Abstract
Objective
To evaluate clinical outcomes associated with extubation timing among extremely preterm neonates.
Design/Methods
Neonates <26 weeks’ GA admitted to four tertiary neonatal centers were included if they met predetermined extubation criteria within first postnatal week and classified into early extubation (≤24 h; exposure group) and delayed extubation (>24 h; control group) after meeting extubation criteria. Patients with known severe IVH and/or significant PDA prior to meeting extubation criteria were excluded.
Results
Of 197 included infants, 75 were in exposure group. Survival without BPD (aOR 1.26; 95% CI 0.62–2.56; P = 0.52) and survival without severe IVH (aOR 1.98; 95% CI 0.93–4.23; P = 0.08) were not different, adjusted for GA, SNAP, number of surfactant doses and center.
Conclusions
Extubation within 24 h of meeting extubation criteria in neonates <26 weeks’ GA was not associated with survival without BPD or survival without severe IVH. However, confounding by indication cannot be ruled out without a prospective trial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Extremely preterm infants (<28 weeks’ gestational age (GA)) require some form of assisted ventilation to survive after birth, and approximately half to two-thirds of them require invasive mechanical ventilation (MV) on the first day of life [1]. As prolonged MV is injurious to developing lungs and brain [2], clinicians aim to extubate these infants early. Despite advances in respiratory care, extubation is often challenging and approximately half to two-thirds of ventilated infants do not tolerate extubation [3]. Infants who fail extubation are at higher risk of death, bronchopulmonary dysplasia (BPD) and intraventricular hemorrhage (IVH) [3].
As both prolonged MV [4] and failed extubation are associated with unfavorable outcomes [2, 3], it poses a clinical conundrum with respect to the optimal time for extubation. This is particularly germane to infants with GA <26 weeks who are particularly prone to both BPD and IVH and especially important during the first week after birth where the risk of IVH [5] is considerable, and patent ductus arteriosus (PDA) can be an issue [6]. Clinical practice in such situations vary markedly between care providers from extubating as soon as the infant is on low ventilator settings versus waiting for few days due to fear of failed extubation and associated complications. Previous cohort studies have favored early extubation in preterm infants despite higher chances of extubation failure, as need for re-intubation by itself was not shown to add to morbidity [4, 7,8,9]. The only randomized clinical trial showed no differences in outcomes (including no difference in the primary outcome of re-intubation) except reduction in ventilation days with delayed extubation (36 h after the extubation criteria were met) [10]. However, this study included preterm infants of GA 26 and 27 completed weeks, a patient group that clinicians may already feel more comfortable in extubating early.
It therefore remains unclear whether delaying extubation in extremely preterm infants with GA < 26 weeks, once the extubation criteria are met, confers any advantage or disadvantage as compared with earlier extubation. Hence, in this retrospective cohort study, we sought to comparatively evaluate clinical outcomes associated with early (within 24 h) versus delayed (>24 h) after meeting predefined clinical extubation criteria based on ventilator settings within the first week after birth in preterm neonates. We hypothesized that early elective extubation would increase the odds of survival without BPD but decrease the odds of survival without severe IVH.
Methods
Study design
This was a multicenter retrospective cohort study at four tertiary Canadian academic hospitals. Records of patients admitted to one of the participating centers between January 1, 2014 and June 30, 2017 were screened for eligibility. Data were gathered from individual patient chart review as well as from the Canadian Neonatal NetworkTM database. Institutional research ethics board approval was obtained at each participating site.
Inclusion criteria
This study included a population of extremely preterm neonates <26 weeks’ GA at birth admitted to one of the participating centers with the following conditions: (A) on invasive MV within the first 24 h after birth; (B) “extubatable” at some time point before 168 h of age (equivalent to 7 days); (C) no major congenital or suspected/confirmed genetic/chromosomal abnormality; (D) no (known) severe IVH (defined in Supplemental file 1) identified prior to meeting extubatable criteria; (E) no (known) significant PDA (defined in Supplemental file 1) on most recent echocardiogram (if conducted) prior to meeting “extubatable” criteria.
“Extubatable” status was defined when an infant met all of the following three criteria within first 168 h of postnatal age: (A) minimal ventilator settings for at least 2 continuous hours, defined as mean airway pressure ≤10 cmH2O and FiO2 <0.35 on high frequency ventilation (including jet and/or oscillatory ventilation); OR set or measured peak inspiratory pressure ≤18 cmH2O and positive end-expiratory pressure ≤6 cmH2O; and ventilator rate ≤30 bpm and FiO2 <0.35 on conventional ventilation (including volume targeted ventilation); (B) on caffeine (loading dose prior to 24 h age); and (C) most recent capillary or arterial blood gas with following parameters: pH > 7.2 and pCO2 < 60 mmHg (taken within 12 h prior to being on extubatable settings). These criteria were very similar to unit-level extubation guidelines for 2 of the centers (Supplemental file 2), whereas the other two centers did not have any local extubation guidelines.
The exposure group consisted of patients whose first extubation attempt was within 24 h of meeting extubatable criteria, whereas the control group comprised of patients whose first extubation attempt was greater than 24 h after meeting extubatable criteria OR those who were never extubated. The co-primary outcomes were survival without BPD and survival without severe IVH. Secondary outcomes were death, BPD, severe IVH, successful 1st extubation attempt (defined as lack of need for re-intubation within 72 h), significant PDA on echocardiogram within first 2 weeks after birth (assessed if present only after meeting extubatable criteria), and total days of supplemental oxygen. Definitions are included in Supplemental file 1.
Data analysis and statistical methods
Univariate analyses were performed to compare baseline and demographic data between the exposure and control groups. Means with standard deviation (normal data) or medians with interquartile ranges (skewed data) were used to report continuous variables and numbers and percentages for categorical variables. The independent t test (normal data) or Mann Whitney U test (skewed data) for continuous variables and the chi-square test (or Fisher’s exact test as appropriate) for categorical variables were used for analyses.
Univariate analyses were performed for the primary and secondary outcomes. In addition, unadjusted and adjusted odds ratios with 95% confidence intervals for primary outcomes were determined. A multilevel generalized estimating equation regression model was developed to account for clustering effect by center, along with the following confounding variables (based on results from univariate analyses): GA, SNAPII score > 20, number of surfactant doses >1 vs. ≤1 dose).
Statistical analytical software v9.4 (Cary, NC, USA) was used for all analyses. A two-sided p-value of <0.05 was considered to be statistically significant. No a priori sample size calculation was conducted due to the exploratory nature of the study. As many preterm neonates meet extubatable criteria within first few days of life when the discomfort and uncertainty among clinicians to extubate maybe highest, an a priori planned set of subgroup analyses were conducted for patients who met extubation criteria within 36 h of age using similar methods as described above.
Results
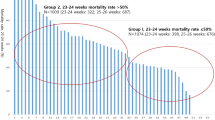
Out of 353 patients with GA <26 weeks admitted to the four participating centers in the study period, 197 met eligibility criteria—including meeting predefined extubation criteria within the first postnatal week. Of these, 75 (38.0%) patients were extubated within 24 h of meeting extubation criteria and constituted the exposure group (Fig. 1).
Baseline and demographic variables are shown in Table 1. The early extubation group had a higher GA and birth weight, lower incidence of SNAPII score >20, less use of high frequency ventilation at time of extubation, lower incidence of preextubation MAP >8 cmH2O and FiO2 >0.25, and less frequent use of >1 dose of surfactant. In addition, one of the centers had higher rate of early extubation than the other three (Table 1). No differences were noted in the remaining variables.
In univariate analyses of the primary outcomes and their individual components, no significant differences were noted between the two groups (Table 2). The exposure group had significantly higher incidence of successful extubation (lack of re-intubation within 72 h), lower incidence of treated PDA, and fewer total days on supplemental oxygen (Table 2). The primary outcomes of survival without BPD and survival without severe IVH were not significantly different after adjustment for potential covariates and confounders, as shown in Table 3. However, in a preplanned subgroup analysis of infants who met extubation criteria within first 36 h of age, both the unadjusted and adjusted odds of survival without severe IVH was higher in early extubation group (Table 3). Baseline demographic and patient characteristics of this subgroup are included in Supplemental file 3. In addition, a post-hoc analysis of the subgroup of infants who failed extubation was performed—focusing on primary outcomes and their components, and results were not markedly different than that of the entire cohort, as shown in Supplemental file 4. Finally, we conducted regression analyses for the primary outcomes in the full cohort as well as the aforementioned subgroup replacing GA with birth weight (Supplemental file 5) and it was noted that survival without severe IVH was statistically significantly higher in the early extubation group.
Discussion
In this multicenter retrospective cohort study of early versus delayed extubation in extremely preterm infants <26 weeks’ GA, we identified no differences in either composite outcome of survival without BPD or survival without severe IVH between neonates extubated early (within 24 h of meeting extubation criteria) compared with neonates extubated later (after 24 h of meeting extubation criteria). However, there was a trend toward increased survival without severe IVH in the early extubation group. Similarly, in a subgroup analysis of infants who met extubation criteria within first 36 h of age, there was higher odds of survival without severe IVH in the early extubation group.
The results from this study are contradictory to our hypothesis that early elective extubation would increase the odds of survival without BPD, whereas decrease the odds of survival without severe IVH. We found no differences in clinically important outcomes between early versus delayed extubation. However, infants in the delayed extubation group were sicker (lower GA, lower birth weight, higher SNAPII score, higher frequency of >1 dose surfactant) compared with infants in the early extubation group. This might have influenced clinicians’ decision to delay the extubation of these sick infants even though when they were ready from ventilation stand-point. Sick infants are at increased risk of mortality and severe IVH. Although, we have attempted to adjust for confounders, we cannot account completely for confounding by indication.
In our study, we defined explicitly that the infants would be included in the study if there is no known severe IVH identified prior to extubating criteria. It is however possible that few infants were identified to have severe IVH after meeting extubation criteria and were held off from extubation—even though, it is unclear whether this is the right approach—which may account for the higher number of severe IVH cases in the delayed extubation group, resulting in the aforementioned trend in survival without severe IVH that appears to favor early extubation. In addition, it is noteworthy that infants in the delayed extubation group were on higher ventilatory settings (pressures) compared with infants in the early extubation group just prior to extubation. One might speculate that this increased exposure to higher pressures and increased invasive ventilation duration [2] (due to delayed extubation) might have impeded the blood flow return from cerebral venous system to the thorax which could have resulted in increased cerebral venous pressure and intracranial bleeding [11]. The reason for increased ventilatory requirements in infants extubated late remains unclear. It could be partly due to higher initial illness severity or from lung injury occurring from delayed extubation [2, 3]. Given these aforementioned findings, and the fact that the early extubation group had no clinically worse outcomes, we posit that if a baby is clinically stable – early extubation may indeed be a feasible and acceptable choice.
Our study adds to previous data indicating a relationship between delayed extubation and adverse neonatal outcomes [2, 3, 7, 8, 10]. The results of our study are similar to the randomized clinical trial that evaluated early (immediate after meeting extubation criteria) versus late extubation (after 36 h of meeting extubation criteria) [10]. This trial showed no differences in survival without BPD between early (77%) and delayed extubation (79%) [10]. The authors also reported nonstatistically significant increased risk of severe IVH in the delayed extubation group (14.2%) compared with the early extubation group (4.5%) [10]. In comparison to this trial [10], our study found much lower rates of survival without BPD (22.7% early extubation and 18.9% in delayed extubation). The likely explanation is that the cohort enrolled in our study (mean GA ~24 weeks) was more immature compared with the cohort enrolled in the clinical trial [10] (mean GA ~26 weeks).
The following are the important strengths of our study. Firstly, it highlights the importance of early extubation in extremely preterm infants <26 weeks GA and addresses the important knowledge gap. Secondly, the study utilizes the explicit criteria to define the study question. Thirdly, the study design included in-depth data abstraction of ventilation parameters. Lastly, the study was multicentered which enhance the generalizability of the study findings. However, certain limitations must be acknowledged. The main limitation of the study is confounding by the indication. Sicker infants are at risk of death and severe IVH [1]. These infants are also likely to fall into the delayed extubation category, while the infants who were clinically more stable more likely to be extubated earlier. This issue is further compounded by the fact that the decision to extubate was neither protocol-driven, nor based on the criteria we devised as part of this study. It is impossible to completely account for this confounding, even though we attempted to adjust for surrogate markers of illness in the adjusted analyses. Another limitation is that our study design was not devised to evaluate the timing of IVH, and as such we speculate that many of cases of severe IVH may have occurred prior to actual extubation in the delayed extubation group. However, our study was designed to start at the moment a patient met extubation criteria, and all outcomes following this moment were captured between the two groups. Finally, the relative contributions of severe IVH as a result of peri-extubation instability versus simply as a result of staying on the ventilator for a longer duration remain unclear. In addition, the extubation criteria that we defined are consensus based and somewhat arbitrary, but may not be universally applied; it is acknowledged that at some centers an FiO2 cut-off of 0.35 maybe rather generous. Another limitation is the lack of clinical contraindications for extubation such as surgery on the same day, pulmonary hemorrhage, hypotension, and clinical sepsis as examples. However, it was felt that documentation of such clinical contraindications may not be always reliable, but would be important to assess for in the prospective study. Lastly, the study was underpowered as evident by the wide confidence intervals for the primary outcomes.
In conclusion, our study did not identify differences in survival without BPD or survival without severe IVH between early and delayed extubation groups. A trend toward increased odds of surviving without severe IVH was noted with early extubation. However, confounding by indication cannot be ruled out without a randomized clinical trial. Overall, the study suggests that early extubation is not inferior and maybe the approach of choice in situations where this is suitable based on clinical discretion. Further, a multicentered comparative effectiveness research study should be planned in future to enhance the quality of evidence [4].
References
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Walsh MC, Morris BH, Wrage LA, Vohr BR, Poole WK, Tyson JE, et al. Extremely low birthweight neonates with protracted ventilation: mortality and 18-month neurodevelopmental outcomes. J Pediatr. 2005;146:798–804.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatr. 2017;189:113–9.
Berger J, Mehta P, Bucholz E, Dziura J, Bhandari V. Impact of early extubation and reintubation on the incidence of bronchopulmonary dysplasia in neonates. Am J Perinatol. 2014;31:1063–72.
Perlman JM, Volpe JJ. Intraventricular hemorrhage in extremely small premature infants. Am J Dis Child. 1986;140:1122–4.
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007;92:F424–7.
Robbins M, Trittmann J, Martin E, Reber KM, Nelin L, Shepherd E. Early extubation attempts reduce length of stay in extremely preterm infants even if re-intubation is necessary. J Neonatal Perinat Med. 2015;8:91–7.
Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7.
Dumpa V, Northrup V, Bhandari V. Type and timing of ventilation in the first postnatal week is associated with bronchopulmonary dysplasia/death. Am J Perinatol. 2011;28:321–30.
Danan C, Durrmeyer X, Brochard L, Decobert F, Benani M, Dassieu G. A randomized trial of delayed extubation for the reduction of reintubation in extremely preterm infants. Pediatr Pulmonol. 2008;43:117–24.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8.
Funding
None specific to this study. Dr Amit Mukerji is supported by a Research Early Career Award from Hamilton Health Sciences Foundation (2019–2021). Dr Prakesh Shah is supported by an Applied Research Chair funding from the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mukerji, A., Razak, A., Aggarwal, A. et al. Early versus delayed extubation in extremely preterm neonates: a retrospective cohort study. J Perinatol 40, 118–123 (2020). https://doi.org/10.1038/s41372-019-0495-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0495-6
- Springer Nature America, Inc.
This article is cited by
-
Risk factors for delayed extubation after pediatric perineal anaplasty in patients less than 1 year of age: a retrospective study
BMC Pediatrics (2024)
-
Peri-extubation settings in preterm neonates: a systematic review and meta-analysis
Journal of Perinatology (2024)
-
Weaning and extubation from neonatal mechanical ventilation: an evidenced-based review
BMC Pulmonary Medicine (2022)