Abstract
Background
Previous studies have modeled the association between fetal exposure to tobacco smoke and body mass index (BMI) growth trajectories, but not the timing of catch-up growth. Research on fetal exposure to maternal secondhand smoking is limited.
Objectives
To explore the associations between fetal exposure to maternal active and secondhand smoking with body composition at birth and BMI growth trajectories through age 3 years.
Methods
We followed 630 mother-child pairs enrolled in the Healthy Start cohort through age 3 years. Maternal urinary cotinine was measured at ~ 27 weeks gestation. Neonatal body composition was measured using air displacement plethysmography. Child weight and length/height were abstracted from medical records. Linear regression models examined the association between cotinine categories (no exposure, secondhand smoke, active smoking) with weight, fat mass, fat-free mass, and percent fat mass at birth. A mixed-effects regression model estimated the association between cotinine categories and BMI.
Results
Compared to unexposed offspring, birth weight was significantly lower among offspring born to active smokers (−343-g; 95% CI: −473, −213), but not among offspring of women exposed to secondhand smoke (−47-g; 95% CI: −130, 36). There was no significant difference in the rate of BMI growth over time between offspring of active and secondhand smokers (p = 0.58). Therefore, our final model included a single growth rate parameter for the combined exposure groups of active and secondhand smokers. The rate of BMI growth for the combined exposed group was significantly more rapid (0.27 kg/m2 per year; 95% CI: 0.05, 0.69; p < 0.01) than the unexposed.
Conclusions
Offspring prenatally exposed to maternal active or secondhand smoking experience rapid and similar BMI growth in the first three years of life. Given the long-term consequences of rapid weight gain in early childhood, it is important to encourage pregnant women to quit smoking and limit their exposure to secondhand smoke.
Similar content being viewed by others
Introduction
The impact of maternal active smoking during pregnancy on birth weight has been established for nearly four decades [1, 2]. A growing body of evidence, including from our own cohort, further demonstrates that fetal exposure to maternal active smoking is associated with decreased neonatal fat mass [3,4,5,6,7]. Growth-restricted fetuses often grow faster than normal in early childhood to eliminate the growth deficit, a phenomenon known as catch-up growth [8]. Studies have modeled the longitudinal associations between fetal exposure to tobacco smoke and body mass index (BMI) growth trajectories [9,10,11,12,13,14], but the timing of postnatal catch-up growth remains unknown.
Research on the impact of fetal exposure to maternal secondhand smoking is limited. Only one published study has examined the association between fetal exposure to maternal secondhand smoking and BMI growth trajectories in early childhood [9]. The potential association between fetal exposure to maternal secondhand smoking and neonatal fat mass has yet to be explored.
Most of the published studies have relied on self-report to characterize fetal exposure to maternal smoking. Self-reports of active and secondhand smoking tend to be under-reported [15], particularly among pregnant women [9]. The resulting measurement error may lead to an underestimation of the true association with offspring growth. Characterizing exposure with cotinine, the major metabolite of nicotine [16], may provide a more accurate representation of these associations.
Nearly half of all children are exposed to prenatal smoking (where the mother was an active smoker or was exposed to secondhand smoke during pregnancy) [9], but the long-term consequences related to this exposure are not fully understood. Therefore, we explored the associations between fetal exposure to maternal active and secondhand smoking with body composition at birth and BMI growth trajectories through age 3 years. Our analysis was conducted among mother-child pairs enrolled in the Healthy Start, a longitudinal pre-birth cohort in Colorado. Maternal urinary cotinine collected during pregnancy was used to classify women and their offspring as having no exposure, maternal exposure to secondhand smoke, and maternal active smoking.
Methods
Study population
The Healthy Start study recruited 1410 pregnant women aged ≥ 16 years with singleton pregnancies before 24 weeks of gestation from the obstetrics clinics at the University of Colorado Hospital between 2010 and 2014. Participants completed two research visits in pregnancy (median 17 and 27 weeks of gestation), and at delivery (median 1-day post-delivery). Women were excluded if they were expecting multiple births, had a previous stillbirth or pre-term birth before 25 weeks gestation; had pre-existing diabetes, asthma, cancer, or psychiatric illness; were younger than 16 years of age; or had already completed the 24 weeks gestation. Mother-child pairs were eligible for the body composition analysis if they had complete body composition measures at birth and had cotinine measured in stored maternal urine samples. Mother-child pairs were eligible for the childhood BMI analysis if they had reached the age of 3 years by October 2017 and had ≥ 3 weight and length/height measurements from pediatric visits. The Healthy Start study protocol was approved by the Colorado Multiple Institutional Review Board. All women provided written informed consent before the first study visit. The Healthy Start study was registered as an observational study at clinicaltrials.gov as NCT02273297.
Maternal urinary cotinine and self-report
Cotinine was measured in a subsample of women with stored urine samples collected at ~ 27 weeks gestation. Cotinine was measured via solid phase competitive ELISA, with a sensitivity of 1 ng/mL (Calbiotech Cotinine ELISA CO096D). The limit of detection (LOD) was 0.05 ng/mL. The cotinine categories were defined as follows: no exposure (< LOD), exposure to secondhand smoke (≥ LOD to 550 ng/mL; the established cutpoint for active smoking [17]), and active smoking (≥ 550 ng/mL).
Self-report of active smoking and exposure to secondhand smoke prenatal smoking was ascertained through questionnaires completed at ~ 27 weeks gestation. Self-report of exposure was defined as follows: no exposure (if they reported not currently smoking and no secondhand smoke exposure), exposure to secondhand smoke (if they reported not currently smoking and > 1 h/week exposure to secondhand smoke), and active smoking (if they reported current smoking).
Neonatal body composition
Fat mass and fat-free mass were measured within ~ 72 h of delivery by trained study staff using whole body air displacement plethysmography (PEA POD, COSMED, Rome, Italy). The PEA POD system measures body mass and volume, calculates body density, and estimates fat mass (g) and fat-free mass (g). Fat mass and fat-free mass were measured twice. If the percent fat mass differed by more than 2.0%, a third measurement was taken. The average of the two closest readings was used in this analysis. Percent fat mass was calculated as fat mass divided by the sum of fat mass and fat-free mass. Birth weight was obtained from obstetric records.
Child BMI
We abstracted weight, recumbent length (generally until 24 months), and standing height (generally after 24 months) from medical records at pediatric visits. These measurements were generally recorded at well-child visits, which occur at 1, 2, 4, 6, 12, 18, 24, 30, and 36 months. BMI was calculated by dividing weight in kilograms by height in meters squared.
Covariates
Mother and child characteristics were collected during the research visits and through medical records. Maternal age at delivery was calculated by subtracting the participant’s date of birth from the date of delivery. Gravidity (number of pregnancies), maternal race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), maternal education (< high school, high school diploma, some college), and annual household income (<$40,000, $40,001 to $70,000,>$70,000, missing or do not know) were self-reported via study questionnaires. Maternal height was measured using a stadiometer during the first pregnancy research visit. Pre-pregnancy weight was obtained from medical records (91%) or self-reported at the first pregnancy research visit (9%). Pre-pregnancy BMI was calculated as pre-pregnancy weight (kg) divided by height squared (m2). Gestational weight gain was calculated as the difference between the last available weight measurement during pregnancy (measured by research staff or medical personnel) and pre-pregnancy weight. The mean gestational age at the last available weight measurement was 38.2 weeks. Approximately 94% of participants had last available weight measures recorded at or after 34 completed weeks of gestation.
Maternal diet was measured throughout pregnancy using the Automated Self-Administered 24-hour Dietary Recall (ASA24), an online platform developed and hosted by the National Cancer Institute (ASA24-Beta and ASA24-2011, Bethesda, Maryland). Maternal diet quality was determined by the Healthy Eating Index-2010 (HEI-2010). The HEI-2010 is a valid and reliable measure of diet quality [18]. Previous work in this cohort demonstrated that maternal HEI-2010 scores are associated with neonatal body composition [19]. We calculated HEI-2010 scores as previously described [19]. Briefly, HEI-2010 scores were based on the following foods/nutrients obtained from the repeated dietary recalls [20]: total fruit, whole fruit, total vegetables, greens, and beans, whole grains, dairy, total protein foods, seafood, and plant proteins, fatty acids, refined grains, sodium, empty calories, total energy, saturated fat, mono- and polyunsaturated fats, and sodium.
During a phone interview at age 5 months, mothers were asked to report the number of adults in the household who were regular smokers. Responses to this question ranged from zero to six. Due to the low number of responses in some of these categories, we dichotomized this data into no household smokers and any household smokers.
Infant diet was assessed through the duration of exclusive breastfeeding and the age at the introduction of solid foods through a questionnaire administered at age 5 months. The duration of exclusive breastfeeding variable has been previously described [21]. Briefly, women were asked in separate questions if they were currently feeding their infant any breast milk, had ever fed their infant formula, or were currently feeding their infant formula. The breastfeeding exclusivity variable was dichotomized as exclusively breastfed through age 5 months (if they answered yes to the first question and no to the remaining questions) and not exclusively breastfed (if they indicated mixed or formula feeding). Mothers reported the age in which they first introduced their child to various foods, such as rice cereal and pureed fruits/vegetables. National guidelines advise that the introduction of solid foods be delayed until age 4 months [22]. Therefore, we dichotomized mothers who reported introducing solid foods before age 4 months and mothers who reported introducing solid foods at or after age 4 months.
Statistical analysis
A kappa statistic was generated to explore the concordance between the categories of exposure as determined by maternal urinary cotinine and self-report.
Separate univariate linear regression analyses were used to estimate the association between the cotinine categories (no exposure, secondhand smoke, and active smoking) and weight (g), fat mass (g), fat-free mass (g), and percent fat mass at birth. Covariates were chosen based on the literature [6, 9] and included the following: maternal age (years), gestational weight gain (kg), pre-pregnancy BMI (kg/m2), maternal race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), maternal education (<high school, high school diploma, some college), household income (<$40,000, $40,001 to $70,000, >$70,000, missing or do not know), offspring sex, and gestational age at birth (weeks). Our final models present adjusted beta coefficients and means with corresponding 95% confidence intervals (CIs).
A mixed-effects regression model was used to examine the longitudinal association between the cotinine categories and BMI levels through age 3 years. Mixed-effects models account for the within-participant correlation between repeated measurements of outcomes [23]. Additionally, mixed-effects models allow for missing and mistimed outcome measures, under the assumption that the outcomes were missing at random [24]. Based on the deviance information criteria [25], the best-fit trajectory for the age variable was a square root transformation. Assumptions of linearity and homoscedasticity were verified via examination of the jackknifed-studentized residuals. The model allowed for a difference in BMI trajectories over time between the cotinine groups. We used Wald tests with Kenward-Roger degrees of freedom and an alpha level of 0.05 to assess the significance of the association between the cotinine categories and BMI over time [26]. Our minimally-adjusted model was determined by including all covariates listed above and removing non-significant covariates to arrive at the best-fitting model. The minimal set of covariates included race/ethnicity, offspring sex, and gestational age. In addition to the minimal set of covariates, our fully-adjusted mixed-effects regression model included maternal education (<high school, high school diploma, some college), household income (<$40,000, $40,001 to $70,000, > $70,000, missing or do not know), maternal diet quality during pregnancy (HEI-2010), number of household smokers at ~ 5 months of age (none, any), duration of exclusive breastfeeding (<5 months, ≥5 months), and the age of introduction of solid foods (<4 months, ≥4 months). We report the predicted mean BMI level and BMI growth velocity at various ages (1 month, 6 months, 12 months, etc.). We computed BMI growth velocity by taking the derivative of the estimated regression equation for the BMI trajectory. We computed estimates of the standard error of the velocity by calculating the variance of the velocity equation, and using the model produced beta coefficients, standard errors of the coefficients and the correlation between the coefficients. We used the estimated velocity standard errors and the critical value for the corresponding t reference distributions to calculate the half-widths of the confidence intervals. We tested for an interaction with sex by introducing a product term into the model.
All statistical analyses except for the mixed-effect regression model were conducted using Stata, Version 14.2 (StataCorp LP, College Station, TX). The mixed-effect regression model was conducted using SAS 9.4 (SAS, Cary, NC).
Sensitivity analysis
The optimal cutoff value of urinary cotinine for distinguishing individuals exposed to secondhand smoke ranges from 31.5 to 550 ng/mL [17, 27, 28]. As a sensitivity analysis, we used the lowest cutoff value (31.5 ng/mL [28]) to explore the potential impact of exposure misclassification. The cotinine categories were defined as follows: no exposure (<LOD), exposure to secondhand smoke (≥LOD to 31.5 ng/mL), and active smoking (≥31.5 ng/mL). A second kappa statistic was generated to explore the concordance between the self-reported exposures and the cotinine categories with the lower cutoff value used in the sensitivity analysis. We explored the association between these cotinine categories with the neonatal outcomes and with childhood BMI growth through 3 years of age.
Results
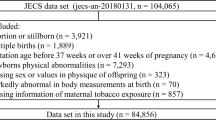
Of the 1410 participants enrolled in the Healthy Start cohort study, 721 had cotinine measured in stored urine samples from mid-pregnancy (Supplemental Figure S1). Of these, 91 mother-child pairs were missing complete body composition measures at birth and 8 were missing information about gestational weight gain. Therefore, the final sample size for the body composition analyses was 622 mother-child pairs. For the analyses of BMI growth trajectories, we further excluded 113 mother-child pairs who did not have at least three length/height and weight measurements abstracted from medical records as of October 2017. The final sample size for the childhood BMI analyses was 509 mother-child pairs. For our fully-adjusted mixed-effects model, the sample size was 434, due to missing information about postnatal exposure to secondhand smoke and the duration of exclusive breastfeeding. There were no substantial differences in maternal or child characteristics between the entire cohort, the body composition analytic sample, and the childhood BMI analytic sample (Supplemental Table S1).
Maternal and child characteristics are presented in Table 1. Based on maternal urinary cotinine, a majority of the women were classified as having no exposure (n = 468, 74%). A total of 127 women (20%) were classified as having been exposed to secondhand smoke and 35 women (6%) were classified as active smokers. Active smokers reported more pregnancies than those with no exposure or exposure to secondhand smoke (p < 0.01). Women exposed to secondhand smoke were younger than active smokers or women with no exposure (p < 0.01). Non-exposed women were more likely to be non-Hispanic white (p < 0.01), to have an annual household income above $70,000 (p < 0.01), to have attended college (p < 0.01), to have had a higher HEI-2010 score during pregnancy (p < 0.01), to have delayed the introduction of solid foods until 4 months of age (p < 0.01), and to have breastfed exclusively until age 5 months (p < 0.01). Offspring born to active smokers were significantly more likely to live with a household smoker at age 5 months(p < 0.01). There were no differences in gestational weight gain (p = 0.97), pre-pregnancy BMI (p = 0.11), offspring sex (p = 0.50), or gestational age at birth (p = 0.32) across the cotinine categories.
Maternal urinary cotinine and self-report
A majority of the women (97%) with a cotinine level indicating no exposure also self-reported no exposure (Table 2). Among women with a cotinine level indicating exposure to secondhand smoke, 70% reported no exposure, 25% reported exposure to secondhand smoke, and 5% reported active smoking. Among women with a cotinine level indicating active smoking, 71% also reported active smoking. Self-report was moderately concordant with maternal urinary cotinine (kappa = 0.44; p < 0.01).
Maternal urinary cotinine and neonatal body composition
Neonates born to active smokers had a statistically significant reduction in weight (−343-g; 95% CI: −473, −213), fat mass (−80-g; 95% CI: −132, −29), fat-free mass (−255-g; 95% CI: −357, −154), and percent fat mass (−1.6%; 95% CI: −3.0, −0.3) at birth, as compared to neonates with no exposure (Table 3). Maternal exposure to secondhand smoke was associated with smaller size at birth, but the associations were not statistically significant (Table 3).
Maternal urinary cotinine and childhood BMI
Fig. 1 presents the growth trajectories according to the cotinine categories and model-based estimated mean BMI levels at various ages. There was no significant difference in the rate of growth of BMI over time between offspring of secondhand smoker and active smokers (p = 0.58). The final model had a single growth rate parameter for the combined exposure groups of active and secondhand smoking. The rate of growth in BMI for the combined exposed group was significantly more rapid (0.27 kg/m2 per year; 95% CI: 0.05, 0.69; p < 0.01) than the unexposed group. By age 12 months, the predicted BMI levels among offspring born to active smokers had caught up to BMI levels among unexposed offspring (mean difference: 0.0 kg/m2). By age 36 months, the predicted BMI levels were 0.9 kg/m2 higher among offspring born to women exposed to secondhand smoke and 0.4 kg/m2 higher among offspring born to active smokers, as compared to unexposed offspring. The BMI growth velocity was consistently higher among offspring born to active smokers or mothers exposed to secondhand smoke, as compared to offspring with no exposure (Table 4). After further adjusting for maternal education, household income, maternal diet quality during pregnancy, postnatal exposure to secondhand smoke, the duration of exclusive breastfeeding, and the age of introduction of solid foods, the rate of growth in BMI for the combined exposed group was not substantially changed (Fig. 2; 0.17 kg/m2 per year; 95% CI: 0.01, 0.68; p < 0.05). There was no evidence of an interaction with sex (results not presented).
BMI growth trajectories according to maternal urinary cotinine categories. The cotinine categories were defined as follows: no exposure (<0.05 ng/ml [LOD]), exposure to secondhand smoke (≥LOD & <550 ng/mL) and active smoker (≥550 ng/mL). The predicted BMI levels are for participants of the following reference groups: non-Hispanic white race/ethnicity, male sex, and 40 weeks gestation. The rate of growth in BMI for the combined exposed groups (secondhand and active smoking) was significantly more rapid (0.27 kg/m2 per year; 95% CI: 0.05, 0.69; p < 0.01) than the unexposed group
BMI growth trajectories according to maternal urinary cotinine categories. The cotinine categories were defined as follows: no exposure ( < 0.05 ng/mL [LOD]), exposure to secondhand smoke ( ≥ LOD & < 550 ng/mL) and active smoker ( ≥ 550 ng/mL). The predicted BMI levels are for participants of the following reference groups: non-Hispanic white race/ethnicity, male sex, 40 weeks gestation, the average maternal HEI-2010 score of 56.3, not living with any household smokers at 5 months of age, exclusively breastfed until at least 5 months of age, and no solid foods prior to 4 months of age. The rate of growth in BMI for the combined exposed groups (secondhand and active smoking) was significantly more rapid (0.17 kg/m2 per year; 95% CI: 0.01, 0.68; p < 0.05) than the unexposed group
Sensitivity analyses
Self-report was moderately concordant with the cotinine categories with the lower cutoff value of 31.5 ng/mL (kappa = 0.41; p < 0.01). Among women with a cotinine level indicating exposure to secondhand smoke, 76% reported no exposure, 23% reported exposure to secondhand smoke, and 1% reported active smoking (Supplemental Table S2). Among women with a cotinine level indicating active smoking, 71% also reported active smoking. The associations between cotinine categories with body composition measures at birth (Supplemental Table S3) and with the BMI growth trajectories (Supplemental Figure S2) were not changed when we used the lower cutoff value.
Discussion
Only a few studies have examined the association between fetal exposure to maternal active or secondhand smoking and offspring early-life growth. Our results suggest that fetal exposure to maternal active smoking is associated with lower weight, fat mass, fat-free mass, and adiposity at birth. Although the effect estimates were in the expected direction, fetal exposure to secondhand smoke was not significantly associated with neonatal body composition. We provide novel evidence that offspring prenatally exposed to maternal active or secondhand smoking experience rapid and similar postnatal BMI growth, already apparent within the first 12 months of life.
Our results expand upon previous work in this cohort. Harrod and colleagues [6] reported offspring born to mothers who self-reported smoking at any point during pregnancy had a lower fat mass (−68-g; 95% CI: −118, −19) and a lower fat-free mass (−114-g; 95% CI: −210, −18) at birth as compared to unexposed offspring. These associations were stronger among pregnant women who smoked throughout the entire pregnancy, as compared to those who smoked only in early to mid-pregnancy [7]. Harrod and colleagues [7] also reported a dose-dependent relationship, where neonatal fat mass and fat-free mass were significantly reduced with each additional pack smoked. Using cotinine to determine exposure, findings from the present study suggest that the impact of maternal active smoking during pregnancy on lower fat mass and fat-free mass may be greater than what was previously reported in this cohort [6, 7]. This observation is likely due to under-reporting of active smoking during pregnancy.
Previous studies have reported that fetal exposure to maternal secondhand smoking is associated with lower weight at birth. A recent meta-analysis of 44 studies representing 71,663 women reported a weighted mean difference of −60-g (95% CI: −80, −39) among neonates prenatally exposed to maternal secondhand smoking, as compared to those with no exposure [29]. However, consistent with our study, 22 of the 44 studies cited in the meta-analysis reported associations that were in the expected direction but with 95% CIs that included the null. Many factors could explain the discrepancies across studies, including uncontrolled or residual confounding due to factors such as maternal age, maternal diet, or socioeconomic status [29], temporal variations in exposure to secondhand smoke [9], or heterogeneity across study populations [30].
Consistent associations between fetal exposure to maternal active smoking and increased BMI growth in early childhood have been reported in the literature [9,10,11,12,13,14]. To date, only one published study has examined the association between fetal exposure to maternal active and secondhand smoking during pregnancy and BMI growth trajectories in early childhood [9]. Braun et al. [9] reported that the predicted BMI level at age 3 years was 1.0 kg/m2 (95% CI: 0.3, 1.8) higher among offspring born to active smokers and 0.4 kg/m2 (95% CI: 0.0, 0.8) higher among offspring born to women exposed to secondhand smoke, as compared to unexposed offspring. In this cohort, we observed that the BMI growth velocity for offspring born to women exposed to secondhand smoke did not differ from that of offspring born to active smokers. However, since offspring born to active smokers were significantly smaller at birth, the predicted BMI level at age 3 years was lower as compared to the predicted BMI level among those born to women exposed to secondhand smoke. These findings suggest that it is equally important to encourage pregnant women to quit smoking and limit their exposure to secondhand smoke.
Our study provides novel evidence about the timing of postnatal catch-up growth. Rapid weight gain in infancy is a compensatory mechanism that follows intrauterine growth restraint. Although compensatory catch-up growth is expected [8], postnatal weight gain can sometimes overcompensate for the initial growth deficit. Excessive and/or rapid weight gain in early childhood is problematic because it is a known risk factor for adulthood obesity [31] and chronic disease [32]. In our study, we observed that offspring exposed to maternal active or secondhand smoking begin to experience BMI growth velocity which exceeds the growth velocity for unexposed offspring within the first 12 months of age. Our identification of this critical window in which growth-restricted fetuses experience excessive or rapid catch-up growth may help to identify strategies for prevention. Potential strategies for stabilizing excessive growth in the first year of life include nutritional interventions, such extending the duration of exclusive breastfeeding or incorporating dietary omega-3 polyunsaturated fatty acids into the child’s diet [33]. Moreover, some of these early-life nutritional factors have also been shown to reduce susceptibility to the obesogenic effects of postnatal exposures to tobacco smoke [21, 34]. Future research should focus on potential nutritional strategies that may promote “healthy” growth velocity [35].
Several mechanisms linking fetal exposure to maternal smoking and reduced offspring size at birth have been discussed in the literature, including blood flow restriction to the placenta due to nicotine-induced vasoconstriction [36], intrauterine growth restriction as a result of fetal hypoxia [37], and changes in the gene expression of peroxisome proliferator–activated receptor gamma (PPAR-γ, the key transcription factor triggering adipocyte differentiation) [38] or other epigenetic changes [39, 40]. Additional mechanisms may underlie the association with offspring BMI in early childhood, such as over-compensatory catch-up growth [8].
As expected, we observed some disagreement between self-reported and cotinine-confirmed exposure. Self-report and cotinine tend to disagree among pregnant women [41], particularly for self-reports of secondhand smoke exposures [9]. Braun and colleagues [9] reported that 84% of pregnant women classified as active smokers by serum cotinine reported active smoking and 23% of pregnant women classified as having exposure to secondhand smoke by serum cotinine also reported this exposure. In this cohort, 71% of pregnant women classified as active smokers by urinary cotinine reported active smoking and 25% of pregnant women classified as having exposure to secondhand smoke also reported this exposure. Several factors could explain the disagreement between self-reported and cotinine-confirmed exposure. First, active smokers who identified themselves as non-smokers may be trying to quit smoking and have continued to smoke cigarettes occasionally or at lower levels [41]. Additionally, women may have inaccurately reported secondhand smoke exposures, particularly if these exposures were intermittent (e.g. only occurred on weekends) [9]. Finally, because the half-life of cotinine is relatively short (~ 18 h), the ability of cotinine to distinguish exposure to secondhand smoke from active smoking requires that the biomarker be measured in close temporal proximity to the exposure [28]. Lower cutoff values of cotinine have been proposed as a way to minimize the potential for exposure misclassification [27, 28, 42]. We explored this issue by using a lower cutoff value. However, the extent of the disagreement was not improved after redefining the cotinine categories using the lower cutoff value.
Several limitations should be considered when interpreting these results. We relied on a one-time measure of cotinine to estimate exposure. Cotinine is an established biomarker of nicotine exposure that is considered a more objective indicator of exposure to secondhand smoke or active smoking than self-report [16]. However, even this biomarker may have been insufficient to accurately classify exposure throughout a woman’s entire pregnancy. Additionally, not all of the children initially enrolled in the study had complete child height/weight measurements and only a subsample had cotinine measures. However, the mother-child pairs included in this report were similar to the entire cohort with respect to household income, race/ethnicity, and other socio-demographic factors.
An important strength of this study is the longitudinal assessment of growth among offspring prenatally exposed to maternal active and secondhand smoking with childhood BMI growth trajectories. Our findings provide evidence about the critical periods during which postnatal growth in exposed offspring either begins to overcompensate for the initial intrauterine growth deficit or is higher than normal, either of which may have important public health implications. Additionally, we used a direct measure of neonatal body composition, as done in previous publications within this cohort [6, 7].
Conclusions
Despite the steady decline in smoking rates since 2000 [43], the prevalence of prenatal exposure to tobacco smoke remains relatively high. In this cohort, we observed that prenatal exposure to maternal active smoking is associated with systematic growth restriction of the fetus. Furthermore, our data provide novel evidence that offspring prenatally exposed to maternal active or secondhand smoking experience rapid growth in the first three years of life. Given the serious and long-term health consequences of rapid weight gain in early childhood [31, 32], it is important to encourage pregnant women to quit smoking and limit their exposure to secondhand smoke.
References
Butler NR, Goldstein H, Ross EM. Cigarette smoking in pregnancy: its influence on birth weight and perinatal mortality. BMJ. 1972;2:127–30.
von Kries R, Bolte G, Baghi L, Toschke AM. Group GMES. parental smoking and childhood obesity--is maternal smoking in pregnancy the critical exposure? Int J Epidemiol. 2008;37:210–6.
Lindsay CA, Thomas AJ, Catalano PM. The effect of smoking tobacco on neonatal body composition. Am J Obstet Gynecol. 1997;177:1124–8.
Zaren B, Lindmark G, Gebre-Medhin M. Maternal smoking and body composition of the newborn. Acta Paediatr. 1996;85:213–9.
Cliver SP, Goldenberg RL, Cutter GR, Hoffman HJ, Davis RO, Nelson KG. The effect of cigarette smoking on neonatal anthropometric measurements. Obstet Gynecol. 1995;85:625–30.
Harrod CS, Fingerlin TE, Chasan-Taber L, Reynolds RM, Glueck DH, Dabelea D. Exposure to prenatal smoking and early-life body composition: the healthy start study. Obes (Silver Spring). 2015;23:234–41.
Harrod CS, Reynolds RM, Chasan-Taber L, Fingerlin TE, Glueck DH, Brinton JT, et al. Quantity and timing of maternal prenatal smoking on neonatal body composition: the Healthy Start study. J Pediatr. 2014;165:707–12.
de Wit CC, Sas TC, Wit JM, Cutfield WS. Patterns of catch-up growth. J Pediatr. 2013;162:415–20.
Braun JM, Daniels JL, Poole C, Olshan AF, Hornung R, Bernert JT, et al. Prenatal environmental tobacco smoke exposure and early childhood body mass index. Paediatr Perinat Epidemiol. 2010;24:524–34.
Riedel C, Fenske N, Muller MJ, Plachta-Danielzik S, Keil T, Grabenhenrich L, et al. Differences in BMI z-scores between offspring of smoking and nonsmoking mothers: a longitudinal study of German children from birth through 14 years of age. Environ Health Perspect. 2014;122:761–7.
Chen A, Pennell ML, Klebanoff MA, Rogan WJ, Longnecker MP. Maternal smoking during pregnancy in relation to child overweight: follow-up to age 8 years. Int J Epidemiol. 2006;35:121–30.
Haga C, Kondo N, Suzuki K, Sato M, Ando D, Yokomichi H, et al. Developmental trajectories of body mass index among Japanese children and impact of maternal factors during pregnancy. PLoS One. 2012;7:e51896.
Howe LD, Matijasevich A, Tilling K, Brion MJ, Leary SD, Smith GD, et al. Maternal smoking during pregnancy and offspring trajectories of height and adiposity: comparing maternal and paternal associations. Int J Epidemiol. 2012;41:722–32.
Oken E, Huh SY, Taveras EM, Rich-Edwards JW, Gillman MW. Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res. 2005;13:2021–8.
Caraballo RS, Giovino GA, Pechacek TF, Mowery PD. Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2001;153:807–14.
Benowitz N, Goniewicz ML, Eisner MD, Lazcano-Ponce E, Zielinska-Danch W, Koszowski B, et al. Urine cotinine underestimates exposure to the tobacco-derived lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in passive compared with active smokers. Cancer Epidemiol Biomark Prev. 2010;19:2795–800.
Zielinska-Danch W, Wardas W, Sobczak A, Szoltysek-Boldys I. Estimation of urinary cotinine cut-off points distinguishing non-smokers, passive and active smokers. Biomarkers. 2007;12:484–96.
Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, et al. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;144:399–407.
Shapiro AL, Kaar JL, Crume TL, Starling AP, Siega-Riz AM, Ringham BM et al. Maternal diet quality in pregnancy and neonatal adiposity: The Healthy Start Study. Int J Obes (Lond) 2016;40:1056–62.
Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, et al. Update of the healthy eating index: HEI-2010. J Acad Nutr Diet. 2013;113:569–80.
Moore BF, Sauder KA, Starling AP, Ringham BM, Glueck DH, Dabelea D. Exposure to secondhand smoke, exclusive breastfeeding and infant adiposity at age 5 months in the Healthy Start study. Pediatr Obes. 2017;12:111–9.
American Academy of Pediatrics Committee on Nutrition. Pediatric Nutrition Handbook, 6th edn. American Academy of Pediatrics: Elk Grove Village, IL, 2008.
Demidenko E. Mixed models: theory and applications with R, John Wiley & Sons, Hoboken, New Jersey 2013.
Little RJ, Rubin DB. Statistical analysis with missing data, John Wiley & Sons, Hoboken, New Jersey 2014.
Royston P, Sauerbrei W. Multivariable model-building: a pragmatic approach to regression anaylsis based on fractional polynomials for modelling continuous variables, vol. 777. John Wiley & Sons, Chicheser, England 2008.
Kenward MG, Roger JH. An improved approximation to the precision of fixed effects from restricted maximum likelihood. Comput Stat Data Anal. 2009;53:2583–95.
Pickett KE, Rathouz PJ, Kasza K, Wakschlag LS, Wright R. Self-reported smoking, cotinine levels, and patterns of smoking in pregnancy. Paediatr Perinat Epidemiol. 2005;19:368–76.
Goniewicz ML, Eisner MD, Lazcano-Ponce E, Zielinska-Danch W, Koszowski B, Sobczak A, et al. Comparison of urine cotinine and the tobacco-specific nitrosamine metabolite 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) and their ratio to discriminate active from passive smoking. Nicotine Tob Res. 2011;13:202–8.
Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89:423–41.
Windham GC, Eaton A, Hopkins B. Evidence for an association between environmental tobacco smoke exposure and birthweight: a meta-analysis and new data. Paediatr Perinat Epidemiol. 1999;13:35–57.
Ekelund U, Ong K, Linne Y, Neovius M, Brage S, Dunger DB, et al. Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: the Stockholm Weight Development Study (SWEDES). Am J Clin Nutr. 2006;83:324–30.
Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ. 1999;318:427–31.
Jain V, Singhal A. Catch up growth in low birth weight infants: striking a healthy balance. Rev Endocr Metab Disord. 2012;13:141–7.
Moore BF, Clark ML, Bachand A, Reynolds SJ, Nelson TL, Peel JL. Interactions between diet and exposure to secondhand smoke on the prevalence of childhood obesity: results from NHANES, 2007-2010. Environ Health Perspect. 2016;124:1316–22.
Ong KK. Catch-up growth in small for gestational age babies: good or bad? Curr Opin Endocrinol Diabetes Obes. 2007;14:30–4.
Lehtovirta P, Forss M. The acute effect of smoking on intervillous blood flow of the placenta. Br J Obstet Gynaecol. 1978;85:729–31.
Walsh RA. Effects of maternal smoking on adverse pregnancy outcomes: examination of the criteria of causation. Hum Biol. 1994;66:1059–92.
Somm E, Schwitzgebel VM, Vauthay DM, Camm EJ, Chen CY, Giacobino JP, et al. Prenatal nicotine exposure alters early pancreatic islet and adipose tissue development with consequences on the control of body weight and glucose metabolism later in life. Endocrinology. 2008;149:6289–99.
Bergen HT. Exposure to smoke during development: fetal programming of adult disease. Tob Induc Dis. 2006;3:5–5.
Suter MA, Anders AM, Aagaard KM. Maternal smoking as a model for environmental epigenetic changes affecting birthweight and fetal programming. Mol Hum Reprod. 2013;19:1–6.
Dietz PM, Homa D, England LJ, Burley K, Tong VT, Dube SR, et al. Estimates of nondisclosure of cigarette smoking among pregnant and nonpregnant women of reproductive age in the United States. Am J Epidemiol. 2011;173:355–9.
Kim S. Overview of Cotinine Cutoff Values for Smoking Status Classification. Int J Environ Res Public Health. 2016;13:1236.
Homa DM, Neff LJ, King BA, Caraballo RS, Bunnell RE, Babb SD, et al. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke--United States, 1999-2012. MMWR Morb Mortal Wkly Rep. 2015;64:103–8.
Acknowledgements
We gratefully acknowledge the contributions of Stephen Brindley for performing the laboratory analysis of cotinine.
Funding
This work was supported by the National Institutes of Health (R01DK076648, UG3OD023248, R01ES02293403, R01GM121081, K99ES028711) .
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: BFM, APS, SM, JLA, and DD designed the work of this study. CSH, WBA, BMR, and DHG contributed to the data acquisition and interpretation. SM, JLA, and DD supervised. BFM, BMR, and DHG performed the statistical analyses. BFM wrote the manuscript. APS, SM, CSH, WBA, JLA, BMR, DHG, and DD provided critical revisions to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Moore, B.F., Starling, A.P., Magzamen, S. et al. Fetal exposure to maternal active and secondhand smoking with offspring early-life growth in the Healthy Start study. Int J Obes 43, 652–662 (2019). https://doi.org/10.1038/s41366-018-0238-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0238-3
- Springer Nature Limited
This article is cited by
-
Prenatal exposure to tobacco and adverse birth outcomes: effect modification by folate intake during pregnancy
Maternal Health, Neonatology and Perinatology (2022)