Abstract
The prognosis for patients multiple myeloma (MM) has improved substantially over the past decade with the development of new, more effective chemotherapeutic agents and regimens that possess a high level of anti-tumor activity. In spite of this important progress, however, nearly all MM patients ultimately relapse, even those who experience a complete response to initial therapy. Management of relapsed MM thus represents a vital aspect of the overall care for patients with MM and a critical area of ongoing scientific and clinical research. This comprehensive manuscript from the International Myeloma Working Group provides detailed recommendations on management of relapsed disease, with sections dedicated to diagnostic evaluation, determinants of therapy, and general approach to patients with specific disease characteristics. In addition, the manuscript provides a summary of evidence from clinical trials that have significantly impacted the field, including those evaluating conventional dose therapies, as well as both autologous and allogeneic stem cell transplantation. Specific recommendations are offered for management of first and second relapse, relapsed and refractory disease, and both autologous and allogeneic transplant. Finally, perspective is provided regarding new agents and promising directions in management of relapsed MM.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a B-cell neoplasm characterized by aberrant expansion of plasma cells, typically within the bone marrow but increasingly in extramedullary sites with disease progression.1 Induction regimens incorporating thalidomide, lenalidomide and/or bortezomib are now standard for newly diagnosed MM.2, 3, 4, 5, 6 Eligible patients may undergo autologous stem cell transplantation (ASCT), which deepens and prolongs the therapeutic response and improves outcome, especially when integrated with novel agents.7, 8, 9 Consolidation/maintenance post-ASCT not only upgrades but also deepens the response which translates into improved progression-free survival (PFS).10, 11 Current approaches to management of newly diagnosed MM have significantly increased survival in MM.12, 13 However, even patients who achieve a high quality and prolonged duration of response with initial therapy will ultimately relapse. Thus, management of relapsed disease is a critical aspect of MM management and an important focus of ongoing research.
Definitions and diagnosis of relapsed/refractory and progressive MM
Definitions
Progressive MM is defined as a 25% increase from baseline in the serum monoclonal protein (M-protein; absolute increase ⩾0.5 g/dl), urine M-protein (absolute increase >200 mg/day), percentage of bone marrow plasma cells (absolute percentage increase >10%), and/or the difference between involved and uninvolved free light chain levels (absolute increase must be >10 mg/dl).14 Progressive disease can also be established based on the presence of definite new bone lesions and/or soft tissue plasmacytomas, with a clear increase in the size of existing plasmacytomas, or hypercalcemia, that cannot be attributed to another cause.
Disease that meets these criteria for progression is defined as relapsed disease. Relapsed and refractory MM, meanwhile, is defined as disease that progresses on salvage therapy or progresses within 60 days of the last treatment in patients who previously achieved at least a minimal response (MR) to treatment.
These entities are distinguished from primary refractory MM, which refers to disease that fails to achieve at least an MR with any therapy. It is also important to note that following ASCT, oligoclonal reconstitution may occur which is temporary and does not indicate relapse.15
Diagnostic evaluation
The diagnostic evaluation includes serum protein electrophoresis with immunofixation, 24-h urine for both total protein and urine protein electrophoresis with immunofixation, and the serum-free light chain assay. A comprehensive metabolic panel is obtained with attention to renal function, calcium concentration and other metabolic abnormalities. A complete blood count with differential is obtained to assess for cytopenias as well as the presence of circulating plasma cells. The β2 microglobulin is usually obtained, as recent analyses suggest value in assessing this parameter prognostically in the context of disease relapse.16
Bone marrow evaluation is considered a standard of care when evaluating relapsed MM, though on some occasions may not be necessary, if disease progression is clearly confirmed by serum protein electrophoresis/urine protein electrophoresis and/or serum-free light chain. Bone marrow evaluation should be performed in cases of non- or oligo-secretory disease as well as when a secondary bone marrow process such as myelodysplasia is suspected. When bone marrow evaluation is undertaken, repeat fluorescence in situ hybridization analysis (with CD138 selection of cIg in situ hybridization) should be performed, since new chromosomal abnormalities may be identified, with possible exceptions in cases where high-risk cytogenetic features had been previously identified.
Imaging with either skeletal survey, magnetic resonance imaging or, in selected cases, fluorodeoxyglucose-positron emission tomography is conducted to assess for new sites of disease, an increase in previous areas of involvement or the presence of extramedullary disease.
Determinants of therapy
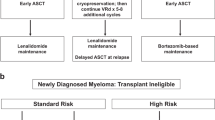
In undertaking the diagnostic evaluation, it is important to consider various factors that will influence treatment strategy (Figure 1). These include characteristics of the disease itself, response and duration of response (DOR) to prior therapy including treatment-related toxicities, eligibility for stem cell transplantation and characteristics of the individual patient.
Disease characteristics
Relapsed MM may manifest as biochemical progression based on an increase in the paraprotein concentration, with no associated symptoms or MM-related organ dysfunction. In other cases, progressive disease develops with prominent symptoms and/or significant organ compromise such as cytopenias, bone or soft tissue plasmacytomas, hypercalcemia, or renal failure.
High-risk relapsed disease is defined by any of the following characteristics (Table 1).
-
Adverse cytogenetic abnormalities (hypodiploidy, t(4;14), del(17p), amp(1q21).
-
High B2M (>5.5 mg/l) or low albumin (<3.5 mg/dl).
-
The presence of extramedullary disease.
-
Short DOR to prior therapy or progression while on current therapy.
-
Aggressive clinical features including.
-
Rapid onset of clinical symptoms
-
Extensive disease at relapse based on laboratory, pathology, or radiographic findings
-
Disease-associated organ dysfunction at relapse including renal failure, hypercalcemia or bone event such as fracture
-
High LDH.
-
Circulating plasma cells.
As in newly diagnosed disease, adverse cytogenetic abnormalities detected at relapse portend a poor outcome.17, 18 High-risk chromosomal abnormalities such as del(17p) may be detected in a patient who previously had standard-risk MM. A patient with high-risk cytogenetics at diagnosis retains that designation throughout the disease course.
Characteristics of prior or ongoing therapy
A thorough review of previous and ongoing therapies, duration of prior therapies, and both depth and DOR to prior treatment is necessary at the time of disease progression. Short DOR and progression while on therapy are associated with adverse outcomes.17, 18 Previous treatment-related toxicities are reviewed and attributed when possible to a specific agent.
Transplant status
Potential eligibility for ASCT or allogeneic SCT (Allo-SCT) is an important consideration. A patient who has previously undergone single ASCT may be eligible for a second course of high-dose therapy with autologous stem cell rescue if the PFS after the first was at least 18–24 months. If the patient did not receive consolidation/maintenance therapy post initial ASCT, such therapy should be considered following the second ASCT. It should be also recognized that this target progression-free interval of at least 18 months post-ASCT was established before consolidation/maintenance was as widely practiced as is now the case. Allo-SCT is associated with significant treatment-related morbidity and mortality, but can be considered in appropriately selected younger patients with a suitable donor.
Patient characteristics
Important clinical features such as performance status, co-morbidities and goals of care have a significant influence on MM treatment decisions, with less intensive approaches reserved for those with frailty and/or significant co-morbidities.
General treatment principles in the management of relapsed mm
When to treat?
Treatment is indicated when patients develop symptomatic relapse, a rapidly rising paraprotein level or extramedullary disease. Patients experiencing biological relapse alone do not necessarily need to be treated immediately. In this case, the speed of increase of the monoclonal peak, such as a doubling time of 3 months or shorter, would suggest initiating treatment. For asymptomatic biochemical relapse and a slow rise in the paraprotein level, restaging with a stringent wait and watch approach and follow up at least every 3 months can be recommended. Some patients develop oligoclonal reconstitution post-ASCT, which can occur in up to 37% of patients in this setting.19 This is transient, can be observed and should not be treated.
General management
A patient who is naïve to an agent (or a class of drugs) is typically treated with a regimen incorporating this agent (or any agent from the drug class). A patient with relapsed MM who has not previously undergone ASCT, for example, can be considered for high-dose therapy. A patient who previously responded to a particular agent with a DOR of at least 6–9 months can be retreated at relapse with similar drugs used previously or in combination with other agents.20, 21
Duration of therapy in relapsed MM is determined by the clinical context. Since no prospective studies addressing this issue are available, the following considerations are based on clinical experience only. The patient with aggressive disease characteristics at the time of relapse is likely to progress without ongoing therapy and typically requires continuous therapy. In the patient with indolent disease who responds to treatment, options include consolidation with ASCT, maintenance therapy or careful observation for a period of time without therapy, but caution here is warranted given the propensity of disease to sometimes rapidly evolve into a more aggressive phenotype.
Approach to the patient with aggressive disease characteristics
Patients with high-risk disease without co-morbidities and with adequate performance status are generally treated with highly active three- or four-drug combinations to achieve maximal response. Appropriately selected patients who respond to initial therapy in the relapsed setting can then be considered for ASCT. Allo-SCT represents an option for a subset of treatment-responsive patients with younger age, an available human leukocyte antigen-matched donor, chemotherapy-sensitive disease and excellent performance status.
Approach to the patient with indolent disease characteristics
Patients with indolent disease at relapse are generally treated with regimens that include an agent to which the patient is either naïve or has known sensitivity. It remains uncertain whether one- or two-drug regimens should be preferentially utilized in this setting over three- or four-drug regimens, although randomized trials increasingly support the three-drug approach for relapsed MM in general. Treatment intensification with ASCT can be considered for patients without prior exposure to high-dose therapy and those who sustained a prolonged response to prior autologous transplant.
Current treatment regimens in relapsed and refractory mm
With the development of multiple new therapeutic agents over the past decade, the repertoire of treatment options for relapsed MM has expanded considerably.
Immunomodulatory drugs
Thalidomide monotherapy
In the initial phase II trial with single-agent thalidomide, 84 individuals with relapsed and refractory MM received daily thalidomide at doses ranging from 200 to 800 mg.22 The overall response rate (ORR) was 32%, with 2-year event-free survival and overall survival (OS) rates of 20 and 48%, respectively.23 The ORR to single-agent thalidomide in relapsed MM has ranged from 14 to 43% with median response durations of 12–14 months.23, 24, 25, 26, 27, 28, 29
Important toxicities associated with these high doses of thalidomide include thrombosis, sedation, fatigue and constipation.30, 31 Peripheral neuropathy (PN) is cumulative, being both dose and time dependent and can be irreversible.
Thalidomide plus dexamethasone
In an analysis of 12 phase II trials of 451 patients with relapsed or relapsed/refractory MM (RR MM) treated with thalidomide dexamethasone, the ORR was 46%.32 Venous thromboembolism occurred in up to 25% of patients with relapsed MM receiving thalidomide with dexamethasone and/or chemotherapy, underscoring the need for effective thromboprophylaxis.33
Lenalidomide monotherapy
In a randomized phase II study, 70 patients with relapsed or relapsed/refractory disease were randomized to lenalidomide 30 mg daily or 15 mg twice daily for 21 days of every 28-day cycle.34 The 15 mg twice daily dose was associated with increased grade 3/4 myelosuppression compared with daily dosing. The ORR to lenalidomide monotherapy was 25% with a median OS of 28 and 27 months in the 30 mg once daily and 15 mg twice daily groups. In a subsequent phase II study of single-agent lenalidomide involving 222 patients with RR MM, the rate of ⩾partial response (PR) was 26%.35 The median PFS and OS in this study were encouraging, at 4.9 and 23.2 months, respectively.
Lenalidomide plus dexamethasone
The efficacy of lenalidomide plus dexamethasone was demonstrated in two randomized, double-blind, placebo-controlled studies in patients with RR MM—the MM-009 trial and the MM-010 trials (Table 2).36, 37 In both studies, patients were randomized to lenalidomide 25 mg or placebo on days 1–21 of a 28-day cycle. All patients received dexamethasone on days 1–4, 9–12 and 17–20 for four cycles and on days 1–4 only in subsequent cycles. Lenalidomide plus dexamethasone (dex) produced superior PR or better rates (Table 1) (MM-009: 61%; MM-010: 60.2%) compared with placebo-dex (MM-009: 19.9%; MM-010: 24%), and the median time to progression (TTP) was significantly longer with lenalidomide plus dex (MM-009: 11.1 months; MM-010: 11.3 months) compared with placebo-dex (4.7 months in both trials). Grade 3/4 toxicities associated with the combination included anemia, neutropenia, thrombocytopenia and venous thrombo‘embolism.33 These pivotal studies led to the approval of lenalidomide plus dex for the treatment of RR MM.
Pomalidomide monotherapy
Pomalidomide, which was approved by the Food and Drug Administration in February 2013, and in combination with dexamethasone by the European Medicines Agency in August 2013, was evaluated as monotherapy at doses ranging from 1 to 10 mg in a phase I study involving 24 patients.38 The rate of ⩾PR was 50%, and rate of ⩾MR 67%. With further evaluation the single-agent activity of pomalidomide in patients with disease resistant to bortezomib and lenalidomide is around 15%.39
Pomalidomide is currently indicated in patients who have received at least 2 prior therapies (including lenalidomide and bortezomib) and have disease progression on or within 60 days of completion of the last therapy.
Pomalidomide plus dexamethasone
In the pivotal 002 randomized Phase 2 study of pomalidomide with or without dexamethasone confirmed ORR of the order of 34% (pomalidomide with dexamethasone) in RR MM in patients resistant to both immunomodulatory drugs (IMiDs) and proteasome inhibitors, including bortezomib and carfilzomib, as well as showing activity in patients with high-risk features including adverse cytogenetics.39 Pomalidomide plus low-dose dexamethasone was compared with high-dose dexamethasone in an open-label phase III study involving 302 patients, and demonstrated the superiority of the combination in terms of PFS (4.0 vs 1.9 months, P<0.0001) and OS (12.7 vs 8.1 months, P=0.028).40 Interestingly, patients with del17p responded better to a combination of pomalidomide and dexamethasone compared to patients with a translocation t(4;14) in a recent French study.41
Proteasome Inhibitors
Bortezomib monotherapy
In a pivotal phase II study, bortezomib monotherapy administered to 202 patients with RR MM was associated with an ORR of 34%.42 The median DOR was 12 months, and median OS, 16 months. The phase III APEX study confirmed the efficacy of single-agent bortezomib in RR MM (Table 3).43 The study included 669 patients with a median of two prior therapies with RR MM who were randomized to intravenous (i.v.) bortezomib or high-dose dex. Bortezomib was superior in terms of ORR (46 vs 21%, P<0.001), median TTP (6.2 vs 3.5 months, P<0.001) and 1-year OS rate (80 vs 66%, P<0.003). Bortezomib activity was independent of chromosomal abnormalities such as del(13) and t(4;14).44 Bortezomib-related toxicities include PN, gastrointestinal symptoms, fatigue, thrombocytopenia, neutropenia and herpes zoster reactivation.
Subcutaneous versus intravenous bortezomib
A phase III study compared the efficacy and safety of subcutaneous (s.c.) versus i.v. bortezomib in patients with relapsed/refractory MM. S.c. bortezomib demonstrated non-inferior efficacy in comparison with standard i.v. administration, with an improved safety profile, especially decreased neurotoxicity.45
Bortezomib plus dexamethasone
The addition of dexamethasone to i.v. bortezomib improves rates of response and also improves tolerability.46, 47 The combination of bortezomib with dexamethasone administered as a second-line therapy was associated with ⩾PR in 66% of patients, with a median TTP of 9.5 months.48
Carfilzomib
Carfilzomib (formerly PR-171) is an irreversible proteasome inhibitor.49 Two parallel phase 2 studies, PX-171-003-A150 and PX-171-004,51 evaluated carfilzomib in patients with RR MM (Table 3).
In the open-label, single-arm phase II PX-171-003-A1 study, patients received carfilzomib 20 mg/m2 i.v. twice weekly for 3 out of 4 weeks in cycle 1, then 27 mg/m2 for up to 12 cycles with low-dose dexamethasone as premedication. Patients had a median of 5 prior lines of therapy and 80% were refractory to or intolerant of both bortezomib and lenalidomide. ORR was 23% with median DOR of 7.8 months and a median OS of 15.6 months. Common adverse events included fatigue (49%), anemia (46%), nausea (45%) and thrombocytopenia (39%). Twelve percent experienced PN, primarily grades 1 to 2, with some significant cardiopulmonary toxicity as well as renal dysfunction also encountered.50
In the PX-171-004 study, carfilzomib with low-dose dexamethasone premedication was given to bortezomib-naïve RR MM patients. Patients in cohort 1 received i.v. carfilzomib 20 mg/m2 for all treatment cycles, while those in cohort 2 received 20 mg/m2 in cycle 1 and 27 mg/m2 in subsequent cycles. The ORR was 59 and 64% in cohorts 1 and 2, respectively. Median DOR was 13 months and not reached in the respective cohorts, and median TTP was 8 months and not reached, respectively.51
Carfilzomib is indicated for patients who have received at least two prior therapies including bortezomib and an immunomodulatory agent and have demonstrated disease progression on or within 60 days of completion of last therapy, and was recently approved for relapsed disease in combination with lenalidomide and dexamethasone.
Bendamustine
Bendamustine monotherapy
Bendamustine has activity as a single agent. In a dose-escalation study of bendamustine in 31 patients up to the age of 70 years (60 up to 100 mg/m2) the ORR was 55% with a PFS of 8 months.52
Bendamustine plus prednisone
A retrospective study analyzed the use of bendamustine in 110 patients with RR MM after prior therapy with alkylators, steroids, IMiDs (lenalidomide or thalidomide) and bortezomib. Bendamustine was given at the doses of 60 to 150 mg/m2 on days 1 and 2 in combination with prednisone in 28 days cycles. The OR rate was 30% (2% CR+28% PR). The median PFS was 9.3 months with a median OS of 12.4 months.53
Panobinostat
Panobinostat is a potent oral pan-deacetylase inhibitor that in preclinical studies has synergistic antimyeloma activity when combined with bortezomib and dexamethasone.54 A phase 3 trial, PANORAMA1, included 768 patients with relapsed or RR MM who were randomly assigned to receive 21 day cycles of placebo or panobinostat (20 mg; on days 1, 3, 5, 8, 10, 12, orally), both in combination with bortezomib (1.3 mg/m2) on days 1, 4, 8, 11 i.v) and dexamethasone (20 mg on days 1, 2, 4, 5, 8, 9, 11, 12 orally). Median PFS was significantly longer in the panobinostat group than in the placebo group (11.99 vs 8·.08 months; hazard ratio (HR)=0.63; P<0.0001). Median OS was 33.64 months for the panobinostat group and 30.39 months for the placebo group (HR 0.87, P=0.26). The proportion of patients achieving an ORR did not differ between treatment groups; however, the proportion of patients with a complete response (CR) or complete response (nCR) was significantly higher in the panobinostat group than in the placebo group (27.6 vs 15.7%; P=0.00006). Thrombocytopenia, diarrhea and fatigue were more frequent in the panobinostat group. Panobinostat is approved for the treatment of relapsed and refractory multiple myeloma after bortezomib and lenalidomide failure.55
Multidrug combinations
IMiD plus alkylating agents
Melphalan plus thalidomide: In a phase II study, patients with relapsed MM received 100 mg/day thalidomide escalated weekly up to 600 mg/day alone (n=23) or in combination with oral 0.20 mg/kg/day melphalan administered monthly for four consecutive days (n=27).56 A PR was observed in 59% of melphalan plus thalidomide-treated patients compared with 26% in the thalidomide group (P=0.009). A CR was achieved by three patients treated with melphalan plus thalidomide versus none in the thalidomide monotherapy group. With 13 months median follow-up (range 6–32), PFS at 2 years was significantly longer in the combination group (61 vs 45%; P=0.0376), whereas OS did not differ significantly.
Cyclophosphamide, thalidomide, dexamethasone: In a phase II trial of weekly oral cyclophosphamide 300 mg/m2, monthly pulsed low-dose dexamethasone and thalidomide 300 mg/day, the PR rate was 62%, including 17% CR. Twenty-seven percent of patients developed infection, most of which were respiratory, but there were no infection-related deaths.57
In another phase II study evaluating the cyclophosphamide, thalidomide, dexamethasone combination, 53 patients received pulsed cyclophosphamide (150 mg/m2 twice daily, days 1–5), thalidomide (400 mg, days 1–5 and 14–18) and dexamethasone (20 mg/m2, days 1–5 and 14–18). Thirty-two patients (60%) achieved PR with a median time to response of 1.5 months.58
Lenalidomide, cyclophosphamide, dexamethasone: The combination of cyclophosphamide, lenalidomide and dexamethasone was evaluated in a phase I/II study in which 31 patients with a median of 3 prior lines of therapy received oral cyclophosphamide (dose range 300–700 mg) on days 1 and 8 of a 28-day cycle; lenalidomide 25 mg on days 1–21; and dex on 20 mg days 1–4 and 8–1 1 (Table 2).59 The rate of ⩾PR was 81%, with a CR rate of 29%. Among 10 patients treated at the maximum tolerated dose of cyclophosphamide 600 mg, the CR rate was 40%.60 High-grade toxicities included neutropenia, thrombocytopenia, infection and somnolence.
Lenalidomide, cyclophosphamide, prednisone: The combination of lenalidomide and continuous oral cyclophosphamide and prednisone was evaluated in a small series of heavily pretreated and lenalidomide refractory patients. Response to therapy was seen in 50% of patients, including 14.3% of patients with a CR and 21.4% with a very good partial response (VGPR). 61 This study was followed by an open-label phase I/II study that evaluated the optimal dose of the different drugs. The maximum tolerated dose was lenalidomide 25 mg (d1–d21), continuous cyclophosphamide (50 mg/day) and prednisone 20 mg/day. The ORR was 67% with a PFS of 6.3 months and OS of 15.5 months62 Grade 3 hematologic adverse events included neutropenia (22%), thrombocytopenia (19%) and anemia (12%). Grade 3 non-hematologic adverse events included infections (22%) and cardiac complications (10%).
Lenalidomide, melphalan, prednisone, thalidomide: In a phase II study involving 44 patients with RR MM and maximum two prior lines of therapy, lenalidomide (10 mg/day) was administered on days 1–21 in combination with thalidomide 50 or 100 mg/day, oral melphalan (0.18 mg/kg) and oral prednisone (2 mg/kg) on days 1–4 of each 28-day cycle. Six cycles of therapy were followed by lenalidomide maintenance until unacceptable toxicity or progression. Seventy-five percent achieved ⩾PR, including 32% VGPR and 2% CR. The 1-year PFS was 51% and 1-year OS was 72%. Grade 4 hematologic adverse events included neutropenia (18%), thrombocytopenia (7%) and anemia (2%). Grade 3 non-hematologic adverse events included infections (14%), neurologic toxicity (4.5%) and fatigue (7%).63
Lenalidomide, bendamustine, dexamethasone: In a phase I/II study involving 29 patients with RR MM, lenalidomide plus bendamustine and dexamethasone yielded a PR rate of 52% and VGPR 24%.64 The median PFS was 6.1 months, the 1-year PFS 20% and the 1-year OS 93%. Frequent toxicities included neutropenia, thrombocytopenia, anemia and fatigue.
A similar combination with prednisone instead of dexamethasone and lower doses of bendamustine (60–75 mg/m2) gave encouraging results: 76% ORR (5% CR+71% PR) and at 18 months 48% PFS and 64% OS.65
Pomalidomide, cyclophosphamide, dexamethasone: Pomalidomide, cyclophosphamide and dexamethasone was compared with pomalidomide and dexamethasone in a randomized phase II trial involving patients with RR MM who were lenalidomide refractory and received at least two prior therapies.66 Patients received pomalidomide 4 mg days 1–21 plus weekly dexamethasone 40 mg in a 28-day cycle, with or without oral cyclophosphamide 400 mg days 1, 8 and 15. The rate of PR or better was 39% versus 65% (P=0.03) in the pomalidomide-dex and pomalidomide-cyclophosphamide-dex arms, respectively. PFS was superior with pomalidomide–cyclophosphamide-dex (9.2 versus 4.4 month, P=0.04) and there was a trend toward improvement in OS (16.4 versus 10.5 months, P=0.08).
IMiD plus anthracyclines
Thalidomide, liposomal doxorubicin, dexamethasone: The combination of thalidomide, liposomal doxorubicin and dexamethasone was evaluated in a phase II involving 50 patients with RR MM who received pegylated liposomal doxorubicin 40 mg/m2 on day 1 of a 28-day cycle, oral dexamethasone 40 mg days 1–4 and 9 –12 and thalidomide 100 mg daily. The ORR was 76%, with 26% achieving a CR. The median event-free survival was 17 months and median OS was not reached. Grade 3 non-hematologic toxicity occurred in 12% of patients, thromboembolic disease in 12% and severe infection in 16%.67
Lenalidomide, adriamycin and dexamethasone: In a phase I/II trial, the combination of lenalidomide, adriamycin, and dexamethasone was evaluated in 69 patients with RR MM and yielded an ORR of 73%.68 Frequent grade 3/4 toxicities included neutropenia, thrombocytopenia and infection.
Proteasome inhibitors plus alkylating agents
Bortezomib, oral cyclophosphamide, prednisone: The combination of i.v. bortezomib, weekly oral cyclophosphamide and alternate day prednisone was investigated in a phase I–II study (Table 2). The combination was highly active, and at the highest dose level of bortezomib 1.5 mg/m2 days 1, 8 and 15; cyclophosphamide 300 mg/m2 days 1, 8 and 15; and prednisone every other day, the ORR was 95% with an encouraging 83% 1-year PFS and 100% 1-year OS.69 Other versions of this regimen include cyclophosphamide i.v. 300–500 mg/m2 (days 1, 8, 15), bortezomib 1.3 mg/m2 (days 1, 4, 8, 11) and dexamethasone (days 1, 2, 4, 5, 8, 9, 11, 12) every 21 days.
Bortezomib, bendamustine, dexamethasone: Three phase II studies were reported, all of them with bendamustine at the doses of 70 mg/m2 on days 1 and 8 (or 4) every 28 days. The first one reported 77% OR rate (20% CR+57% PR) with a median PFS of 15.5 months.70 The second one focused on patient in first relapse. The response rates were similar with 70% OR rate but survival was slightly shorter: median PFS of 10.8 months and an OS of 23 months.71 In the third study, the survival was very comparable (PFS of 9.7 months and OS of 25.6 months) and patients with adverse cytogenetics (defined by in situ hybridization) had similar results.72 In all three studies, the toxicity was mostly hematological and generally limited.
Proteasome inhibitors plus anthracyclines
Bortezomib, doxorubicin, dexamethasone: The combination of bortezomib, doxorubicin, and dexamethasone was evaluated in 64 patients with relapsed MM (Table 2).73 Prior treatments among these patients included ASCT (58%), anthracycline (70%) and/or bortezomib (27%). PR or better was achieved in 67% of this heavily pretreated population and VGPR in 25%. Common grades 3 or 4 toxicities included thrombocytopenia, neutropenia, anemia and PN.
Bortezomib plus pegylated liposomal doxorubicin: A large-scale randomized phase III trial comparing bortezomib alone (1.3 mg/m2 i.v.) with bortezomib+pegylated liposomal doxorubicin (30 mg/m2) showed superiority of the combination in terms of median TTP (9.3 vs 6.5 months, P<0.001) and OS rate (76 vs 65%, P=0.03) although the increase in ORR was only modest (44 vs 41%, P=0.43) (Table 2).74 These important results led to regulatory approval of bortezomib plus pegylated liposomal doxorubicin in 2007.
IMiD plus proteasome inhibitors
Bortezomib, thalidomide and dexamethasone: A prospective, multicenter, phase III trial (MMVAR/IFM 2005-04 trial) compared the efficacy and safety of bortezomib plus thalidomide and dex with thalidomide and dex in 269 patients who relapsed after ASCT (Table 2).75 Median TTP was longer with bortezomib (1.3 mg/m2) plus thalidomide (200 mg/day) and dex (40 mg/day d1–d4) (19.5 vs 13.8 months, P=0.001), CR plus nCR was higher (45 vs 25%, P=0.001) and median DOR was longer (17.2 vs 13.4 months, P=0.03). Two-year OS favored the three-drug combination (71 vs 65%, P=0.093). Grade 3 PN was more frequent with the three-drug combination (29 vs 12%, P=0.001) as were the rates of grades 3 and 4 infection and thrombocytopenia.
Lenalidomide plus bortezomib: In a phase I study evaluating lenalidomide and bortezomib in RR MM, the ORR was 61%, with a CR/nCR rate of 8%.76 The most common grades 3 or 4 treatment-related toxicities were neutropenia, thrombocytopenia, anemia and leukopenia; there were no cases of grade 3/4 PN. Grades 1 or 2 PN occurred in 42% of patients and was manageable. Median OS was encouragingly at 37 months. In a subsequent phase II study of bortezomib plus lenalidomide with added dexamethasone in RR MM, the ORR was 78% and grades 3/4 toxicities included 30% neutropenia, 22% thrombocytopenia and only 3% PN (Table 1).77 Median TTP was 9.5 months, median PFS was 9.5 months and the 2-year OS rate was 55%.
Carfilzomib, lenalidomide and dexamethasone: Carfilzomib, lenalidomide and low-dose dexamethasone has shown activity in a phase II study of 52 patients with RR MM.78 It was confirmed in a phase III trial in which 792 patients were randomly assigned to carfilzomib with lenalidomide and dexamethasone (carfilzomib group) or lenalidomide and dexamethasone alone (control group).79 PFS, the primary end point, was significantly improved with carfilzomib (median, 26.3 vs 17.6 months (HR=0.69; P=0.0001). The median OS was not reached in either group at the interim analysis. The ORR were 87.1 and 66.7% in the carfilzomib and control groups, respectively (P<0.001; 31.8 and 9.3% of patients in the respective groups had a ⩾CR; 14.1 and 4.3% had a stringent CR). Encouragingly, patients in the carfilzomib group also reported superior health-related quality of life.
Adverse events of grade 3 or higher were reported in 83.7 and 80.7% of patients in the carfilzomib and control groups, respectively, with similar rates of treatment discontinuation between the arms, although rates of hypertension and venous thrombosis were higher in the carfilzomib group.
Carfilzomib, pomalidomide and dexamethasone: The combination of carfilzomib, pomalidomide and dexamethasone has been evaluated in a phase I/II study.80 The phase I portion of the study established maximum tolerated dose at carfilzomib 27 mg/m2 days 1, 2, 8, 9, 15 and 16 of a 28-day cycle; pomalidomide 4 mg days 1–21; and dexamethasone 40 mg days 1, 8, 15 and 22. In an interim analysis including data from 67 patients, the ORR was 64%, with a rate of ⩾MR of 81%. Median PFS and OS were 12.0 and 16.3 months, respectively. Grade >3 adverse events included fatigue, neutropenia, anemia, thrombocytopenia and diarrhea.
IMiD-proteasome inhibitor plus alkylating agents
Bortezomib, cyclophosphamide, thalidomide, dex: The clinical efficacy and safety of this four-drug combination was assessed in 70 patients with RR MM.81 They received at least two cycles of bortezomib (1.3 mg/m2 i.v. days 1, 4, 8 and 11), cyclophosphamide (150 mg/m2 orally days 1–4), thalidomide (50 mg/day daily) and dexamethasone (20 mg/m2 i.v. days 1, 4, 8 and 11). The ORR was very encouraging at 88%, with 46% CR, 9% VGPR and 33% PR. After a median follow-up of 12.6 months, median PFS was 14.6 months with a 3-year PFS of 14%. Median OS was 31.6 months with a 3-year OS of 47%. Grades 3 or 4 toxicities included thrombocytopenia (12%), neutropenia (4%), peripheral neuropathy (3%) and very rare cases of thrombosis (<1%).
IMiD–alkylating agent–cisplatinum–etoposide, with or without proteasome inhibitors
Dexamethasone and thalidomide plus cisplatin, doxorubicin, cyclophosphamide, etoposide (DT-PACE): DT-PACE is a salvage therapy which combines high-dose dexamethasone (40 mg orally daily for 4 days) with thalidomide at 100 mg per day and a 4-day continuous infusion of cisplatin (10 mg/m2/day), doxorubicin (10 mg/m2/day), cyclophosphamide (400 mg/m2/day) and etoposide (40 mg/m2/day). The cycles are usually administered every 4–6 weeks and 2–4 cycles are planned.82 This regimen is commonly used as last salvage treatment because it has drugs that have often not been used before, some of which penetrate the blood brain barrier. In a retrospective study, the role of DT-PACE as salvage therapy for high-risk patients with aggressive relapsed and refractory MM was analyzed. The ORR was 49% (VGPR=16%, PR=33%) with stable disease in 36%. The PFS was 5.5 months and the OS was 14 months. The toxicity was mostly hematological.83
Bortezomib, dexamethasone and thalidomide (VDT-PACE): Bortezomib in combination with DT-PACE has been evaluated in a series of 16 patients with RR MM in whom DT-PACE was administered as described previously along with i.v. bortezomib 1.0 mg/m2 days 1, 4, 8 and 11.84 The ORR was 63% and median PFS 7 months. Hematologic toxicity was common, including grade 3–4 neutropenia in 56% and febrile neutropenia in 56%.
Autologous stem cell transplantation
A number of studies have examined outcomes of second ASCT for relapsed disease in patients who had undergone ASCT at an earlier point in their management. The Royal Marsden Group analyzed 172 patients who had relapsed after a first transplant, 68% of whom received cyclophosphamide-vincristine-doxorubicin-melphalan-prednisone as salvage chemotherapy while the others received a non-specified salvage approach.85 Forty-eight of the patients subsequently received a second high-dose melphalan autograft based on suitability and patient choice, whereas 52% received a variety of other treatment approaches. There was no significant difference between these two groups in terms of event free survival (1.3 vs 0.9 years) or OS (2.9 vs 1.7 years). A relapse-free interval of over 18 months following first transplant was associated with a prolonged OS (2.9 vs 1.0 year) regardless of whether a second transplant was received although a trend toward superior OS for those receiving a second autograft was suggested (4.6 vs 2.9 years; P=0.33).
Similar outcomes were reported in a second study that assessed outcomes of 41 patients who received a second melphalan-based autograft as part of salvage chemotherapy.86 All had received preceding salvage chemotherapy but only 37% had chemosensitive disease at the time of second transplant. Although an ORR of 55% was reported following second autograft, this was associated with a treatment-related mortality of 7%. The median PFS after second autograft was 8.5 months and median OS was 20.7 months. Multivariate analysis of prognostic markers for PFS identified ⩾5 prior lines of therapy and poor response to first autograft as poor prognostic markers. Similarly, ⩾5 prior lines of therapy and TTP ⩽12 months following first autograft were predictive for a poor OS.
Several studies have suggested that a minimum interval of 18 months with a range of 1.5–3 years from first ASCT to relapse results in a second PFS of about half that time after salvage ASCT, prompting many centers to view at least 18 months as a reasonable interval after first ASCT to recommend second ASCT in relapsed patients.
In order to consider salvage second ASCT, stem cells must have been collected prior to the first ASCT or a new collection has to be done. It has been shown that mobilization after reinduction using various mobilization regimen (granulocyte colony stimulating factor only, cyclophosphamide+granulocyte colony stimulating factor or plerixafor) is feasible.87
Allogeneic SCT
Allo-SCT is a possible option for treatment of relapse in patients younger than 65–70 years, as shown in recent studies of patients relapsing after ASCT.88, 89, 90, 91, 92, 93 Myeloablative conditioning has been considered associated with excessive non-relapse mortality as shown in earlier studies both as upfront treatment and for relapsed patients.94, 95 However reducing the intensity of the conditioning before allotransplantation (RICallo) should reduce non-relapse mortality.94, 96 In recent studies non-relapse mortality with RICallo has been in the range of 10–16% in patients treated upfront after ASCT and up to 26% in relapsed/progression patients usually heavily pretreated before RICallo. This has been considered a reasonable risk based on the observation that relapse risk is reduced and PFS improved. However, the impact on OS is controversial, not only in upfront treatment, but also in RR MM. In one retrospective study of 51 heavily pretreated relapsed and refractory patients the PFS and OS at 2 years were 19 and 32%, respectively.88 Seven of these patients were in remission up to 6 years following RICallo. In a recently published prospective study, 169 progressive or relapsed patients following ASCT underwent human leukocyte antigen typing.89 Out of 75 patients with a suitable donor, 68 underwent RIC allo, either with an identical sibling donor (n=24) or an human leukocyte antigen-matched unrelated donor (n=44). Patients who did not have a donor received novel agents including lenalidomide and bortezomib, at the discretion of the treating physician. The 2-year PFS from study entry was 42% in the RIC allo group, which was significantly better than 18% in the non-RIC donor group. However there was no significant difference in OS.
Allo-SCT is frequently used as a last option, when other approaches are no longer effective. Some patients may benefit from the treatment, but earlier use of this modality in the tandem ASCT/RICallo setting may be a better option although tolerability can be challenging.97, 98 Studies of RIC allo modalities are in progress both for treatment of patients with relapsed disease and for the upfront treatment of high-risk patients. Such studies should be compared with the best options using new drug combinations, like bortezomib plus thalidomide and dex which showed encouraging results in a recent prospective European Blood and Marrow Transplantation (EBMT) trial of patients relapsing after ASCT.75 Such studies may help better define the role for allogeneic SCT in the treatment of RR MM.
Specific management recommendations
First relapse
-
Clinical trial participation should be offered if an appropriate study is available.
-
In patients who experience a high quality, prolonged response with minimal toxicity to initial therapy, re-treatment can be considered if they have obtained at least a 6–9 months treatment-free interval. The alternative is to change to a different class of drug and reserve the original treatment scheme for second relapse.
-
We recommend ASCT be considered for eligible patients who have not had an ASCT in first line, or had an ASCT with long response duration.
-
We advise patients who experience suboptimal response or significant toxicity with initial therapy receive a regimen that incorporates at least one agent to which the patient has not been previously exposed.
-
There is no specific preference between regimens that contain lenalidomide, bortezomib, or both drugs; the choice of regimen should be based on response and tolerability to immediate prior therapy, current clinical status and co-morbidities of the patient, and access and availability of agents.
-
We suggest patients with poor prognosis disease characteristics at time of relapse be considered for three- or four-drug regimens while those with indolent disease characteristics be considered for one- or two-drug combinations, recognizing that randomized studies are necessary to validate these recommendations.
-
We recommend patients with poor prognosis disease characteristics be treated until disease progression recognizing the risk of rapid relapse in the absence of sustained exposure to chemotherapy. Treatment-free intervals can be considered in patients with indolent disease characteristics based on discretion of the treating physician and preferences of the patient.
-
We recommend carfilzomib and pomalidomide be primarily used for patients refractory and/or intolerant to both bortezomib and lenalidomide.
-
We recommend allogeneic stem cell transplantation be discussed in eligible patients with poor prognostic features, preferably in the context of a clinical trial.
Second relapse and beyond
-
Clinical trial participation should be offered if an appropriate study is available.
-
We recommend patients in second relapse or beyond receive a salvage regimen incorporating at least one agent to which there has not been prior evidence of resistance or intolerability.
-
We suggest patients with aggressive disease characteristics at time of relapse be considered for three- or four-drug regimens while those with indolent disease characteristics be considered for one-or two-drug regimens, and here in cytotoxic agents can be added to appropriate proteasome inhibitor and IMiD-based combinations.
-
We recommend patients in second relapse and beyond receive ongoing therapy until the particular regimen is no longer tolerated or there is evidence of disease progression, at which time an alternative regimen should be chosen
Regimens that can be employed in first or subsequent stages of relapse are summarized in Table 4 with level of evidence and grade of recommendation (http://www.cebm.net/?o=1025) corresponding to each regimen. However, with increasing episodes of relapse, less information from randomized trials is available making evidence-based suggestions difficult. Hence, the suggestions made are based mainly on expert experience.
Relapse and refractory to lenalidomide and bortezomib
In 2011, a retrospective study conducted on behalf of the International Myeloma Working Group established that patients with relapsed MM, who were refractory to bortezomib and refractory to or ineligible to receive treatment with an IMiD (thalidomide or lenalidomide), had a OS and event-free survival of 9 and 5 months, respectively.16 Treatment options in these patients are limited. Carfilzomib and pomalidomide, in conjunction with dexamethasone, have shown some efficacy in patients refractory to bortezomib and lenalidomide, respectively.
-
We recommend a regimen containing carfilzomib or pomalidomide be considered for patients with myeloma relapsed and refractory to lenalidomide and bortezomib.
-
Carfilzomib should preferably be used in combination with lenalidomide and low-dose dexamethasone consistent with the results of the ASPIRE trial.79 Similarly, pomalidomide is preferably used in combination with low-dose dexamethasone, and can be combined with other agents, including bortezomib. Besides these regimens, there is no specific preference between other regimens that contain pomalidomide, carfilzomib or both drugs in this setting; the choice of regimen should be based on response and tolerability to immediate prior therapy, current clinical status and co-morbidities of the patient, as well as access and availability of agents.
-
Panobinostat in combination with bortezomib and dexamethasone can be considered for patients with myeloma whom are relapsed and refractory to lenalidomide and bortezomib, or similar combinations.
Relapse and autotransplantation
-
We recommend consideration of a second autograft for salvage in patients who have a minimum TTP of at least 18 months or more after first ASCT.
-
In patients who have not undergone an ASCT at first response, we recommend consideration at the time of first relapse.
Relapse and allogeneic transplantation
-
We recommend consideration of an Allo-SCT largely in the context of clinical trials, particularly focusing on high-risk patients.
-
Considering lack of consistent data indicating superiority of Allo-SCT over tandem auto SCT and concerns for treatment-related mortality despite RIC as well as rates of graft-versus-host disease in studies so far, consideration of an Allo-SCT within or outside a clinical trial should be with appropriate informed consent of the patient outlining the risks of treatment-related mortality and graft-versus-host disease.
New agents and future directions in relapsed myeloma
Numerous novel compounds are undergoing evaluation in RR MM; this topic was the focus of a recent report from the International Myeloma Working Group.99 Monoclonal antibody therapy targeting plasma cell antigens including CS1 glycoprotein, CD38 and CD138 is showing promising results. The anti-CS1 monoclonal antibody, elotuzumab,100 the anti-CD38 antibodies, daratumumab101 and SAR650984, and the CD138 conjugate BT062 comprised of the anti-CD138 chimerized MAb and the cytotoxic agent DM4102 are examples of monoclonal antibodies currently being investigated, with elotuzumab in combination with lenalidomide and dexamethasone being particularly active and well tolerated. Daratumumab is especially potent and highly effective in relapsed and refractory myeloma, both as monotherapy and in combination. A summary of monoclonal antibodies in development in MM is shown in Table 5.
The pan-histone deacetylase inhibitors romidepsin,103 as well as the HDAC6 specific inhibitor, ACY 1215,104 have demonstrated significant anti-MM effect in preclinical studies, with the latter now undergoing evaluation in combination with lenalidomide, pomalidomide and bortezomib, in various settings, and promising activity as well as favorable tolerability has been seen. Prior studies with vorinostat have also shown promise but a large randomized trial in combination with bortezomib demonstrated response rate advantages with only limited, although statistically significant, PFS improvement.105, 106
Following promising early-phase trials of the agent in relapsed and refractory MM,107, 108 perifosine, a small-molecule inhibitor of the phosphatidylinositol 3-kinase (PI3-K/AKT) pathway was assessed in a phase III study in combination with bortezomib and dexamethasone versus bortezomib/dexamethasone, but this trial had to be closed prematurely because of resource limitations, slow accrual and no substantial difference in outcome seen on an interim analysis, although safety was favorable. Other studies of small molecule inhibitors in this category are ongoing.
The kinesin spindle protein inhibitor, ARRY-520, the cyclin-dependent kinase (CDK) inhibitor, dinaciclib, the CRM1 inhibitor selinexor, and another monoclonal antibody targeting B-cell activating factor (BAFF), tabalumab are examples of next generation novel agents that have preliminarily shown encouraging activity with ongoing trials in RR MM.109, 110, 111
Finally, with continued improvement in prevention and treatment of graft versus host disease and treatment-related mortality using a variety of agents, the role of allogeneic stem cell transplant may be revisited in the future in selected high-risk patients with RR MM, as well as recent strong interest in other immuno-oncologic strategies, including checkpoint inhibitors, vaccines and CAR-T therapy.
Conclusion
The management of relapsed MM requires a systematic approach based on several characteristic features of the patient. Prior treatment, including degree and depth of response, as well as treatment-related toxicities is important determinants in choosing subsequent treatment options. Risk stratification at the time of relapse based on chromosomal abnormalities and gene expression profiling is an emerging field. While OS of patients with MM has improved, the survival of patients progressing after treatment with the IMiDs and bortezomib remains dismal16 underscoring the importance of continued efforts to better understand disease biology at the time of relapse and translate this into viable and effective treatment options and rational combinations to further improve patient outcome.112, 113, 114 The regulatory approval of multiple novel agents for relapsed and RR MM in 2015—panobinostat in combination with bortezomib and dexamethasone, pomalidomide plus dexamethasone, carfilzomib in combination with lenalidomide and dexamethasone, and most recently daratumumab (as the first monoclonal antibody), followed by elotuzumab in combination with lenalidomide and dexamethasone, and the oral proteasome inhibitor ixazomib in combination with lenalidomide and dexamethasone—represent a record for approvals in one year. These therefore are critical steps toward this goal and reflect real hope for the future in this otherwise incurable disease.
References
Mckenna RWKR, Kuehl WM, Grogan TM, Harris NL, Coupland RW. Plasma cell neoplasms. In: Swerdlow SHCE, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW (eds). WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer: Lyon, 2008, pp 200–213..
Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010; 11: 29–37.
Cavo M, Tacchetti P, Patriarca F, Petrucci MT, Pantani L, Galli M et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet 2010; 376: 2075–2085.
Harousseau JL, Attal M, Avet-Loiseau H, Marit G, Caillot D, Mohty M et al. Bortezomib plus dexamethasone is superior to vincristine plus doxorubicin plus dexamethasone as induction treatment prior to autologous stem-cell transplantation in newly diagnosed multiple myeloma: results of the IFM 2005-01 phase III trial. J Clin Oncol 2010; 28: 4621–4629.
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med 2008; 359: 906–917.
Rajkumar SV, Rosinol L, Hussein M, Catalano J, Jedrzejczak W, Lucy L et al. Multicenter, randomized, double-blind, placebo-controlled study of thalidomide plus dexamethasone compared with dexamethasone as initial therapy for newly diagnosed multiple myeloma. J Clin Oncol 2008; 26: 2171–2177.
Attal M, Harousseau JL, Stoppa AM, Sotto JJ, Fuzibet JG, Rossi JF et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Francais du Myelome. N Engl J Med 1996; 335: 91–97.
Child JA, Morgan GJ, Davies FE, Owen RG, Bell SE, Hawkins K et al. High-dose chemotherapy with hematopoietic stem-cell rescue for multiple myeloma. N Engl J Med 2003; 348: 1875–1883.
Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG et al. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med 2003; 349: 2495–2502.
Cavo M, Pantani L, Petrucci MT, Patriarca F, Zamagni E, Donnarumma D et al. Bortezomib-thalidomide-dexamethasone is superior to thalidomide-dexamethasone as consolidation therapy after autologous hematopoietic stem cell transplantation in patients with newly diagnosed multiple myeloma. Blood 2012; 120: 9–19.
Ladetto M, Pagliano G, Ferrero S, Cavallo F, Drandi D, Santo L et al. Major tumor shrinking and persistent molecular remissions after consolidation with bortezomib, thalidomide, and dexamethasone in patients with autografted myeloma. J Clin Oncol 2010; 28: 2077–2084.
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Venner CP, Connors JM, Sutherland HJ, Shepherd JD, Hamata L, Mourad YA et al. Novel agents improve survival of transplant patients with multiple myeloma including those with high-risk disease defined by early relapse (<12 months). Leuk Lymphoma 2011; 52: 34–41.
Rajkumar SV, Harousseau JL, Durie B, Anderson KC, Dimopoulos M, Kyle R et al. Consensus recommendations for the uniform reporting of clinical trials: report of the International Myeloma Workshop Consensus Panel 1. Blood 2011; 117: 4691–4695.
Chim CS, Lie AK, Chan EY, Leung YY, Cheung SC, Chan SY et al. A staged approach with vincristine, adriamycin, and dexamethasone followed by bortezomib, thalidomide, and dexamethasone before autologous hematopoietic stem cell transplantation in the treatment of newly diagnosed multiple myeloma. Ann Hematol 2010; 89: 1019–1027.
Kumar SK, Lee JH, Lahuerta JJ, Morgan G, Richardson PG, Crowley J et al. Risk of progression and survival in multiple myeloma relapsing after therapy with IMiDs and bortezomib: a multicenter international myeloma working group study. Leukemia 2012; 26: 149–157.
Avet-Loiseau H, Soulier J, Fermand JP, Yakoub-Agha I, Attal M, Hulin C et al. Impact of high-risk cytogenetics and prior therapy on outcomes in patients with advanced relapsed or refractory multiple myeloma treated with lenalidomide plus dexamethasone. Leukemia 2010; 24: 623–628.
Dimopoulos MA, Kastritis E, Christoulas D, Migkou M, Gavriatopoulou M, Gkotzamanidou M et al. Treatment of patients with relapsed/refractory multiple myeloma with lenalidomide and dexamethasone with or without bortezomib: prospective evaluation of the impact of cytogenetic abnormalities and of previous therapies. Leukemia 2010; 24: 1769–1778.
Tovar N, de Larrea CF, Arostegui JI, Cibeira MT, Rosinol L, Rovira M et al. Natural history and prognostic impact of oligoclonal humoral response in patients with multiple myeloma after autologous stem cell transplantation: long-term results from a single institution. Haematologica 2013; 98: 1142–1146.
Conner TM, Doan QD, Walters IB, LeBlanc AL, Beveridge RA . An observational, retrospective analysis of retreatment with bortezomib for multiple myeloma. Clin Lymphoma Myeloma 2008; 8: 140–145.
Hrusovsky I, Emmerich B, von Rohr A, Voegeli J, Taverna C, Olie RA et al. Bortezomib retreatment in relapsed multiple myeloma—results from a retrospective multicentre survey in Germany and Switzerland. Oncology 2010; 79: 247–254.
Singhal S, Mehta J, Desikan R, Ayers D, Roberson P, Eddlemon P et al. Antitumor activity of thalidomide in refractory multiple myeloma. N Engl J Med 1999; 341: 1565–1571.
Barlogie B, Desikan R, Eddlemon P, Spencer T, Zeldis J, Munshi N et al. Extended survival in advanced and refractory multiple myeloma after single-agent thalidomide: identification of prognostic factors in a phase 2 study of 169 patients. Blood 2001; 98: 492–494.
Dimopoulos MA, Anagnostopoulos A, Weber D . Treatment of plasma cell dyscrasias with thalidomide and its derivatives. J Clin Oncol 2003; 21: 4444–4454.
Glasmacher A, Hahn C, Hoffmann F, Naumann R, Goldschmidt H, von Lilienfeld-Toal M et al. A systematic review of phase-II trials of thalidomide monotherapy in patients with relapsed or refractory multiple myeloma. Br J Haematol 2006; 132: 584–593.
Kumar S, Gertz MA, Dispenzieri A, Lacy MQ, Geyer SM, Iturria NL et al. Response rate, durability of response, and survival after thalidomide therapy for relapsed multiple myeloma. Mayo Clin Proc 2003; 78: 34–39.
Richardson P, Schlossman R, Jagannath S, Alsina M, Desikan R, Blood E et al. Thalidomide for patients with relapsed multiple myeloma after high-dose chemotherapy and stem cell transplantation: results of an open-label multicenter phase 2 study of efficacy, toxicity, and biological activity. Mayo Clin Proc 2004; 79: 875–882.
Mileshkin L, Biagi JJ, Mitchell P, Underhill C, Grigg A, Bell R et al. Multicenter phase 2 trial of thalidomide in relapsed/refractory multiple myeloma: adverse prognostic impact of advanced age. Blood 2003; 102: 69–77.
van Rhee F, Dhodapkar M, Shaughnessy JD Jr, Anaissie E, Siegel D, Hoering A et al. First thalidomide clinical trial in multiple myeloma: a decade. Blood 2008; 112: 1035–1038.
Grover JK, Uppal G, Raina V . The adverse effects of thalidomide in relapsed and refractory patients of multiple myeloma. Ann Oncol 2002; 13: 1636–1640.
Dimopoulos MA, Eleutherakis-Papaiakovou V . Adverse effects of thalidomide administration in patients with neoplastic diseases. Am J Med 2004; 117: 508–515.
von Lilienfeld-Toal M, Hahn-Ast C, Furkert K, Hoffmann F, Naumann R, Bargou R et al. A systematic review of phase II trials of thalidomide/dexamethasone combination therapy in patients with relapsed or refractory multiple myeloma. Eur J Haematol 2008; 81: 247–252.
Palumbo A, Rajkumar SV, Dimopoulos MA, Richardson PG, San Miguel J, Barlogie B et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia 2008; 22: 414–423.
Richardson PG, Blood E, Mitsiades CS, Jagannath S, Zeldenrust SR, Alsina M et al. A randomized phase 2 study of lenalidomide therapy for patients with relapsed or relapsed and refractory multiple myeloma. Blood 2006; 108: 3458–3464.
Richardson P, Jagannath S, Hussein M, Berenson J, Singhal S, Irwin D et al. Safety and efficacy of single-agent lenalidomide in patients with relapsed and refractory multiple myeloma. Blood 2009; 114: 772–778.
Dimopoulos M, Spencer A, Attal M, Prince HM, Harousseau JL, Dmoszynska A et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 2007; 357: 2123–2132.
Weber DM, Chen C, Niesvizky R, Wang M, Belch A, Stadtmauer EA et al. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med 2007; 357: 2133–2142.
Schey SA, Fields P, Bartlett JB, Clarke IA, Ashan G, Knight RD et al. Phase I study of an immunomodulatory thalidomide analog, CC-4047, in relapsed or refractory multiple myeloma. J Clin Oncol 2004; 22: 3269–3276.
Richardson PG, Siegel D, Baz R, Kelley SL, Munshi NC, Laubach J et al. Phase 1 study of pomalidomide MTD, safety, and efficacy in patients with refractory multiple myeloma who have received lenalidomide and bortezomib. Blood 2013; 121: 1961–1967.
San Miguel J, Weisel K, Moreau P, Lacy M, Song K, Delforge M et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): a randomised, open-label, phase 3 trial. Lancet Oncol 2013; 14: 1055–1066.
Leleu X, Karlin L, Macro M, Hulin C, Garderet L, Roussel M et al. Pomalidomide plus low-dose dexamethasone in relapsed or refractory multiple myeloma (RRMM) with deletion (del)17p and/or translocation t(4;14). Blood 2013; 122: 689.
Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med 2003; 348: 2609–2617.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med 2005; 352: 2487–2498.
Sagaster V, Ludwig H, Kaufmann H, Odelga V, Zojer N, Ackermann J et al. Bortezomib in relapsed multiple myeloma: response rates and duration of response are independent of a chromosome 13q-deletion. Leukemia 2007; 21: 164–168.
Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol 2011; 12: 431–440.
Jagannath S, Richardson PG, Barlogie B, Berenson JR, Singhal S, Irwin D et al. Bortezomib in combination with dexamethasone for the treatment of patients with relapsed and/or refractory multiple myeloma with less than optimal response to bortezomib alone. Haematologica 2006; 91: 929–934.
Mikhael JR, Belch AR, Prince HM, Lucio MN, Maiolino A, Corso A et al. High response rate to bortezomib with or without dexamethasone in patients with relapsed or refractory multiple myeloma: results of a global phase 3b expanded access program. Br J Haematol 2009; 144: 169–175.
Dimopoulos MA, Beksac M, Benboubker L, Roddie H, Allietta N, Broer E et al. Phase II study of bortezomib-dexamethasone alone or with added cyclophosphamide or lenalidomide for sub-optimal response as second-line treatment for patients with multiple myeloma. Haematologica 2013; 98: 1264–1272.
Demo SD, Kirk CJ, Aujay MA, Buchholz TJ, Dajee M, Ho MN et al. Antitumor activity of PR-171, a novel irreversible inhibitor of the proteasome. Cancer Res 2007; 67: 6383–6391.
Siegel DS, Martin T, Wang M, Vij R, Jakubowiak AJ, Lonial S et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood 2012; 120: 2817–2825.
Vij R, Wang M, Kaufman JL, Lonial S, Jakubowiak AJ, Stewart AK et al. An open-label, single-arm, phase 2 (PX-171-004) study of single-agent carfilzomib in bortezomib-naive patients with relapsed and/or refractory multiple myeloma. Blood 2012; 119: 5661–5670.
Knop S, Straka C, Haen M, Schwedes R, Hebart H, Einsele H . The efficacy and toxicity of bendamustine in recurrent multiple myeloma after high-dose chemotherapy. Haematologica 2005; 90: 1287–1288.
Damaj G, Malard F, Hulin C, Caillot D, Garidi R, Royer B et al. Efficacy of bendamustine in relapsed/refractory myeloma patients: results from the French compassionate use program. Leuk Lymphoma 2012; 53: 632–634.
Richardson PG, Schlossman RL, Alsina M, Weber DM, Coutre SE, Gasparetto C et al. Time to event analyses in PANORAMA 2: a phase 2 study of panobinostat, bortezomib, and dexamethasone in patients with relapsed and bortezomib-refractory multiple myeloma. Blood 2013; 122: 1970.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol 2014; 15: 1195–1206.
Offidani M, Corvatta L, Marconi M, Olivieri A, Catarini M, Mele A et al. Thalidomide plus oral melphalan compared with thalidomide alone for advanced multiple myeloma. Hematol J 2004; 5: 312–317.
Kyriakou C, Thomson K, D'Sa S, Flory A, Hanslip J, Goldstone AH et al. Low-dose thalidomide in combination with oral weekly cyclophosphamide and pulsed dexamethasone is a well tolerated and effective regimen in patients with relapsed and refractory multiple myeloma. Br J Haematol 2005; 129: 763–770.
Dimopoulos MA, Hamilos G, Zomas A, Gika D, Efstathiou E, Grigoraki V et al. Pulsed cyclophosphamide, thalidomide and dexamethasone: an oral regimen for previously treated patients with multiple myeloma. Hematol J 2004; 5: 112–117.
Schey SA, Morgan GJ, Ramasamy K, Hazel B, Ladon D, Corderoy S et al. The addition of cyclophosphamide to lenalidomide and dexamethasone in multiply relapsed/refractory myeloma patients; a phase I/II study. Br J Haematol 2010; 150: 326–333.
Morgan GJ, Schey SA, Wu P, Srikanth M, Phekoo KJ, Jenner M et al. Lenalidomide (Revlimid), in combination with cyclophosphamide and dexamethasone (RCD), is an effective and tolerated regimen for myeloma patients. Br J Haematol 2007; 137: 268–269.
van de Donk NW, Wittebol S, Minnema MC, Lokhorst HM . Lenalidomide (Revlimid) combined with continuous oral cyclophosphamide (endoxan) and prednisone (REP) is effective in lenalidomide/dexamethasone-refractory myeloma. Br J Haematol 2010; 148: 335–337.
Nijhof IS, Zweegman S, Levin M-D, Koene HR, Beeker A, Bloem AC et al. Phase 1/2 trial of lenalidomide in combination with cyclophosphamide and prednisone (REP) in patients with lenalidomide-refractory multiple myeloma (REPEAT-study). Blood 2013; 122: 287.
Palumbo A, Larocca A, Falco P, Sanpaolo G, Falcone AP, Federico V et al. Lenalidomide, melphalan, prednisone and thalidomide (RMPT) for relapsed/refractory multiple myeloma. Leukemia 2010; 24: 1037–1042.
Lentzsch S, O'Sullivan A, Kennedy RC, Abbas M, Dai L, Pregja SL et al. Combination of bendamustine, lenalidomide, and dexamethasone (BLD) in patients with relapsed or refractory multiple myeloma is feasible and highly effective: results of phase 1/2 open-label, dose escalation study. Blood 2012; 119: 4608–4613.
Ponisch W, Heyn S, Beck J, Wagner I, Mohren M, Hoffmann FA et al. Lenalidomide, bendamustine and prednisolone exhibits a favourable safety and efficacy profile in relapsed or refractory multiple myeloma: final results of a phase 1 clinical trial OSHO - #077. Br J Haematol 2013; 162: 202–209.
Baz R, Martin TG, Alsina M, Shain KH, Cho HJ, Wolf JL et al. Pomalidomide, cyclophosphamide, and dexamethasone is superior to pomalidomide and dexamethasone in relapsed and refractory myeloma: results of a multicenter randomized phase II study. Blood 2014; 124: 303–303.
Offidani M, Corvatta L, Marconi M, Visani G, Alesiani F, Brunori M et al. Low-dose thalidomide with pegylated liposomal doxorubicin and high-dose dexamethasone for relapsed/refractory multiple myeloma: a prospective, multicenter, phase II study. Haematologica 2006; 91: 133–136.
Knop S, Gerecke C, Liebisch P, Topp MS, Platzbecker U, Sezer O et al. Lenalidomide, adriamycin, and dexamethasone (RAD) in patients with relapsed and refractory multiple myeloma: a report from the German Myeloma Study Group DSMM (Deutsche Studiengruppe Multiples Myelom). Blood 2009; 113: 4137–4143.
Reece DE, Rodriguez GP, Chen C, Trudel S, Kukreti V, Mikhael J et al. Phase I-II trial of bortezomib plus oral cyclophosphamide and prednisone in relapsed and refractory multiple myeloma. J Clin Oncol 2008; 26: 4777–4783.
Offidani M, Corvatta L, Maracci L, Liberati AM, Ballanti S, Attolico I et al. Efficacy and tolerability of bendamustine, bortezomib and dexamethasone in patients with relapsed-refractory multiple myeloma: a phase II study. Blood Cancer J 2013; 3: e162.
Rodon P, Hulin C, Pegourie B, Tiab M, Anglaret B, Benboubker L et al Bendamustine, bortezomib and dexamethasone (BVD) in Elderly Patients with Multiple Myeloma in First Relapse: Updated Results of the Intergroupe Francophone Du Myelome (IFM) 2009-01 Trial. ASH Annual Meeting Abstracts, Vol. 120, 2012, p 4044.
Ludwig H, Kasparu H, Leitgeb C, Rauch E, Linkesch W, Zojer N et al. Bendamustine-bortezomib-dexamethasone is an active and well-tolerated regimen in patients with relapsed or refractory multiple myeloma. Blood 2014; 123: 985–991.
Palumbo A, Gay F, Bringhen S, Falcone A, Pescosta N, Callea V et al. Bortezomib, doxorubicin and dexamethasone in advanced multiple myeloma. Ann Oncol 2008; 19: 1160–1165.
Orlowski RZ, Nagler A, Sonneveld P, Blade J, Hajek R, Spencer A et al. Randomized phase III study of pegylated liposomal doxorubicin plus bortezomib compared with bortezomib alone in relapsed or refractory multiple myeloma: combination therapy improves time to progression. J Clin Oncol 2007; 25: 3892–3901.
Garderet L, Iacobelli S, Moreau P, Dib M, Lafon I, Niederwieser D et al. Superiority of the triple combination of bortezomib-thalidomide-dexamethasone over the dual combination of thalidomide-dexamethasone in patients with multiple myeloma progressing or relapsing after autologous transplantation: the MMVAR/IFM 2005-04 Randomized Phase III Trial from the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 2012; 30: 2475–2482.
Richardson PG, Weller E, Jagannath S, Avigan DE, Alsina M, Schlossman RL et al. Multicenter, phase I, dose-escalation trial of lenalidomide plus bortezomib for relapsed and relapsed/refractory multiple myeloma. J Clin Oncol 2009; 27: 5713–5719.
Richardson PG, Jagannath S, Jakubowiak AJ, Lonial S, Raje N, Alsina M et al Phase II Trial of Lenalidomide, Bortezomib, and Dexamethasone In Patients (pts) with Relapsed and Relapsed/Refractory Multiple Myeloma (MM): Updated Efficacy and Safety Data After >2 Years of Follow-up. ASH Annual Meeting Abstracts. Vol. 116, 2010, p. 3049.
Wang M, Martin T, Bensinger W, Alsina M, Siegel DS, Kavalerchik E et al. Phase 2 dose-expansion study (PX-171-006) of carfilzomib, lenalidomide, and low-dose dexamethasone in relapsed or progressive multiple myeloma. Blood 2013; 122: 3122–3128.
Stewart AK, Rajkumar SV, Dimopoulos MA, Masszi T, Spicka I, Oriol A et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med 2015; 372: 142–152.
Shah JJ, Stadtmauer EA, Abonour R, Cohen AD, Bensinger W, Gasparetto C et al. Phase I/II dose expansion of a multi-center trial of carfilzomib and pomalidomide with dexamethasone (Car-Pom-d) in patients with relapsed/refractory multiple myeloma. Blood 2013; 122: 690.
Kim YK, Sohn SK, Lee JH, Yang DH, Moon JH, Ahn JS et al. Clinical efficacy of a bortezomib, cyclophosphamide, thalidomide, and dexamethasone (Vel-CTD) regimen in patients with relapsed or refractory multiple myeloma: a phase II study. Ann Hematol 2010; 89: 475–482.
Lee CK, Barlogie B, Munshi N, Zangari M, Fassas A, Jacobson J et al. DTPACE: an effective, novel combination chemotherapy with thalidomide for previously treated patients with myeloma. J Clin Oncol 2003; 21: 2732–2739.
Gerrie AS, Mikhael JR, Cheng L, Jiang H, Kukreti V, Panzarella T et al. D(T)PACE as salvage therapy for aggressive or refractory multiple myeloma. Br J Haematol 2013; 161: 802–810.
Buda G, Orciuolo E, Galimberti S, Ghio F, Petrini M . VDTPACE as salvage therapy for heavily pretreated MM patients. Blood 2013; 122: 5377–5377.
Alvares CL, Davies FE, Horton C, Patel G, Powles R, Morgan GJ . The role of second autografts in the management of myeloma at first relapse. Haematologica 2006; 91: 141–142.
Olin RL, Vogl DT, Porter DL, Luger SM, Schuster SJ, Tsai DE et al. Second auto-SCT is safe and effective salvage therapy for relapsed multiple myeloma. Bone Marrow Transplant 2009; 43: 417–422.
Lemieux E, Hulin C, Caillot D, Tardy S, Dorvaux V, Michel J et al. Autologous stem cell transplantation: an effective salvage therapy in multiple myeloma. Biol Blood Marrow Transplant 2013; 19: 445–449.
Efebera YA, Qureshi SR, Cole SM, Saliba R, Pelosini M, Patel RM et al. Reduced-intensity allogeneic hematopoietic stem cell transplantation for relapsed multiple myeloma. Biol Blood Marrow Transplant 2010; 16: 1122–1129.
Patriarca F, Einsele H, Spina F, Bruno B, Isola M, Nozzoli C et al. Allogeneic stem cell transplantation in multiple myeloma relapsed after autograft: a multicenter retrospective study based on donor availability. Biol Blood Marrow Transplant 2012; 18: 617–626.
de Lavallade H, El-Cheikh J, Faucher C, Furst S, Stoppa AM, Coso D et al. Reduced-intensity conditioning allogeneic SCT as salvage treatment for relapsed multiple myeloma. Bone Marrow Transplant 2008; 41: 953–960.
Shimoni A, Hardan I, Ayuk F, Schilling G, Atanackovic D, Zeller W et al. Allogenic hematopoietic stem-cell transplantation with reduced-intensity conditioning in patients with refractory and recurrent multiple myeloma: long-term follow-up. Cancer 2010; 116: 3621–3630.
Kroger N, Shimoni A, Schilling G, Schwerdtfeger R, Bornhauser M, Nagler A et al. Unrelated stem cell transplantation after reduced intensity conditioning for patients with multiple myeloma relapsing after autologous transplantation. Br J Haematol 2010; 148: 323–331.
Qazilbash MH, Saliba R, De Lima M, Hosing C, Couriel D, Aleman A et al. Second autologous or allogeneic transplantation after the failure of first autograft in patients with multiple myeloma. Cancer 2006; 106: 1084–1089.
Crawley C, Iacobelli S, Bjorkstrand B, Apperley JF, Niederwieser D, Gahrton G . Reduced-intensity conditioning for myeloma: lower nonrelapse mortality but higher relapse rates compared with myeloablative conditioning. Blood 2007; 109: 3588–3594.
Gahrton G, Tura S, Ljungman P, Belanger C, Brandt L, Cavo M et al. Allogeneic bone marrow transplantation in multiple myeloma. European Group for Bone Marrow Transplantation. N Engl J Med 1991; 325: 1267–1273.
Maloney DG, Molina AJ, Sahebi F, Stockerl-Goldstein KE, Sandmaier BM, Bensinger W et al. Allografting with nonmyeloablative conditioning following cytoreductive autografts for the treatment of patients with multiple myeloma. Blood 2003; 102: 3447–3454.
Bruno B, Rotta M, Patriarca F, Mordini N, Allione B, Carnevale-Schianca F et al. A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med 2007; 356: 1110–1120.
Bjorkstrand B, Iacobelli S, Hegenbart U, Gruber A, Greinix H, Volin L et al. Tandem autologous/reduced-intensity conditioning allogeneic stem-cell transplantation versus autologous transplantation in myeloma: long-term follow-up. J Clin Oncol 2011; 29: 3016–3022.
Ocio EM, Richardson PG, Rajkumar SV, Palumbo A, Mateos MV, Orlowski R et al. New drugs and novel mechanisms of action in multiple myeloma in 2013: a report from the International Myeloma Working Group (IMWG). Leukemia 2014; 28: 525–542.
Lonial S, Vij R, Harousseau JL, Facon T, Moreau P, Mazumder A et al. Elotuzumab in combination with lenalidomide and low-dose dexamethasone in relapsed or refractory multiple myeloma. J Clin Oncol 2012; 30: 1953–1959.
Plesner T, Lokhorst H, Gimsing P, Nahi H, Lisby S, Richardson PG Daratumumab, a CD38 Monoclonal Antibody in Patients with Multiple Myeloma - Data From a Dose-Escalation Phase I/II Study. ASH Annual Meeting Abstracts, Vol. 20, 2012, p 73.
Heffner LT, Jagannath S, Zimmerman TM, Lee KP, Rosenblatt J, Lonial S et al BT062, an Antibody-Drug Conjugate Directed Against CD138, Given Weekly for 3 Weeks in Each 4 Week Cycle: Safety and Further Evidence of Clinical Activity. ASH Annual Meeting Abstracts. Vol. 120, 2012, p 4042.
Harrison SJ, Quach H, Link E, Seymour JF, Ritchie DS, Ruell S et al. A high rate of durable responses with romidepsin, bortezomib, and dexamethasone in relapsed or refractory multiple myeloma. Blood 2011; 118: 6274–6283.
Raje N, Hari PN, Vogl DT, Jagannath S, Orlowski RZ, Supko JG et al Rocilinostat (ACY-1215), a Selective HDAC6 Inhibitor, Alone and in Combination with Bortezomib in Multiple Myeloma: Preliminary Results From the First-in-Humans Phase I/II Study. ASH Annual Meeting Abstracts, Vol. 120, 2012, p 4061.
Weber DM, Graef T, Hussein M, Sobecks RM, Schiller GJ, Lupinacci L et al. Phase I trial of vorinostat combined with bortezomib for the treatment of relapsing and/or refractory multiple myeloma. Clin Lymphoma Myeloma Leuk 2012; 12: 319–324.
Cea M, Cagnetta A, Gobbi M, Patrone F, Richardson PG, Hideshima T et al. New insights into the treatment of multiple myeloma with histone deacetylase inhibitors. Curr Pharm Des 2013; 19: 734–744.
Jakubowiak AJ, Richardson PG, Zimmerman T, Alsina M, Kaufman JL, Kandarpa M et al. Perifosine plus lenalidomide and dexamethasone in relapsed and relapsed/refractory multiple myeloma: a Phase I Multiple Myeloma Research Consortium study. Br J Haematol 2012; 158: 472–480.
Richardson PG, Wolf J, Jakubowiak A, Zonder J, Lonial S, Irwin D et al. Perifosine plus bortezomib and dexamethasone in patients with relapsed/refractory multiple myeloma previously treated with bortezomib: results of a multicenter phase I/II trial. J Clin Oncol 2011; 29: 4243–4249.
Shah JJ, Zonder JA, Cohen A, Bensinger W, Kaufman JL, Orlowski RZ et al The Novel KSP Inhibitor ARRY-520 Is Active Both with and without Low-Dose Dexamethasone in Patients with Multiple Myeloma Refractory to Bortezomib and Lenalidomide: Results From a Phase 2 Study. ASH Annual Meeting Abstracts, 120, 2012, p 449.
Kumar SK, LaPlant BR, Chng WJ, Zonder JA, Callander N, Roy V et al Phase 1/2 Trial of a Novel CDK Inhibitor Dinaciclib (SCH727965) in Patients with Relapsed Multiple Myeloma Demonstrates Encouraging Single Agent Activity. ASH Annual Meeting Abstracts, Vol. 120, 2012, p 76.
Raje N, Faber EA Jr., Richardson PG, Schiller GJ, Hohl RJ, Cohen AD et al Phase 1 Study of Tabalumab, a Human Anti-BAFF Antibody and Bortezomib in Patients with Previously-Treated Multiple Myeloma. ASH Annual Meeting Abstracts Vol. 120, 2012, p 447.
Richardson PG, Mitsiades C, Schlossman R, Munshi N, Anderson K . New Drugs for Myeloma. The Oncologist 2007; 12: 664–689.
Lonial S, Mitsiades CS, Richardson PG . Treatment options for relapsed and refractory multiple myeloma. Clin Cancer Res 2011; 17: 1264–1277.
Laubach JP, Voorhees PM, Hassoun H, Jakubowiak A, Lonial S, Richardson PG . Current strategies for treatment of relapsed/refractory multiple myeloma. Expert Rev Hematol 2014; 7: 97–111.
Smetana J, Berankova K, Zaoralova R, Nemec P, Greslikova H, Kupska R et al. Gain(1)(q21) is an unfavorable genetic prognostic factor for patients with relapsed multiple myeloma treated with thalidomide but not for those treated with bortezomib. Clin Lymphoma Myeloma Leuk 2013; 13: 123–130.
Jakubowiak AJ, Siegel DS, Martin T, Wang M, Vij R, Lonial S et al. Treatment outcomes in patients with relapsed and refractory multiple myeloma and high-risk cytogenetics receiving single-agent carfilzomib in the PX-171-003-A1 study. Leukemia 2013; 27: 2351–2356.
Reece D, Song KW, Fu T, Roland B, Chang H, Horsman DE et al. Influence of cytogenetics in patients with relapsed or refractory multiple myeloma treated with lenalidomide plus dexamethasone: adverse effect of deletion 17p13. Blood 2009; 114: 522–525.
Rasche L, Bernard C, Topp MS, Kapp M, Duell J, Wesemeier C et al. Features of extramedullary myeloma relapse: high proliferation, minimal marrow involvement, adverse cytogenetics: a retrospective single-center study of 24 cases. Ann Hematol 2012; 91: 1031–1037.
Papanikolaou X, Repousis P, Tzenou T, Maltezas D, Kotsopoulou M, Megalakaki K et al. Incidence, clinical features, laboratory findings and outcome of patients with multiple myeloma presenting with extramedullary relapse. Leuk Lymphoma 2013; 54: 1459–1464.
Sellner L, Heiss C, Benner A, Raab MS, Hillengass J, Hose D et al. Autologous retransplantation for patients with recurrent multiple myeloma: a single-center experience with 200 patients. Cancer 2013; 119: 2438–2446.
Jimenez-Zepeda VH, Mikhael J, Winter A, Franke N, Masih-Khan E, Trudel S et al. Second autologous stem cell transplantation as salvage therapy for multiple myeloma: impact on progression-free and overall survival. Biol Blood Marrow Transplant 2012; 18: 773–779.
Anagnostopoulos A, Hamilos G, Zorzou MP, Grigoraki V, Anagnostou D, Dimopoulos MA . Discordant response or progression in patients with myeloma treated with thalidomide-based regimens. Leuk Lymphoma 2004; 45: 113–116.
Brioli A, Giles H, Pawlyn C, Campbell JP, Kaiser MF, Melchor L et al. Serum free immunoglobulin light chain evaluation as a marker of impact from intraclonal heterogeneity on myeloma outcome. Blood 2014; 123: 3414–3419.
Ahn JS, Jung SH, Yang DH, Bae SY, Kim YK, Kim HJ et al. Patterns of relapse or progression after bortezomib-based salvage therapy in patients with relapsed/refractory multiple myeloma. Clin Lymphoma Myeloma Leuk 2014; 14: 389–394.
Shah JJ, Orlowski RZ, Alexanian R, Wang M, Thomas S, Qazilbash MH et al Phase I Trial of the Combination of Lenalidomide, Thalidomide and Dexamethasone In Relapsed/Refractory Multiple Myeloma. ASH Annual Meeting Abstracts 2010 Vol. 116, 2010, p1948.
Niesvizky R, Martin TG 3rd, Bensinger WI, Alsina M, Siegel DS, Kunkel LA et al. Phase Ib dose-escalation study (PX-171-006) of carfilzomib, lenalidomide, and low-dose dexamethasone in relapsed or progressive multiple myeloma. Clin Cancer Res 2013; 19: 2248–2256.
Jagannath S, Barlogie B, Berenson J, Siegel D, Irwin D, Richardson PG et al. A phase 2 study of two doses of bortezomib in relapsed or refractory myeloma. Br J Haematol 2004; 127: 165–172.
Dimopoulos M, Siegel DS, Lonial S, Qi J, Hajek R, Facon T et al. Vorinostat or placebo in combination with bortezomib in patients with multiple myeloma (VANTAGE 088): a multicentre, randomised, double-blind study. Lancet Oncol 2013; 14: 1129–1140.
Acknowledgements
We gratefully acknowledge the editorial support of Megan Hiserodt, Michelle Maglio and Lisa Paik in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JL reports grants from Novartis, grants from Celgene, grants from Onyx, grants from Millennium, outside the submitted work. LG reports personal fees from BMS, personal fees from Amgen, outside the submitted work. AM has received honorarium from Millennium Pharmaceuticals in the last 36 months for advisory board. GG reports grants and personal fees from Celgene, personal fees from Fujimoto Pharmaceutical Company, Japan, outside the submitted work. OS reports personal fees from Amgen, personal fees from Celgene and personal fees from Janssen. PV reports personal fees and other from Celgene Corporation, personal fees from Millennium Pharmaceuticals: A Takeda Oncology Company, personal fees from Novartis, other from Array Biopharma, grants and other from Oncopeptides, grants from Onyx Pharmaceuticals, grants and personal fees from GlaxoSmithKline, grants from Janssen and grants from Acetylon Pharmaceuticals. XL has received honorarium from Celgene, Millennium, Amgen, Janssen, Novartis, BMS, TEVA, LeoPHARMA and Pierre Fabre. MS has received Speakers Fees from Celgene and Janssen. HL reports grants from Takeda, grants and personal fees from Celgene, personal fees from Amgen/Onyx, personal fees from Janssen-Cilag. U-HM reports honoraria from Novartis, Mundipharma, Celgene, Amgen and Janssen and participated in advisory boards for Amgen and Celgene. WJC has received Honorarium from Celgene, Janssen, Millennium Takeda, Novartis and Onyx. EZ has received honoraria from Celgene and Janssen. CSC has received honorarium from Celgene and Janssen. TR has received honoraria from Celgene and Janssen. DJ has served on the advisory boards for Celgene, Onyx and Janssen; DJ has received payment for services from Celgene and Janssen. MR reports grants and personal fees from Celgene, grants from Janssen and grants from Onyx. POG has received honoraria from Celgene, Janssen and Takeda. ET has received honoraria and research grants from Amgen and Janssen-Cilag; ET has received honoraria from Celgene and Roche. PM has received compensation/honoraria for participation in scientific advisory boards for Celgene, Janssen, Sanofi, Karyopharm, The Binding Site and Bristol Myers Squibb. MD has received honoraria from Celgene, Janssen, Onyx, Takeda and Novartis. PM has served on the advisory board for Janssen, Celgene, Takeda, Novartis and Amgen. RO has been funded by the NIH, and has also received research grants from Array Biopharma, Bristol-Myers Squibb, Celgene Corporation, Janssen, Millennium Pharmaceuticals and Spectrum Pharmaceuticals. In addition, he has served on scientific advisory boards with compensation for Abbott Laboratories, Amgen, Inc., Array Biopharma, Bristol-Myers Squibb, Celgene Corporation, Forma Therapeutics, Incyte, Janssen, Millennium Pharmaceuticals, on scientific advisory boards without compensation for Acetylon Pharmaceuticals, Inc. KCA has served on Advisory boards for Celgene, Millennium, Sanofi Aventis, Gilead and Bristol-Myers Squibb. KA is also the scientific founder of Acetylon and Oncopep. AP has received honoraria from Janssen, Celgene, Amgen, Millennium/Takeda and BMS. SK’s institution has received consulting fees from Merck, Millennium, Celgene, Sanofi/Genzyme and Onyx and grants from R01. SK has received payment for services from Sharp Healthcare. PGR has served on advisory boards for Celgene, Millennium, Johnson & Johnson, Novartis, Bristol-Myers Squibb and Onyx. JC, HEJ, AJ, LP, HE, JH, IT, AM, JW, JL, SK, VR and BD have nothing to disclose.
Rights and permissions
About this article
Cite this article
Laubach, J., Garderet, L., Mahindra, A. et al. Management of relapsed multiple myeloma: recommendations of the International Myeloma Working Group. Leukemia 30, 1005–1017 (2016). https://doi.org/10.1038/leu.2015.356
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.356
- Springer Nature Limited
This article is cited by
-
Efficacy and Safety Analysis of VRD-PDCE in Treatment-Native Patients with Multiple Extramedullary Plasmacytomas or Plasma Cell Leukemia
Indian Journal of Hematology and Blood Transfusion (2023)
-
Novel cellular immunotherapies for hematological malignancies: recent updates from the 2021 ASH annual meeting
Experimental Hematology & Oncology (2022)
-
Optimal timing of treatment at relapse after autologous stem cell transplantation in patients with multiple myeloma: a study of the Korean Multiple Myeloma Working Party (KMM-1909)
Bone Marrow Transplantation (2022)
-
Prognostic value of 18F-fluorodeoxyglucose positron emission tomography/computed tomography at diagnosis in untreated multiple myeloma patients: a systematic review and meta-analysis
Clinical and Experimental Medicine (2022)
-
LncRNA HCP5 acts as a miR-128-3p sponge to promote the progression of multiple myeloma through activating Wnt/β‐catenin/cyclin D1 signaling via PLAGL2
Cell Biology and Toxicology (2022)