Abstract
Introduction Devon and Cornwall have been identified as 'dental deserts' with limited NHS dental access and high levels of oral health inequality. Challenges around recruitment and retention of the dental workforce have been acknowledged as an important contributory factor.
Aims The aim of this research was to explore the experiences of dental practices within Devon and Cornwall in relation to recruitment and retention of the dental workforce.
Method A self-administered, online questionnaire was used to explore various aspects of workforce recruitment and retention. The questionnaire included categorical rating scale and free-text question formats providing quantitative and qualitative data.
Results In total, 106 dental practices responded to the survey, providing a response rate of 36%. The vast majority of respondents (94%) considered recruitment and retention to be a major barrier to delivering NHS services. Additionally, 77% of practices had a current staff vacancy, 57% had a dentist vacancy and 48% had a vacancy for dental nurses. Thematic analysis led to identification of four main themes which were considered to influence recruitment and retention: NHS system; economic challenges; logistics; and support networks.
Conclusion A large number of dental practices in Devon and Cornwall are failing to operate at capacity due to workforce shortages, which is affecting access to services in both NHS and private practices. Recruitment and retention of dentists and dental nurses appears to be the most challenging factor, with NHS practices affected more than the private sector.
Key points
-
Challenges in recruitment and retention of the dental workforce are a significant contributory factor in the delivery of dental services in Devon and Cornwall, and this is likely to reflect the situation in other rural and coastal areas of the UK.
-
Over three-quarters of respondent dental practices currently have vacancies within their workforce, with 57% of practices having a vacancy for at least one dentist. Practices with an NHS contract are most affected, but rural private practices are also facing significant challenges.
-
The key factors which were considered to influence recruitment and retention were: the NHS system; current economic challenges; logistics; and support networks.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The crisis within NHS dentistry is well-documented,1 with many rural and coastal areas experiencing particular challenges in delivering services.2,3,4 The South West Peninsula (SWP), comprising Devon and Cornwall, has been described as a 'dental desert',5,6 with a recent Healthwatch report declaring that no dental practices in Devon were accepting new adult or child patients under the NHS.6 This depressing picture of NHS dentistry in England was reinforced by a BBC report in August 2022, which again highlighted South West England as an area of particular concern.7 In March 2021, NHS England reported that there were 73,872 patients on a waiting list for NHS treatment in Devon, with over 16,000 in Plymouth alone.8
The chief medical officer for England has previously highlighted the health inequality which exists within rural and coastal communities when compared to inland urban neighbours.9 Areas such as Devon and Cornwall experience a high level of health inequality, yet receive limited policy and research attention.10 The level of oral health inequality is well-illustrated in the data from the Plymouth oral health needs assessment undertaken in 2019.11 In wards with the greatest deprivation, 56% of five-year-olds had decay compared to only 6.7% in the more affluent areas.11 The same report highlighted the age-standardised incidence rate and the mortality rates for oral cancer in Plymouth, which were significantly higher than in England as a whole.11
Access to and availability of NHS dentistry is crucial in preventing oral disease and reducing oral health inequality. This has been a major challenge for rural and coastal areas for many years and appears to be closely linked to recruitment and retention (R&R) of the dental workforce. The situation was exacerbated by the COVID-19 pandemic,12 with strong indications that increasing numbers of dental professionals are leaving the profession.13 Data from England and Wales show that more than 1,000 dentists left the NHS during the last five years14 and a recent report from one of the large dental body corporates indicates that they have experienced an attrition rate of 18% for dentists over the year 2020-21 and 29.5% for qualified dental nurses.5,15 A reduction in workforce numbers can have a significant impact on access to dental services, erode the health and wellbeing of staff and undermine the financial sustainability of dental practices.4
Study rationale and aims
During the last five years there has been an 8% decrease in the number of dentists working within the NHS in Devon,14 and although this may be due to a variety of factors, R&R appears to be key. In response to growing concerns around R&R within dentistry, researchers at Peninsula Dental School collaborated with Devon and Cornwall Local Dental Committees (LDC) to explore the experiences of dental practices within the SWP through the question: 'what is the extent and nature of the recruitment and retention issues in the dental workforce in Devon and Cornwall?' The results provide insight into the extent and nature of recruitment issues facing dental practices within this rural and coastal community.
Materials and methods
Study design
A self-administered, online questionnaire delivered via JISC Online Surveys16 was used. The 29-item survey included 22 questions exploring various aspects of R&R and was distributed to dental practices in Devon and Cornwall. The survey questions were predominantly quantitative and focused on current practice vacancies, previous experience of recruitment and any specific problems encountered with workforce retention. Five questions invited free-text answers, providing the opportunity to express views on factors which could affect R&R. An overview of the questionnaire is included within Appendix 1.
The survey was voluntary and anonymous, although practice postcode data were collected to enable deduplication to ensure a single response per practice. The survey was piloted with members of Devon LDC and revised in line with their feedback on the content, format, relevance and readability of the survey.
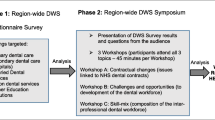
Rating scales were analysed using frequency analysis with quantitative data subject to descriptive statistical analysis and paired t-tests. Qualitative data from responses to free-text questions were analysed using Braun and Clarke's six recursive steps for reflexive thematic analysis.17,18 Independent coding, theme development and cross-checking were undertaken by multiple members of the research team. Final themes and codes were agreed by all and overseen by an experienced qualitative researcher to ensure rigour. A further step - utilising a framework approach19 based on existing sociological theory20 and influenced by previous dental research21 - was adopted to present the findings in a more practical format.
Participant recruitment
The survey (including study information and consent) was distributed through professional networks to all 295 dental practices in Devon, Cornwall and the Isles of Scilly (197 from Devon; 98 from Cornwall). The survey was open for a period of eight weeks between 29 July and 23 September 2022, with one response per practice requested. Reminders were sent out to maximise the response rate. As all practices were invited to participate, a sample size calculation was considered unnecessary. Ethical approval was obtained from the University of Plymouth Faculty of Health Research Ethics and Integrity Committee (reference number: 3382).
Results
In total, 134 responses were received. Deduplication accounted for exclusion of 26 responses, with a further two responses removed as they were outwith geographical boundaries. This provided a sample of 106 practices, equating to a 36% response rate. A similar response rate was obtained across the two counties, with a greater response obtained from practices that held an NHS contract compared to those which were solely private (Fig. 1).
The vast majority of respondents (94.4%) considered R&R a major factor in enabling patient access to NHS dentistry. The NHS dental contract was widely considered to be the main barrier to R&R of dental associates within the NHS, with income generation identified as a 'major' (n = 69) or 'significant' factor (n = 33) by 95.3% of respondents.
Recruitment
A large proportion of practices indicated they had vacancies at the time of data collection (76.6%; n = 82). More than half of practices currently had a vacancy for a dentist (57%; n = 60), and over three-quarters of these vacancies were within NHS practices (77%; n = 46). Several of these practices had multiple vacancies, with one declaring as many as six unfilled associate positions. Of the private practices responding to the survey, 54% had a vacancy for a dentist (n = 13).
Almost half the practices (48%; n = 51) had vacancies for a dental nurse, with several having multiple unfilled positions. The majority of practices affected were NHS, accounting for 80% of dental nurse vacancies. Other groups from within the dental team appeared to be less affected: hygienists/therapists with a 12% vacancy rate (n = 13); receptionists with 10% (n = 11); and practice managers with 1% (n = 1) (Fig. 2).
Previous difficulty in recruiting dentists was reported in 60.7% (n = 65) of practices, with 24.3% (n = 26) of practices reporting this had frequently been a problem, and 36.4% (n = 39) reporting this had always been a problem. Only 1.9% (n = 2) of respondents reported that recruitment of dentists had never been a problem.
Only 5.6% (n = 6) of practices stated they had never experienced difficulties recruiting dental staff. The number of practices experiencing difficulty with recruitment outweighed this considerably, with 27.1% (n = 29) stating they had always experienced difficulties, and 31.8% (n = 34) reporting that they had frequently experienced this difficulty. Moreover, 65.4% of practices reported that recruitment of dental staff had become much harder in recent years (n = 70), and 24.3% (n = 26) reported dental staff recruitment had become harder.
There were no significant differences in perception of recruitment of dentists between practices based in Devon and those based in Cornwall [t(104) = 0.394; p = 0.117]. Correspondingly, there were no significant differences between Cornwall- and Devon-based practices for reported recruitment or retention issues [t(104) = -0.430; p = 0.459 and t(102) = -0.281; p = 0.898, respectively].
Retention
In total, 43% said retention of dental staff was an issue, with 28% (n = 30) stating 'frequently' and 15% (n = 16) 'always'. Similarly, a large proportion of practices (78.5%; n = 84) reported retention of dental staff had become increasingly difficult in recent years, with 30.8% (n = 33) reporting it was much harder to retain dental staff, and 47.7% (51) reporting it was harder to retain dental staff.
Qualitative data
Free-text questions invited participants to share their views on the influencing factors impacting on R&R and the findings are summarised in Table 1. There were no significant differences between private practice and NHS practice, with the exception of the response 'career opportunities' [t(99) = -0.794; p <0.001*] which were reported as better within the private sector than the NHS. It is important to recognise that there is overlap within these themes/sub-themes and factors are often inextricably linked and interdependent.
NHS system
The current NHS dental contract was seen as the key factor impacting on R&R within the NHS, which was primarily related to remuneration and workload when compared to the private sector:
-
'The NHS dental service is a national disgrace and dentists and staff don't want to work in it' (#13).
The need for urgent change was highlighted by several respondents, with many fearful for the future of NHS dentistry:
-
'I am leaving NHS and going privately as my patience with the current contract is over' (#14).
Respondents noted that a lack of investment in NHS dentistry was a barrier to R&R within NHS practices. The financial constraints imposed by NHS funding impacted on the ability of practices to remunerate staff at a competitive rate, which was seen as a factor in R&R of staff:
-
'Lack of investment in NHS dentistry is the main reason for practices inability to offer staff competitive salaries' (#51).
Workload under the NHS was another issue raised, and many felt the continuing pressure to deliver units of dental activity (UDA) targets within an increasingly challenging environment led to significant stress and increased risk of mistakes, complaints and legal action:
-
'Risks of litigation, inability for dentists to provide the time and care patients need, pressures from practices to see more patients than appropriate for each dentist. Increases risk of mistakes, serious issues being missed such as oral cancer' (#50).
Economic challenges
Many respondents highlighted the lack of investment in NHS dentistry and reported the impact of the COVID-19 pandemic on the ability to retain and recruit dental staff within the NHS:
-
'Many dental nurses left during/post COVID-19 due to the increase workload for no reward' (#60).
Wage stagnation within the NHS and the rising cost of living led to staff seeking alternative roles within the job market:
-
'COVID and people deciding to take alternate careers...in lots of places, supermarkets are paying the same and have far less expectations on the role' (#99).
A number of respondents also suggested that 'Brexit' was a particular barrier to recruitment and retention of non-UK dentists:
-
'Brexit makes recruitment of EU dentists much more difficult' (#21).
Logistics
Location and travel were cited as an issue due to access to training, poor transport links, road congestion during summer months, and a preference for younger staff to live in urban locations:22
-
'We lost one dentist as her commute became intolerable as the traffic in Cornwall in the summer months has become incredibly congested, and she needed to work closer to home with her young children' (#109).
Accommodation and cost of living was identified as another factor, with house prices rising significantly in recent years:
-
'It is also more difficult in Cornwall now given the price of housing is astronomical' (#109)
Support networks
Respondents frequently mentioned 'support', although this had several different elements, including clinical, emotional and financial support. Leadership and management, mentoring and the value of personal and professional networks were also identified as important:
-
'Working in a rural practice can be quite isolating for younger dentists, especially after the support of the dental school environment' (#86).
Isolation was also highlighted in relation to cultural identity and lack of diversity within many rural areas:
-
'There is definitely a cultural barrier too...ie Diwali which would widely be celebrated in my previous practice in London. Here in Devon some of my colleagues had never even heard of it which can make one feel more isolated' (#20).
Access to training was seen as a potential barrier to R&R, with dental professionals having to travel significant distances to support their continuing professional development:
-
'More courses/teaching in Cornwall to enhance further training...not having to travel to Bristol and beyond for any worthwhile course' (#119).
The reduced number of dental foundation training practices in the area, their distribution, and ongoing mentorship were also highlighted as a potential issue:
-
'I also think the NHS needs to consider alternative options for foundation training and/or mentor training - this would help newer dentists' (#4).
The inability to retain students from Peninsula Dental School beyond graduation was highlighted as a frustration, and this was viewed by some as a shortcoming in admissions where too few 'local' students were being given the opportunity to train as a dentist or therapist at the University of Plymouth:
-
'Recruit local students to the dental school, otherwise they all return back to their homes in [the] UK away from Devon' (#19).
Deterioration in the state of mental health and wellbeing among many in the profession, particularly those within the NHS, was highlighted:
-
'In over 30 years of practice, I cannot remember a time when morale and enthusiasm for dentistry was lower' (#116).
Career progressionwas reported as a reason for dental staff leaving the NHS, and in some cases, the profession, which aligned with the work of Holmes et al.23 The lack of opportunities within dentistry, particularly the NHS, was deemed to impact deleteriously on retention, with respondents describing staff desire to pursue 'new challenges' (#86), 'career development outside of dentistry' (#25) and 'opportunities for a bigger or different challenge' (#26). This appeared to affect dental nurses more than any other group within the dental workforce.
Factors influencing recruitment and retention
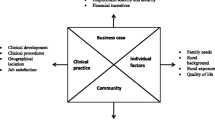
The four major themes identified from thematic analysis (see Table 1) are presented within a framework across two main dimensions (Table 2). Firstly, the framework delineates whether the factors operate at the macro- (societal, political, governmental), the meso- (group, institution), or the micro- (individual) level.20 Secondly, the framework also distinguishes between those factors which are national or general, and those which were identified as being of specific concern locally within the SWP region.
The factors set out in this framework constitute barriers to effective R&R in dentistry. Inevitably, factors at the different levels are interlinked, with many of those identified at the micro-level being framed by the socioeconomic issues situated at the macro-level, for example.
This framework allows identification of the different characteristics of the barriers described by our respondents, enabling consideration of how these issues may best be addressed, and by whom. Some proposed solutions exist at the macro level, requiring governmental intervention. This is certainly the case with some of the national issues, for example dental contract reform (DCR) or workforce planning, but is also the situation with some regional issues, such as transport infrastructure and the availability and cost of housing. The meso- and micro-level factors are potentially more easily addressed, although implementing changes to undergraduate training, overseas examinations, or dental foundation places are unlikely to be straightforward or rapid.
Recruitment solutions
Suggestions to improve R&R within the region included addressing issues at a local, regional and national level. The solutions focused on DCR, local recruitment into dentistry, increased numbers of training places, incentives to retain SWP graduates to stay in the South West, better access to training/continuing professional development (CPD) and improvements in peer support and mentorship.
Discussion
R&R within dentistry in rural and coastal areas has previously been highlighted as a serious issue which directly impacts on the availability oral healthcare services.4 The findings within this survey confirm that R&R is one of the major issues affecting dental access in Devon and Cornwall, with over three-quarters of practices reporting a current vacancy. The majority of dentist vacancies were within NHS practices (78%), but it is worth noting several private practices also reported a vacancy. Although the response rate from private practices was relatively small, of the 24 practices who did respond, over half (54%) reported a vacancy. Suggestions have previously been made that there is no shortage of dentists, simply a shortage of dentists willing to work in the NHS.24,25,26,27 Our findings would seem to contradict this view, when applied to a rural setting.
This is supported by the experience of others who have found recruitment of dentists to be challenging within the private sector in rural areas.3 The South West data on dentists are comparable with a recently published report from Cumbria, which indicates that 54% of practices in that region currently have at least one vacancy for a dentist.2 The survey data from Devon and Cornwall provide further evidence that, despite the establishment of a dental school within the region, R&R of dentists and dental staff remains a major barrier to care. The responses suggest that the situation is deteriorating, with almost 90%of respondents declaring that recruitment of dental staff had become more difficult in recent years. The data also revealed that retention was also a major problem, with more than three-quarters of practices reporting that it had now become harder to retain staff.
Training and support for the dental team were areas identified in our survey, the Cumbria report,2 and within the wider literature.23,28 This is an area which could, and should, be addressed in the short-term, with a focus on all members of the dental team, in order to support CPD, career progression, networking and social interaction.23 The Advancing dental care report29 published in 2021 highlighted the need to modernise training and provided a 'blueprint for change to reform dental education and training'.29 Many of the suggested initiatives could potentially have a positive impact on rural and coastal regions through flexible training and utilisation of skill mix, and this is an area currently being pursued in the South West.
A shortage of dentists is only part of the problem, and the challenges of R&R for other members of the dental team must not be overlooked. A dentist cannot operate without the rest of the dental team and with 54% of practices reporting at least one staff vacancy, this will undoubtedly impact on availability of services, standards of care and patient safety. R&R of dental staff appears to primarily affect NHS practices, and this may reflect a lack of opportunities for training, CPD and career development. Market conditions may also impact on R&R of dental staff within the NHS, with potentially better terms and conditions available in the private sector.
The number of vacancies for dental hygienists and therapists (DHT) were relatively small in comparison to dentists and nurses, although it was interesting to note that both private and NHS practices struggled to recruit. It would be overly simplistic to assume that low vacancy rates indicate no DHT workforce shortage and this may reflect under-utilisation within the NHS.30 The DCR changes proposed by NHS England, when fully implemented, will hopefully enable DHTs to utilise their full scope of practice within the NHS.31 If the proposed regulatory changes support and incentivise the use of DHTs within the general dental services, this is likely to lead to an increased demand within NHS practice, and recruitment could become more of an issue in the future.32
Difficulty with R&R does not only affect patient access to services - it can also impact on the health and wellbeing of the team and their ability to provide high-quality care. The loss of highly trained work colleagues can compromise teamwork, create additional stress within the team and undermine morale. Stability within a team is important and the constant churn of staff can also impact on patient safety, clinical outcomes and undermine patient experience.33,34 Patients value continuity of care33 and constant changes in workforce can directly impact on the quality of care provided.34
Concerns around mental health and wellbeing of the profession as highlighted within our survey is considered an important factor in staff attrition.35 Stress and burnout have been recognised as a serious issue within dentistry35 and it is incumbent on the profession, and those who regulate and commission our services, to create a supportive environment.30
As reported in our results, a more flexible approach to dental school admissions to facilitate a greater intake of students from the South West was considered a potential solution to improve R&R in the region. This is an area currently being explored by Peninsula Dental School through their Widening Participation Programme, which is supported by the Dental Schools Council and Health Education England.29 It is hoped this approach will not only promote equality of access to dentistry, but may also have a positive impact on R&R within the SWP.
There are limitations to this survey in terms of the response rate, particularly from the private sector. There is also a potential for sampling bias, with respondents affected by R&R issues more likely to participate in the survey. The survey was limited to practices within Devon and Cornwall and did not extend to an exploration of the barriers which exist for potential applicants who have chosen to work elsewhere. Despite these limitations, the authors consider the survey findings to be an important contribution to the literature base.
Conclusion
This research provides further evidence that rural areas are experiencing serious challenges with R&R in dentistry. This is impacting on access to dental services and although many of the problems are chronic, the situation appears to be deteriorating.
Our survey data highlighted a number of factors which need to be addressed to improve R&R in rural areas, which builds on the work of other published research.2,3,23 Some of these factors depend on a significant change in commissioning (NHS contract) or training (workforce planning/overseas registration exam [ORE]), while others are beyond the control and influence of the dental profession (transport, housing, cost of living). Other issues, such as access to training, support, mentorship and opportunities for career progression, can be addressed at both a practice and local level. This will require collaboration across multiple stakeholders in order to address some of the disadvantages (real and perceived) in living and working in a rural community.
This survey is an initial step in identifying some of the main issues which affect R&R in Devon and Cornwall and provide the beginnings of a robust evidence base for influencing change. Further in-depth research is key and will need to explore the various barriers which exist for different groups within the dental team. We believe this to be a critical area of research which could have a profound impact on service provision, workforce health and wellbeing, oral health improvements, and the long-term sustainability of NHS dentistry.

Appendix 1 Summary of survey questionnaire
References
National Audit Office. Dentistry in England. 2020. Available at https://www.nao.org.uk/wp-content/uploads/2020/03/Dentistry-in-England.pdf (accessed August 2023).
Burford B, Vance G. Report: The Dental Workforce in Cumbria: Newcastle University. October 2022. (Copy available from authors upon reasonable request).
Lewis J. Rural recruitment issues: A Cumbrian perspective. BDJ In Pract 2021; 34: 12-13.
Evans D, Mills I, Burns L, Bryce M, Hanks S. The dental workforce recruitment and retention crisis in the UK. Br Dent J 2023; 243: 573-577.
UK Parliament. Written evidence submitted by the Association of Dental Groups (RTR0010). 2022. Available at https://committees.parliament.uk/writtenevidence/42289/pdf/ (accessed August 2023).
Healthwatch. What people have told us about NHS dentistry: A review of our evidence - April to September 2021. 2021. Available at https://nds.healthwatch.co.uk/sites/default/files/reports_library/20211014_HWE%2520Dentistry%2520Update%2520Dec%25202021.pdf (accessed August 2023).
Green R, Agerholm H, Rogers L. Full extent of NHS dentistry shortage revealed by far-reaching BBC research. BBC News (London) 2022 August 8.
NHS England and NHS Improvement. Summary Oral Health Needs Assessment: South West of England. 2021. Available at https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2021/02/South-West-OHNA-Summary-Report.pdf (accessed August 2023).
UK Government. Chief Medical Officer's annual report 2021: health in coastal communities. 2021. Available at https://www.gov.uk/government/publications/chief-medical-officers-annual-report-2021-health-in-coastal-communities (accessed August 2023).
Asthana S, Gibson A. Averting a public health crisis in England's coastal communities: a call for public health research and policy. J Public Health (Oxf) 2022; 44: 642-650.
Plymouth City Council. Plymouth Oral Health Needs Assessment. 2019. Available at https://www.plymouth.gov.uk/sites/default/files/Oral%20Health%20Needs%20Assessment%202019%20%28v1.1%29.pdf (accessed August 2023).
Khaled K. Access to NHS dental care. BDJ in Pract 2021; 34: 5.
Dingle M, Balmer C. The impact of COVID-19 on dental nursing - The forgotten profession. BDJ Team 2021; 8: 14-19.
Ferguson S. 'Hanging by a thread': NHS dentists. Available at https://nhsdentists.github.io/website/ (accessed August 2023).
Association of Dental Groups. England's dental deserts: the urgent need to "level up" access to dentistry. May 2022. Available at https://www.theadg.co.uk/wp-content/uploads/2022/05/ADG-Report_The-urgent-need-to-level-up-access_April-2022_V3.pdf (accessed August 2023).
Jisc Online Surveys. About online surveys. Available at https://www.onlinesurveys.ac.uk/about/ (accessed August 2023).
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol 2006; 3: 77-101.
Braun V, Clarke V, Terry G. Thematic analysis. In Lyons A, Rohleder P (eds) Qualitative Research in Clinical and Health Psychology. London: Palgrave MacMillan, 2014.
Gale N K, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13: 117.
Collins R. Jonathan Turner's Macro-Micro-Meso Theory. Oxfordshire: Routledge, 2021.
Gallagher J E, Colonio-Salazar F B, White S. Supporting dentists' health and wellbeing - workforce assets under stress: a qualitative study in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3130-9.
NHS England and NHS Improvement. Dental Access for Adults and Children in Devon. 2021. Available at https://democracy.devon.gov.uk/documents/s34891/2021%2003%2008%20Devon%20Briefing%20Paper%20Final.pdf (accessed August 2023).
Holmes R D, Burford B, Vance G. Development and retention of the dental workforce: findings from a regional workforce survey and symposium in England. BMC Health Serv Res 2020; 20: 255.
BDJ Jobs. BDJ Jobs Recruitment Whitepaper. 2021. Available at https://www.morgannwgldc.org.uk/wp-content/uploads/2022/02/BDJ-Recruitment-Whitepaper-2021.pdf (accessed August 2023).
Tapper J. Cuts, closures, DIY dentistry: welcome to the NHS in Thérèse Coffey's seat. The Guardian (London) 2022 October 22.
General Dental Council. Registration Reports. Available at https://www.gdc-uk.org/about-us/what-we-do/the-registers/registration-reports (accessed August 2023).
D'Cruz L. BBC London Politics Show: Dental Crisis. 2022. Available at https://twitter.com/TheBDA/status/1528307851504103426 (accessed August 2023).
Evans D, Burns L, Mills I, Bryce M, Hanks S. Recruitment and retention in dentistry in the UK: a scoping review to explore the challenges across the UK, with a particular interest in rural and coastal areas. Br Dent J 2023; DOI: 10.1038/s41415-022-5406-0.
Health Education England. HEE's Advancing Dental Care Review: Final Report. 2021. Available at https://www.hee.nhs.uk/sites/default/files/documents/Advancing%20Dental%20Care%20Report%20Sept%2021.pdf (accessed August 2023).
Hallett G, Witton R, Mills I. A survey of mental wellbeing and stress among dental therapists and hygienists in South West England. Br Dent J 2022; DOI: 10.1038/s41415-022-5357-5.
NHS England. Letter: first stage of dental reform. 2022. Available at https://www.england.nhs.uk/wp-content/uploads/2022/07/B1802_First-stage-of-dental-reform-letter_190722.pdf (accessed August 2023).
NHS England. Building dental teams: Supporting the use of skill mix in NHS general dental practice. 2023. Available at https://www.england.nhs.uk/long-read/building-dental-teams-supporting-the-use-of-skill-mix-in-nhs-general-dental-practice-long-guidance/ (accessed August 2023).
The King's Fund. Continuity of care and the patient experience. 2010. Available at https://www.kingsfund.org.uk/sites/default/files/field/field_document/continuity-care-patient-experience-gp-inquiry-research-paper-mar11.pdf (accessed August 2023).
Mills I J. A person-centred Approach to holistic Assessment. Prim Dent J 2017; 6: 18-23.
Plessas A, Paisi M, Bryce M et al. Mental health and wellbeing interventions in the dental sector: a systematic review. Evid Based Dent 2022; DOI: 10.1038/s41432-022-0831-0.
Acknowledgements
The authors would like to thank Devon and Cornwall Local Dental Committees for their advice on developing the questionnaire and their support in distributing the survey. Additionally, we would like to thank our dental colleagues who participated in the study.
You can read more articles about developing your career via BDJ Jobs: https://www.bdjjobs.com/careers/.
Funding
The study was supported by a grant from the Faculty of Health Strategic Investment Fund, University of Plymouth.
Author information
Authors and Affiliations
Contributions
Ian Mills: developed questionnaire, undertook quantitative and qualitative analysis and led on writing the manuscript. Marie Bryce: contributed to all aspects of the study, including questionnaire development, qualitative analysis and oversight, writing text, language editing and proof-reading manuscript. Laura Clarry: contributed to quantitative and qualitative analysis, writing text and proof-reading manuscript. Deborah Evans: contributed to all aspects of the study, including questionnaire development, analysis, revising text and proof-reading manuscript. Sally Hanks: contributed to all aspects of the study, including questionnaire development, oversight of project, writing text, language editing and proof-reading manuscript.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval was obtained from the University of Plymouth Faculty of Health Research Ethics and Integrity Committee (reference number: 3382). Participants completed a consent form before undertaking the survey questionnaire which included agreement to allow the data to be used for research purposes and future publication.
A copy of the survey questionnaire is available in the appendix. The corresponding author should be contacted for access to the response data.
Rights and permissions
About this article
Cite this article
Mills, I., Bryce, M., Clarry, L. et al. Dental practice workforce challenges in rural England: survey into recruitment and retention in Devon and Cornwall. Br Dent J (2023). https://doi.org/10.1038/s41415-023-6276-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-6276-9
- Springer Nature Limited