Abstract
Background
The clinical part of this randomized controlled trial concerning phototherapy of neonates with hyperbilirubinemia showed that the recommended blue–green LED light (≈478 nm) was 31% more efficient than standard blue LED light (≈459 nm) measured by the decline in total serum bilirubin. Lumirubin has biologic effects. The aim was to compare the serum bilirubin isomers, efficacy, and biologic effects between the two phototherapy groups.
Methods
Inclusion criteria: neonates healthy except for hyperbilirubinemia, gestational age ≥33 weeks, birth weight ≥1800 g, and postnatal age >24 h. Forty-two neonates were randomized to receive overhead blue–green light and 44 blue light. Treatment 24 h. The light irradiance was equal.
Results
The percentage decrease of combined bilirubin isomers was 47.8% for blue–green light vs 33.4% for blue light, the ratio being 1.43. Corresponding values for Z,Z-bilirubin were 55.6% vs 44.2%, the ratio being 1.26. The increase in the absolute serum concentrations of the photoisomer Z,E-bilirubin and thereby combined photoisomers were greater using blue light.
Conclusion
Blue–green light was essentially more efficient determined by the decline of combined bilirubin isomers and Z,Z-bilirubin itself. Regarding biological effects neonates receiving blue–green light might be more affected than neonates receiving blue light.
Impact
-
Phototherapy of hyperbilirubinemic neonates using blue–green LED light with a peak emission of 478 nm was 43% more efficient than standard blue LED light with a peak emission of 459 nm was measured by the decline of serum combined bilirubin isomers, and the decline of toxic Z,Z-bilirubin was 26% greater.
-
Apparently, there was a discrepancy between the huge drop in total serum bilirubin and the low serum concentrations of E,Z-bilirubin and E,Z-lumirubin. This was caused by the rapid excretion of E,Z-lumirubin.
-
Lumirubin has biologic effects. Due to greater lumirubin production neonates exposed to blue–green light might be more affected than those exposed to blue light.
Similar content being viewed by others
Introduction
All neonates develop hyperbilirubinemia during the first days of life. In a few cases, the bilirubin concentration rises to such a high level that the neonate risks developing acute- and, in some cases chronic, bilirubin encephalopathy (kernicterus spectrum disorders).1,2 The standard treatments are phototherapy and blood exchange transfusion. In the industrialized world, 2–5% of healthy neonates with a gestational age ≥35 weeks receive phototherapy.3,4 The frequencies are higher in neonates with lower gestational ages.
During the last 60 years, studies have been performed to determine what light quality (wavelength) is most effective.5 Blue light with peak emission around 460 nm, corresponding to the in vitro light absorption curve of the bilirubin–albumin complex in plasma, has been the standard treatment worldwide.5 In three randomized controlled trials, including the present trial, we have compared the efficacy of blue–green (turquoise) light with standard blue light during phototherapy of hyperbilirubinemic neonates, as determined by the decrease of total serum bilirubin (TSB).6,7,8 In the first trial we found that the effect of blue–green fluorescent light with peak emission at 490 nm was 18% more efficient than the blue fluorescent light with peak emission at 452 nm.6 The second trial showed that blue–green LED light with peak emission at 497 nm and blue LED light with peak emission at 459 nm were equally efficient7. In the clinical part of the present trial, we showed that blue–green LED light with peak emission at 478 nm was 31% more efficient than blue LED light with peak emission at 459 nm,8 as measured by the decline in TSB determined by a diazo-method.9 Based on these studies, we demonstrated a clinical action spectrum within the spectral range 452–497 nm with peak efficacy at 478 nm for phototherapy of jaundiced neonates.10 This action spectrum is in agreement with the clinical action spectrum in the circulating blood calculated by Lamola et al.11,12 using an optical model of neonatal skin. Therefore, we recently recommended the use of blue–green LED light with peak emission at 480 nm instead of standard blue light with peak emission at 460 nm,8,10 as also proposed by Lamola et al.11,12 and the American Academy of Pediatrics.1 This highlights the question of the bilirubin isomers in plasma during the present phototherapy trial. The distribution of the bilirubin isomers in the two earlier trials has been described earlier.6,13
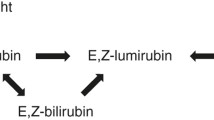
When the natural Z,Z-bilirubin molecule absorbs a photon, it can be converted to stereoisomers, reversibly to the configurational isomers Z,E- and E,Z- bilirubin, and irreversibly to the structural isomers E,Z- and E,E-lumirubin (cyclobilirubin) (Fig. 1).14,15
The aim of the study was to compare (1) the serum bilirubin isomers, (2) efficacy determined by the decline in Z,Z-bilirubin, and combined bilirubin isomers, and (3) biological effects between the neonates exposed to blue–green light and those exposed to standard blue light.
Methods
Study groups
The study was performed at the Department of Pediatrics, Aalborg University Hospital, Aalborg, Denmark between 1 March 2017 and 31 July 2018. The study groups have been described in the clinical part of this randomized controlled trial.8 In short, inclusion criteria: Healthy neonates except for treatment-dependent hyperbilirubinemia, gestational age ≥33 weeks, birth weight ≥1800 g, and postnatal age >24 h and ≤28 days. One hundred and two neonates were randomized to either blue–green LED light with a peak emission wavelength of 478 nm or blue LED light with a peak emission wavelength of 459 nm, 51 in each group. In the clinical part of the trial, two neonates in each group were excluded. Furthermore, in the present part of the trial seven neonates in the blue–green light group and five neonates in the blue-light group were withdrawn, because too little serum volume was obtained to analyze the bilirubin isomers. Thus, we present data from 42 neonates exposed to blue–green overhead light and 44 neonates to blue overhead light. The neonates were treated when their TSB was above the phototherapy limit according to the Guidelines of the North Denmark Region,16 which are based on the Norwegian Guidelines.17 All neonates were treated for 24 h.
Measurements
The irradiance was measured with a specialized spectrometer with equal sensitivity in the entire emission wavelength range (Ocean Optics, Model 2000+, Dunedin, FL). The irradiance was equal for the two groups: 9.2 × 1015 photons/cm2/s and 9.0 × 1015 photons/cm2/s, respectively.
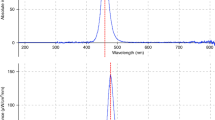
The serum concentrations of the bilirubin isomers were measured in capillary blood drawn by heel prick. They were analyzed at the initiation of phototherapy and after 24 h of treatment. The bilirubin isomers were identified and quantified using isocratic reverse-phase high-performance liquid chromatography according to Itoh et al.18 using a Dionex UltiMate 3000 system equipped with a Kinetex 2.6 µm C18, 150 ×4.6 mm column (Phenomenex). Separation of photoisomers was achieved using a gradient of primary buffer A and secondary buffer B: 0% B 5 min, 0–100% B 5–20 min, 100% B 4 min, and 0% B 7 min. The flow rate was 0.3 mL/min. Eluted isomers were measured at 455 nm. Coefficients of variation were: combined bilirubin isomers 2.4%, Z,Z-bilirubin 3.3%, Z,E-bilirubin 3.3%, E,Z-bilirubin 3.5%, and E,Z-lumirubin 5.1%. The concentrations of E,E-lumirubin were too low to be determined. An HPLC chromatogram demonstrating the separation of the individual bilirubin isomers is shown in Fig. 2 after 24 h of treatment.
Shown on the x-axis: are retention times (min.) and on the y-axis: are absorption units (mAU). WVL 455 nm: The wavelength at which the absorptions were measured. 1. E,E-lumirubin (not used in the article). 2. E,Z-lumirubin. 3. Z,E-bilirubin. 4. E,Z-bilirubin. 5. Z,Z-bilirubin. The retention times are shown behind the numbers.
Statistics
Categorical variables are summarized using counts and percentages, continuous variables are summarized using means and standard deviations or median and minimum, maximum. Clinical and demographic characteristics between the light groups were compared using Fisher’s exact test for categorical variables and median tests for continuous variables. Comparisons of bilirubin isomers were done using t-tests with unequal variances. All statistical analyses were done in Stata version 17. Tests with p-values below 0.05 were considered statistically significant.
Results
Demographic and clinical data are shown in Table 1. The two groups were comparable. The sex was the only statistically significant difference between the groups (p = 0.03).
The serum levels of the bilirubin isomers are shown in Table 2, both at initiation of the treatment and after 24 h of treatment. In both groups the serum absolute concentrations of Z,Z-bilirubin decreased, and the concentrations of the photoisomers Z,E-bilirubin, E,Z-bilirubin, and E,Z-lumirubin increased, all results being highly statistically significant (p < 0.001). The percentage decrease of combined bilirubin isomers was statistically significantly greater for the blue–green light group than for the blue light group, median of 47.8% vs 33.4%; the ratio between them being mean of 1.43, i.e., the efficacy of the blue–green light was 43% greater than of the blue light. Likewise, the statistically significant percentage decreases of Z,Z-bilirubin were 55.6% vs 44.2%; the ratio between them being 1.26, i.e., the decline of Z,Z-bilirubin was 26% greater for the blue–green light than of the blue light. The difference between the two groups in the decrease of the absolute concentrations of combined bilirubin isomers, as well as Z,Z-bilirubin was insignificant, while as mentioned the differences in the percentage decreases were highly significant. The increase in the absolute concentrations of Z,E-bilirubin, as well as combined bilirubin photoisomers were statistically significantly greater for the blue light group than for blue–green light group, while no difference was seen in the increase of the absolute concentrations of E,Z-bilirubin and E,Z-lumirubin. However, due to the low concentrations of these two bilirubin photoisomers, it is difficult to determine differences between the two groups.
After 24 h of phototherapy the median concentrations of the abundant photoisomer Z,E-bilirubin and thereby combined bilirubin photoisomers were significantly greater for the neonates exposed to blue light than blue–green light.
Discussion
The study showed that the therapeutic effect of the blue–green LED light with peak emission at 478 nm was 43% greater than the blue light with peak emission at 459 nm, as measured by the decrease of combined bilirubin isomers in serum, and 26% greater measured by the decrease of the toxic substance Z,Z-bilirubin, the irradiance of the exposed light being equal. The decrease of TSB found in the clinical part of this trial was 31% greater for the blue–green than for the blue light, measured by the diazo-method.9 The difference between the measured declines may be caused by the fact, that the bilirubin declines were determined by two different methods, and that the groups compared are not exactly the same in the two studies.
The reason why the blue–green light was more efficient may involve several factors: (1) the production of photoisomers in relation to the wavelength, (2) the excretion rate, (3) the competition of light absorption between bilirubin and hemoglobin, as well as melanin, which decreases with increasing wavelength, and (4) back scattering also decreases with increasing wavelength.11,12
Vreman et al.19 found that the production of lumirubin in vitro was greatest at 500 nm, when bilirubin was exposed to light with different wavelengths. This support that blue–green light is more efficient than standard blue light.
The variation in the quantum yield of bilirubin photoisomers during exposure of neonates to light with different wavelengths has been explained by the fact that the Z,Z-bilirubin molecule consists of two interacting light-absorbing di-pyrrol units. As was found in vitro, configurational isomerization is highly regioselective and wavelength-dependent.20,21,22 The selectivity decreases at a longer wavelength, which increases the proportion of E,Z-bilirubin, from which E,Z-lumirubin is derived, and declines the proportion of Z,E-bilirubin.20,21,22
Apparently, there was a discrepancy between the huge drop in TSB and the low serum concentrations of E,Z-bilirubin and E,Z-lumirubin. This discrepancy is caused by the rapid excretion of E,Z-lumirubin.23 The serum concentration of Z,E-bilirubin was about ten times higher due to its extremely slow excretion.24
Mreihil et al.25,26 showed that after 15 min of phototherapy with standard fluorescent blue light, Z,E-bilirubin reached up to 10% of combined bilirubin isomers, and 20–25% after equilibrium between Z,Z- and Z,E-bilirubin, which occurs after about two hours of treatment. This shows that the changes of the bilirubin isomers in plasma occur relatively quick, and that the action site for the photochemical processes occurs in the circulating blood in the superficial capillaries in the neonatal skin, beyond the extravascular space.27
The fact that the natural Z,Z-bilirubin is toxic has been known the decades. The bilirubin isomers appear to be less toxic than Z,Z-bilirubin: (1) when Z,E-bilirubin, E,Z-bilirubin and Z,E-lumirubin were incorporated in the growing media none of these bilirubin products exerted any toxic effect on cell viability28 and (2) lumirubin was found to induce fewer changes in mitochondrial respiration, substrate metabolism and reactive oxygen species than Z,Z-bilirubin.29
Lumirubin upregulated in vitro the pro-inflammatory genes that encode the interleukins TNFα, IL-1β, and IL-6 in rat hypocampal slices.30 That the lumirubin production increases with longer wavelengths means that (1) the upregulation of the production of TNFα, IL-1β, and IL-6 may be higher for the neonates exposed to blue–green light than for those exposed to blue light. This confirms that the plasma concentration of these interleukins was found to be increased during phototherapy using blue and white fluorescent light.31 The isomers may play crucial and multiple roles in CNS inclusive in neurodevelopment.30 (2) In vitro investigations on human neural stem cells showed that lumirubin affected cell morphology and expression of neural stem cells' specific proteins collectively indicating that lumirubin may affect early human development.32 As above neonates receiving blue–green light might be more affected.
Studies in the phototherapy of Gunn-rats suggested that the exclusion of low wavelength light in the spectral range 400–450 nm in favor of that of longer wavelengths in the spectral range 450–500 nm reduced photodynamic DNA damage.33,34 Thus, less photodynamic damage may occur using blue–green light than using blue light as neonates exposed to blue–green light receive less light in the spectral range 400–450 nm.
During phototherapy, the Z,Z bilirubin molecule also undergoes oxidation to several polar colorless products, mono-pyrrolic (BOX A and B), di-pyrrolic and three-pyrrolic substances. They contribute only little to the degradation of bilirubin during phototherapy.30 They did not affect cell viability and did not upregulate proinflammatory genes.30 These oxidation products were not determined in this study.
The bilirubin photoisomers seen before the initiation of phototherapy were probably the result of the neonates being exposed to ambient light, though minor light exposure during blood collection and procession cannot be excluded.
This study has some limitations. The differences in the decline of combined bilirubin isomers and Z,Z-bilirubin between blue–green light and blue light were only statistically significant for the percentage decrease, not for the absolute concentrations. This is explained by the fact that at the initiation of phototherapy, the difference in Z,Z-bilirubin concentration between the two groups was statistically significant, and that the decrease in the absolute concentration is dependent on the initial concentration. This is not the case for the percentage decrease. Therefore, also in our earlier trials and the clinical part of this trial, we used the percentage declines as a measure of the efficacy even though the initial TSB concentrations were not different.7,8 Another limitation was that 16 (16%) of the randomized neonates were not included in the study. However, because the drop-out was neither related to exposure nor outcome the risk of selection bias is very small.
The strengths of the study were that (1) the levels of light irradiance were adjusted to be equal through the use of a specialized spectrometer with equal sensitivity within the entire spectrum of the used light, (2) the study population was homogeneous, and (3) the neonates were healthy except for hyperbilirubinemia.
Conclusion
The decline in the absolute concentrations of combined bilirubin isomers and Z,Z-bilirubin itself in serum was essentially greater for hyperbilirubinemic neonates exposed to the recommended blue–green LED light with peak emission at 478 nm than standard blue LED light with peak emission at 459 nm. That is the pharmacological efficacy of the blue–green light was essentially greater for the neonates exposed to blue–green light. The increase in the absolute concentrations of Z,E-bilirubin and thereby combined bilirubin photoisomers were greatest for the blue light due to the extremely slow excretion of Z,E-bilirubin. Concerning biologic effects neonates receiving blue–green light may be more affected than those receiving blue light.
Data availability
The materials described in the manuscript, including all the raw data, will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
American Academy of Pediatrics, Kemper et al. Clinical practical guideline revision: management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 150, e2022058959 (2022).
Pichon, J.-B., Riordan, S. M., Watchko, J. & Shapiro, S. The neurological sequelae of hyperbilirubinemia: definitions, diagnosis and treatment of the kernicterus spectrum disorders (KSDs). Curr. Pediatr. Rev. 13, 199–209 (2017).
Alken, J., Haakansson, S., Ekeus, C., Gustafson, P. & Norman, M. Rates of extreme neonatal hyperbilirubinemia and kernicterus in children and adherence to national for screening, diagnosis, and treatment in Sweden. JAMA Netw. Open 2, e190858 (2019).
Toenne, A., Meberg, A. & Hager, H. B. Erindring i diagnostik og behandling av hyperbilirubinemi hos nyfødte. Tidskr. Nor. Legeforen 130, 18–24 (2010).
Hansen, T. W. R. et al. Sixty years of phototherapy for neonatal jaundice: from serendipitous observation to standardized treatment and rescue for millions. J. Perinatol. 40, 180–193 (2020).
Ebbesen, F., Madsen, P., Stoevring, S., Hundborg, H. & Agati, G. Therapeutic effect of turquoise versus blue light with equal irradiance in preterm infants with jaundice. Acta Paediatr. 96, 837–841 (2007).
Ebbesen, F. et al. Effect of phototherapy with turquoise vs. blue LED light of equal irradiance in jaundiced neonates. Pediatr. Res. 79, 308–312 (2016).
Ebbesen, F., Rodrigo-Domingo, M., Moeller, A. M., Vreman, H. J. & Donneborg, M. L. Effect of blue LED phototherapy centered at 478 nm versus 459 nm in hyperbilirubinemic neonates: a randomized study. Pediatr. Res. 89, 598–603 (2021).
Doumas, B. T. et al. Candidate reference method for determination of total bilirubin in serum: development and validation. Clin. Chem. 31, 1779–1789 (1985).
Ebbesen, F., Donneborg, M. L., Vandborg, P. K. & Vreman, H. J. Action spectrum of phototherapy in hyperbilirubinemic neonates. Pediatr. Res. 92, 816–821 (2022).
Lamola, A. A., Bhutani, V. K., Wong, R. J., Stevenson, D. K. & McDonagh, A. F. The effect of hematocrit on the efficacy of phototherapy for neonatal jaundice. Pediatr. Res. 74, 54–60 (2013).
Lamola, A. A. A pharmacologic view of phototherapy. Clin. Perinatol. 43, 259–276 (2016).
Ebbesen, F. et al. Bilirubin isomer distribution in jaundiced neonates during phototherapy with LED light centered at 497 nm (turquoise) vs. 459 nm (blue). Pediatr. Res. 80, 511–515 (2016).
McDonagh, A. F. Controversies in bilirubin biochemistry and their clinical relevance. Semin. Fetal Neonatal Med 15, 141–147 (2010).
Onishi, S. et al. Metabolism of bilirubin and its photoisomers in newborn infants During phototherapy. J. Biochem. 100, 789–795 (1986).
Vandborg, P. K. et al. Danish Paediatric Society. Behandlingsstandard for neonatal hyperbilirubinaemi. https://paediatri.dk/images/dokumenter/Retningslinjer_2019/Hyperbilirubin guideline.Juli_2019.pdf (Guideline in Danish).
Bradlid, D., Nakstad, B. & Hansen, T. W. National guidelines for treatment of jaundice in the newborn. Acta Paediatr. 100, 499–05 (2011).
Ito, S., Isobe, K. & Onishi, S. Accurate and sensitive high-performance liquid chromatographic method for geometric and structural photoisomers of bilirubin IXα using the relative molar absorptivity values. J. Chromatogr. A. 848, 169–177 (1999).
Vreman, H. J. et al. The effect of light wavelength on in vitro bilirubin photodegradation and photoisomer production. Pediatr. Res. 85, 865–873 (2019).
McDonagh, A. F., Agati, G., Fusi, F. & Pratesi, R. Quantum yields for laser photocyclization of bilirubin in the presence of human serum albumin. Dependence of quantum yield on excitation wavelength. Photochem. Photobiol. 50, 305–319 (1989).
Greenberg, J. W., Malhotra, V. & Ennever, J. F. Wavelength dependence of the quantum yield for the structural isomerization of bilirubin. Photochem. Photobiol. 46, 453–456 (1987).
Itoh, S., Onishi, S., Isobe, K., Manabe, M. & Yamakawa, T. Wavelength dependence of the geometric and structural photoisomerization of bilirubin bound to human serum albumin. Biol. Neonate 51, 7–10 (1987).
Okada, H. et al. Developmental changes in serum half-life of E,Z-cyclobilirubin. Early Hum. Dev. 81, 619–622 (2005).
Ennever, J. F., Knox, I., Denne, S. C. & Speck, W. T. Phototherapy for neonatal jaundice: in vivo clearance of bilirubin photoproducts. Pediatr. Res. 19, 205–208 (1985).
Mreihil, K., McDonagh, A. F., Nakstad, B. & Hansen, T. W. R. Early isomerization of bilirubin in phototherapy of neonatal jaundice. Pediatr. Res. 67, 656–659 (2010).
Mreihil, K. et al. Early formation of bilirubin isomers during phototherapy for neonatal jaundice: effects of single vs. double fluorescent lamps vs. photodiodes. Pediatr. Res. 78, 56–62 (2015).
Vogl, T. P. Phototherapy of neonatal hyperbilirubinemia: bilirubin in unexposed areas of the skin. J. Pediatr. 85, 707–710 (1974).
Jasprova, J. et al. The biologic effects of bilirubin photoisomers. PLoS One 11, e0148126 (2016).
Dvorak, A. et al. The effects of bilirubin and lumirubin on metabolic and oxidative stress markers. Front. Pharmacol. 12, 7001–7019 (2021).
Jasprova, J. et al. Neuro-inflammatory effects of photodegradative products of bilirubin. Sci. Rep. 8, 7444 (2018).
Kurt, A. et al. Use of phototherapy for neonatal hyperbilirubinemia affects cytokine production and lymphocyte subsets. Neonatology 95, 262–266 (2009).
Makova, N. et al. The effects of bilirubin and lumirubin on the differentiation of human pluripotent cell-derived neural stem cells. Antioxidants 10, 1532–1548 (2021).
Ushida, Y. et al. Phototherapy with blue and green mixed-light is as effective against unconjugated jaundice as blue light and reduces oxidative stress in the Gunn rat model. Early Hum. Dev. 97, 391–395 (2015).
van der Schoor, L. W. E. et al. LED-phototherapy does not induce oxidative DNA damage in hyperbilirubinemic Gunn rats. Pediatr. Res. 85, 1041–1047 (2019).
Acknowledgements
We thank physicians and nurses for their collaboration and enthusiasm for carrying out the study. We thank Hendrik J. Vreman and Thor Willy Ruud Hansen for an exhaustive and excellent review of the manuscript and for giving valuable advice for the improvement of the manuscript. Further, Hendrik J. Vreman is thanked for producing the phototherapy devices and performing the measurements of the light irradiance.
Funding
None of the authors have any financial support to disclose.
Author information
Authors and Affiliations
Contributions
F.E. conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. P.H.M. performed the biochemical analyses, and reviewed and revised the manuscript. M.R.-D. performed the statistical analyses, and reviewed and revised the manuscript. M.L.D. conceptualized and designed the study, collected the data, and reviewed and revised the manuscript. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Verbal and written informed consent was obtained from the parents. All regulations concerning research, at the time the studies were conducted, were followed. The trial was approved by the Committee for Biomedical Research Ethics in the North Denmark Region, N-20160071, and registered in the Clinical Trial Registry number NCT 03183986.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ebbesen, F., Madsen, P.H., Rodrigo-Domingo, M. et al. Bilirubin isomers during LED phototherapy of hyperbilirubinemic neonates, blue–green (~478 nm) vs blue. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03493-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03493-w
- Springer Nature America, Inc.