Abstract
Traditional response criteria in myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) are based on bone marrow morphology and may not accurately reflect clonal tumor burden in patients treated with non-cytotoxic chemotherapy. We used next-generation sequencing of serial bone marrow samples to monitor MDS and AML tumor burden during treatment with epigenetic therapy (decitabine and panobinostat). Serial bone marrow samples (and skin as a source of normal DNA) from 25 MDS and AML patients were sequenced (exome or 285 gene panel). We observed that responders, including those in complete remission (CR), can have persistent measurable tumor burden (that is, mutations) for at least 1 year without disease progression. Using an ultrasensitive sequencing approach, we detected extremely rare mutations (equivalent to 1 heterozygous mutant cell in 2000 non-mutant cells) months to years before their expansion at disease relapse. While patients can live with persistent clonal hematopoiesis in a CR or stable disease, ultimately we find evidence that expansion of a rare subclone occurs at relapse or progression. Here we demonstrate that sequencing of serial samples provides an alternative measure of tumor burden in MDS or AML patients and augments traditional response criteria that rely on bone marrow blast percentage.
Similar content being viewed by others
Introduction
DNA-hypomethylating agents such as decitabine and azacitidine are commonly used to treat myelodysplastic syndromes (MDS) and older adults with acute myeloid leukemia (AML).1, 2, 3 Although rates of complete remission (CR) are relatively low, hypomethylating agents are associated with an improved overall survival when compared with conventional care regimens.2, 3, 4, 5, 6 In contrast to traditional cytotoxic agents such as anthracyclines and cytarabine, maximum responses can be delayed 4–6 cycles from initiation of therapy.7 In addition, patients will invariably relapse, which underscores the need for novel therapies.
Despite being non-curative, patients treated with hypomethylating agents who achieve hematologic improvement or stable disease (SD) may derive clinical benefit from these agents, suggesting that traditional response criteria may not accurately reflect antitumor activity.8 Monitoring tumor burden in MDS can be particularly challenging where the blast percentage underestimates tumor burden and is often <5% of bone marrow cells.9 In patients who otherwise meet criteria for CR, the presence of persistent dysplasia is highly subjective and may also not accurately reflect tumor burden. Tracking cytogenetic abnormalities can serve as a useful adjunct in monitoring treatment responses but up to 50% of MDS and AML patients have normal karyotypes. Therefore, traditional response criteria in MDS and AML that primarily rely on bone marrow morphology (for example, myeloblast percentage) or karyotype may not accurately reflect antitumor responses or clinical benefit.10, 11
A major advance in our understanding of MDS and AML biology has come from next-generation sequencing studies that have identified recurring somatic mutations. In MDS and AML, hematopoietic cells contain gene mutations that are variably distributed between the founding clone and daughter subclone(s).9, 12, 13, 14 A minor subclone present at diagnosis can escape eradication during initial therapy, acquire additional mutations and ultimately contribute to relapse. We hypothesized that serially monitoring tumor burden using next-generation sequencing would provide additional information that can augment traditional measures of response. To test this hypothesis, we used next-generation sequencing of serial bone marrow samples to monitor tumor burden and to characterize the changes in the clonal structure of MDS and AML that occur during treatment with epigenetic therapy. In this study, we combined the histone deacetylase inhibitor panobinostat with decitabine in older adults with high-risk MDS or AML.15 The addition of panobinostat to a previously established decitabine regimen allowed us to evaluate the concept that two epigenetic modifiers with distinct mechanisms of action may improve the responses of patients compared with historical treatment with decitabine alone.
Materials and methods
Patients
This trial was a phase I/II open-label study of panobinostat plus decitabine in older adults with high-risk MDS or AML. The primary clinical end points were to determine the maximum-tolerated dose and dose-limiting toxicity of panobinostat when given in combination with decitabine, and to determine the CR rate for the regimen. Eligible patients were age 60 years and older with high-risk MDS (International Prognostic Scoring System Int-2 or High) or AML excluding AML with promyelocytic leukemia/retinoic acid receptor and core-binding factor leukemias. Patients with prior treatment with either a hypomethylating agent or histone deacetylase inhibitor were ineligible. This study is registered at ClinicalTrials.gov (NCT00691938) and approved by the Institutional Review Board of Washington University. The study was carried out in accordance with the Declaration of Helsinki and amendments and written informed consent was obtained from all subjects before enrollment. Three patients enrolled in this study (PPI019, 023, 025) were reported in another publication.16
Treatment plan
Decitabine 20 mg/m2 was administered by intravenous infusion on days 1–5 of a 28-day cycle. Oral panobinostat was initially administered three times a week on nonconsecutive days in a 28-day cycle. Following a protocol amendment, subsequent dose levels of panobinostat were administered three times a week for the first 2 weeks only. A phase I dose escalation of panobinostat was performed using a standard 3+3 design ranging from 10 to 40 mg daily. In the phase II, the cohort was expanded to include total of 20 patients at the selected phase I dose. Serial bone marrow samples were collected prestudy, cycle 1 day 15, after every two cycles of treatment, and at the time of relapse for both clinical assessment and next-generation sequencing. A subset of patients had sequencing performed on bone marrow samples obtained after study completion. Responses were assessed according to International Working Group (IWG) criteria for AML and proposed modifications to the IWG criteria for MDS.10, 11
Sequencing and single-nucleotide polymorphism arrays
DNA from paired normal skin and bone marrow was enriched for a custom set of 285 recurrently mutated MDS and AML genes (recurrently mutated gene (RMG) panel including all coding exons; Supplementary Table 1) either alone (n=24 patients) or 'spiked in' to an exome-sequencing reagent (n=7 patients; enhanced exome sequencing (EES)). Exome-sequencing data was deposited in the dbGAP database (phs000159, study version 9). Enriched libraries were sequenced on a HiSeq2000 instrument (Illumina, San Diego, CA, USA) with 2 × 101 bp reads, as described previously.17 Paired tumor/normal variant calling for single-nucleotide variants and indels was performed, as described previously.17, 18 Copy number alteration analysis using sequencing and single-nucleotide polymorphism arrays is described in the Supplementary Methods. Single-nucleotide polymorphism array data was deposited in the GEO database (GSE81738). Ultradeep error-corrected sequencing (ED and MW, unpublished data) was performed on 45 serial treatment bone marrows. Briefly, ligation-based amplification probes were designed to target both DNA strands of all mutations identified by EES or RMG sequencing interrogating a total of 384 positions covered by 2054 amplicons. DNA (500 ng) was digested and hybridized to probes plus 10 bp degenerate oligonucleotides (molecular barcodes), and sample-specific indexes. Cases were sequenced to target 20 000 × to 100 000x coverage. Data were analyzed using the Barcrawler sequencing pipeline (ED, unpublished data), with a maximum sensitivity of 0.1% (additional details are provided in the Supplementary Methods). A complete list of the various genomic assays performed on patient samples and time-points is provided in Supplementary Table 2.
Results
Patient characteristics and clinical response rates
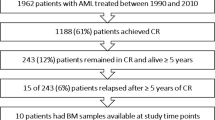
A total of 52 patients with a median age of 70 years were enrolled and treated on the study protocol (Table 1). The study population consisted of 38 patients with AML and 14 with MDS. Fifteen patients including 14 with AML had prior therapy for their hematologic disorder (Table 1).
In the phase I, panobinostat was escalated from 10 to 40 mg three times a week without reaching the maximum-tolerated dose. Although no dose-limiting toxicities were identified, a decision was made to reduce the dose to 40 mg for the first 2 out of 4 weeks in the dose expansion phase based on data suggesting improved tolerability.19 The most common adverse events reported during treatment include fatigue (88%), febrile neutropenia (76%), diarrhea (75%) and nausea (69%; Supplementary Table 3).
Fifty-one patients received at least one dose of panobinostat and were included in the efficacy analysis (37 patients with AML and 14 with MDS). Subjects received a median of two cycles of treatment (range <1–12). The phase I and II efficacy results were pooled. Using the International Working Group criteria, the overall rate of CR, cytogenetic CR (CRc), morphologic CR with incomplete blood count recovery (CRi) for AML patients (n=37) was 10% (1 CR, 1 CRc and 2 CRi), with an additional 19% of patients achieving a morphologic leukemia-free state (mLFS, n=7). For patients with MDS, 2 of 14 achieved a CR, including one CRc. An additional four MDS patients achieved a marrow CR (mCR) defined as <5% blasts in the bone marrow but not meeting the criteria for CR because of continued cytopenias or lack of RBC transfusion independence (Table 2). One MDS patient met the criteria for hematologic improvement in both platelets and neutrophils without achieving a CR. With a median follow-up of 58 months, the median overall survival for the 51 patients who received treatment was 6.44 months. For the phase II cohort, dose level 5B, the median overall survival was 3.8 months (Supplementary Figure 1).
Sequencing metrics
We identified 10 MDS and 15 AML patients with adequate banked skin (as a source of normal DNA) and paired bone marrow that also had at least one somatic mutation previously identified (data not shown). We sequenced skin and serial bone marrow samples from these 25 patients using a panel of 285 genes (including all coding exons) that are known to be recurrently mutated in AML and MDS (that is, RMGs). In addition, 7 of these 25 patients also had EES (exome plus RMG) of their skin and bone marrow samples from prestudy and one later time-point. Averaged coverage depth for the 285 RMG panel was 104x for skin and 160x for tumor. Averaged coverage depth for the EES was 65x for skin and 276x for tumor. For samples evaluated by ultradeep error-corrected sequencing, we obtained 31 849x average total coverage depth (mean range 11 711–207 272x) corresponding to 4936x average unique read family coverage depth (mean range 596–5842x) (Supplementary Figure 2 and Supplementary Methods).
Spectrum of gene mutations at diagnosis
The landscape of genomic alterations was highly concordant with previous studies of patients with MDS and AML (Figure 1a and Supplementary Table 4). Thirteen genes were mutated in at least three prestudy samples (Figure 1b) and we detected an average of 4.9 tier 1 (coding and splice sites) single-nucleotide variants and indels per patient (range 1–15) when only the RMG panel was used, compared with 27.4 mutations per patient (range 9–43) using EES (Figure 1c). A total of 26 genes had tier 1 mutations in two or more patients (Supplementary Table 4) at prestudy banking. The vast majority of these recurrently mutated genes include those with well-established association in MDS or AML. There was no significant association between the mutational status of a gene at prestudy and achieving a CR using this treatment regimen.
Heatmap of molecular and clinical findings. (a) Distribution of mutations in 25 patients (10 MDS, 15 AML) with at least one mutation in 16 genes or pathways in samples from any time-point. Each column represents an individual patient sample and each row represents a gene with a mutation. Mutations are indicated by colored cells and gene groups/families are indicated at the left. (b) The number of mutations in each gene present in prestudy samples is listed. Splice mutations include the splice acceptor and donor dinucleotides. (c) Number of coding mutations detected in the prestudy samples (excluding silent mutations). RMG, recurrently mutated genes in AML and MDS; complex cytogenetics, ⩾3 clonal abnormalities; complete remission, CR/CRc/CRi; non-evaluable, received <2 cycle of treatment; TF, transcription factors; PPI, positive patient identifier.
Monitoring of tumor burden during treatment
We next analyzed mutation variant allele fractions (VAFs) in serial samples to monitor changes in tumor burden during treatment. We segregated patients who had a prestudy sample sequenced and received two or more cycles of treatment into those that achieved a CR (CRi or CRc; n=4; Figure 2a), those with SD (n=2), mLFS (n=2) or mCR (n=2; Figure 2b) and those with treatment failure (n=4; Figure 2c). As expected, the majority of mutation VAFs from patients with treatment failure did not change during treatment. While some patients with a CR had complete disappearance of VAFs at serial time-points, others had persistence of mutation VAFs. Persistence of mutations was also observed for mCR, mLFS and SD categories. The average mutation VAF at the end of treatment was lower in patients achieving a CR versus those with mCR, mLFS and SD (4.3% vs 8.8%, respectively, P=0.03). Similarly, the average decrease in mutation VAFs from prestudy to end of treatment was greater in patients achieving a CR versus those who did not (21.4% vs 13.4%, respectively, P=0.0007). Further analysis of individual patients revealed five distinct mutation VAF patterns that were associated with different clinical responses, including (i) AML patients achieving a CR or CRc (PPI013, PPI019, respectively): mutation VAFs were undetectable by cycle 2 using next-generation sequencing of the RMG panel, (ii) AML with mLFS (PPI023, PPI031): mutation VAFs remained detectable but decreased to <10%, (iii) MDS with CRc and mCR (PPI005, PPI035, respectively): mutation VAFs decreased to <10% and were intermittently below the level of detection, (iv) MDS with mCR and CR (PPI008, PPI010, respectively) or SD (PPI049, PPI050): mutation VAFs were unchanged or decreased but some remained >10% and (v) AML with treatment failure (PPI006, PPI011, PPI022, PPI025): mutation VAFs were essentially unchanged and remained >30% (Supplementary Figure 3).
Dynamic changes in mutation VAFs during treatment. Mutation VAF in paired prestudy and time of best response samples from patients that achieved a CR (a) versus those that did not (b and c) (left panels). Each line represents a mutation that occurred in a diploid part of the genome. Serial mutation VAFs are displayed in the right panel. SD (n=2, blue), mLFS (n=2, orange) or mCR (n=2, orange).
Sequencing, cytogenetic, fluorescence in situ hybridization studies (FISH) and copy number alteration data (Supplementary Tables 5–7) for three representative cases with different mutation VAF patterns are shown in Figure 3. A cytogenetically normal AML patient (PPI013; AML with CR) started treatment with a blast count >80% (Figure 3a). Sequencing of the initial bone marrow sample demonstrated five mutations in recurrently mutated genes with a mean VAF of 24%. The patient achieved a CR with a normal blast count by the end of cycle 2. VAFs for these mutations became undetectable at cycle 2 by sequencing of the RMG panel, consistent with the clinical response. We also observed that the blast percentage decreases before dramatic changes in mutation VAFs at cycle 1 day 15, suggesting that the differentiation of blasts could falsely underestimate tumor burden (Figure 3a; see also PPI005 in Supplementary Figure 3).
Persistence of mutation VAFs in CR and SD. (a) An AML patient with normal cytogenetics (PPI013) achieved a CR at the end of cycle 2. The blast % (shown as a dark yellow line) decreased at cycle 1 day 15 before a decrease in five mutation VAFs, and normalized by the end of cycle 2. The molecular and morphologic response was similar in this patient. (b) An MDS patient with normal cytogenetics (PPI010) achieved a CR at the end of cycles 6 and 12. Mutations VAFs remained detectable throughout treatment, including a mutation in KDM6A that was present with a copy number-adjusted VAF ~20–30% (that is, ~40–60% of cells harboring a mutation). The molecular and morphologic response was discordant in this patient with a normal karyotype. (c) An MDS patient with abnormal cytogenetics (PPI050) had persistent SD throughout treatment. Cytogenetics and FISH normalized by cycle 8. While there was an initial decrease in mutation VAFs, they remained detectable throughout treatment. A mutation in ASXL1 was unchanged during treatment and may represent a clone that is independent of the malignant clone (that is, clonal hematopoiesis of indeterminate potential). The molecular and morphologic response was similar and the patient remained with cytopenias despite having a low level of detectable mutations. (d) Copy number alterations detected by RMG sequencing for PPI050 are shown. Copy number gains have a log 2 ratio of tumor versus normal >0 and losses <0. The altered regions are not detected by the end of cycle 2, including del(5). CNA, copy number alterations; PR, partial remission. *Copy number-adjusted VAF.
A cytogenetically normal MDS patient with RAEB-2 (PPI010; MDS with CR) presented with a blast count of 14% and a mean mutation VAF of 6.5% across multiple clones (Figure 3b). The patient had SD at the end of cycle 4 with a blast count of 6% and a mean VAF of 7.3%. The patient completed the study in CR with a blast count of 2%; however, the mean mutation VAF was 8.7% across multiple clones, indicating that ~17% of tumor cells were present in the bone marrow despite having achieved a morphologic and clinical CR.
The third patient (PPI050; MDS with SD), an MDS patient with RCMD and complex cytogenetics (including del(5q)), began the study with a blast count of 3% and a mean VAF of 20% (Figure 3c). The patient achieved SD by the end of cycle 2 with a blast count of <5% and mean VAF of 5.2% and completed the study in SD with a blast count of <5% and a mean VAF of 4.2%. This patient also had clonal cytogenetic findings that were variably detected during treatment. While conventional cytogenetics (20 metaphases) did not detect clonal findings beyond the prestudy time-point, FISH performed after cycles 4 and 6 showed low-level persistence of del(5) (9% and 1.33% of cells, respectively) consistent with sequencing results. However, cytogenetics, FISH and copy number alterations based on RMG gene panel sequencing were negative at cycles 8 and 10, whereas sequencing remained positive (Figures 3c and d). This patient had incomplete recovery of blood counts, despite having very low tumor burden based on FISH and sequencing. Collectively, the data indicate that there can be discrepancies between clinical and molecular response in patients treated with this regimen.
Complex patterns of clonal evolution
We have previously shown that MDS and AML samples contain both founding clone mutations (present in every cell of the tumor) and subclonal mutations, which occur in only a fraction of the tumor cells (and have lower VAFs). We identified dynamic changes in the size of distinct subclones by tracking mutation VAFs in serial samples. 'Falling' subclones with diminishing VAFs indicate specific susceptibility to therapy, whereas 'rising' subclones indicate a relative growth advantage and suggest treatment resistance.
AML patient PPI011 did not achieve a CR, but sequencing revealed selective clearance of a subclone harboring TP53 and RAD21 mutations (Figure 4a). The founding clone persisted and contained biallelic TP53 mutations. These cells subsequently acquired a deletion of the TP53 L130V allele at the end of cycle 4. While not curative in this patient, the falling subclone containing TP53 and RAD21 mutations identifies a combination of mutations that may be sensitive to panobinostat and decitabine treatment.
Differential sensitivity of tumor clones during treatment. (a) An AML patient (PPI011) with treatment failure harbors a subclone defined by three somatic RAD21 mutations (colored lines) that become undetectable by the end of treatment (that is, falling clone). An additional mutation (gray) defines the founding clone that is treatment-resistant and contains two TP53 mutations (colored in orange and cyan). (b) An MDS patient who achieved CR at cycle 4 progressed to sAML 924 days after the end of treatment on this study. Two subclones (red and blue) emerge and are detectable in the sAML sample. These subclones were not detected at prestudy or during the treatment cycles using a VAF threshold of 0.1% (that is, rising clones). (c) The mutation VAFs from MDS patient PPI005 are shown at the prestudy MDS stage and after progression to sAML at 924 days after the end of treatment. Mutation VAFs were adjusted for chromosomal copy number. Unsupervised clustering of individual mutations identified four distinct mutation clusters representing clones, two of which (red and blue) are specific to the sAML sample. (d) Spectrum of single base substitutions in clusters 1 and 2 (present in initial prestudy MDS) versus clusters 3 and 4 (detectable in sAML). The sAML-specific clusters show a greater proportion of C–G transversions that are associated with decitabine treatment, suggesting that some mutations are caused by the treatment. (e) For patient PPI005, the tumor phylogeny was inferred using the clonevol package (https://github.com/hdng/clonevol, manuscript in preparation). Two models are possible, differing only in whether subclone 4 is derived from subclone 2 or 3 (Supplementary Figure 6). The model assigned higher likelihood was used to produce the above plot summarizing the clonal evolution from the MDS stage to the sAML. Residual non-mutant normal cells are not depicted at MDS or sAML time-points (that is, percentage of cells with cluster mutations represents tumor cells only). Cells in clone 1 contain cluster 1 mutations. Clone 1 (green) is the founding clone and is present in nearly all bone marrow cells at MDS and sAML time-points; clone 2 (yellow) is similarly present in almost all cells at the MDS prestudy time-point, but is present in only 33% of cells in the sAML time-point. Clones 3 and 4 (blue and red) are not detected in the prestudy MDS sample but emerge at sAML and are present in 60% and 32% of bone marrow cells, respectively. EOT, end of treatment.
We also observed that progression from MDS to secondary AML (sAML) is sometimes characterized by the expansion of a rare subclone (that is, rising subclone; Figure 4b). We performed whole-exome sequencing on a bone marrow sample obtained 924 days after the end of treatment when this patient presented with sAML. Clustering of mutations present in the prestudy and sAML samples reveal that while the sAML is derived from the same founding clone, it also contains new subclonal mutations (Figure 4c). While C to T transitions are most common in the founding clone, the new subclones are dominated by C to G transversions (P=0.03; Figure 4d). Coupled with the knowledge that decitabine can induce C to G transversions,20 this altered mutation spectrum suggests that many of these rising subclone mutations may have been caused by decitabine treatment. The overall pattern of clonal evolution of PPI005 is complex and characterized by the fall of the MDS founding clone (green) and a subclone (yellow) during treatment, followed by the return of the founding clone (green) and emergence of three subclones at sAML progression (yellow, blue and red; Figure 4e).
Transient response of TP53 mutant clones is common
We next attempted to identify mutations that are predictive of a response to treatment by searching for genes that consistently showed a decrease in their mutation VAFs during treatment, regardless of whether present in a founding clone or subclone. TP53 and SRSF2 were the only genes mutated in at least three patients who had follow-up sequencing at cycle 2 or later, allowing us to correlate mutation status with clinical response. Although there was a consistent decrease in TP53 VAFs during treatment (Figure 5), this was not associated with obtaining a CR at the treatment dose and schedule of drugs used in this study. TP53 mutation VAFs decreased by an average of 26.5-fold in four patients; however, the VAF subsequently increased during relapse in three of five patients with follow-up samples. Only PPI050 has not relapsed and has since been maintained on single-agent decitabine (Figure 5). Two of the three patients with SRSF2 mutations had a decrease in their VAFs, but neither VAF dropped below 10% (Supplementary Figure 4).
TP53 mutation VAFs decrease during treatment. Four patients harbored somatic mutations inTP53 with VAFs >5% in prestudy or cycle 1 time-point, completed at least two cycles of treatment and had no evidence of TP53 loss of heterozygosity. These patients showed a mean VAF decrease of 26.5-fold at the end of treatment. All four patients had follow-up bone marrows obtained after completing the study, and three of four showed a subsequent increase in TP53 VAFs; the remaining patient (PPI050) continued on single-agent decitabine after completing the study (indicated by an asterisks). Mutations are indicated in standard p-syntax.
Mutations persist at low levels during clinical CR
Next, we investigated the extent to which clonal mutations were cleared under this regimen using an ultradeep error-corrected sequencing approach with a sensitivity of 0.1% VAF (see Supplementary Methods). We sequenced serial samples from eight patients using ultradeep error-corrected sequencing, including four patients achieving CRs (CRc or CRi) or mCR (Supplementary Table 2). In patient PPI005, nearly all mutations detected in the initial prestudy MDS sample could be detected in subsequent treatment time-points using this approach, often with VAFs much lower compared with that detectable by standard sequencing (that is, ~2.5% VAF). The TP53 p.R306* mutation, present with a VAF of 37% at the start of treatment, was not detected at treatment cycle 8 using standard sequencing (0 variant reads out of 113 unique reads). Using ultradeep error-corrected sequencing, we confirmed its presence with a VAF of 0.16% (6 unique read families out of 3692 total read families passing filter; Figure 6a, inset). We further validated these findings using droplet digital PCR (Supplementary Figure 5). Thus, even during clinical and molecular CR (based on standard sequencing, cytogenetics and FISH), ultradeep error-corrected sequencing provided evidence of persistent disease.
Persistence of rare tumor cells are detected using ultradeep error-corrected sequencing. (a) An MDS patient (PPI005) achieved CR at the end of cycle 4, consistent with the absence of mutation detection by standard sequencing platforms (conservative sensitivity indicated by the dashed line at 2.5% VAF). Somatic mutations were detected at all treatment time-points using ultradeep error-corrected sequencing and high sequence coverage, including during CR when many mutations are present with VAFs <1% (inset panel). Canonical gene mutations are indicated by colored circles. (b) An MDS patient with SD (no CR) shows similar persistence of detectable somatic mutations using ultradeep error-corrected sequencing across all treatment time-points, including those with VAFs <1% (inset). Mutations were detectable at cycles 8 and 10 when cytogenetics and FISH were negative. The ASXL1 mutation (green) does not change with treatment and is likely present in a non-malignant clone distinct from the founding clone.
We then demonstrated persistence and eventual expansion of clonal mutations, including the TP53 mutation, at progression to secondary AML, 924 days after the end of treatment. At secondary AML transformation, new progression-specific (that is, rising subclone) mutations were detected using whole-exome sequencing (Figure 4b). Patient PPI050 showed a similar persistence of MDS mutations using ultradeep error-corrected sequencing despite mutation VAFs being below the threshold of detection using standard non-error-corrected next-generation sequencing (Figure 6b, inset). While the majority of mutations travel together as a single clone in this patient, the ASXL1 variant, initially present with a VAF of 4.2%, appears to represent a distinct clone that is not affected by chemotherapy, and it probably represents a non-malignant clone.
Discussion
In this paper, we describe our results combining decitabine and panobinostat in older adults with high-risk MDS or AML. Although the combination was well tolerated by most patients, the addition of panobinostat did not improve rates of CR/CRi in comparison with prior studies of decitabine alone with reported CR rates of 13–18% in phase 3 studies.21, 22 Despite the low overall rates of CR/CRi, we were able to gain important insights into the clonal dynamics of MDS and AML during treatment with epigenetic therapy. We observed that blast percentage frequently underestimates the burden of disease in these patients, particularly in MDS, and that molecular responses can be discordant with clinical response criteria. Using a sensitive barcoded sequencing technique, we were able to reliably identify low-level persistence of mutations in patients with clinical CRs. Many of these mutations were not detected using standard next-generation sequencing. In addition, rare tumor cells were identified months to years before patients presented with a morphologic relapse. Collectively, detection and serial tracking of mutation VAFs provided a unique molecular signature for each patient, and allowed for the dynamic monitoring of tumor clones and detection of measurable residual disease.
Molecular profiling of tumors has contributed greatly to our understanding of the pathogenesis of hematologic malignancies.12, 18, 23, 24 Most tumors have several recognized driver mutations that are variably distributed between the founding clone and subclones, yielding an enormous number of combinations that might be important to tumorigenesis and outcomes. Prior studies have also suggested that mutations in genes encoding epigenetic modifiers, including DNMT3A or TET2, are predictive of response to hypomethylating agents.25, 26, 27, 28 The small sample size of this study limited our ability to study comprehensively the impact of many genotypes on response. However, we did observe that subclones with TP53 mutations show marked, but not durable, responses to treatment with panobinostat and decitabine. Collectively, there remains a large degree of variability in clinical outcomes based on single gene mutation status (categorized simply as absent or present). This lack of predictive power may reflect the combinatorial complexity of mutations in AML and MDS. While baseline mutations have some predictive ability in MDS and AML, our goal was to assess the feasibility and utility of monitoring tumor burden by serially monitoring mutations and clones during treatment. The serial sequencing of samples from the same patient allowed us to make several clinically relevant observations.
First, mutations frequently persist using this treatment regimen, even during a CR. The low-level mutation VAFs we detect in remission may represent persistence of mutant hematopoietic stem and progenitor cells (HSPCs) following epigenetic therapy, as previously shown using FISH and flow-sorted hematopoietic stem and progenitor cells.29, 30 Ultradeep error-corrected sequencing that we used here may allow for the detection and tracking of these rare cells without isolating hematopoietic stem and progenitor cells. Second, tracking individual mutation VAFs may not accurately reflect tumor burden. The persistence of the KDM6A mutation in this subject achieving a CR suggests that the abnormal blast count and cytopenias were not driven by the clone containing the KDM6A mutation. Whether this mutation resides in the hematopoietic stem cell or a later progenitor is not clear, but it is a long-lived cell as the clone persists for at least 12 months. The persistence of an ASXL1 mutation in PPI050 likely represents an unrelated clonal hematopoiesis of indeterminate potential mutation rather than a tumor clone.31, 32, 33, 34 Sequencing serial samples was necessary to decipher this possibility. Similarly, the persistence of clonal mutations does not necessarily indicate a clinical benefit is not obtainable. For example, PPI010 achieved a durable CR and PPI050 had a lasting SD with persistent mutation VAFs. Finally, we observed that tracking mutation VAFs only present in a subclone can underestimate the tumor burden in a patient (for example, RAD21 mutations in PPI011). Ultimately, tracking every clone with serial sampling will overcome these limitations.
Sequencing results provide an objective measure of tumor burden that may complement traditional response criteria and help guide treatment decisions. For PPI023 and PPI031 with mLFS, sequencing results indicate that the lack of hematopoietic recovery may be related to drug toxicity rather than tumor burden, suggesting a delay in treatment may be justified. Recently, Merlevede et al.35 reported that mutation VAFs were largely unchanged in monocytes from chronic myelomonocytic leukemia patients who responded to hypomethylating agents and achieved a mCR (that is, decrease in bone marrow blasts to <5% without hematologic improvement). Our data for patients with a mCR are similar, reinforcing the discordance between marrow blast percentage and mutation clearance. Sequencing results also indicate that decitabine can induce mutations during the course of treatment. PPI005 progressed to secondary AML, and two subclones emerged. These subclones contained new C to G transversions, a signature of decitabine exposure.20 A larger set of secondary AML samples arising after decitabine treatment will need to be sequenced to address whether decitabine-induced mutations may influence disease progression. This observation may have implications, as hypomethylating agents have been proposed and tested as maintenance therapy for AML.36 The contribution of panobinostat to the mutational and clonal changes is not known.
The development of effective therapies for patients with MDS or AML has been hampered by the lack of surrogate trial end points that can predict clinical benefit. Historically, phase 2 studies in high-risk MDS and AML have relied on CR as encouraging evidence of antitumor activity but almost uniformly have failed in phase 3 studies. By performing serial sequencing of samples obtained during the course of therapy, we gained important clinical insights into the tumor response to epigenetic therapy. As sequencing technologies continue to mature, we believe that serial analyses may provide important information that is complementary to traditional measures of outcome in clinical trials. Indeed, clearance of mutation VAFs after induction therapy is predictive of outcomes in AML.17 Given the clonal complexity of hematologic cancers, platforms that can identify and track all clones may be necessary to inform clinical practice. Ultimately, incorporating serial sequencing studies into clinical trial design may allow us to monitor tumor burden and better evaluate agents at earlier stage and guide strategies for subsequent drug development.
References
Cashen AF, Schiller GJ, O'Donnell MR, DiPersio JF . Multicenter, phase II study of decitabine for the first-line treatment of older patients with acute myeloid leukemia. J Clin Oncol 2009; 28: 556–561.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol 2002; 20: 2429–2440.
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer 2006; 106: 1794–1803.
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood 2015; 126: 291–299.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Gattermann N, Germing U et al. Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J Clin Oncol 2010; 28: 562–569.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 2009; 10: 223–232.
Silverman LR, Fenaux P, Mufti GJ, Santini V, Hellstrom-Lindberg E, Gattermann N et al. Continued azacitidine therapy beyond time of first response improves quality of response in patients with higher-risk myelodysplastic syndromes. Cancer 2011; 117: 2697–2702.
Gore SD, Fenaux P, Santini V, Bennett JM, Silverman LR, Seymour JF et al. A multivariate analysis of the relationship between response and survival among patients with higher-risk myelodysplastic syndromes treated within azacitidine or conventional care regimens in the randomized AZA-001 trial. Haematologica 2013; 98: 1067–1072.
Walter MJ, Shen D, Ding L, Shao J, Koboldt DC, Chen K et al. Clonal architecture of secondary acute myeloid leukemia. N Engl J Med 2012; 366: 1090–1098.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol 2003; 21: 4642–4649.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 2006; 108: 419–425.
Walter MJ, Shen D, Shao J, Ding L, White BS, Kandoth C et al. Clonal diversity of recurrently mutated genes in myelodysplastic syndromes. Leukemia 2013; 27: 1275–1282.
Welch JS, Ley TJ, Link DC, Miller CA, Larson DE, Koboldt DC et al. The origin and evolution of mutations in acute myeloid leukemia. Cell 2012; 150: 264–278.
Ding L, Ley TJ, Larson DE, Miller CA, Koboldt DC, Welch JS et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature 2012; 481: 506–510.
Atadja P . Development of the pan-DAC inhibitor panobinostat (LBH589): successes and challenges. Cancer Lett 2009; 280: 233–241.
Welch J, Petti A, Miller C, Fronick C, O'Laughlin M, Fulton R et al. TP53 and decitabine in acute myeloid leukemia and myelodysplastic syndromes. NEJM, in press.
Klco JM, Miller CA, Griffith M, Petti A, Spencer DH, Ketkar-Kulkarni S et al. Association between mutation clearance after induction therapy and outcomes in acute myeloid leukemia. JAMA 2015; 314: 811–822.
Research TCGA. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med 2013; 368: 2059–2074.
San-Miguel JF, Richardson PG, Gunther A, Sezer O, Siegel D, Blade J et al. Phase Ib study of panobinostat and bortezomib in relapsed or relapsed and refractory multiple myeloma. J Clin Oncol 2013; 31: 3696–3703.
Jackson-Grusby L, Laird PW, Magge SN, Moeller BJ, Jaenisch R . Mutagenicity of 5-aza-2'-deoxycytidine is mediated by the mammalian DNA methyltransferase. Proc Natl Acad Sci USA 1997; 94: 4681–4685.
Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol 2012; 30: 2670–2677.
Lubbert M, Suciu S, Baila L, Ruter BH, Platzbecker U, Giagounidis A et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol 2011; 29: 1987–1996.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 2014; 28: 241–247.
Papaemmanuil E, Gerstung M, Malcovati L, Tauro S, Gundem G, Van Loo P et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood 2013; 122: 3616–3627.
Metzeler KH, Walker A, Geyer S, Garzon R, Klisovic RB, Bloomfield CD et al. DNMT3A mutations and response to the hypomethylating agent decitabine in acute myeloid leukemia. Leukemia 2012; 26: 1106–1107.
Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia 2011; 25: 1147–1152.
Bejar R, Lord A, Stevenson K, Bar-Natan M, Perez-Ladaga A, Zaneveld J et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood 2014; 124: 2705–2712.
Traina F, Visconte V, Elson P, Tabarroki A, Jankowska AM, Hasrouni E et al. Impact of molecular mutations on treatment response to DNMT inhibitors in myelodysplasia and related neoplasms. Leukemia 2014; 28: 78–87.
Craddock C, Quek L, Goardon N, Freeman S, Siddique S, Raghavan M et al. Azacitidine fails to eradicate leukemic stem/progenitor cell populations in patients with acute myeloid leukemia and myelodysplasia. Leukemia 2013; 27: 1028–1036.
Will B, Zhou L, Vogler TO, Ben-Neriah S, Schinke C, Tamari R et al. Stem and progenitor cells in myelodysplastic syndromes show aberrant stage-specific expansion and harbor genetic and epigenetic alterations. Blood 2012; 120: 2076–2086.
Xie M, Lu C, Wang J, McLellan MD, Johnson KJ, Wendl MC et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat Med 2014; 20: 1472–1478.
Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med 2014; 371: 2488–2498.
Genovese G, Kahler AK, Handsaker RE, Lindberg J, Rose SA, Bakhoum SF et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med 2014; 371: 2477–2487.
McKerrell T, Park N, Moreno T, Grove CS, Ponstingl H, Stephens J et al. Leukemia-associated somatic mutations drive distinct patterns of age-related clonal hemopoiesis. Cell Rep 2015; 10: 1239–1245.
Merlevede J, Droin N, Qin T, Meldi K, Yoshida K, Morabito M et al. Mutation allele burden remains unchanged in chronic myelomonocytic leukaemia responding to hypomethylating agents. Nat Commun 2016; 7: 10767.
Boumber Y, Kantarjian H, Jorgensen J, Wen S, Faderl S, Castoro R et al. A randomized study of decitabine versus conventional care for maintenance therapy in patients with acute myeloid leukemia in complete remission. Leukemia 2012; 26: 2428–2431.
Acknowledgements
This work was supported by Novartis, NIH/NCI K23CA140707 (GLU) and a SPORE in Leukemia (P50CA171963 to DCL, EJD, JFD, JSW, TJL, TAG, and MJW), ICTS-CTSA (to EJD), Gabrielle’s Angel Foundation (to MJW), a Leukemia and Lymphoma Society Scholar Award (to MJW), and the Lottie Caroline Hardy Trust (TAG, MJW). Support for procurement of human samples was provided by an NIH/NCI grant (P01 CA101937). Technical assistance was provided by the Alvin J Siteman Cancer Center Tissue Procurement Core supported by an NCI Cancer Center Support Grant (P30CA91842).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
GLU has received compensation as a consultant for Novartis. The other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Uy, G., Duncavage, E., Chang, G. et al. Dynamic changes in the clonal structure of MDS and AML in response to epigenetic therapy. Leukemia 31, 872–881 (2017). https://doi.org/10.1038/leu.2016.282
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2016.282
- Springer Nature Limited
This article is cited by
-
Combined inhibition of histone deacetylase and cytidine deaminase improves epigenetic potency of decitabine in colorectal adenocarcinomas
Clinical Epigenetics (2023)
-
Clonal architecture predicts clinical outcomes and drug sensitivity in acute myeloid leukemia
Nature Communications (2021)
-
Prognostic significance of serial molecular annotation in myelodysplastic syndromes (MDS) and secondary acute myeloid leukemia (sAML)
Leukemia (2021)
-
Hypomethylating agents (HMA) for the treatment of acute myeloid leukemia and myelodysplastic syndromes: mechanisms of resistance and novel HMA-based therapies
Leukemia (2021)
-
Secondary AML Emerging After Therapy with Hypomethylating Agents: Outcomes, Prognostic Factors, and Treatment Options
Current Hematologic Malignancy Reports (2021)