomes in the G93A mouse model of amyotrophic lateral sclerosis. PLoS ONE. 2011;6:e29354.
Lương K, Nguyễn LTH. Roles of vitamin D in amyotrophic lateral sclerosis: possible genetic and cellular signaling mechanisms. Mol Brain. 2013;6:16.
Atif F, Sayeed I, Ishrat T, Stein DG. Progesterone with vitamin D affords better neuroprotection against excitotoxicity in cultured cortical neurons than progesterone alone. Mol Med. 2009;15:328–36.
Garcion E, Sindji L, Leblondel G, Brachet P, Darcy F. 1,25-dihydroxyvitamin D3 regulates the synthesis of γ-glutamyl transpeptidase and glutathione levels in rat primary astrocytes. J Neurochem. 1999;73:859–66.
Byers S, Shah S. Vitamin D and the regulation of Wnt/beta-catenin signaling and innate immunity in colorectal cancer. Nutr Rev. 2007;65:S118–20.
Sato Y, Honda Y, Asoh T, Kikuyama M, Oizumi K. Hypovitaminosis D and decreased bone mineral density in amyotrophic lateral sclerosis. Eur Neurol. 1997;37:225–9.
Paganoni S, Macklin EA, Karam C, Yu H, Gonterman F, Fetterman KA, et al. Vitamin D levels are associated with gross motor function in amyotrophic lateral sclerosis. Muscle Nerve. 2017;56:726–31.
Karam C, Barrett MJ, Imperato T, Macgowan DJ, Scelsa S. Vitamin D deficiency and its supplementation in patients with amyotrophic lateral sclerosis. J Clin Neurosci. 2013;20:1550–3.
Camu W, Tremblier B, Plassot C, Alphandery S, Salsac C, Pageot N, et al. Vitamin D confers protection to motoneurons and is a prognostic factor of amyotrophic lateral sclerosis. Neurobiol Aging. 2014;35:1198–205.
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci. 1999;169:13–21.
Blasco H, Madji Hounoum B, Dufour-Rainfray D, Patin F, Maillot F, Beltran S, et al. Vitamin D is not a protective factor in ALS. CNS Neurosci Ther. 2015;21:651–6.
Libonati L, Onesti E, Gori MC, Ceccanti M, Cambieri C, Fabbri A, et al. Vitamin D in amyotrophic lateral sclerosis. Funct Neurol. 2017;32:35–40.
Woodford HJ, Barrett S, Pattman S. Vitamin D: too much testing and treating? Clin Med (Lond). 2018;18:196–200.
Aspray TJ, Bowring C, Fraser W, Gittoes N, Javaid MK, Macdonald H, et al. National Osteoporosis Society vitamin D guideline summary. Age Ageing. 2014;43:592–5.
Brooks BR, Miller RG, Swash M, Munsat TL. World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Mot Neuron Disord. 2000;1:293–9.
Turner MR, Cagnin A, Turkheimer FE, Miller CC, Shaw CE, Brooks DJ, et al. Evidence of widespread cerebral microglial activation in amyotrophic lateral sclerosis: an [(11)C](R)-PK11195 positron emission tomography study. Neurobiol Dis. 2004;15:601–9.
O’Connell NS, Dai L, Jiang Y, Speiser JL, Ward R. Methods for analysis of pre-post data in clinical research: a comparison of five common methods. J Biom Biostat. 2017;8:2.
Suzuki M, Yoshioka M, Hashimoto M, Murakami M, Noya M, Takahashi D, et al. Randomized, double-blind, placebo- controlled trial of vitamin D supplementation in Parkinson disease. Am J Clin Nutr. 2013;97:1004–13.
Stein MS, Scherer SC, Ladd KS, Harrison LC. A randomized controlled trial of high-dose vitamin D2 followed by intranasal insulin in Alzheimer’s disease. J Alzheimer’s Dis. 2011;26:477–84.
Ascherio A, Munger KL, White R, Köchert K, Simon KC, Polman CH, et al. Vitamin D as an early predictor of multiple sclerosis activity and progression. JAMA Neurol. 2014;71:306–14.
Gangwar AK, Rawat A, Tiwari S, Tiwari SC, Narayan J, Tiwari S. Role of vitamin-D in the prevention and treatment of Alzheimer’s disease. Indian J Physiol Pharmacol. 2015;59:94–9.
Munger KL, Kochert K, Simon KC, Kappos L, Polman CH, Freedman MS, et al. Molecular mechanism underlying the impact of vitamin D on disease activity of MS. Ann Clin Transl Neurol. 2014;1:605–17.
Bhargava P, Gocke A, Calabresi PA. 1,25-Dihydroxyvitamin D3 impairs the differentiation of effector memory T cells in vitro in multiple sclerosis patients and healthy controls. J Neuroimmunol. 2015;279:20–4.
Simpson S Jr, Taylor B, Blizzard L, Ponsonby AL, Pittas F, Tremlett H, et al. Higher 25-hydroxyvitamin D is associated with lower relapse risk in multiple sclerosis. Ann Neurol. 2010;68:193–203.
Lucas RM, Ponsonby AL, Dear K, Valery PC, Pender MP, Taylor BV, et al. Sun exposure and vitamin D are independent risk factors for CNS demyelination. Neurology. 2011;76:540–8.
Sotirchos ES, Bhargava P, Eckstein C, van Haren K, Baynes N, Ntranos A, et al. Safety and immunologic effects of high- vs low-dose cholecalciferol in multiple sclerosis. Neurology. 2016;86:382–90.
Cannell JJ, Grant WB, Holick MF. Vitamin D and inflammation. Dermatoendocrinol. 2015;6:e983401.
Yang J, Park JS, Oh KW, Oh SI, Park HM, Kim SH. Vitamin D levels are not predictors of survival in a clinic population of patients with ALS. J Neurol Sci. 2016;367:83–8.
Finamor DC, Sinigaglia-Coimbra R, Neves LC, Gutierrez M, Silva JJ, Torres LD, et al. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermatoendocrinol. 2013;5:222–34.
Rolland Y, de Souto Barreto P, Abellan Van Kan G, Annweiler C, Beauchet O, Bischoff-Ferrari H, et al. Vitamin D supplementation in older adults: searching for specific guidelines in nursing homes. J Nutr Health Aging. 2013;17:402–12.
Zittermann A, Prokop S, Gummert JF, Borgermann J. Safety issues of vitamin D supplementation. Anticancer Agents Med Chem. 2013;13:4–10.
Hackman KL, Gagnon C, Briscoe RK, Lam S, Anpalahan M, Ebeling PR. Efficacy and safety of oral continuous low-dose versus short-term high-dose vitamin D: a prospective randomised trial conducted in a clinical setting. Med J Aust. 2010;192:686–9.
Ding H, Dhima K, Lockhart KC, Locascio JJ, Hoesing AN, Duong K, et al. Unrecognized vitamin D3 deficiency is common in Parkinson disease: Harvard Biomarker Study. Neurology. 2013;81:1531–7.
Zhao Y, Sun Y, Ji HF, Shen L. Vitamin D levels in Alzheimer’s and Parkinson’s diseases: a meta-analysis. Nutrition. 2013;29:828–32.
Wicherts IS, van Schoor NM, Boeke AJ, Visser M, Veeg DJ, Smit J, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007;92:2058–65.
Fraser WD, Milan AM. Vitamin D assays: past and present debates, difficulties, and developments. Calcif Tissue Int. 2013;92:118–27.
Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PH, et al. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014;83:920–8.
Chun RF, Peercy BE, Orwoll ES, Nielson CM, Adams JS, Hewison M, et al. Vitamin D and DBP: the free hormone hypothesis revisited. J Steroid Biochem Mol Biol. 2014;144:132–7.
Acknowledgements
The authors are grateful to all patients with ALS who kindly agreed to take part in this research.
Author information
Authors and Affiliations
Contributions
FT, MS, GS, MRM, and GT conceived and designed the experiments; FT, MS, CP, AB, AR, LL, SE, and DR performed the experiments; FT, MS, CP, and GS analyzed the data; FT, MS, CP, AB, AR, LL, SE, DR, MRM, and GT contributed reagents/materials/analysis tools; FT, MS, GT, and GS wrote and/or revised the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Trojsi, F., Siciliano, M., Passaniti, C. et al. Vitamin D supplementation has no effects on progression of motor dysfunction in amyotrophic lateral sclerosis (ALS). Eur J Clin Nutr 74, 167–175 (2020). https://doi.org/10.1038/s41430-019-0448-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0448-3
- Springer Nature Limited