Abstract
Background
The clinical behavior of prostate cancer is highly heterogeneous, with most patients diagnosed with localized disease that successfully responds to surgery or radiotherapy.
However, a fraction of men relapse after initial treatment because they develop drug resistance. The failure of anticancer drugs leaves resistant cancer cells to survive and proliferate, negatively affecting patient survival. Thus, drug resistance remains a significant obstacle to the effective treatment of prostate cancer patients. In this scenario, the involvement of extracellular vesicles (EVs) in intrinsic and acquired resistance have been reported in several tumors, and accumulating data suggests that their differential content can be used as diagnostic or prognostic factors. Thus, we propose a systematic study of literature to provide a snapshot of the current scenario regarding EVs as diagnostic and prognostic biomarkers resource in resistant prostate cancer.
Methods
We performed the current systematic review according to PRISMA guidelines and comprehensively explored PubMed, EMBASE and Google Scholar databases to achieve the article search.
Results
Thirty-three studies were included and investigated. Among all systematically reviewed EV biomarkers, we found mainly molecules with prognostic significance (61%), molecules with diagnostic relevance (18%), and molecules that serve both purposes (21%). Moreover, among all analyzed molecules isolated from EVs, proteins, mRNAs, and miRNAs emerged to be the most investigated and proposed as potential tools to diagnose or predict resistance/sensitivity to advanced PCa treatments.
Discussion
Our analysis provides a snapshot of the current scenario regarding EVs as potential clinical biomarkers in resistant PCa. Nevertheless, despite many efforts, the use of EV biomarkers in PCa is currently at an early stage: none of the selected EV biomarkers goes beyond preclinical studies, and their translatability is yet far from clinical settings.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the second most common cancer and the fifth leading cause of worldwide death among men, with about 375,000 men dying each year [1]. PCa is a very heterogeneous disease, with considerable differences in clinical evolution, ranging from clinically insignificant tumors to lethal castration-resistant PCa (CRPC). Despite advances in screening, surgery, and treatments, the prognosis of PCa patients is still unsatisfactory because relapse or late diagnosis occurs. The first line of treatment against advanced PCa is hormone therapy, also known as androgen-deprivation therapy (ADT). Hormone therapy usually works well initially, but most patients develop resistance to this treatment. Developing castration-resistant PCa (CRPC), cancer grows again within a few years, and new therapeutic options are required to treat the disease [2]. Taxane, docetaxel, or paclitaxel are currently used as first-line chemotherapy in CRPC patients. In addition, second-line hormonal therapies, such as abiraterone and enzalutamide, are also becoming available for metastatic CRPC (mCRPC) [3]. Despite these new therapeutics, the median survival of patients remains poor [4,5,6]. Thus, drug resistance remains a significant obstacle to the effective treatment of PCa patients. Current diagnostic assays, including serum prostate-specific antigen (PSA), commonly used as a marker for tumor growth, lack adequate specificity and sensitivity to diagnose the aggressiveness of the disease [7]. In the same way, although the advent of multiparametric imaging [8] has improved diagnostic performance in PCa diagnosis, it remains challenging to fully determine the severity and the aggressiveness of PCa [9, 10]. Therefore, there is an unmet need for non-invasive markers to select or predict CRPC patients sensitive to a specific drug, improve therapeutic decisions and minimize adverse effects.
In this scenario, extracellular vesicles (EVs) represent an appealing source of biomarkers derived from non-invasive liquid biopsy techniques for diagnosing cancer and monitoring disease evolution and therapeutic efficacy. EVs comprise heterogeneous subtypes of vesicles (i.e., exosomes, ectosomes, microvesicles) differentiated based on their biogenesis, release pathway, content, size and function. Because there is still no consensus on specific markers to determine their origin, we prefer to use the generic term of EVs.
EVs are secreted by cells in the body. They can reach body fluids, including blood, urine, semen, saliva, and their content (such as protein, miRNA, RNA, and DNA) directly relates to the physiopathological status of the cells from which they derived [11]. EVs mediate local and systemic intercellular communications [12] and play an active role in tumor development [13], including PCa [14, 15]. Moreover, they can induce phenotypic changes in recipient cells, and increasing experimental evidence supports their involvement in modulating tumor drug resistance [16, 17]. There are multiple ways in which EVs can affect drug resistance in cells, such as transferring drug efflux pumps, apoptotic modulators, and the drugs themselves [18]. Although the role of exosomes in drug resistance is not entirely known, data suggest that EVs are involved in the development of drug resistance in PCa. EVs from docetaxel-resistant PCa cell lines could confer resistance to docetaxel-sensitive lines [19]. Similarly, EVs isolated from camptothecin-resistant PCa cells transferred phenotypes associated with malignant transformation as well as chemoresistance to sensitive cell lines [20]. Moreover, PCa cell lines resistant to enzalutamide (Enz) exhibited higher EV secretion than their parental Enz-sensitive lines.
Additionally, EV secretion inhibition significantly reduced the viability of Enz-resistance lines [21]. Overall, this evidence highlights the role of EVs in drug resistance in PCa cells. Therefore, the molecular content of EVs can be utilized as a non-invasive means to help diagnose PCa or distinguish a subtype, monitor the disease state, or tailor the therapeutic choices. Here, we propose a systematic study of literature to summarize current knowledge on EVs as a source for diagnostic and/or prognostic biomarkers in resistant PCa.
Materials and methods
The systematic review was performed to establish if EVs can be used as biomarkers for diagnosing and prognosis of resistant PCa. This study did not require ethical approval because the data were carried out based on previously published data.
Literature search and study selection
We conducted this Systematic Review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (for more details, see PRISMA Checklist in Supplementary Materials). Three scientific electronic databases (PubMed, EMBASE, and Google Scholar) were used to conduct a systematic literature search. Studies published since 2000 were selected. The key terms used for the literature search are listed in Supplementary Materials (S1). Two authors independently reviewed the articles for eligibility from titles and abstracts. The full article was checked when it met the inclusion criteria, but the information was unclear only in the title and abstract. Finally, we included only manuscripts dealing with the utility of EVs as a resource of potential biomarkers to diagnose or predict resistance in PCa. The exclusion criteria involved non-English papers, reviews, metadata, single case reports, letters to the editor, methodological studies, and papers exclusively focused on mechanistic involvement of EVs. Moreover, we also excluded studies that did not deal with PCa therapeutic resistance. Finally, the entire selection flow and results of the literature search were checked by a third researcher.
Data extraction and collection
After selecting all collected records, two investigators summarized data that met the inclusion criteria into a customized Excel sheet database. For each study, the following characteristics were collected: type of biomarker, target, EV size, EV isolation, detection methods, in vitro model, in vivo model, clinical patients, clinical sample, drug, biomarker role, performance.
Results
Study selection
A flowchart of the literature search and the detailed selection process of the articles is reported in Fig. 1. A total of 344 potential eligible records related to EVs and their potential diagnostic and prognostic significance in drug resistance in PCa were retrieved from public databases and additional sources, such as relevant studies identified by references of other scientific papers. Then, 191 duplicates were deleted, and of the remaining 153 records, 69 were excluded because they were not original articles. Then, 35 records were further excluded after screening the abstract because irrelevant. The remaining eligible papers (49 records) were all downloaded and read, and 16 of them were excluded due to the lack of sufficient information or because they were not relevant to the topic. Finally, we included 33 records for qualitative synthesis.
EVs serving as diagnostic and prognostic biomarkers
Although the molecular content of EVs shows a large diversity, the search for novel PCa EV biomarkers in PCa drug resistance has focused mainly on analyzing non-coding RNAs (miRNAs, lncRNAs, circRNAs), mRNAs, and proteins (Fig. 2). In addition, changes in the number of EVs also appear to be potential biomarkers of resistant PCa forms.
In this systematic review, we classified the final 33 eligible articles into four subgroups according to the type of biomarker to diagnose or predict resistance/sensitivity to advanced PCa: (i) non-coding RNA, (ii) coding RNA, (iii) protein, and (iv) enumeration of EVs. All selected characteristics are summarized in Table 1.
Non-coding RNA
miRNA involvement in the initiation and progression of PCa has made this type of cargo of particular interest for biomarker development. Here we found nine works focused on miRNAs. Corcoran et al. proposed miR-34a as an exosomal predictive biomarker for response to docetaxel in PCa [22]. miR-34a expression decreased in PCa tissues from patients who experimented with recurrence after radical prostatectomy or radiation therapy compared with normal tissue. Then, the authors also verified the regulatory role of miR-34a on BCL-2 in response to docetaxel, suggesting it as an indicator of potential early treatment failure. Successively, a miRNA-array study identified and validated 12 deregulated miRNAs in EVs isolated from two PCa docetaxel-resistant cell models (DU145-TXR and PC3-TXR): miR-16-5p, miR-32-5p, miR-99b-5p, miR-451a, miR-1204, miR-23c, miR-3607-3p, miR-3915 were over-expressed; whereas miR-141-3p, miR-429, miR-192-3p, miR-3176 were down-expressed compared with parental cells [23]. Moreover, a bioinformatics approach identified a group of miRNAs (miR-32-5, miR-141-3p, miR-606, miR-381, miR-429) able to target TCF4 and confer resistance to docetaxel. However, the study did not investigate miRNA expression also in resistant patients. Several studies have identified specific EV miRNAs from blood as valuable prognostic biomarkers in CRPC patients. Notably, Huang et al. 2015 identified two plasma exosomal miRNAs, miR-1290 and miR-375, and verified their significant association with overall survival (OS) in CRPC patients [24]. Kaplan-Meier curves demonstrated that the combination of miR-1290 and miR-375 expressions had a strong synergistic effect. Moreover, incorporating both miRNAs into a putative clinical prognostic factors-based model that included PSA and ADT in CRPC stage significantly improved the predictive performance of the multivariate model (AUC: 0.73). More recently, plasma EV miRNAs have been proposed as biomarkers to predict the early occurrence of CRPC, with the advantage of allowing prompt remodeling of therapeutic regimens before CRPC is fully developed. By performing exosomal miRNA expression profiles from plasma of PCa patients native to treatment versus CRPC, CRPC-associated plasma miRNAs emerged (miR-423-3p, miR-320a, miR-99a-5p, miR-320d, miR-320b, and miR-150-5p) [25]. Among these, miR-423-3p was further validated in an additional multicenter cohort because it was most associated with CRPC. In this way, Guo et al. demonstrated that plasma exosomal miR-423-3p expression changed during PCa development, but it was not associated with the response to ADT treatment. Furthermore, combining miR-423-3p with PSA enhanced the prediction of CRPC (AUC: from 0.784 to 0.908). Also, serum EV miRNAs emerged as candidate prognostic biomarkers in CRPC patients. MiR-1246 was identified and validated as a serum exosomal biomarker of aggressive PCa (AUC: 0.926) [26]. Interestingly, this miR significantly correlated with poor prognostic clinicopathologic parameters (stage, lymph node metastasis, positive distant metastasis) and the highest expression in the group with distant metastasis. In addition, in vitro and in vivo data demonstrated its tumor suppressor role in PCa. Indeed, miR-1246 restoration in PC3 cells reduced cellular proliferation, anchorage-independent growth, invasiveness, and migration, inhibited endothelial mesenchymal transition, and promoted apoptosis. Recently, the same authors demonstrated that as PCa transit to neuroendocrine PCa (NEPC), an aggressive variant of CRPC, EVs released from tumor cells undergo alterations in the expression of specific miRNAs [7]. Interestingly, based on NGS dataset of NE tissues and CRPC-NE cell line (NCI-H660), authors employed machine learning algorithms to develop a miRNA-based classifier (miR-9-3p, miR-28-5p, miR-378d, miR-592, miR-155-5p, miR-23a-3p, miR-1180-3p, miR-143-3p, miR-499a-5p, miR-152-3p, miR-877-5p, miR-148a-39) able to stratify CRPC-NE from CRPC-Adeno.
Exosomal miRNAs isolated by serum of PCa patients after radiation therapy and their differential expression after radiation treatment showed their utility as biomarkers for predicting the efficacy of radiation therapy. A first study disclosed that the expression level of let-7a-5p and miR-21 was higher after radiation therapy in PCa patients with intermediate- and high-risk disease treated with curative radiotherapy (RT) [27]. A second one showed the overexpression of a set of miRNAs (miR-493-5p, miR-323a-3p, miR-411-5p, miR-494-3p, miR-379-5p, miR-654-3p, miR-409-3p, miR-543, and miR-200c-3p) significantly predicted the therapeutic benefit of carbon ion radiotherapy (CIRT). Furthermore, after therapy, the expression level of two specific miRNAs, miR-654-3p and miR-379-5p, was associated with CIRT efficacy [28].
We found only one study that proposed urine-derived EV miRNAs as predictive biomarkers. Fredsøe and colleagues developed and validated a biomarker model comprising five urine EV miRNAs (miR-151a-5p, miR-204-5p, miR-222-3p, miR-23b-3p, and miR-331-3p) with the serum PSA test. This model predicted disease aggressiveness and risk of postoperative biochemical recurrence risk in three cohorts (hazard ratio: 3.12, 2.24, and 2.15) of PCa patients, proving helpful in guiding treatment decisions [29].
Recently, several studies have investigated the prognostic role of circRNAs in CRPC. CircRNAs, are non-coding RNAs, that form continuous covalently closed-loops with neither 5ʹ-end cup nor 3ʹ-end poly-A tail. Increasing evidence indicates that circRNAs regulate many physiological and pathological processes, including cancer [30]. However, we found only one study that proposed circRNAs as diagnostic biomarkers of resistant PCa. Cao et al. identified 13 circRNAs derived from the AR gene through RNA-seq of 47 metastatic mCRPC specimens, cell models, and RNase R RNA-seq of patient-derived xenografts (PDXs) [31]. The expression of the four most abundant circRNAs (circAR-E2, circAR-E2In1, circAR-E2In2, circAR-E2) increased during the castration-resistant progression of PDXs and further to enzalutamide resistance. These same AR-derived circRNAs were also detected in plasma from mCRPC patients, suggesting them as circulating disease makers for CRPC.
Coding RNAs
We found ten studies that used EV mRNAs as biomarkers for resistant PCa. Most of these focused on androgen receptor (AR) as a useful biomarker in predicting or monitoring resistance to androgen targeted therapies in CRPC patients. Metastatic CRPC patients, treated with enzalutamide or abiraterone, showed a higher level of AR-V7 transcript in plasma-derived EVs. This marker correlated with shorter progression-free survival (PFS) and overall survival (OS) [32]. The same research group, some years later, aimed at verifying whether the expression of full-length AR (AR-FL) in EVs was helpful as a predictive biomarker of resistance to hormonal therapy (HT), in addition to AR-V7 [33]. Also, AR-LF expression significantly increased in AR-V7 positive patients, and it resulted helpful to stratify response and survival of patients. Specifically, based on the expression level of plasma-derived AR-FL, in combination with AR-V7, authors proposed a flowchart of clinical decisions to stratify responders, non-responders, and an intermediate population of patients that could benefit from HT, although AR-V7 positive. Similarly, also Joncas and colleagues revealed that plasmatic AR-V7 positive EVs were associated with a shorter PFS in CRPC patients [34]. Furthermore, the absolute quantification of AR-V7 and AR-FL was also performed from urinary EVs from patients with PC [35] and AR-FL expression was higher in hormone-sensitive PC (HSPC). On the contrary, the AR-V7 expression level was higher in CRPC patients, and also the ratio AR-V7/AR-FL was significantly higher in patients with CRPC than in those with HSPC. In another study, the presence of AR-V7 mRNA variant isolated in plasma of CRPC patients allowed identification of responders from not responders to anti-androgen drugs (such as abiraterone or enzalutamide) or standard-of-care treatments for advanced PCa (such as docetaxel or cabazitaxel) [36]. More recently, Del Re and colleagues evaluated the impact of AR-V7 and AR gain in plasma-derived EVs and in circulating free DNA on clinical outcome in chemotherapy-naïve mCRPC patients, treated with first-line abiraterone or enzalutamide, aiming to identify a valuable biomarker for the early detection of resistance to treatment [37]. AR-V7 and AR gain at baseline were associated with more aggressive cancers. The AR gain/AR-V7 combined analysis showed a prognostic and predictive value since both resulted significantly associated with shorter OS and PFS [37].
Among other potential biomarkers, two transcription factors, BRN4 and BRN2, were identified as biomarkers for predicting neuroendocrine differentiation in CRPC [38]. Authors demonstrated that PCa cells actively expressed and secreted both transcription factors in EVs to reprogram cancer cells, and enzalutamide treatment augmented their release. An interesting study conducted by Kato et al. showed that CD44 mRNA copy numbers could predict resistance to docetaxel in CRCP patients [39]. Zavridou and colleagues performed a comparison study on gene expression and DNA methylation markers in CTCs and paired plasma-derived EVs to evaluate their prognostic significance in mCRPC [40]. The authors reported a strong positive correlation between CTC counts and EV counts, and the level of CK-8 expression, GSTP1 and RASSF1A methylation status in EVs significantly correlated with shorter survival.
Recently, Vardaki and colleagues interrogated plasma-derived exosomes for predictive markers associated with radium-223 (Ra-223) treatment resistance [41]. Transcriptome analysis of EVs from patients revealed changes in RNA and protein levels related to bone-forming and bone lytic pathways and DNA damage repair and immune pathways. Notably, patients with a negative response to Ra-233 showed higher levels of PD-L1.
Proteins
The most investigated mechanism to explain resistance to chemotherapy remains the overexpression of multidrug resistance (MDR) genes. These genes encode the transporter proteins that play the role of a molecular pump leading to a decrease in the intracellular concentration of drugs. Several MDR proteins, such as P-glycoprotein (P-gp), could serve as biomarkers for assessing therapeutic resistance in PCa to docetaxel [42]. Furthermore, P-gp expression was associated with docetaxel resistance but not with the anticancer activity of cabazitaxel [43]. Therefore, serum exosomal P-gp level appeared helpful for diagnosing resistance and selecting a taxoid for CRPC patients.
Compared to a single EV protein, a panel of EV proteins is likely to provide greater specificity and sensitivity. In this perspective, Kharaziha et al. identified a panel of proteins differently enriched in exosomes secreted from docetaxel-sensitive and resistant PCa cells (DU145 Tax-Sen and DU145 Tax-Res, respectively) [44]. In particular, higher MDR-1, MDR-3, Endophilin-A2, and PABP4 levels characterized DU145 Tax-Res exosomes. The higher content of these proteins also featured EV isolated from the serum of docetaxel-resistant PCa patients compared with sensitive patients.
Some studies have reported altered integrin expression in association with PCa progression.
Integrin β4 (ITGB4) and vinculin (VCL) were also screened as potential diagnostic markers to define the progression and aggressiveness of taxane-resistant PCa [45]. Although these proteins were highly expressed in EVs derived from PC-3R cells compared with PC-3 cells, downregulation of ITGB4 and VCL did not affect tumor proliferation and taxane resistance but only reduced migration and invasion of PC-3R cells.
Krishn et al. proposed αvβ3 integrin as a diagnostic tool for PCa because it was more concentrated in the blood of CRCP patients than in unaffected individuals [46]. Furthermore, the authors demonstrated that αvβ3 integrin was co-expressed with CD-9 in a subpopulation of PSMA-positive exosomes. However, αvβ3 integrin level did not result informative to monitor response to therapy because it did not change in EVs isolated from plasma of mCRPC patients treated with ADT (enzalutamide or abiraterone acetate) compared to non-treated cases. In the same year, another study focused its attention on αV-integrin positive large oncosomes in PCa with aggressive features and proposed it as a potential prognostic biomarker [47]. In particular, a significant increase in large EVs shedding from invasive PCa cells resistant (DU145R80) to inhibitors of the mevalonate pathway was detected. These large EVs showed an increased amount of integrin alpha-V on their surface, functionally involved in the increased adhesion and invasion of recipient cells via AKT [47]. Also, gamma-glutamyltransferase 1 (GGT1), a cell surface enzyme that regulates the catabolism of extracellular gamma-glutamyl transpeptidase (GSH), has been proposed as a possible marker for advanced PCa [48]. Although GGT1 was upregulated in EVs isolated from androgen-independent C4-2 and bone-metastatic C4-2B cells, no association was found between GGT activity and CRPC patients. On the otherwise, it resulted useful to distinguish PCa patients from benign prostatic hypertrophy (BPH) patients, although both exhibited similar serum PSA levels.
Recently, also protein EVs cargo emerged as valuable biomarkers for resistance form of PCa. Examination of the protein repertoire of EVs from NEPC cellular models (LNCaP-AR-Enzalutamide resistant cells and NCI-H660 cells compared to LNCap-AR) by mass spectrometry identified thrombospondin 1 (TSP1) as over-expressed [7]. In addition, the study consolidated its potential diagnostic value for NEPC, revealing its over-expression also in EVs isolated from sera of CRPC-NE patients. Ishizuya and colleagues showed higher protein expression levels of actinin-4 (ACTN4) in serum EVs of CRPC patients compared to those from patients who received ADT. Furthermore, as ACTN4 appeared highly expressed in tumor biopsies from untreated patients with metastatic PCa, the authors suggested that the expression level of this protein in serum could reflect the metastatic progression of PCa [49]. ACTN4 was also proposed as a potential therapeutic target for CRPC because its RNA interference-mediated downregulation reduced tumor growth and invasion in vivo. Another recent study revealed the diagnostic and therapeutic potential of yes-associated protein (YAP1) for enzalutamide resistance [50]. EVs isolated from LNCaP-Enzalumide resistant cells and sera of patients resistant to the drug overexpressed YAP1. In addition, the study demonstrated for the first time the role of COUP-TFII/miR-21/YAP1 regulation axis to enzalutamide resistance in PCa via positive regulation of cancer stemness and lipid metabolism.
Enumeration of EVs
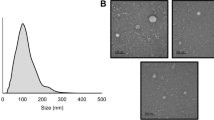
Some clinical studies have also shown that the number of plasmatic exosomes may represent a valuable new tool for monitoring cancer patients. Thus, tumor-derived EV (tdEV) enumeration has also gained much attention as a potential biomarker to aid CRPC patients’ management. Biggs and colleagues developed a liquid biopsy approach based on enumeration of prostate microvesicles (PMP, range size: 100–1000 nm) for diagnosing and clinical follow-up [51]. PMP levels significantly increased in plasma of metastatic and CRPC patients compared to patients with localized PCa and distinguished PCa patients with Gleason Score ≥ 8 disease, a high-risk prognostic factor of PCa recurrence. Moreover, PMP levels could also be used to predict early PCa recurrence after prostatectomy. Using the CellSearch system, Nanou et al., reported that the concentration of large tdEVs (1000–14000 nm) in the blood of CRPC patients was significantly higher and associated with worse OS [52, 53]. In addition, enumeration of tdEVs showed equivalent prognostic power of circulating tumor cells (CTCs) in CRPC, but more helpful utility because more concentrated (20 times higher than CTCs).
Discussion
Considerable efforts have been made through the years to identify biomarkers for PCa. However, identifying new biomarkers reflecting the phenotype of this multifocal and heterogeneous malignancy with high discriminative precision for diagnosis, risk-stratification, and treatment tailoring remains an urgent need. In this context, EVs represent an attractive source of cancer-derived molecules in liquid biopsy. They offer the possibility of reflecting tumor heterogeneity through molecular analysis of body fluids, providing comprehensive information about the genetic landscape at diagnosis, and tracking genomic evolution over time.
The production of EVs from prostate cells was first reported in the 1970–1980s [54, 55]; from then on, they are detected in tumor tissues, plasma/serum, and urine from PCa patients. The detection of biomolecules protected by the lipid layer such as the EVs, is advantageous in susceptibility to degradation. It may improve the sensitivity of new or established PCa biomarkers. Recently, a prospective study reported that plasmatic exosomes expressing PSA discriminated PCa from BPH patients and healthy controls, with sensitivity and specificity significantly higher than conventional PSA test [56]. ExoDx Prostate (IntelliScore) test is the first commercial exosomal molecular test, which analyzes RNA expression of three genes (ERG, PCA3, and SPDEF) from urine. Two trials have reported its better sensitivity to predict high-grade PCa (GS ≥ 7) at initial biopsy and defer unnecessary biopsies than existing risk calculators and standard clinical data [57, 58]. Including this test in the 2019 National Comprehensive Cancer Center Network Guidelines (NCCN) for early detection of PCa highlights the utility of exosome-derived biomarkers for early PCa detection.
To date, several clinical trials are currently ongoing (Table 2), but among these, few studies concern therapeutic resistance in PCa: only one clinical study (NCT03601143) is currently underway to predict resistance under androgen-receptor signaling inhibitors using AR-V7.
Thus, the development of non-invasive methods to facilitate early diagnosis of PCa, determine the patients’ prognosis, and predict responses to a given therapeutic intervention, above all for more aggressive disease stages as CRPC, remain unmet needs. To better understand how EVs may be useful as diagnostic or prognostic biomarkers in resistant PCa, we analyzed the state of the art of performed studies in which EVs molecular content and quantitative and molecular analyses were assessed for providing clinically relevant information about resistance/sensitivity in PCa. We identified 33 studies meeting the set inclusion criteria: 81% of the selected studies proposed molecular markers, while only a few studies (9%) focused on quantitative markers as EVs enumeration. Among our selected papers, the primary clinical value provided from selected biomarkers was prognostic with identifying several molecules that could serve as drug-resistance predictors for PCa treatment. Our work showed that blood-derived EVs were extensively investigated in biomarker studies for resistant PCa, while few studies performed analyses with urine. Therefore, blood appears to be eligible biofluid, especially for PCa patients with distal metastasis or after radical prostatectomy. The isolation of EV from blood and urine with high purity is not trivial because both fluids contain structures or components that may mask or disrupt analysis. Many methods are available for EVs isolation based on different physical and molecular EV features (differential centrifugation, filtration, immunocapture). Our results showed extensive use of extraction kits for EV isolation and purification. Although isolation kits seem more suitable for the clinical setting than low-throughput and time-consuming methods such as differential centrifugation, it is not always specified how they may affect the sample source. Among selected papers, the search for novel PCa EV biomarkers appeared focused mainly on analyzing miRNAs, mRNAs, and proteins (29, 29, and 32%, respectively). We found no study dealing with lipids or glycans as biomarkers in resistant PCa. Standard analytical methods to assay the molecules of interest, such as PCR for nucleic acid and immune-based methods for protein, were mainly used. In addition, several omics methods, such as next-generation sequencing and mass spectroscopy, allowed massive analyses for identifying novel EV biomarkers for resistant PCa.
According to a new report by Grand View Research, Inc, the global exosome diagnostic and therapeutics market size was valued at $ 39 million in 2016 and is expected to reach USD 2.28 billion by 2030. Despite EVs’ growing potential clinical utility and the growing number of successful examples of proposed markers, there is a significant disparity in the number of new EV biomarkers proposed and those currently in clinical use. The lack of gold standards is an obstacle in reaching the clinical application of EV-based biomarkers. In this sense, a first hurdle that needs to be addressed regards EV heterogeneity. There is no broad consensus on specific markers to determine EV origin and identify their specific disease sources. Many efforts should be addressed to better explore the heterogeneity of EVs in terms of biophysical properties, surface composition, and molecular cargo to develop more specific and sensitive assays for detecting prostate-specific EV biomarkers.
Moreover, the lacking of standardized methods to EV isolate, purify, characterize makes it challenging to compare results of different studies and affects experimental data reproducibility. The lack of a universal normalization method for the results of EV experiments also does not facilitate the interpretation and comparison of results. In addition, extensive prospective studies comparing these new emerging biomarkers are required to assess their clinical value in PCa detection and prognosis.
Concluding, the search for potential EV biomarkers is open and promising. As multiple reservoirs of biomarkers, EVs pave truly massive utilities and advantages in personalized medicine of cancer. Therefore, EVs are expected to become part of the diagnosis, prognosis, and treatment management of PCa and its resistant forms, but methodological challenges remain to address before their clinical translation.
Data availability
The literature datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca-a Cancer J Clin. 2021;71:209–49.
Bumbaca B, Lin W. Taxane resistance in castration-resistant prostate cancer: mechanisms and therapeutic strategies. Acta Pharmaceutica Sin B. 2018;8:518–29.
Liu JM, Lin CC, Liu KL, Lin CF, Chen BY, Chen TH, et al. Second-line hormonal therapy for the management of metastatic castration-resistant prostate cancer: A real-world data study using a claims database. Scientific Rep. 2020;10:1–7.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
Bhagirath D, Liston M, Akoto T, Lui B, Bensing BA, Sharma A, et al. Novel, non-invasive markers for detecting therapy induced neuroendocrine differentiation in castration-resistant prostate cancer patients. Sci Rep. 2021;11:8279.
Hoeks CMA, Barentsz JO, Hambrock T, Yakar D, Somford DM, Heijmink S, et al. Prostate cancer: Multiparametric MR imaging for detection, localization, and staging. Radiology 2011;261:46–66.
Purysko AS, Bittencourt LK, Bullen JA, Mostardeiro TR, Herts BR, Klein EA. Accuracy and interobserver agreement for prostate imaging reporting and data system, Version 2, for the characterization of lesions identified on multiparametric MRI of the prostate. Am J Roentgenol. 2017;209:339–45.
Girometti R, Giannarini G, Greco F, Isola M, Cereser L, Como G, et al. Interreader agreement of PI-RADS v. 2 in assessing prostate cancer with multiparametric MRI: A study using whole-mount histology as the standard of reference. J Magn Reson Imaging. 2019;49:546–55.
Jan AT, Rahman S, Khan S, Tasduq SA, Choi I. Biology, pathophysiological role, and clinical implications of exosomes: A critical appraisal. Cells. 2019;8:1–19.
Penfornis P, Vallabhaneni KC, Whitt J, Pochampally R. Extracellular vesicles as carriers of microRNA, proteins and lipids in tumor microenvironment. Int J Cancer. 2016;138:14–21.
Akoto T, Saini S. Role of exosomes in prostate cancer metastasis. Int J Mol Sci. 2021;22:1–19.
Ni J, Bucci J, Malouf D, Knox M, Graham P, Li Y. Exosomes in cancer radioresistance. Front Oncol. 2019;9:1–9.
Malla B, Zaugg K, Vassella E, Aebersold DM, Dal Pra A. Exosomes and exosomal MicroRNAs in prostate cancer radiation therapy. Int J Radiat Oncol Biol Phys. 2017;98:982–95.
Lucotti S, Rainaldi G, Evangelista M, Rizzo M. Fludarabine treatment favors the retention of miR-485-3p by prostate cancer cells: implications for survival. Mol Cancer. 2013;12:52.
Sahebi R, Langari H, Fathinezhad Z, Bahari Sani Z, Avan A, Ghayour Mobarhan M, et al. Exosomes: New insights into cancer mechanisms. J Cell Biochem. 2020;121:7–16.
Xavier CPR, Caires HR, Barbosa MAG, Bergantim R, Guimaraes JE, Vasconcelos MH. The role of extracellular vesicles in the hallmarks of cancer and drug resistance. Cells. 2020;9:1–34.
Corcoran C, Rani S, O’Brien K, O’Neill A, Prencipe M, Sheikh R, et al. Docetaxelresistance in prostate cancer: Evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS ONE. 2012;7:1–12.
Panagopoulos K, Cross-Knorr S, Dillard C, Pantazatos D, Del Tatto M, Mills D, et al. Reversal of chemosensitivity and induction of cell malignancy of a non-malignant prostate cancer cell line upon extracellular vesicle exposure. Mol Cancer. 2013;12:1–16.
Peak TC, Panigrahi GK, Praharaj PP, Su YX, Shi LH, Chyr J, et al. Syntaxin 6-mediated exosome secretion regulates enzalutamide resistance in prostate cancer. Mol Carcinogenesis. 2020;59:62–72.
Corcoran C, Rani S, O’Driscoll L. miR-34a is an intracellular and exosomal predictive biomarker for response to docetaxel with clinical relevance to prostate cancer progression. Prostate 2014;74:1320–34.
Li J, Yang X, Guan H, Mizokami A, Keller ET, Xu X, et al. Exosome-derived microRNAs contribute to prostate cancer chemoresistance. Int J Oncol 2016;49:838–46.
Huang X, Yuan T, Liang M, Du M, Xia S, Dittmar R, et al. Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. Eur Urol. 2015;67:33–41.
Guo T, Wang Y, Jia J, Mao X, Stankiewicz E, Scandura G, et al. The identification of plasma exosomal miR-423-3p as a potential predictive biomarker for prostate cancer castration-resistance development by plasma exosomal miRNA sequencing. Front Cell Dev Biol. 2020;8:602493.
Bhagirath D, Yang TL, Bucay N, Sekhon K, Majid S, Shahryari V, et al. microRNA-1246 is an exosomal biomarker for aggressive prostate cancer. Cancer Res. 2018;78:1833–44.
Malla B, Aebersold DM, Dal Pra A. Protocol for serum exosomal miRNAs analysis in prostate cancer patients treated with radiotherapy. J Trans Med. 2018;16:1–13.
Yu Q, Li P, Weng ML, Wu S, Zhang YF, Chen X, et al. Nano-vesicles are a potential tool to monitor therapeutic efficacy of carbon ion radiotherapy in prostate cancer. J Biomed Nanotechnol. 2018;14:168–78.
Fredsoe J, Rasmussen AKI, Mouritzen P, Borre M, Orntoft T, Sorensen KD. A five-microRNA model (pCaP) for predicting prostate cancer aggressiveness using cell-free urine. Int J Cancer. 2019;145:2558–67.
Vo JN, Zhang YJ, Shukla S, Xiao LB, Robinson D, Wu YM, et al. The landscape of circular RNA in cancer. Cancer Res. 2018;176:869–81.
Cao SB, Ma TF, Ungerleider N, Roberts C, Kobelski M, Jin LJ, et al. Circular RNAs add diversity to androgen receptor isoform repertoire in castration-resistant prostate cancer. Oncogene 2019;38:7060–72.
Del ReM, Biasco E, Crucitta S, Derosa L, Rofi E, Orlandini C, et al. The detection of androgen receptor splice variant 7 in plasma-derived exosomal RNA strongly predicts resistance to hormonal therapy in metastatic prostate cancer patients. Eur Urol. 2017;71:680–7.
Del ReM, Crucitta S, Sbrana A, Rofi E, Paolieri F, Gianfilippo G, et al. Androgen receptor (AR) splice variant 7 and full-length AR expression is associated with clinical outcome: a translational study in patients with castrate-resistant prostate cancer. BJU Int. 2019;124:693–700.
Joncas FH, Lucien F, Rouleau M, Morin F, Leong HS, Pouliot F, et al. Plasma extracellular vesicles as phenotypic biomarkers in prostate cancer patients. Prostate 2019;79:1767–76.
Woo HK, Park J, Ku JY, Lee CH, Sunkara V, Ha HK, et al. Urine-based liquid biopsy: Non-invasive and sensitive AR-V7 detection in urinary EVs from patients with prostate cancer. Lab a Chip. 2019;19:87–97.
Foroni C, Zarovni N, Bianciardi L, Bernardi S, Triggiani L, Zocco D, et al. When less is more: Specific capture and analysis of tumor exosomes in plasma increases the sensitivity of liquid biopsy for comprehensive detection of multiple androgen receptor phenotypes in advanced prostate cancer patients. Biomedicines. 2020;8:1–14.
Del Re M, Conteduca V, Crucitta S, Gurioli G, Casadei C, Restante G, et al. Androgen receptor gain in circulating free DNA and splicing variant 7 in exosomes predict clinical outcome in CRPC patients treated with abiraterone and enzalutamide. Prostate Cancer Prostatic Dis. 2021;24:524–31.
Bhagirath D, Yang TL, Tabatabai ZL, Majid S, Dahiya R, Tanaka Y, et al. BRN4 is a novel driver of neuroendocrine differentiation in castration-resistant prostate cancer and is selectively released in extracellular vesicles with BRN2. Clin Cancer Res. 2019;25:6532–45.
Kato T, Mizutani K, Kawakami K, Fujita Y, Ehara H, Ito M. CD44v8-10 mRNA contained in serum exosomes as a diagnostic marker for docetaxel resistance in prostate cancer patients. Heliyon 2020;6:e04138.
Zavridou M, Strati A, Bournakis E, Smilkou S, Tserpeli V, Lianidou E. Prognostic significance of gene expression and DNA methylation markers in circulating tumor cells and paired plasma derived exosomes in metastatic castration resistant prostate cancer. Cancers (Basel). 2021;13:1–14.
Vardaki I, Corn P, Gentile E, Song JH, Madan N, Hoang A, et al. Radium-223 treatment increases immune checkpoint expression in extracellular vesicles from the metastatic prostate cancer bone microenvironment. Clin Cancer Res. 2021;27:3253–64.
Corcoran C, Rani S, O’Brien K, O’Neill A, Prencipe M, Sheikh R, et al. Docetaxel-resistance in prostate cancer: Evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS One. 2012;7:e50999.
Kato T, Mizutani K, Kameyama K, Kawakami K, Fujita Y, Nakane K, et al. Serum exosomal P-glycoprotein is a potential marker to diagnose docetaxel resistance and select a taxoid for patients with prostate cancer. Urologic Oncol: Semin Original Investig. 2015;33:385.e15–e20.
Kharaziha P, Chioureas D, Rutishauser D, Baltatzis G, Lennartsson L, Fonseca P, et al. Molecular profiling of prostate cancer derived exosomes may reveal a predictive signature for response to docetaxel. Oncotarget 2015;6:21740–54.
Kawakami K, Fujita Y, Kato T, Mizutani K, Kameyama K, Tsumoto H, et al. Integrin β4 and vinculin contained in exosomes are potential markers for progression of prostate cancer associated with taxane-resistance. Int J Oncol 2015;47:384–90.
Krishn SR, Singh A, Bowler N, Duffy AN, Friedman A, Fedele C, et al. Prostate cancer sheds the αvβ3 integrin in vivo through exosomes. Matrix Biol. 2019;77:41–57.
Ciardiello C, Leone A, Lanuti P, Roca MS, Moccia T, Minciacchi VR, et al. Large oncosomes overexpressing integrin alpha-V promote prostate cancer adhesion and invasion via AKT activation. J Experimental Clin Cancer Res. 2019;38:1–16.
Kawakami K, Fujita Y, Matsuda Y, Arai T, Horie K, Kameyama K, et al. Gammaglutamyltransferase activity in exosomes as a potential marker for prostate cancer. BMC Cancer. 2017;17:1–12.
Ishizuya Y, Uemura M, Narumi R, Tomiyama E, Koh Y, Matsushita M, et al. The role of actinin-4 (ACTN4) in exosomes as a potential novel therapeutic target in castration-resistant prostate cancer. Biochem Biophys Res Commun. 2020;523:588–94.
Lee HC, Ou CH, Huang YC, Hou PC, Creighton CJ, Lin YS, et al. YAP1 overexpression contributes to the development of enzalutamide resistance by induction of cancer stemness and lipid metabolism in prostate cancer. Oncogene 2021;40:2407–21.
Biggs CN, Siddiqui KM, Al-Zahrani AA, Pardhan S, Brett SI, Guo QQ, et al. Prostate extracellular vesicles in patient plasma as a liquid biopsy platform for prostate cancer using nanoscale flow cytometry. Oncotarget 2016;7:8839–49.
Nanou A, Coumans FAW, Dalum G, Zeune LL, Dolling D, Onstenk W, et al. Circulating tumor cells, tumor-derived extracellular vesicles and plasma cytokeratins in castration-resistant prostate cancer patients. Oncotarget 2018;9:19283–93.
Nanou A, Miller MC, Zeune LL, de Wit S, Punt CJA, Groen HJM, et al. Tumour-derived extracellular vesicles in blood of metastatic cancer patients associate with overall survival. Br J Cancer. 2020;122:801–11.
Stegmayr B, Ronquist G. PROMOTIVE EFFECT ON HUMAN-SPERM PROGRESSIVE MOTILITY BY PROSTASOMES. Urological Res. 1982;10:253–7.
Post H, Wiche R, Sen PC, Hoffbauer G, Albrecht M, Seitz J, et al. Identification of a plasma membrane Ca2+-ATPase in epithelial cells and aposomes of the rat coagulating gland. Prostate 2002;52:159–66.
Logozzi M, Angelini DF, Giuliani A, Mizzoni D, Di Raimo R, Maggi M, et al. Increased plasmatic levels of PSA-expressing exosomes distinguish prostate cancer patients from benign prostatic hyperplasia: A prospective study. Cancers. 2019;11:1–11.
McKiernan J, Donovan MJ, O’Neill V, Bentink S, Noerholm M, Belzer S, et al. A novel urine exosome gene expression assay to predict high-grade prostate cancer at initial biopsy. Jama Oncol. 2016;2:882–9.
McKiernan J, Donovan MJ, Margolis E, Partin A, Carter B, Brown G, et al. Prospective adaptive utility trial to validate performance of a novel urine exosome gene expression assay to predict high-grade prostate cancer in patients with prostate-specific antigen 2-10 ng/ml at initial biopsy. Eur Urol. 2018;74:731–8.
Author information
Authors and Affiliations
Contributions
Conceptualization—AMG and CC. Methodology—AMG and CC. Validation—AMG, CC, and MS. Investigation—AMG and CC, Resources—AMG and CC, Data curation—AMG and CC. Writing-original draft preparation—AMG. Writing-review and editing—CC. Supervision—MS. Funding acquisition—MS. All authors have read and agreed to the published version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Grimaldi, A.M., Salvatore, M. & Cavaliere, C. Diagnostic and prognostic significance of extracellular vesicles in prostate cancer drug resistance: A systematic review of the literature. Prostate Cancer Prostatic Dis 26, 228–239 (2023). https://doi.org/10.1038/s41391-022-00521-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00521-w
- Springer Nature Limited
This article is cited by
-
ND630 controls ACACA and lipid reprogramming in prostate cancer by regulating the expression of circKIF18B_003
Journal of Translational Medicine (2023)