Abstract
Background:
An epidemiological association between excess weight and increased risk of cancer has been described in melanoma, for which the physiopathological mechanisms are still unknown. The study of tumor microenvironment and of the role of adipocytes in cancer development, progression and metastasis has recently received great interest. However, the role of peritumoral adipocytes has been characterized only in a few types of cancer, and in melanoma it still remains to be defined.
Methods:
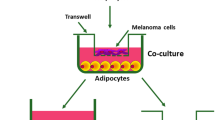
We investigated the interactions between adipocytes and melanoma cells using an in vitro co-culture system. We studied the morphological and functional properties of 3T3-L1 adipocytes before and after co-culture with A375 melanoma cells, in order to assess the role of adipocytes on melanoma migration.
Results:
Morphological analysis showed that after 6 days of co-culture 3T3-L1 adipocytes were reduced in number and size. Moreover, we observed the appearance of dedifferentiated cells with a fibroblast-like phenotype that were not present in controls and that had lost the expression of some adipocyte-specific genes, and increased the expression of collagen, metalloproteinases and genes typical of dedifferentiation processes. Through the Matrigel Invasion Test, as well the Scratch Test, it was possible to observe that co-culture with adipocytes induced in melanoma cells increased migratory capacity, as compared with controls. In particular, the increase in migration observed in co-culture was suppressed after adding the protein SFRP-5 in the medium, supporting the involvement of the Wnt5a pathway. The activation of this pathway was further characterized by immunofluorescence and western blot analysis, showing in melanocytes in co-culture the activation of β-catenin and LEF-1, two transcription factors involved in migration processes, neo-angiogenesis and metastasis.
Conclusions:
These data allow us to hypothesize a dedifferentiation process of adipocytes toward fibroblast-like cells, which can promote migration of melanoma cells through activation of Wnt5a and the intracellular pathways of β-catenin and LEF-1.
Similar content being viewed by others
Introduction
A large amount of epidemiological data supports the existence of a strong relationship between excess adiposity and the majority of cancers,1, 2, 3, 4 with a sex-specific1, 3 or sometimes histology-specific association,1, 2 if we consider both measures of total adiposity (as body mass index)1, 2, 3 and its distribution (such as waist circumference).1, 4
Recently, a panel of international experts has expanded the list of cancers for which there is sufficient strength of evidence of an association of cancer with excess adiposity,5 including melanoma as an obesity-related cancer.6
Several systemic mechanisms have been proposed to explain this epidemiological association.1, 7, 8 From a physiopathological point of view, adipose tissue (AT) may influence tumor development and progression by altered sex hormone metabolism,1, 7, 8 as well as by the production of different adipokines,9 determining a state of low-grade inflammation.1, 7, 8 Finally, circulating levels of insulin, both directly or indirectly, through an increase in insuline-like growth factor-1 (IGF-1) bioavailability, have also been shown to trigger cancer-relevant intracellular pathways.10
In addition to these systemic mechanisms, some authors have hypothesized that local fat surrounding tumors could profoundly influence early events in tumor growth, invasion and metastasization.8, 11, 12 AT has also recently been recognized as an important constituent of tumor microenvironment (TME);13 however, it has been the object of studies in just a few types of cancer.8, 14, 15
One of the hypothesized role for adipocytes in the TME is the possibility that they provide energy for rapid tumor growth to support the high proliferation rate of the cancer cells.16
It has also been suggested that during interaction with cancer cells, adipocytes in the TME can be reprogrammed into cancer-associated adipocytes (CAA) or can dedifferentiate into ‘fibroblast-like cells’, the so-called cancer-associated fibroblasts (CAFs).12, 17 Adipocytes are cells characterized by high physiological plasticity,18 and it has been shown that even mature fat cells are able to dedifferentiate generating cells with multipotent capacities.19, 20 However, this phenotypic shift from dysfunctional adipocytes to dysfunctional mesenchymal cells has been demonstrated only for breast cancer12, 17 and only a few data are available in the literature about other types of cancers.15
Although progress has generally been made over the last decade in establishing the structural and functional roles of TME in malignant processes, much remains to be discovered in particular about melanoma–adipocyte crosstalk. To evaluate the role of adipocytes in a the melanoma microenvironment, we set up an in vitro model of co-culture of 3T3-L1 adipocytes and a cell line of melanoma (A375); after a few days of co-culture we observed morphological changes in adipocytes, which resemble the aspect of mesenchymal pluripotent cells; we showed that these reprogrammed cells may contribute to the migratory and invasive capacity of melanoma.
Materials and methods
Cell culture
Low-passage human melanoma cell line A375 was kindly donated by Dr Natalia Realini from the University of Verona. Mouse preadipocyte 3T3-L1 cells came from ECACC Sigma-Aldrich SRL (Milano, Italy). All cells were cultured at 37 °C in a 5% CO2 DMEM/GlutaMAX culture medium (Gibco, Gaithersburg, MD, USA), with both containing 10% fetal bovine serum (FBS) and 1% Antibiotic Antimycotic Solution (Sigma-Aldrich). At 85–90% of confluence, 3T3-L1 cells were detached by trypsin-EDTA (Gibco) and seeded in six-wells or twelve wells (Becton Dickinson, Milano, Italy) containing a presterilized slide (Menzel-glaser Thermo Scientific). At 90% of confluence, 3T3-L1 cells were induced to differentiate in DMEM/F12 containing 10% FBS, 1% Antibiotic Antimycotic Solution, 0.2 mM 3-Isobutyl-1-methylxanthine, 10 μM rosiglitazone, 1 μM dexamethasone and 10 μg ml−1 insulin for 3 days. After 72 h post induction (post-induction day 3=PID 3), the medium was replaced with an adipocyte maintenance medium, composed of DMEM/F12 enriched with 10% FBS, 1% Antibiotic Antimycotic Solution and 10 μg ml−1 insulin (Sigma-Aldrich), in which cells were cultured for 2 days. Five days after adipocyte induction (PID 5), the cells were co-cultured with A375 cells using a Transwell culture system (0.4 μm pore size; Becton Dickinson) in an adipocyte maintenance medium without insulin. Overall, 15 000 cells cm−2 of A375 cells were seeded in the top chamber. Co-culture medium was replaced every 3 days at 50%. Cells were co-cultured with A375 for a further 3 days (PID 8) and 6 days (PID 11); A375 and 3T3-L1 adipocytes were cultivated alone and evaluated at the same time points as controls. Each experimental condition was carried out at least in triplicate. The vitality of cells under the different experimental conditions was assayed with Trypan blue and did not significantly change at the different time points between co-culture and control adipocytes (data not shown).
Oil Red O staining and optical image capturing and analyses
Cells cultures were fixed and stained with Mayer’s Hematoxylin (Bio-Optica, Milano, Italy) as previously described.15 Cells were observed in an Olympus BX51 photomicroscope equipped with a KY-F58 CCD camera (JVC, Milano, Italy). The images were analyzed using ImageJ software Version 1.47e (NIH, Bethesda, MD, USA) to count the cells within 10 representative fields (100 × magnification, number of cells expressed on mm2) and to calculate the area of 10 randomly chosen cells (400 × magnification, area expressed in μm2).
RNA extraction, complementary DNA synthesis and real-time polymerase chain reaction
RNA was extracted from 600 μl of cellular lysate of 3T3-L1, as previously detailed.15 Extracted and purified RNA was checked with an Agilent RNA 6000 Nano Kit (Agilent, Cernusco sul Naviglio, Milano, Italy).13 Reverse transcription of RNA to complementary DNA (cDNA) was performed with iScript cDNA Synthesis Kit by Bio-Rad (Milano, Italy) using protocols previously detailed.15 Real-time polymerase chain reaction (RT-PCR) was performed with a Bio-Rad MyiQ RT-PCR System, using a QuantiTect SYBR Green RT-PCR Kit by QIAGEN (Milano, Italy), according to the manufacturer's protocol. Expression levels of the genes of interest were normalized using internal control (β-Actin). Relative expression levels were calculated using the formula 2−(ΔΔCt). Each analysis was conducted at least in triplicate.
Lipolysis assay
A cultured adipocyte lipolysis assay kit (Glycerol cell based Assay kit, Cat 10011725, Cayman, Ann Arbor, MI, USA) was used to determine free glycerol released in medium during co-culture at PID 8 and 11. The absorbance was measured at 540 nm. A standard curve was created and the amount of free glycerol was determined in duplicate.
Western blot
A375 cells were lysed in ice-cold buffer, and centrifuged and lysed in a specific lysis buffer.15 Supernatant of lysates of both type of cells was collected. Equal amounts of proteins were loaded on 10% sodium dodecyl sulfate-polyacrylamide gels. Electrophoresis was performed at 100 V with a running buffer.15 The resolved protein was electroblotted onto a polyvinylidene difluoride membrane and subsequently incubated with the primary antibodies (WNT5a, Santa Cruz Biotechnology, Dallas, TX, USA; beta catenin, Bethyl Laboratories Inc, Montgomery, TX, USA; LEF-1, Thermo scientific, Monza, Italy; pAkt (S473), KTtot Cell Signaling, Leiden, Zuid-Holland, The Netherlands).
After washing, the membrane was further incubated with an horseradish peroxidase-conjugated secondary antibody (anti-goat and anti-rabbit, Santa Cruz Biotechnology) and, after washing, the membrane was developed using a chemiluminescent detection system.15
Invasion assay
Tumor melanoma cells A375 were grown alone or were co-cultivated with mature 3T3-L1 adipocytes starting 5 days post-adipogenesis induction. After 3 days, controls and co-cultured cells were serum-starved for 16 h; subsequently, A375s were trypsinized and seeded at 40 000 cells per well in pre-coated 8-μm inserts. The experiments were run in the presence of 10% FBS, used as chemoattractant as well as in the absence of serum (as negative control). Cells invaded Matrigel over a 24-h period and were quantitated using Calcein-AM. Similar experiments were repeated in the presence of Wnt5a inhibitor SFRP-5 (2 μg ml−1).
Wound-closure cell migration assay
A scratch wound-healing assay was performed as previously described.14 Cells A375 were seeded and grown to reach a confluent monolayer. A 10-μl pipette tip was then used to create a wound through the center of the confluent cell layer and then washed twice with media. Cells were then treated with a complete medium containing 1% FBS or a conditioned medium from adipocyte culture at PID 8 and incubated for 72 h. Photos were taken of the wound every 20 min throughout the assay. Cell migration was evaluated under the microscope, and images were taken every 20 min for 72 h. To quantify the data, the size of the wound was determined at the beginning of the assay and was compared with the size of the wound upon assay commencement.
Immunofluorescence microscopy
Cells were incubated overnight at 4 °C with rabbit anti-LEF-1 antibody (1:150, Thermo Scientific), washed in 0.1% Triton X-100 in 1 × PBS for three times, 10 min each, and incubated for 30 min at room temperature with anti-Rabbit IgG DyLight 488-conjugated antibody (1:100, Bethyl Laboratories Inc). Nuclei were stained for 5 min at room temperature with 4',6-diamidino-2-phenylindole (ready-to-use, BosterBio, Pleasanton, CA, USA).
Finally, cells were observed in an Olympus BX51 fluorescence microscope equipped with a KY-F58 CCD camera (JVC). The images were analyzed and stored using the software Image-ProPlus version 7.0 (National Institutes of Health, (NIH), Bethesda, MD, USA) on a personal computer.
The mean fluorescence intensity for treatment was calculated on 50 nuclei LEF-1 (+) at 200 × magnification using ImageJ software Version 1.50i (NIH, Bethesda, MD, USA) (integrated density, ID).
The background was obtained by measuring the fluorescence intensity of regions outside the cells. The corrected total cell fluorescence (CTCF) was then determined by subtracting the background from the ID (CTCF=ID−background).15
Statistical analysis
Data were analyzed as mean±s.e. in the different experimental conditions. Data were tested for their statistical significance after evaluating their normal distribution. We used the analysis of variance test with the least significant difference post hoc test to detect statistical differences between the different experimental conditions. Differences were considered statistically significant at P<0.05.
Results
Mature 3T3-L1 adipocytes dedifferentiate to fibroblast-like cells after co-culture with A375 melanoma cell line
In order to study the crosstalk between adipocytes and melanoma cancer cells, we used a co-culture model.
After 3 and 6 days of co-culture of 3T3-L1 adipocytes and A375, we observed the appearance of fibroblast-like cells (Figures 1c and d and detail in Figure 1g), which were absent in control conditions (Figures 1a and b). During co-culturing, mature adipocytes progressively lost a considerable amount of lipid droplets, the nuclei became more centralized and the cells became elongated in shape, similar to a fibroblast morphology (Figure 1g). In particular, the number of fibroblast-like cells significantly increased at PID 11, after 6 days of co-culture, compared with control cultures of 3T3-L1 adipocytes (Figure 1l). This increased number of fibroblast-like cells was registered at the same time with a progressively decreasing number of mature adipocytes (Figures 1h) with a significant reduction in lipid droplets' content and size (Figure 1f), when compared with control cells (Figure 1e).
Morphological changes of 3T3-L1 adipocytes during co-culture with A375 cells. Using Red Oil O staining, we showed a progressive change in morphology of 3T3-L1 cells in co-culture with A375 cells (c,d) versus control adipocytes (a,b) from PID 8 to PID 11 (100 × magnification, scale bar 50 μm). Co-cultured adipocytes presented a progressive reduction in number (h) and area (i) when compared with control conditions. At the same time points, there was a progressive increase in the number of fibroblast-like cells (j) in co-culture conditions not present in controls. In (e–g) are presented images, respectively, of a control adipocyte, a co-culture adipocyte and a dedifferentiated cell (400 × magnification, scale bar 10 μm). PID, post-induction day. *P<0.05.
In order to investigate the changes in the gene expression profile of dedifferentiated adipocytes, we analyzed the expression of mature adipocyte and fibroblast-specific markers using RT-PCR. After 6 days of co-culture, we observed a significant decrease in adiponectin and GLUT4 expression, when compared with controls (Figure 2a). Moreover, MMP2 and α-SMA expression significantly increased after 6 days of co-culture (Figure 2a). Finally, using RT-PCR assay, we analyzed the expression of genes required for the cell-reprogramming process, such as Klf4 and c-Myc, and we found a significant increase in the expression of these genes (Figure 2a).
Functional changes of 3T3-L1 adipocytes in co-culture compared with control cells. (a) RT-PCR analysis showed that 3T3-L1 adipocytes co-cultured with A375 melanoma cells presented a significantly lower expression of mature adipose-specific genes after 6 days of co-culture (PID 11), a higher gene expression of fibroblast-specific markers and of reprogramming genes, when compared with controls. (b) At PID 11 co-cultured adipocytes presented a decrease in glycerol release in culture medium, compared with controls, in the lipolysis assay. Data are presented as mean±s.e. PID, post-induction day; RT-PCR, real-time PCR.
To characterize further morphological and functional changes observed in 3T3-L1 adipocytes in co-culture, we measured glycerol release in culture medium after 3 and 6 days. Glycerol release significantly decreased in co-culture compared with control adipocytes at PID 8 and 11 (Figure 2b).
We further tried to describe, even though indirectly, the metabolic changes in this experimental setting by measuring the pH changes in the medium after co-culture. We found that after 3 and 6 days of co-culture of 3T3-L1 adipocytes with cancer cells, the pH of the medium was significantly reduced, when compared with the control medium of adipocytes grown alone (PID 8: control pH 7.2 versus co-culture pH 7; PID 11: control pH 7.2 versus co-culture pH 6.8; data not shown in figure).
3T3L-1 adipocytes and melanoma invasiveness and migratory capacity
A scratch test was used to determine the migratory capacity of the A375 melanoma cells in conditions of co-culture with 3T3-L1 adipocytes, compared with controls. From a time-lapse movie, it is evident that the movement of melanoma cells after co-culture is significantly greater than that in control cells (Supplementary Figure 1). In fact, the cells grown in co-culture medium during the 72 h of the test time, migrate and distribute to nearly fill the furrow created at the beginning of the experiment (Figure 3c); in control conditions at the end of the 72 h the furrow was still visible (Figure 3a).
3T3L-1 adipocytes and melanoma invasiveness and migratory capacity. (a–d) Scratch test images at the end of the test (72 h) to determine the migratory capacity of the A375 melanoma cells in control conditions (a), after exposure to adipocyte medium (b), co-culture medium (c) and co-culture medium plus SFRP-5 protein (d). (e) Invasion test on Matrigel of A375 melanoma cells alone and after co-culture with 3T3-L1 adipocytes, with and without SFRP-5; the test was conducted in the presence and absence of FBS. (f) Western blot analysis of Akt phosphorylation in the cytosol of melanoma cells after 6 days of co-culture with adipocytes as compared with controls.
To study further the influence of adipocytes on the migratory capacity of melanoma cells, we performed an invasion assay in Matrigel (Figure 3e). The melanoma cells grown in co-culture medium show a percentage of migration in Matrigel that was significantly greater than that in control cells (Figure 3e).
3T3L-1 adipocytes and melanoma-invasive and migratory capacity after inhibition with SFRP-5
As it is known in the literature that melanoma cells secrete Wnt5a and that this is directly related to the aggressiveness of the tumor, we hypothesized an involvement of this pathway in the increased cell migration observed in our experiment.21, 22
We thus repeated the Scratch Test using melanoma cells grown in control medium, in conditioned medium from adipocytes and in co-culture medium with and without treatment with SFRP-5, a Wnt5a inhibitor (Figure 3d). The migration of A375 melanoma cells increased in cells grown in adipocyte medium (Figure 3b) and even more so in co-culture medium (Figure 3c), as compared with the controls (Figure 3a). Interestingly, migration was instead reduced in melanoma cells treated with co-culture medium and addition of SFRP-5 (Figure 3d).
In the hypothesis that the increased motility observed in melanoma cells after co-culture was induced by the activation of the Wnt5a pathway, we repeated the invasion test in Matrigel after adding SFRP-5 protein to the medium (Figure 3e). The percentage of migration of melanoma cells grown in co-culture and treated with SFRP-5 was significantly reduced compared with cells grown in co-culture (Figure 3e).
Pathways involved in the crosstalk between melanoma and adipocytes mediating the increased migratory and invasive capacity of melanoma cells
To characterize further the molecular signaling activated in the crosstalk between melanoma and adipocytes, we studied the expression of the pathway of the β-catenin (Figure 4). This pathway has been associated with phenotypes of more aggressive melanoma.23, 24, 25 The activation of the pathway of the β-catenin is dependent on the activation of AKT.25 When phosphorylated, Akt inhibits the phosphorylation of β-catenin and, consequently, its proteasome degradation; the β-catenin can thus translocate to the nucleus activating the expression of different genes promoting migration and invasiveness capacity of melanoma cells (Figure 4).25 Using western blot analysis we confirmed an increase in phosphorylation of Akt in the cytosol of melanoma cells after 6 days of co-culture with adipocytes, when compared with controls (Figure 3f).
Possible pathway involved in the crosstalk between adipocytes and melanoma cells. When Wnt binds to its cell surface receptor, Akt is phosphorylated, inhibiting the phosphorylation of β-catenin and consequently its proteasome degradation; the β-catenin can thus translocate to the nucleus activating the expression of different genes promoting migratory and invasive capacity of melanoma. The activation of WNT5a receptor and downstream signaling is prevented by the binding with its inhibitor SFRP-5. SFRP-5, secreted frizzled-related protein 5.
We then analyzed the expression of β-catenin in melanoma cells under the different experimental conditions by immunofluorescence and, in particular, in A375 cells cultivated in control medium (Figure 5a), in medium from adipocytes (Figure 5b) and in medium from co-culture experiments (Figure 5c). The nuclear expression of β-catenin in melanoma cells grown in normal medium is very low (Figure 5a); in contrast, there is an increased nuclear expression of β-catenin in cells grown in medium derived from the culture of adipocytes (Figure 5b) and even more in A375 cells grown in the co-culture medium (Figure 5c).
Immunofluorescence analysis of β-catenin nuclear expression in melanoma cells under different experimental conditions. (a–d) Expression of β-catenin in melanoma cells in A375 cells cultivated in control medium (a), in medium from adipocytes (b) and in medium from co-culture experiments (c) with their specific quantification (d). (e) Western blot analysis of β-catenin protein in nuclear extracts of A375 melanoma cells grown in co-culture medium, compared with A375 cells grown in medium from adipocytes and in control medium.
In line with these results we found using western blot analysis, there was a significant increase in β-catenin protein in nuclear extracts of A375 melanoma cells grown in co-culture medium, compared with A375 cells grown in medium from adipocytes and in control medium (Figure 5e).
To characterize further the molecular pathways activated in the crosstalk between melanoma and adipocytes, we studied the expression of LEF-1 by IF and WB under the same experimental conditions. LEF-1 is a nuclear protein that binds to β-catenin in the nucleus to determine the activation of different target genes25 (Figure 4).
Figure 6 shows the expression of LEF-1 under the different experimental conditions in IF. LEF1 expression is localized only at the nuclear level. A375 melanoma cells grown in co-culture medium (Figure 6c) again showed a significantly increased nuclear expression of LEF1 compared with melanoma cells grown in control medium (Figure 6a). These data were also confirmed using western blot analysis (Figure 6e) and they showed a significantly greater expression of LEF-1 in the nuclear extract of melanoma cells treated with co-culture medium, when compared with controls.
Immunofluorescence analysis of LEF-1 nuclear expression in melanoma cells under the different experimental conditions. (a–d) Expression of LEF-1 in melanoma cells in A375 cells cultivated in control medium (a), in medium from adipocytes (b) and in medium from co-culture experiments (c) with their specific quantification (d). (e) Western Blot analysis of LEF-1 protein in nuclear extracts of A375 melanoma cells grown in co-culture medium, compared with A375 cells grown in medium from adipocytes and in control medium.
Discussion
The study of the dynamic interaction between cancer cells and the tumor stroma itself has received growing attention, as several aspects of cancer progression, such as invasiveness and metastasization, as well as therapeutic resistance, may be linked to reciprocal and specific interactions between cancer cells and their TME components.
TMEs involve a multifaceted collection of cells composed of CAFs, endothelial cells and inflammatory cells.13 Even though an increasing number of cancers have been epidemiologically associated with excess adiposity1, 2, 3, 4, 5 and even though a great number of them grow in the proximity of ectopic and/or dysfunctional fat depots,1, 7, 8 the role of adipocytes in the TME has been confirmed and studied for just a few types of cancers, in particular in breast,1, 11, 14, 17 pancreatic,11, 15 esophageal,8, 11 colon8, 11 and melanoma cancer.16 Different systemic and local mechanisms have been hypothesized in the physiopathological association between excess adiposity and cancer.1, 7, 8, 11 Only a few studies have tried to face this complexity, focusing, for example, on the different roles of different fat depots in cancer,26, 27 with interesting but, in some ways, preliminary data.
The study of the crosstalk between adipocytes and melanoma cells in this in vitro model of co-culture described for the first time the existence of phenomena of reprogramming of adipocytes toward cells resembling those of mesenchymal ones, for their morphological and functional characteristics.
The unique and principal function of adipocytes is to store energy in the form of triglycerides and to release fatty acids for other tissues and organs.9 In the TME the fatty acids released from adipocytes can provide energy for rapid tumor growth and support the high proliferation rate of cancer cells, which has also been confirmed by fluorescently labeled studies conducted in melanoma cancer lines.16
In our experiment we measured the rate of glycerol release and found a significant decrease in the rate of lipolysis in parallel with the dedifferentiation of adipocytes into fibroblast-like cells. Moreover, with the appearance of fibroblast-like cells in co-culture, we observed significant acidification in the culture medium, which probably reflects a profound metabolic change in the TME. As previously described in another similar experiment,15 the dedifferentiation process leads to a reduction in content and size of mitochondria, which supports a shift toward a more glycolytic metabolism of the cells. Other in vitro studies demonstrate that CAFs provide critical metabolites for tumor growth and undergo metabolic reprogramming to support a metabolic switch from oxidative phosphorylation to aerobic glycolysis;28 this process is also identified as the reverse Warburg effect and could be induced by the crosstalk with tumoral cells.28 This variation in energy metabolism leads to an increased production of lactate and ketone bodies with acidification of the TME favoring angiogenesis and increasing cell proliferation of cancerous cells.28, 29
The literature supports a critical role for CAFs not only in cancer metabolism but also in influencing extracellular matrix quality and composition.11, 12 Extracellular matrix quality has been shown to be crucial in determining cancer cell migration and invasion, the local immune response and the release of different growth factors and cytokines, which ultimately promotes tumor growth, angiogenesis and invasiveness.11, 17, 30
It has recently been suggested that, during their interaction with cancer cells, adipocytes in the TME can be reprogrammed into CAAs or dedifferentiate into ‘fibroblast-like cells’.8, 11, 12 However, this phenotypic shift from CAA to CAF has been demonstrated only for breast cancer,14, 17 and very little data are available in the literature about other types of cancers.15, 17 We previously showed a shift of adipocytes to fibroblast-like cells in a model of co-culture of pancreatic cancer cells and adipocytes.15 In line with these observations are those of Tan et al.,14 who speculated that CAFs may originate from CAAs. In this study, after co-culture with A375 melanoma cells, adipocytes showed once more morphological changes of fibroblast-like cells with the loss of specific adipocyte markers and the expression of characteristic fibroblasts and reprogramming genes.
This crosstalk between melanoma cells and dedifferentiated adipocytes profoundly influences the migratory capacity of melanoma cells in culture. One of the pathways central to the modulation of this crosstalk was the Wnt pathway. We showed that this increased invasiveness of cancer cells was prevented by the treatment of co-culture with SFRP-5, a receptorial inhibitor of Wnt. Moreover, we found a significantly greater phosphorylation of Akt and an increased expression of β-catenin and LEF-1 in melanoma cells in co-culture.
Wnt signaling is one of the key cascades that regulates cancer stemness, metastasis and immune surveillance, and mutations in the Wnt pathway occur frequently in human cancers.24, 25 It is interesting to note that also in human obesity circulating concentrations of WNT5a are increased and that noncanonical Wnt signaling is activated,31 probably contributing to the pro-inflammatory state in visceral AT.
Wnt ligands bind to their receptors on the cell surface and transduce signals through at least three distinct paths;24, 25 among these pathways, the ß-catenin has been extensively studied. When Wnt binds to its cell surface receptor, Akt is phosphorylated, inhibiting the phosphorylation of β-catenin and consequently its proteasome degradation; the β-catenin can thus translocate to the nucleus activating the expression of different genes promoting the migratory and invasive capacity of melanoma cells such as c-Myc, cyclin D1, c-Jun, matrix metalloproteinase-1 (MMP-1) and MMP-7.24, 25
In mouse mutant models, activated ß-catenin leads to accelerated melanoma development, promotion and metastasis.32 It has recently been shown that in malignant melanoma cell lines, treatment with recombinant Wnt5a induces the release of exosomes containing inflammatory and pro-angiogenic molecules as interleukin-6, VEGF and MMP2.33 Moreover, interleukin-6 may induce the expression of Wnt5a in melanoma cells itself to form a positive loop.34
In our study we showed that dysfunctional adipocytes undergoing dedifferentiation might also contribute to these signals in the TME, as they produce inflammatory molecules and metalloproteinases. It could be hypothesized that excess adiposity with its local inflammatory milieu could be a potential trigger or, at least, an amplifier of processes involved in cancer growth and development.
Some limitations to the present study and future lines of development of the present findings should be acknowledged. Even though mixed models of co-cultures have already been used in the literature,35 the results of this experiment should be confirmed in future in vitro studies using human adipocytes. Secondly, these in vitro data should be translated into in vivo studies taking into account different fat depot and AT close to lymphonodes, in patients with different disease stages. Moreover, the influence of excess adiposity with the systemic production of adipokines and inflammatory mediators should be taken into account as other possible modulators of the relationship between adipocytes and cancer cells in the microenvironment as well.
In conclusion, the data presented in this paper allow us to hypothesize a dedifferentiation process of adipocytes toward fibroblast-like cells, which can promote migration and metastasis of melanoma cells, through activation of Wnt5a and of the intracellular pathways of β-catenin and LEF-1, as a possible focus for future research and potential target in the modulation of the physiopathological processes of cancer growth, invasiveness and metastasis.
References
Renehan A, Zwahlen M, Egger M . Adiposity and cancer risk: new mechanistic insights from epidemiology. Nature Rev Cancer 2015; 15: 484–498.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M . Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371: 569–578.
Wang J, Yang DL, Chen ZZ, Gou BF . Associations of body mass index with cancer incidence among populations, genders, and menopausal status: a systematic review and meta-analysis. Cancer Epidemiol 2016; 42: 1–8.
Freisling H, Arnold M, Soerjomataram I, O'Doherty MG, Ordóñez-Mena JM, Bamia C et al. Comparison of general obesity and measures of body fat distribution in older adults in relation to cancer risk: meta-analysis of individual participant data of seven prospective cohorts in Europe. Br J Cancer 2017; 116: 1486–1497.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K et al.Body fatness and cancer—viewpoint of the IARC working group. N Engl J Med 2016; 375: 794–798.
Sergentanis TN, Antoniadis AG, Gogas HJ, Antonopoulos CN, Adami H, Ekbom A et al. Obesity and risk of malignant melanoma: a meta-analysis of cohort and case–control studies. Eur J Cancer 2013; 49: 642–657.
Calle EE, Kaaks R . Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 2004; 4: 579–591.
Nieman KM, Romero IL, Van Houten B, Lengyel E . Adipose tissue and adipocytes support tumorigenesis and metastasis. Bioch Biophys Acta 2013; 1831: 1533–1541.
Fischer-Posovszky P, Wabitsch M, Hochberg Z . Endocrinology of adipose tissue—an update. Horm Metab Res 2007; 39: 314–321.
Pollak M . The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat Rev Cancer 2012; 12: 159–169.
Park J, Euhus DM, Scherer PE . Paracrine and endocrine effects of adipose tissue on cancer development and progression. Endocr Rev 2011; 32: 550–570.
Whipple CA . Tumor talk: understanding the conversation between the tumor and its microenvironment. Cancer Cell Microenviron 2015; 26: e773.
Balkwill FR, Capasso M, Hagemann T . The tumor microenvironment at a glance. J Cell Sci 2012; 125: 5591–5596.
Tan J, Buache E, Chenard MP, Dali-Youcef N, Rio MC . Adipocyte is a non-trivial, dynamic partner of breast cancer cells. Int J Dev Biol 2011; 55: 851–859.
Zoico E, Darra E, Rizzatti V, Budui S, Franceschetti G, Mazzali G et al. Adipocytes Wnt-5a mediated dedifferentiation: a possible target in pancreatic cancer microenvironment. Oncotarget 2016; 7: 20223–20235.
Kwan HY, Fu X, Liu B, Chao X, Chan CL, Cao H et al. Subcutaneous adipocytes promote melanoma cell growth by activating the Akt signaling pathway: role of palmitic acid. J Biol Chem 2014; 289: 30525–30537.
Bochet L, Lehuede C, Dauvillier S, Wang YY, Dirat B, Laurent V et al. Adipocyte-derived fibroblasts promote tumor progression and contribute to the desmoplastic reaction in breast cancer. Cancer Res 2013; 73: 5657–5668.
Cinti S . Transdifferentiation properties of adipocytes in the adipose organ. Am J Physiol Endocrinol Metab 2009; 297: E977–E986.
Matsumoto T, Kano K, Kondo D, Fukuda N, Iribe Y, Tanaka N et al. Mature adipocyte-derived dedifferentiated fat cells exhibit multilineage potential. J Cell Physiol 2008; 215: 210–222.
Szabó P, Kolář M, Dvořánková B, Lacina L, Gabius HJ, Strnad H et al. Mouse 3T3 fibroblasts under the influence of fibroblasts isolated from stroma of human basal cell carcinoma acquire properties of multipotent stem cells. Biol Cell 2011; 103: 233–248.
Da Forno PD, Jh Pringle, Hutchinson P, Osborn J, Huang Q, Potter L et al. WNT5A expression increases during melanoma progression and correlates with outcome. Clin Cancer Res 2008; 14: 5825–5832.
Weeraratna AT, Jiang Y, Hostetter G, Rosenblatt K, Duray P, Bittner M et al. Wnt5a signaling directly affects cell motility and invasion of metastatic melanoma. Cancer Cell 2002; 1: 279–288.
Spranger S, Bao R, Gajewski TF . Melanoma-intrinsic b-catenin signalling prevents anti-tumour immunity. Nature 2015; 523: 231–235.
Zhan T, Rindtorff N, Boutros M . Wnt signaling in cancer. Oncogene 2017; 36: 1461–1473.
Klaus A, Birchmeier W . Wnt signalling and its impact on development and cancer. Nat Rev Cancer 2008; 8: 387–398.
Trevellin E, Scarpa M, Carraro A, Lunardi F, Kotsafti A, Porzionato A et al. Esophageal adenocarcinoma and obesity: peritumoral adipose tissue plays a role in lymph node invasion. Oncotarget 2015; 6: 11203–11215.
Zoico E, Budui SL, Rizzatti V, Franceschetti G, Darra E, Pedrazzani C et al. Immunophenotipical changes and browning phenomena in the peri-tumoral adipose tissue of colorectal cancer patients. Obesity doi:10.1002/oby.22008.
Zhang D, Wang Y, Shi Z, Liu J, Sun P, Hou X et al. Metabolic reprogramming of cancer-associated fibroblasts by IDH3α downregulation. Cell Rep 2015; 10: 1335–1348.
Fiaschi T, Marini A, Giannoni E, Taddei ML, Gandellini P, De Donatis A et al. Reciprocal metabolic reprogramming through lactate shuttle coordinately influences tumor-stroma interplay. Cancer Res 2012; 72: 5130–5140.
Ishii G, Ochiai A, Neri S . Phenotypic and functional heterogeneity of cancer-associated fibroblast within the tumor microenvironment. Adv Drug Deliv Rev 2016; 99: 186–196.
Catalán V, Gomez-Ambrosi J, Rodriguez A, Perez-Hernandez AI, Gurbindo J, Ramirez B et al. Activation of noncanonical Wnt signaling through WNT5a in visceral adipose tissue of obese subjects is related to inflammation. J Clin Endocrinol Metab 2014; 99: E1407–E1417.
Damsky WE, Curley DP, Santhanakrishnan M, Rosenbaum LE, Platt JT, Gould Rothberg BE et al. β-catenin signaling controls metastasis in Braf-activated Pten-deficient melanomas. Cancer Cell 2011; 20: 741–754.
Ekström E, Bergenfelz C, von Bülow V, Serifler F, Carlemalm E, Jönsson G et al. WNT5A induces release of exosomes containing pro-angiogenic and immunosuppressive factors from malignant melanoma cells. Mol Cancer 2014; 13: 88.
Linnskog R, Jönsson G, Axelsson L, Prasad CP, Andersson T . Interleukin-6 drives melanoma cell motility through p38α-MAPK-dependent up-regulation of WNT5A expression. Mol Oncol 2014; 8: 1365–1378.
Dirat B, Bochet L, Dabek M, Daviaud D, Dauvillier S, Majed B et al. Cancer-associated adipocytes exhibit an activated phenotype and contribute to breast cancer invasion. Cancer Res 2011; 71: 2455–2465.
Acknowledgements
We thank Professor Mark Newman who corrected the English of the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Zoico, E., Darra, E., Rizzatti, V. et al. Role of adipose tissue in melanoma cancer microenvironment and progression. Int J Obes 42, 344–352 (2018). https://doi.org/10.1038/ijo.2017.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.218
- Springer Nature Limited
This article is cited by
-
Melanoma cells induce dedifferentiation and metabolic changes in adipocytes present in the tumor niche
Cellular & Molecular Biology Letters (2023)
-
Focus on dedifferentiated adipocytes: characteristics, mechanisms, and possible applications
Cell and Tissue Research (2019)