Abstract
Fine particulate matter <2.5 μm (PM2.5) has been associated with human health issues; however, findings regarding the influence of PM2.5 on respiratory disease remain inconsistent. The short-term, population-based association between the respiratory clinic visits of children and PM2.5 exposure levels were investigated by considering both the spatiotemporal distributions of ambient pollution and clinic visit data. We applied a spatiotemporal structured additive regression model to examine the concentration–response (C–R) association between children’s respiratory clinic visits and PM2.5 concentrations. This analysis was separately performed on three respiratory disease categories that were selected from the Taiwanese National Health Insurance database, which includes 41 districts in the Taipei area of Taiwan from 2005 to 2007. The findings reveal a non-linear C–R pattern of PM2.5, particularly in acute respiratory infections. However, a PM2.5 increase at relatively lower levels can elevate the same-day respiratory health risks of both preschool children (<6 years old) and schoolchildren (6–14 years old). In preschool children, same-day health risks rise when concentrations increase from 0.76 to 7.44 μg/m3, and in schoolchildren, same-day health risks rise when concentrations increase from 0.76 to 7.52 μg/m3. Changes in PM2.5 levels generally exhibited no significant association with same-day respiratory risks, except in instances where PM2.5 levels are extremely high, and these occurrences do exhibit a significant positive influence on respiratory health that is especially notable in schoolchildren. A significant high relative rate of respiratory clinic visits are concentrated in highly populated areas. We highlight the non-linearity of the respiratory health effects of PM2.5 on children to investigate this population-based association. The C–R relationship in this study can provide a highly valuable alternative for assessing the effects of ambient air pollution on human health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.INTRODUCTION
Increased rates of mortality, cardiovascular disease, and respiratory disease associated with exposure to particulate matter have been observed in numerous studies.1, 2, 3, 4, 5, 6, 7 In particular, a consensus has confirmed the causality between elevated PM2.5 concentrations and increased mortality rates for cardiovascular disease, especially for fine particulate matter with aerodynamic diameters of <2.5 μm (PM2.5).8 Numerous studies have also suggested that high levels of PM2.5 might elevate the risk of hospitalizations and emergency admissions for respiratory diseases.9, 10, 11, 12 For example, an investigation has shown that a modest increased risk of bronchiolitis is attributable to high PM2.5 levels, particularly for infants born during peak respiratory syncytial virus seasons.13 Significant positive associations between PM2.5 levels and the prevalence of both asthma and influenza were also revealed.14 Additionally, PM2.5 levels had a significant impact on pneumonia mortality and hospitalizations.15, 16 For people who suffer from chronic obstructive pulmonary disease, significant relationships between PM2.5 levels and hospital admissions, emergency room visits, and mortality rates were assessed.17, 18, 19, 20 However, to date, the limited number of studies focusing on the association of PM2.5 levels and respiratory diseases resulting in minor health effects have rendered inconsistent conclusions.10, 21, 22, 23
Epidemiologic associations determined from assessing respiratory health effects that result from exposure to air pollutants have been derived from a variety of statistical methods, such as generalized linear models, logistic regressions, and Poisson regressions.22, 24, 25, 26, 27 This methodology is primarily based on the linear assumption that changes in any health measure are incrementally related to exposure. However, studies have investigated possible non-linear relationships between health measures and exposure levels by using threshold-based models or generalized additive models.3, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Some of these studies have shown a non-linear association between mortality and PM2.5 concentrations, implying that the relationship between concentration change and health responses is not proportional.30, 31, 38, 39, 40 In other words, the analysis of health outcomes that use models with linear assumptions to explain exposure variables might be influenced by the variation of concentration–response (C–R) slopes at different concentration levels, yielding inconsistent or unreliable results in the previous studies. While the assessment of mortality was discussed in Pope in 2000,39 analyzing non-linear C–R relationships can help determine the threshold of environmental pollution levels associated with a variety of selected health issues. Very few studies have investigated the non-linear C–R relationships of the health outcomes associated with respiratory diseases (e.g., clinic visits).
Substantial geographic heterogeneity has been shown to be a factor in the adverse health responses that result from PM2.5 exposure across spatial locations in several multiregional studies.7, 23, 25, 26, 41, 42, 43, 44 This can be partially explained by the fact that the measurement of particulate matter actually involves the measurement of chemical compositions, which can vary across geographical regions. Therefore, the toxicological effects and associated health impacts of particulate matter can change even at similar PM2.5 levels. Moreover, the average levels of PM2.5 that vary depending on location can affect the C–R slope across the study area if non-linearity exists in C–R relationships. As shown in a report by the World Health Organization,45 it is not unusual that long- or short-term PM2.5 levels in Asian countries are much higher than those in the United States or Europe, particularly in heavily populated metropolitan areas. In other words, the epidemiologic analyses of the effects of PM2.5 levels on health obtained from studies in Western countries at certain PM2.5 levels or with specific chemical compositions may not be appropriate for direct application to other countries. In particular, analyses that only consider the linear association between health outcomes and air pollutant levels may be skewed.
To uncover any short-term respiratory health effect associated with specified levels of PM2.5 exposure, this study adopted a Bayesian spatiotemporal modeling approach for investigating the non-linear C–R relationship between PM2.5 concentrations and children’s respiratory health outcomes while controlling for temporal autoregressive correlation, spatial autocorrelation, and copollutants.46 The health data were obtained from the National Health Insurance database in Taiwan between 2005 and 2007. The two main research objectives are as follows: (1) to establish the C–R association between PM2.5 levels and children’s respiratory diseases; and (2) to display the role of spatial impact in the evaluation of the C–R curve.
METHODS
Clinic Visit Data
Children’s respiratory clinic visit data were obtained from the database of Taiwan’s National Health Insurance program, which is contracted with more than 97% of the hospitals and clinics in Taiwan and enrolls more than 96% of Taiwanese residents. Because it contains the information of more than 99.6% of the insured inhabitants of Taiwan, the database is one of the most comprehensive health insurance databases worldwide. The Taiwan National Health Research Institutes maintains this database and has established a standard procedure to guarantee the quality and accuracy of claims data.47 Owing to personal confidentiality concerns, all individual health informations such as personal and hospital identification numbers are encrypted before release. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) is used to retrieve cause-specific diseases. Children ≤14 years old with the following respiratory diseases were recruited in this study: acute respiratory infections that include the common cold, sinusitis, pharyngitis, tonsillitis, laryngitis and tracheitis, bronchitis, and bronchiolitis (ICD-9-CM: 460–466); other diseases of the upper respiratory tract that include allergic rhinitis, peritonsillar abscess, and laryngotracheitis (ICD-9-CM: 470–478); pneumonia and influenza (ICD-9-CM: 480–488). This population-based clinic visit data includes both ambulatory and emergency room visits. In this study, we analyze the clinic visit data of preschool children (<6 years old) and schoolchildren (6–14 years old) that occur in the Taipei area from 2005 to 2007.
Study Area and Air Quality Data
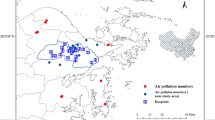
Taipei is the largest metropolitan area in Taiwan and comprises two administrative areas (i.e., Taipei City and New Taipei City) with a population size of ~7 million. Traffic is the dominant emission source of air pollution in the area.48 This study area is located in the Taipei Basin, which is bound by the Yangming Mountains to the north, Linkou Mesa to the west and the ridge of Snow Mountains to the southeast. The characteristics of the basin landscape can constrain the diffusion of PM particles from emission sources and exacerbate the poor air quality in the metropolitan area.49 Figure 1 shows the topography, main highways, and rivers of the Taipei metropolitan area. The air quality monitoring network operated by Taiwan Environmental Protection Agency regularly monitors the criteria pollutants. As shown in Figure 1, the monitoring stations are mostly located in populated areas. The spatiotemporal daily estimations of air quality data in each district from 2005 to 2007 was based on the Bayesian maximum entropy method. In our analysis, the air quality data that was under detection limits were considered as the soft data with ranges between 0 and instrumental detection limits published by TWEPA. Details of the Bayesian maximum entropy method used in air quality modeling in Taiwan can refer to Yu and Wang.50The substantial discrepancy of the estimated PM2.5 measurements at the district level revealed that the PM2.5 level in the urbanized regions of Taipei are ~1.7 times higher than those in the surrounding areas (Supplementary Table S1).
Data Analysis
This study considered a structured additive regression model to describe the non-linear association between air pollutants and clinic visits by children owing to respiratory diseases imposed upon a spatiotemporal pattern. Suppose the outcome Ydt is the number of clinic visits for children’s respiratory disease at day t (t=1, 2, …, 1095) in district d (d=1, 2,…, 41), following a Poisson distribution denoted by POI(μdt). This parameter can be modeled via a Poisson model framework; however, the Ydt exhibits larger variances than the one allowed in the theoretical Poisson model.51 Hence, we adopted a quasi-Poisson model framework to accommodate the observed overdispersion effects:

where (DOW)t contains six dummy variables for days-of-the-week from Monday to Saturday (i.e., Sunday is the reference level), and a holiday dummy variable for national holidays and summer/winter vacations. Σf(copollutant)dt contains smoothers of copollutants only from NOx, O3, and cPM (i.e., PM10−PM2.5). The smoothing function for PM2.5 was denoted by f(PM2.5dt). The time smoothing function f(t) stands for calendar time-adjusted long-term temporal trends during the study period. The temperature smoother f(TPdt) adjusted the effects of weather. All smoothing functions applied the B-spline with a second-order random walk penalty,52 so the smoothing function f(PM2.5dt) was used to evaluate the C–R association. A series of model selections was implemented to determine whether copollutants should be linear or non-linear in the final STAR model. The spatial influence was analyzed by Markov random fields using a normally distributed conditional autoregressive prior: 53

where the denominator Nd is the number of neighboring districts adjacent to district d, and Θd is a subset of neighbors of district d. The variance σ2d and unknown smoothing parameters are estimated simultaneously with hyperpriors following inverse Gamma distributions IG(0.001, 0.001). The offset was the logarithm of the district-level population of children.
The percentage increase of relative rate (RR) was calculated using (exp(linear estimates)−1) × 100%, whereas the C–R curve of PM2.5 was demonstrated by the percentage increase of RR per 10 μg/m3 increase, using (exp(non-linear estimates × 10)−1) × 100%. The exponentiation of spatial function can estimate the RR in each district compared with the mean RR for all districts.54 Each spatial function has a 95% posterior distribution to determine the significance of the spatial estimate in each district. The visualization for RR from the spatial function with corresponding 95% posterior probability was proposed to highlight the spatial pattern of children’s respiratory clinic visits. The autocorrelation function for estimated parameters with the maximum lag number reveals that all the lags were within −0.1 and 0.1, suggesting that autocorrelations were well controlled in the final model (data not shown here). The McNemar’s test was applied to test whether the spatial significance among districts is concordant between preschool children and schoolchildren. A sensitivity analysis was performed by changing the number of knots in temperature and time smoothers in the final model to identify whether the PM2.5 smoother has explicit changes. Data management, demographic statistics, and categorical data analysis were generated using SAS v9.3 software (SAS Institute, Cary, NC, USA). Spatiotemporal data analyses were conducted using the BayesX v2.1 software package.55
RESULTS
Table 1 shows summary statistics for the four air pollutants used in this study as well as temperature, revealing greater deviations, especially in PM2.5 and NOx, which can have minimum values below 1 μg/m3 or 1 p.p.b., but maximum values can be as large as 119.56 μg/m3 and 159.56 p.p.b., respectively. Figure 2 displays district-level crude rates of children’s daily respiratory clinic visits and reveals that the distribution of each crude clinic visit rate was not uniform across the study area, especially for acute respiratory infections.
Figure 3 presents the geographic distribution of the daily average air pollutant measurements in Taipei over the 3 years of the study period, displaying the varied spatial patterns among the four air pollutants. Greater average PM2.5 values reached concentrations as high as 32.03 μg/m3 per day in eastern districts of Taipei, whereas districts located in the mountain area (i.e., southern and western Taipei) exhibited smaller averages as low as 14.27 μg/m3 per day. Similar situations also occurred with regard to cPM. NOx was distributed uniformly across most districts, but three districts exceeded the average levels of the other districts, with the Sanchong District having the highest levels (66.29 p.p.b. per day).
The RR percentage change for each day of the week compared with Sunday for children’s respiratory clinic visits is shown in Supplementary Table S2. The results suggest the following: (1) the highest RR percentage increase for clinic visits involving three of the three respiratory diseases studied occurred on Mondays in both age groups investigated. However, upper respiratory tract disease clinic visits occurred with a greater RR percentage increase on Saturdays; (2) pneumonia and influenza clinic visits exhibited a significant RR percentage increase on each day of the week, ranging from 4.00% (95% CI: 2.76, 5.25) on Wednesday to 48.89% (95% CI: 47.35, 50.44) on Monday for preschool children, and from 3.93% (95% CI: 2.52, 5.36) on Thursday to 50.15% (95% CI: 48.38, 51.95) on Monday for schoolchildren. Moreover, national holidays and summer/winter vacations had significantly decreased RR percentages up to −6.03% (95% CI=−6.93, −5.12), except for other upper respiratory tract diseases in schoolchildren.
For acute respiratory infections, the C–R curve of PM2.5 concentrations in Figure 4a exhibited a strong association of increasing RR percentages for both groups with respect to PM2.5 concentration increases at relatively lower levels. The RR percentage for preschool children visits exhibits an increasing trend from negative to positive at relatively low PM2.5 levels in the range between 0.76 and 7.44 μg/m3. Similarly, an increasing trend of RR percentage for schoolchildren clinic visits also presented from 0.76 to 7.52 μg/m3. No significant association was found between PM2.5 concentration changes and acute respiratory infections at relatively higher PM2.5 levels, except at extremely high PM2.5 concentrations. For preschool children, a high PM2.5 concentration (>93.44 μg/m3) caused the RR percentage of clinic visits to greatly increase from 7.50% to 42.11% when PM2.5 concentrations reached 100.33 μg/m3. A significant impact on clinic visits by schoolchildren are noted when PM2.5 concentrations are >90.52 μg/m3. With extreme increases in PM2.5 concentrations >97.92 and 95.91 μg/m3, RR percentage increases in clinic visits were observed in other diseases of the upper respiratory tract for both preschool children and schoolchildren, as shown in Figure 4b. While Figure 4c indicates that preschool children’s clinic visits for pneumonia and influenza did not exhibit explicit variations on the C–R curve for PM2.5, the significant impact of extremely high concentrations of PM2.5 on the clinic visits of schoolchildren still appeared.
Figure 5 displays the varied spatial pattern of RR computed from the estimated spatial function among three types of respiratory diseases for preschool children’s clinic visits in Taipei. For acute respiratory infections in Figure 5a, 32 of 41 districts (78.05%) have RRs that are significantly higher than the average. The RRs in the other districts, which are all located in the outskirts close to mountains and coastal lines, are significantly lower than the average. A similar spatial pattern was also observed in other diseases of the upper respiratory tract in Figure 5b, but the highest RR located in the Jhongjheng District was elevated to 9.26 (95% CI: 8.65, 9.90). Fewer districts with significantly higher RRs for pneumonia and influenza are shown in Figure 5c.
Figure 6 displays the spatial pattern of RR for schoolchildren’s respiratory clinic visits. Compared with preschool children, over a half of districts had a smaller RR for schoolchildren, especially in those districts of Taipei City for other upper respiratory tract diseases (9 of 12 districts) and pneumonia/influenza (11 of 12 districts) shown in Figures 6b and c. Nonetheless, the significant spatial patterns were similar for both groups. In particular, upper respiratory tract diseases had identical significance maps between preschool children and schoolchildren (Figure 5b versus 6b). For the other two types of respiratory diseases, we also found no statistically significant difference between two groups because all P-values are >0.05. Sensitivity analysis results show that the PM2.5 smoothers were robust with respect to the varying of the number of knots in temperature and time smoothers in each of the respiratory disease categories studied in both preschool children and schoolchildren. These findings imply that the proposed model in this study can adequately capture the non-linear C–R association between PM2.5 concentration levels and children’s respiratory clinic visits.
DISCUSSION AND CONCLUSIONS
This was the first spatiotemporal study to assess a population-based C–R curve evaluating the occurrence of respiratory disease in relation to PM2.5 exposure. We focused on the short-term associations between children’s daily clinic visits and concurrent PM2.5 concentrations with additional consideration of other ambient air pollutants. The availability of National Health Insurance (data in Taiwan enables this population-based C–R association analysis, and yields more representative results than those obtained in previous studies, which have analyzed local hospital admissions and mortality data.12, 27, 34, 40, 41, 56 In addition, hospital admissions and mortality data review severe illnesses, which implies that the results from previous analyses might have underestimated effects in the general population.57, 58 In other words, the C–R relationship for clinic visit data in this study can provide a highly valuable alternative for assessing the effects of ambient air pollutant exposure on human health.
This study revealed a non-linear association between health outcomes and different levels of PM2.5. Children’s respiratory health is sensitive to increments of PM2.5 concentration primarily at relatively low and high ranges, which are concentrations lower than 10% and higher than 75%, respectively. Specifically, in acute respiratory infections, this study reveals the increasing RR of respiratory clinic visits that may have been impacted by PM2.5 concentration levels in both preschool and school children populations. This finding is consistent with the results of previous studies that have shown an association between the incidence of respiratory infections and elevated PM2.5 levels.25, 27, 59 Furthermore, this paper reveals the non-linear behavior for associations between PM2.5 levels and respiratory health outcomes. These findings might partially explain the high discrepancy in the slope of health changes regarding PM2.5 levels and emission characteristics that were noted in previous studies.21, 22, 56 For example, no significant association between PM2.5 concentration levels and the incidence of respiratory diseases were identified in a multicity study conducted in France.56 These findings can possibly be attributed to the high heterogeneity of the study population and the emission patterns within the studied cities. In this study, there was also a high variance of topography and medical resources in the areas studied. In addition to acute respiratory infections, our results reveal that PM2.5 concentrations can increase the risk of other upper respiratory diseases, pneumonia and influenza.9, 27, 59 The potential non-linear PM2.5 C–R association for pneumonia and influenza can be primarily observed in schoolchildren, but not in preschool children. The results document that the changes in PM2.5 levels have less impact on the respiratory health status of preschool children compared with the respiratory health status of schoolchildren. In particular, no association is observed in schoolchildren, especially in pneumonia and influenza. Although our study was population-based, some uncertainty remains in our analysis owing to the potential scaling issue in space. Both the environmental and clinic data are averaged with respect to townships, which can smooth out the C–R associations in the analysis.
The evaluation of C–R curves has been widely used for identifying the potential PM2.5 threshold under which no health outcomes can be observed. Such an approach has primarily been applied to investigate the relationship between mortality and air quality levels.30, 31, 38, 43, 60 Our results document no PM2.5 threshold for health effects that can be identified for respiratory infections and diseases. This result is similar to previous findings for other conditions such as mortality and cardiovascular diseases.3, 39 In addition, when PM2.5 concentrations are low, the association between the respiratory health responses and PM2.5 levels are nearly linear, which is similar to previous findings regarding mortality.31 This study further revealed that respiratory health effects can be saturated as long as PM2.5 levels do not exceed 90.52 μg/m3. The occurrence of PM2.5 levels >90.52 μg/m3 is relatively rare, but does occur during events such as Asian dust storms. During these dust storms, chemical compositions of PM2.5 concentrations are completely different from those of regular days.61, 62, 63
The spatial function using a conditional autoregressive prior in Markov random fields in this study notes the existence of a significant geographic disparity in children’s respiratory clinic visits, and this disparity was unable to be identified by unstructured random effects. The spatial distributions of all respiratory health measures are closely associated with the topography of Taipei, where districts with a higher RR for respiratory clinic visits are more urbanized and populated. The geographical distribution of RR is associated not only with the spatial variation of exposure levels, but also with other confounding factors, such as the distribution of medical resources and population characteristics.64, 65 The geographical heterogeneity among the urbanized districts is lower for upper respiratory infections than for more severe health conditions (e.g., pneumonia), and this holds particularly true for schoolchildren.
This study highlights the importance of accounting for the non-linearity of C–R relationship in understanding the possible health impact of PM2.5 concentrations on respiratory diseases. In other words, this non-linearity can make the interpretation of the short-term respiratory health effects of PM2.5 concentrations difficult. Comparing the linear PM2.5 concentration results with the non-linear PM2.5 concentration smoother results, more detailed PM2.5 impacts are demonstrated. This gives more accurate scientific meaning to the diverse variation of PM2.5 affecting children’s respiratory disease. Through the use of a population-based health data set, this study provides information on the health effects of PM2.5 exposure, and displays the high variability of the C–R relationship with PM2.5 that is verified in this analysis. Other confounders associated with clinic visits for respiratory diseases (e.g., prevalence of cold and flu) may also impact the findings. Furthermore, complex physical and chemical interactions associated with high PM2.5 concentrations can occur in a variety of environmental conditions, which can additionally strengthen or weaken any acute respiratory effects. Further analysis is required to determine the interaction between PM2.5 concentrations and other environmental and air pollution conditions. Moreover, it would be valuable to perform further assessments when more of the NHRI data set is available, as this analysis was only based upon the 2005–2007 data. In addition, this study did not investigate the lagged effects of PM2.5 exposure on health responses because the inclusion of multiple-time non-linear functions in this analysis might induce an overparameterization issue. However, when additional health data sets are available, lagged effect analysis should be performed.
This study focused on a highly vulnerable population to investigate any substantial effects of PM2.5 concentration levels on three types of respiratory diseases. Access to daily clinic visit data from the National Health Insurance in Taiwan provided the most complete medical records and also encompassed a broad geographic area over a lengthy time period. Our findings can be indispensable for policy makers when considering the potential effects of air pollution on children’s health, and can help them establish appropriate interventions for protecting vulnerable residents living in areas where extreme air disasters, such as Asian dust storms, occur.
References
Pope CA, 3rd, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002; 287: 1132–1141.
Dockery DW, Pope CA, 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med 1993; 329: 1753–1759.
Pope CA, 3rd, Dockery DW . Health effects of fine particulate air pollution: lines that connect. J Air Waste Manage Assoc 2006; 56: 709–742.
Dockery DW, Pope CA, III . Acute respiratory effects of particulate air pollution. Annu Rev Public Health 1994; 15: 107–132.
Schwartz J, Dockery DW, Neas LM, Wypij D, Ware JH, Spengler JD, et al. Acute effects of summer air pollution on respiratory symptom reporting in children. Am J Respir Crit Care Med 1994; 150: 1234–1242.
Laden F, Neas LM, Dockery DW, Schwartz J . Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Environ Health Perspect 2000; 108: 941–947.
Franklin M, Zeka A, Schwartz J . Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. J Expos Sci Environ Epidemiol 2007; 17: 279–287.
USEPA Integrated Science Assessment for Particulate Matter (Final Report). US Environmental Protection Agency: Washington, DC, USA. 2009.
Zanobetti A, Schwartz J . Air pollution and emergency admissions in Boston, MA. J Epidemiol Commun Health 2006; 60: 890–895.
Winquist A, Klein M, Tolbert P, Flanders WD, Hess J, Sarnat SE . Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ Health 2012; 11: 70.
Zanobetti A, Franklin M, Koutrakis P, Schwartz J . Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ Health 2009; 8: 58.
Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR . Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Archiv Environ Health 1999; 54: 130–139.
Karr CJ, Rudra CB, Miller KA, Gould TR, Larson T, Sathyanarayana S, et al. Infant exposure to fine particulate matter and traffic and risk of hospitalization for RSV bronchiolitis in a region with lower ambient air pollution. Environ Res 2009; 109: 321–327.
Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J 2007; 29: 879–888.
Katanoda K, Sobue T, Satoh H, Tajima K, Suzuki T, Nakatsuka H, et al. An association between long-term exposure to ambient air pollution and mortality from lung cancer and respiratory diseases in Japan. J Epidemiol/Jpn Epidemiol Assoc 2011; 21: 132–143.
Neupane B, Jerrett M, Burnett RT, Marrie T, Arain A, Loeb M . Long-term exposure to ambient air pollution and risk of hospitalization with community-acquired pneumonia in older adults. Am J Respir Crit Care Med 2010; 181: 47–53.
Ko FW, Tam W, Wong TW, Chan DP, Tung AH, Lai CK, et al. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax 2007; 62: 780–785.
Kumar N, Liang D, Comellas A, Chu AD, Abrams T, Satellite-based PM . Satellite-based PM oncentrations and their application to COPD in Cleveland, OH. J Expos Sci Environ Epidemiol 2013; 23: 637–646.
Qiu H, Yu IT, Tian L, Wang X, Tse LA, Tam W, et al. Effects of coarse particulate matter on emergency hospital admissions for respiratory diseases: a time-series analysis in Hong Kong. Environ Health Perspect 2012; 120: 572–576.
Valdes A, Zanobetti A, Halonen JI, Cifuentes L, Morata D, Schwartz J . Elemental concentrations of ambient particles and cause specific mortality in Santiago, Chile: a time series study. Environ Health 2012; 11: 82.
Delfino RJ, Staimer N, Gillen D, Tjoa T, Sioutas C, Fung K, et al. Personal and ambient air pollution is associated with increased exhaled nitric oxide in children with asthma. Environ Health Perspect 2006; 114: 1736–1743.
Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, Claiborn C . Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expos Anal Environ Epidemiol 2005; 15: 153–159.
Nachman KE, Parker JD . Exposures to fine particulate air pollution and respiratory outcomes in adults using two national datasets: a cross-sectional study. Environ Health 2012; 11: 25.
Schwartz J, Neas LM . Fine particles are more strongly associated than coarse particles with acute respiratory health effects in schoolchildren. Epidemiology 2000; 11: 6–10.
Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006; 295: 1127–1134.
Bell ML, Ebisu K, Peng RD, Walker J, Samet JM, Zeger SL et al. Seasonal and regional short-term effects of fine particles on hospital admissions in 202 US counties, 1999-2005. Am J Epidemiol 2008; 168: 1301–1310.
Ostro B, Roth L, Malig B, Marty M . The effects of fine particle components on respiratory hospital admissions in children. Environ Health Perspect 2009; 117: 475–480.
Atkinson RW, Yu D, Armstrong BG, Pattenden S, Wilkinson P, Doherty RM, et al. Concentration-response function for ozone and daily mortality: results from five urban and five rural U.K. populations. Environ Health Perspect 2012; 120: 1411–1417.
Kim SY, Lee JT, Hong YC, Ahn KJ, Kim H . Determining the threshold effect of ozone on daily mortality: an analysis of ozone and mortality in Seoul, Korea, 1995-1999. Environ Res 2004; 94: 113–119.
Daniels MJ, Dominici F, Samet JM, Zeger SL . Estimating particulate matter–mortality dose–response curves and threshold levels: an analysis of daily time-series for the 20 largest US cities. Am J Epidemiol 2000; 152: 397–406.
Schwartz J, Laden F, Zanobetti A . The concentration–response relation between PM(2.5) and daily deaths. Environ Health Perspect 2002; 110: 1025–1029.
Samoli E, Schwartz J, Wojtyniak B, Touloumi G, Spix C, Balducci F, et al. Investigating regional differences in short-term effects of air pollution on daily mortality in the APHEA project: a sensitivity analysis for controlling long-term trends and seasonality. Environ Health Perspect 2001; 109: 349–353.
Dominici F, McDermott A, Zeger SL, Samet JM . On the use of generalized additive models in time-series studies of air pollution and health. Am J Epidemiol 2002; 156: 193–203.
Galan I, Tobias A, Banegas JR, Aranguez E . Short-term effects of air pollution on daily asthma emergency room admissions. Eur Resp J 2003; 22: 802–808.
Tenias JM, Ballester F, Perez-Hoyos S, Rivera ML . Air pollution and hospital emergency room admissions for chronic obstructive pulmonary disease in Valencia, Spain. Arch Environ health 2002; 57: 41–47.
Erbas B, Kelly AM, Physick B, Code C, Edwards M . Air pollution and childhood asthma emergency hospital admissions: estimating intra-city regional variations. Int J Environ Health Res 2005; 15: 11–20.
Farhat SC, Paulo RL, Shimoda TM, Conceicao GM, Lin CA, Braga AL, et al. Effect of air pollution on pediatric respiratory emergency room visits and hospital admissions. Braz J Med Biol Res 2005; 38 (2): 227–235.
Samoli E, Analitis A, Touloumi G, Schwartz J, Anderson HR, Sunyer J, et al. Estimating the exposure–response relationships between particulate matter and mortality within the APHEA multicity project. Environ Health Perspect 2005; 113: 88–95.
Pope CA, III . Particulate matter–mortality exposure–response relations and threshold. Am J Epidemiol 2000; 152: 407–412.
Li S, Batterman S, Wasilevich E, Wahl R, Wirth J, Su FC, et al. Association of daily asthma emergency department visits and hospital admissions with ambient air pollutants among the pediatric Medicaid population in Detroit: time-series and time-stratified case-crossover analyses with threshold effects. Environ Res 2011; 111: 1137–1147.
Englert N . Fine particles and human health – a review of epidemiological studies. Toxicol Lett 2004; 149: 235–242.
Dominici F, McDermott A, Zeger SL, Samet JM . National maps of the effects of particulate matter on mortality: exploring geographical variation. Environ Health Perspect 2003; 111: 39–44.
Dominici F, Daniels M, Zeger SL, Samet JM . Air pollution and mortality: estimating regional and national dose–response relationships. J Am Stat Assoc 2002; 97: 100–111.
Dominici F, Samet JM, Zeger SL . Combining evidence on air pollution and daily mortality from the 20 largest US cities: a hierarchical modelling strategy. J R Stat Soc 2000; 163: 263–302.
WHO Health Effects of Particulate Matter: Policy Implications for Countries in Eastern Europe, Caucasus and Central Asia. World Health Organization: Copenhagen, Denmark. 2013.
Chien L-C, Bangdiwala S . The implementation of Bayesian structural additive regression models in multi-city time series air pollution and human health studies. Stoch Environ Res Risk Assess 2012; 26: 1041–1051.
Tseng CH . Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care 2004; 27: 1605–1609.
Chang SC, Lee CT . Evaluation of the trend of air quality in Taipei, Taiwan from 1994 to 2003. Environ Monitor Assess 2007; 127: 87–96.
Tzeng GH, Tsaur SH, Laiw YD, Opricovic S . Multicriteria analysis of environmental quality in Taipei: public preferences and improvement strategies. J Environ Manage 2002; 65: 109–120.
Yu HL, Wang CH . Quantile-based Bayesian maximum entropy approach for spatiotemporal modeling of ambient air quality levels. Environ Sci Technol 2013; 47: 1416–1424.
Akaike H . A new look at the statistical model identification. IEEE Trans Automat Control 1974; 19: 716–723.
Lang S, Brezger A . Bayesian P-splines. J Comput Graph Statist 2004; 13: 183–212.
Kindermann R, Snell JL . Markov Random Fields and their Applications. American Mathematical Society: Providence, RI, USA. 1980.
Fromont A, Binquet C, Sauleau EA, Fournel I, Bellisario A, Adnet J, et al. Geographic variations of multiple sclerosis in France. Brain 2010; 133: 1889–1899.
Belitz C, Brezger A, Kneib T, Lang S., BayesX – Software for Bayesian Inference in Structured Additive Regression Models Version 2.1. http://www.BayesX.org/.
Host S, Larrieu S, Pascal L, Blanchard M, Declercq C, Fabre P, et al. Short-term associations between fine and coarse particles and hospital admissions for cardiorespiratory diseases in six French cities. Occup Environ Med 2008; 65: 544–551.
McClellan RO . Setting ambient air quality standards for particulate matter. Toxicology 2002; 181–182: 329–347.
Chien LC, Yang CH, Yu HL . Estimated effects of Asian dust storms on spatiotemporal distributions of clinic visits for respiratory diseases in Taipei children (Taiwan). Environ Health Perspect 2012; 120: 1215–1220.
Barnett AG, Williams GM, Schwartz J, Neller AH, Best TL, Petroeschevsky AL, et al. Air pollution and child respiratory health: a case-crossover study in Australia and New Zealand. Am J Resp Crit Care Med 2005; 171: 1272–1278.
Jimenez E, Linares C, Rodriguez LF, Bleda MJ, Diaz J . Short-term impact of particulate matter (PM2.5) on daily mortality among the over-75 age group in Madrid (Spain). Sci Total Environ 2009; 407: 5486–5492.
Hsu S-C, Liu SC, Lin C-Y, Hsu R-T, Huang Y-T, Chen Y-W . Metal compositions of PM10 and PM2. 5 aerosols in Taipei during spring, 2002. Terr Atmos Ocean Sci 2004; 15: 925–948.
Tsai YI, Chen C-L . Characterization of Asian dust storm and non-Asian dust storm PM 2.5 aerosol in southern Taiwan. Atmos Environ 2006; 40: 4734–4750.
Chou CC-K, Lin C-Y, Chen T-K, Hsu S-C, Lung S-C, Liu SC, et al. Influence of long-range transport dust particles on local air quality: a case study on Asian dust episodes in Taipei during the spring of 2002. Terr Atmos Ocean Sci 2004; 15: 881–889.
Yu HL, Yang CH, Chien LC . Spatial vulnerability under extreme events: a case of Asian dust storm's effects on children's respiratory health. Environ Int 2013; 54: 35–44.
Ouyang L . The geographical study of health care facility distribution in Taipei City, Taiwan. J Geogr Res 2006; 45: 51–72.
Acknowledgements
This work was supported by funds from Taiwan National Science Council (NSC 101-2628-E-002-017-MY3 and NSC 102-2221-E-002-140-MY3) and the Environmental Protection Department of the New Taipei City Government in Taiwan. The funders had no role in the study design, data collection, statistical analysis, decision to publish and manuscript preparation. We also appreciate Mrs. Mary Trottier’s help in the English editing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
About this article
Cite this article
Yu, HL., Chien, LC. Short-term population-based non-linear concentration–response associations between fine particulate matter and respiratory diseases in Taipei (Taiwan): a spatiotemporal analysis. J Expo Sci Environ Epidemiol 26, 197–206 (2016). https://doi.org/10.1038/jes.2015.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2015.21
- Springer Nature America, Inc.
Keywords
This article is cited by
-
Association between ambient air pollutants and upper respiratory tract infection and pneumonia disease burden in Thailand from 2000 to 2022: a high frequency ecological analysis
BMC Infectious Diseases (2023)
-
Impact of the critical episode management program on emergency room admissions for respiratory diseases in south-central Chile
Air Quality, Atmosphere & Health (2022)
-
Observed causative impact of fine particulate matter on acute upper respiratory disease: a comparative study in two typical cities in China
Environmental Science and Pollution Research (2022)
-
Short-term exposure to ambient air pollution and daily atherosclerotic heart disease mortality in a cool climate
Environmental Science and Pollution Research (2019)
-
Effect and threshold of PM2.5 on population mortality in a highly polluted area: a study on applicability of standards
Environmental Science and Pollution Research (2019)