Abstract
Objective:
The main objective of this study was to investigate whether children's perceptions of neighborhood safety are associated with their weight status and weight-related behaviors, independently of their parents' perceptions.
Methods:
Data were from the baseline wave (collected in 2005–2008) of the Quebec Adipose and Lifestyle Investigation in Youth (QUALITY), an ongoing prospective study of 630 children aged 8–10 years (from Quebec, Canada) at risk of obesity. Weight and height were measured, and World Health Orgaization age- and sex-specific body mass index (BMI) z-scores were computed. Physical activity was measured by accelerometry, and time spent watching television, playing computer and video games during week and weekend days was self-reported. Structural equation modeling was used to simultaneously estimate the associations between parent and child perceived safety, with children's BMI z-score, physical activity and screen time.
Results:
The results suggest that, when parent perceived safety was at the mean, children who perceived their neighborhood as being safest had nearly an additional 70 daily activity counts per minute (representing an ~10% increase in overall physical activity level) compared with children who perceived it as being least safe. Among children who perceived a mean level of safety, those whose parents perceived their neighborhood as being safest spent approximately an hour less per day in front of screens compared with those whose parents perceived their neighborhood as being least safe. Parent and child perceptions of safety both indirectly contribute to children's weight status by differentially impacting weight-related behaviors.
Conclusion:
Findings indicate that targeting both parent and child perceived neighborhood safety could bolster efforts to promote healthy weight and weight-related behaviors among children.
Similar content being viewed by others
Introduction
Approximately one in three Canadian youth aged between 5 and 17 years are overweight or obese,1 representing nearly a doubling of the proportion observed in the late 1970s.2 This increase has drawn attention to declining levels of youth physical activity and increasing sedentary behavior. Current guidelines recommend that youth engage in 60 min of moderate- to vigorous-intensity physical activity per day and limit their time spent watching television or on the computer to up to 2 h per day.3, 4 In Canada, under 7% of children and youth meet physical activity guidelines5 and fewer than 20% of youth aged 10 to 16 years meet screen time guidelines.3
A socioecological approach emphasizes targeting the social (e.g., neighborhood disorder) and built environment (e.g., walkability) given their etiological role in the development of obesity.6, 7 The World Health Organization specifically recommends improving perceived neighborhood safety as an evidence-based approach to reduce child obesity levels.8 In the context of child health, perceived safety is a complex concept that can reflect concerns about exposure to concrete threats (e.g., traffic, ‘stranger danger’),9 and also broader experiences (e.g., contact with others in the neighborhood) and individual differences (e.g., income level, ethnicity).10, 11 Generalized beliefs about overall safety therefore capture individuals’ ‘everyday’ model of the experience of safety.12 These generalized perceptions of the environment may be particularly important in explaining psychosocial functioning and health.13
Much of the research on children’s weight and weight-related behaviors has considered associations with objective (e.g., crime rate, traffic flow, street connectivity) or subjective measures of safety based on parents’ reports.9, 10, 14, 15 Parent perceived neighborhood safety is associated with greater physical activity (e.g., outdoor play), decreased screen time and a decreased likelihood of obesity in children.10, 16, 17, 18, 19, 20 Although some of the findings linking neighborhood safety features to weight-related outcomes are inconsistent,11, 21 there is at least some evidence that parents’ perceptions have a role (e.g., due to their ability to restrict children's independent mobility if they perceive the environment as being unsafe).9, 18
Although adults' perceptions of safety are a stronger predictor of their own weight status than objective neighborhood measures,22 little research considers school-aged children's perceptions of safety in relation to their own weight-related outcomes. Children’s perceptions may be more salient as they start to experience greater freedom and autonomy (e.g., in using active transportation to school).9, 23 Children's perceived safety may also have a greater role in linking the environment to their health outcomes, notably through stress pathways.24 Children who feel less safe may experience psychological distress (e.g., depressive and anxious symptoms), which is associated with poorer weight-related behaviors (e.g., decreased physical activity)25 and with poorer health.26
We adopted a child-centered socioecological approach to investigate whether children’s own perceptions of neighborhood safety are associated with overall physical activity level, screen time and weight status. No other study has simultaneously considered independent direct and indirect associations between child and parent perceived safety and child weight-related outcomes. We hypothesized that greater child perceived safety was positively associated with favorable weight-related behaviors (i.e., increased physical activity and decreased screen time), independently of parent perceptions. Moreover, in light of the association between psychological distress and poorer health, we hypothesized that child perceived safety was inversely associated with weight, independently of behaviors. We also consider whether child and parent perceptions interact in predicting weight-related outcomes.
Subjects and methods
Subjects
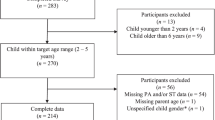
Participants were drawn from the Quebec Adipose and Lifestyle Investigation in Youth (QUALITY) study, an ongoing prospective study of Caucasian families with a child aged 8–10 years (from Quebec, Canada) at risk of childhood obesity, due to the presence of obesity in at least one biological parent. Families were recruited using a population-based sampling strategy that targeted all schools within 75 km of three major Quebec cities (i.e., Montreal, Quebec and Sherbrooke). Of 3350 families who expressed interest in participating, 1320 met the eligibility criteria and 630 of these (48%) completed the baseline visit between September 2005 and December 2008 (see Lambert et al.27 for full details of eligibility and the selection procedure). Data collection occurred during full-day visits at the Unité de recherche clinique du Centre Hospitalier Universitaire (CHU) Sainte-Justine in Montreal and Hôpital Laval in Quebec City, and includes interviewer-administered questionnaires for children, self-administered questionnaires for parents and physiological measurements for both children and parents. The ethics review boards of CHU Sainte-Justine and Laval University approved the study protocol. Because data were only available for the first wave at the time of analysis, this study tests the hypothesized associations using cross-sectional data from the first wave.
Outcome measure: BMI z-score
Anthropometric measurements were taken using a stadiometer for height and an electronic scale for weight. Age- and sex-adjusted BMI z-scores were computed from World Health Organization growth curves.
Main mediating variables: weight-related behaviors
To measure screen time, children were asked to fill the blanks in the following questions: 'usually, during week days, I watch [blank] hours of television per day' and 'usually, during week days, I use the computer (for leisure) and play video games (includes Nintendo, Gameboy, etc) [blank] hours per day'. The same questions were repeated for weekend days (Cronbach's α=0.60). Self-reported screen time shows some reliability among children aged as young as 11 years28 and can more strongly predict adiposity among 8–11 year olds compared with objective measures of overall sedentary time (e.g., based on accelerometry), which capture a range of potentially less adverse sedentary behaviors such as reading or doing homework.29 Weekday and weekend day screen times were summed and weighted to reflect average daily screen time in hours. Physical activity was assessed using an Actigraph LS 7164 activity monitor accelerometer (Actigraph LLC, Pensacola, FL, USA). Accelerometers capture vertical accelerations with magnitude and frequency that detect human motion while filtering out high-frequency movements (e.g., vibrations). Acceleration signals are converted into activity counts. Children were required to wear the accelerometer for 7 days, from the time they woke to the time they went to bed (except when bathing, showering or swimming). Children’s average daily total physical activity was calculated based on total counts per minute, including sedentary minutes (⩽100 counts per minute (c.p.m.)), divided by measured wear time per day. The results of metanalyses suggest that measures of total physical activity—as measured by c.p.m.—are valid predictors of indicators of adiposity (e.g., waist circumference).30 In keeping with recommendations, children who wore the accelerometer for at least 10 h per day, over 4 days, were retained in the analyses.5 Accelerometer data were either missing or incomplete for 95 children. Separate analyses suggested that children with missing or incomplete accelerometer data did not significantly differ from children with complete data in terms of age, sex, family income level, BMI z-score or screen time. For the main analyses, measures of c.p.m. were rescaled to range between 1 and 10.
Parent and child perceived neighborhood safety
Children indicated to what extent they agreed with the statements ‘There is no danger walking around or cycling alone in my neighborhood during the day’ and, in a separate item, ‘at night’ (1=completely agree, 2=somewhat agree, 3=somewhat disagree, 4=completely disagree). These variables correlated positively (r=0.54, P<0.001). As of the age of 6 years, self-reporting of fears is considered a valid approach.31 Parent perceived neighborhood safety was measured based on agreement that their neighborhood ‘is at high risk of crime’, ‘is attractive’ and that ‘kids can play outside without danger’ (1=very true, 5=not at all true). Similar items have been used in previous composite measures reflecting perceived neighborhood safety.11, 32 Because latent variables can only be estimated using a minimum of three indicator items, the models included a reverse-coded mean measure of child perceived safety (high values indicated greater perceived safety) and a latent variable reflecting parent perceived safety (all items loaded significantly, P’s <0.001). These measures are taken to represent global perceived neighborhood safety. Previous research suggests that these measures of parent and child perceived neighborhood safety are reliable and valid as they are moderately correlated, and each predicted by neighborhood safety features and individual differences (e.g., family income, sex, age).32
Covariates
The models included covariates such as children’s age and sex. Because youths’ weight can also be shaped by genes and familial transmission of weight-related behaviors, mother’s weight—a strong predictor of children’s weight—was also included in the analyses.33, 34 Mother’s BMI (kg m−2) was calculated based on measures of weight and height carried out in a clinical setting by a trained nurse. Family income level was considered in the analyses given that low-income families are likely to have fewer resources available to provide their children with a wide range of social and recreational activities, with some evidence suggesting that low-income families tend to be more frequent televiewers, and to more frequently equip children’s rooms with a television set.35 Family income level was assessed based on self-reported total household income in Canadian dollars for the last completed fiscal year, before taxes and deductions (1=<10 000, 2=10 000–14 999, 3=15 000–19 999, 4=20 000–29 999, 5=30 000–39 999, 6=40 000–49 999, 7=50 000–59 999, 8=60 000–79 999, 9=80 000–99 999, 10=100 000–119 999, 11=120 000– 139 999, 12=140 000 and more). Finally, measures of child average daily caloric intake (rescaled to range between 1 and 10) and average number of hours of sleep per night (based on accelerometry data) were included as covariates and as predictors of weight status.
Statistical analysis
The analyses consisted of two structural equation models estimated using MPLUS 5.1. Structural equation modeling is appropriate to test hypothesized structural relations between multiple independent and dependent variables (through the use of estimated regression parameters). Although the use of structural equation model with cross-sectional data cannot lead to establishing causal pathways, this approach is useful for testing the fit of a hypothesized model (including directional associations between variables, and the entire system of variables) with the observed data through goodness-of-fit statistics.36 Structural equation models include both a measurement model and a structural model. The measurement part of the model allows for the estimation of latent variables reflecting constructs of interest. The structural part of the model simultaneously estimates the associations between multiple observed and latent independent and dependent variables.
In the first model (Model 1), a latent variable estimating parent perceived neighborhood safety was used to predict children’s screen time, level of physical activity and BMI z-score. The model also estimated direct pathways from weight-related behaviors to child BMI z-score, and adjusted for mother’s BMI, diet and sleep. In Model 2, children’s own perceived safety was added to the model and allowed to predict both their weight-related behaviors and their BMI z-score. In this model, we used a factor score to represent parent perceived safety and included an interaction term between parent and child perceived safety to predict outcomes. Because of inconsistent evidence on the direction of the association between children’s screen time and level of physical activity, these two variables were allowed to correlate.37 Both models adjusted for child age, sex and family income, and maternal BMI was allowed to correlate with family income. For the sake of visual clarity, figures depicting the estimated models only show estimated pathways between key variables. All non-depicted estimated associations between key variables and covariates are reported in Table 1. The analyses were conducted using complete case analysis, with complete data available for 81% of the sample.
Results
Overall descriptive statistics for each of the study variables, as well as by different levels of child perceived safety, are shown in Table 2. Children’s mean age was 9.12 years (s.d.=0.91) and 45.6% were girls. On average, children perceived their neighborhood as being moderately safe (mean=2.57, s.d.=0.93), with ~47% of children in complete agreement that there was no danger to walk or to cycle alone during the day. Parents also perceived a substantial degree of safety, with 42% reporting that it was ‘very true’ that children could play outside in the neighborhood without danger. On average, children's physical activity levels as measured by c.p.m. (M=589.35, s.d.=186.55) were consistent with averages reported for similarly aged children, whereas screen time (M=2.72, s.d.=1.94) was slightly above average.38, 39, 40 Median family income was between CAD$80 000 and 99 000.
The results of Model 1 (N=513, χ2=30.12, degrees of freedom=27, P>0.05, CFI (comparative fit index)=0.99, RMSEA (root mean square error of approximation)=0.02) suggested that children of parents who perceived their neighborhood as being safer spent less time in front of screens, after adjusting for child level of physical activity and other covariates (see Figure 1). However, children of parents who perceived more safety were not more likely to engage in physical activity after adjusting for screen time and other covariates. Parent perceived safety was not directly associated with their child’s BMI z-score after adjusting for weight-related behaviors and covariates, but had a marginally significant indirect association through screen time (indirect effect B=−0.03, P=0.06). Children’s BMI z-score was most strongly associated with their screen time, physical activity and mother’s BMI.
Model depicting the associations between parent perceived safety, child screen time, physical activity and BMI z-score (Model 1). Ovals represent latent variables, rectangles represent manifest variables. Although not depicted in the model, child age, sex, family income and parent perceived safety were allowed to predict diet and sleep. Diet and sleep were included as predictors of BMI z-score, and were allowed to correlate with each other, with maternal BMI and with other weight-related behaviors (results available upon request). *P<0.05; **P<0.01; ***P<0.001.
In Model 2 (N=513, χ2=14.86, df=16, P>0.05, CFI=1, RMSEA=0.00) (see Figure 2), children’s own perceptions of neighborhood safety and an interaction term with parent perceptions were added to the model. Because physical activity was the only outcome that was significantly associated with the interaction term, no paths were estimated with screen time and BMI. When parents perceived a mean level of neighborhood safety, children who perceived their neighborhood as being safer were more physically active. After adjusting for parent perceived safety, there was no association between child perceived safety and screen time, nor with BMI z-score. Child perceived safety was marginally significantly indirectly associated with BMI through physical activity (indirect effect B=−0.02, P=0.07). Parents’ perceptions of neighborhood safety continued to be significantly associated with screen time.
Model depicting the associations between parent and child perceived safety, child screen time, physical activity and BMI z-score (Model 2). The black dot (●) represents the interaction term between parent and child perceived safety. Although not depicted, child age, sex, family income and child and parent perceived safety were allowed to predict diet and sleep. Diet and sleep were included as predictors of BMI z-score, and were allowed to correlate with each other, with maternal BMI and with other weight-related behaviors (results available upon request). *P<0.05; **P<0.01; ***P<0.001.
Although parent perceived safety was not directly associated with physical activity, there was a significant interaction with child perceptions. Predicted values suggested that children's perceptions were particularly important in explaining physical activity when parents perceived lower levels of safety (see Figure 3).
Predicted values of daily screen time (in h) and physical activity (in c.p.m.) were estimated using regression coefficients from a separate model that reestimated Model 2 using non-rescaled values for physical activity. Predicted values were for a 9-year-old boy and a 9-year-old girl, with a median family income. Values for child and parent perceived safety were held at the minimum, mean and maximum, respectively.
Substantively, when parents perceived a mean level of safety, a child who perceived the most safety had approximately an additional 70 daily activity counts per minute compared to one who perceived the least safety. This increase represented about a 10 percentage point increase in overall physical activity level. When children perceived a mean level of safety, a child of parents who perceived the most safety also spent on average approximately an hour less per day in front of screens compared with one whose parents perceived the least safety.
Children’s age, sex, family income and parent perceived neighborhood safety accounted for 11.1% of the variance in children’s perceptions of neighborhood safety. Family income alone accounted for 4.5% of the variance in parents’ perceived neighborhood safety. Taken together, children’s age and sex, family income, parent and child perceived safety accounted for 15% of the variance in child levels of physical activity and 7.8% of the variance in screen time. The full model, including mother’s BMI, diet and sleep, in turn, explained 11.7% of the variance in children’s BMI z-score.
Discussion
Previous research suggests that parent perceived neighborhood safety is an important determinant of children's weight-related behaviors and weight. Parents exert a degree of control over their child's behavior and may limit their children’s independent mobility if they perceive the neighborhood as being unsafe. This study tested the hypothesis that school-aged children's own perceived safety may also be associated with their weight-related behaviors and weight, as they begin to exert some autonomy and freedom in their preferences and behaviors.
Our results suggest that parents’ perceived neighborhood safety was more important in explaining children’s screen time, whereas children’s perceived neighborhood safety was more important in explaining their level of physical activity as measured by an accelerometer. Parent and child perceived neighborhood safety had marginally significant independent indirect associations with children’s BMI z-score through weight-related behaviors.
The findings stand in contrast to previous research, which suggests inconsistent associations between neighborhood safety features and weight-related outcomes,11, 18 and at best that parental perceptions of safety are more important than youths' perceptions in predicting their level of physical activity.9, 18, 41 However prior research had at times relied solely on concerns about specific types of safety issues (e.g., stranger danger, traffic), or on parent reports or objective measures (e.g., crime rates) of neighborhood safety, and neglected to simultaneously consider children’s perceptions. Our study’s use of broader measures of perceived safety and sophisticated statistical modeling techniques may have allowed for a more nuanced exploration of the associations between generalized parent and child experiences of safety, child weight-related behaviors and weight status.
Our findings identify different pathways linking perceived neighborhood safety to children’s weight. The association between parent perceived lack of safety and children’s increased screen time could suggest that parents who are concerned about their child’s safety allow their children to spend more time in front of screens, or restrict children’s outdoor activities, resulting in more time spent indoors in front of screens. The direct association between children’s perceived lack of safety and lower levels of physical activity could suggest decreased interest in physical activity. Although our study adjusted for sleep and diet, the study did not consider potential psychological pathways linking feeling unsafe to weight-related behaviors and weight. Previous research suggests that children who feel less safe may experience more psychophysiological distress.26, 42 Psychological distress or depressive symptoms have been found to be associated with lower levels of physical activity in prospective longitudinal research,43 potentially because of the affective components of depression (e.g., sadness, the loss of ability to experience pleasure).44
The findings also suggest that children's perceptions of safety may have a greater role in explaining physical activity levels when they live in a neighborhood that their parents deem unsafe. It may also be the case that neighborhood features come to differentially affect children’s weight-related outcomes through parent and child perceptions of safety. For instance, parents may limit their child’s outdoor play because of safety concerns related to traffic, which is less likely to be an ongoing major preoccupation among children themselves.41 Previous findings suggest that distinct neighborhood features help explain parent and child perceived safety,32 and may therefore have separate or additive effects on children’s and parents' perceptions of safety. Alternatively, we cannot exclude the possibility that the differences in measures used to capture parent and child perceived safety led to measuring substantively different aspects of perceived safety.
As in previous studies, the findings provide evidence that family income is positively associated with parent and child perceived safety.18, 41 Individuals with lower incomes are less likely to feel safe45 and are more likely to live in disadvantaged areas that are more densely populated, and perceived as being less attractive and less safe.46 In separate analyses, we used a spatial data infrastructure32 to explore the associations between physical (e.g., trees, lighting) and social (e.g., proportion of low-income and lone-parent households) neighborhood features, children’s perceived safety and weight-related outcomes. The results suggested that some neighborhood features were associated with weight-related behaviors, but we interpret these results with caution owing to the introduction of potential biases linked to missing data. Future research could further investigate whether neighborhood features and other factors, such as individual characteristics (e.g., integration in a social network, poorer health),47 contribute to children’s perceived safety and weight-related outcomes. Moreover, although the association between parent and child perceived safety and individual differences (e.g., family income, child age and sex) suggests some validity for our global measures of perceived safety, further research on the reliability of these measures is warranted.
As with all studies, some methodological limitations need to be acknowledged. The families involved in this study were Caucasian and were relatively more affluent than the average Quebec family.27 Still, the families lived in residential neighborhoods that varied substantially with regard to socioeconomic disadvantage,48 with concordant observed variance in perceptions of safety in the present study. By design, families were selected into the study based on the presence of parental obesity; although the generalizability of our findings is unknown, its relevance and timeliness is unquestionable, as ~1/3 of adults and children in Canada are overweight or obese.1 The study, although not representative, makes an important contribution toward identifying socioenvironmental features associated with poorer weight-related behaviors for children at risk of obesity. Last, future research using more objective measures for screen time and investigating whether the observed associations are particularly pronounced for 'out-of-school' weight-related behaviors that take place in the residential neighborhood is also warranted.
To counter rising rates of childhood obesity, national and international agencies recommend improving parent perceived safety and that parents of children aged 5–11 years encourage their children to engage in a number of independent physical activities such as walking to school, using active forms of transportation (e.g., skateboarding, cycling or running) and doing outdoor activities (e.g., raking leaves, shoveling snow).8, 49 This study suggests that both parent and child perceptions of a lack of safety could act as barriers for children’s healthy weight-related behaviors. Although parents and children may face actual security threats (e.g., major roadways), evidence suggests that perceptions of safety are particularly important in explaining health outcomes.9 Improving parent and child perceived safety by targeting neighborhood features, for instance, reducing signs of physical and social disorder (e.g., graffiti, litter, dilapidated housing)50, 51 and increasing neighborhood greenery,52 should be part of comprehensive interventions to increase child levels of physical activity, reduce screen time and promote healthy weights. Implementing such environmental interventions to reduce overweight in childhood and adolescence may have long-term benefits in preventing adverse health conditions in adulthood, such as cardiovascular and chronic disease.53
References
Statistics Canada Canadian Health Measures Survey: Cycle 2 Data Tables 2009 to 2011. Statistics Canada: Ottawa, Canada, 2013.
Shields M . Overweight and obesity among children and youth. Health Rep 2006; 17: 27–42.
Mark AE, Boyce WF, Janssen I . Television viewing, computer use and total screen time in Canadian youth. Paediatr Child Health 2006; 11: 595.
Tremblay MS, Warburton DE, Janssen I, Paterson DH, Latimer AE, Rhodes RE et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab 2011; 36: 36–46.
Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS . Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep 2011; 22: 15–23.
Booth KM, Pinkston MM, Poston WS . Obesity and the built environment. J Am Diet Assoc 2005; 105: S110–S117.
Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters SM, McCaslin C, Joyce R et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med 2013; 95: 106–114.
Schoeppe S, Braubach M . Tackling Obesity by Creating Healthy Residential Environments. World Health Organization: Geneva, Switzerland, 2007.
Carver A, Timperio A, Crawford D . Playing it safe: the influence of neighbourhood safety on children's physical activity: A review. Health Place 2008; 14: 217–227.
Bacha JM, Appugliese D, Coleman S, Kaciroti N, Bradley RH, Corwyn RF et al. Maternal perception of neighborhood safety as a predictor of child weight status: The moderating effect of gender and assessment of potential mediators. Int J Pediatr Obes 2010; 5: 72–79.
Foster S, Giles-Corti B . The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Prev Med 2008; 47: 241–251.
Gray E, Jackson J, Farrall S . Reassessing the fear of crime. Eur J Criminol 2008; 5: 363–380.
Daniel M, Moore S, Kestens Y . Framing the biosocial pathways underlying associations between place and cardiometabolic disease. Health Place 2008; 14: 117–132.
Certain LK, Kahn RS . Prevalence, correlates, and trajectory of television viewing among infants and toddlers. Pediatrics 2002; 109: 634–642.
Carson V, Janssen I . Neighborhood disorder and screen time among 10-16 year old Canadian youth: a cross-sectional study. Int J Behav Nutr Phys Act 2012; 9: 66.
Veugelers P, Sithole F, Zhang S, Muhajarine N . Neighborhood characteristics in relation to diet, physical activity and overweight of Canadian children. Int J Pediatr Obes 2008; 3: 152–159.
Weir LA, Etelson D, Brand DA . Parents' perceptions of neighborhood safety and children's physical activity. Prev Med 2006; 43: 212–217.
Ding D, Bracy NL, Sallis JF, Saelens BE, Norman GJ, Harris SK et al. Is fear of strangers related to physical activity among youth? Am J Health Promot 2012; 26: 189–195.
Datar A, Nicosia N, Shier V . Parent perceptions of neighborhood safety and children's physical activity, sedentary behavior, and obesity: evidence from a national longitudinal study. Am J Epidemiol 2013; 177: 1065–1073.
Burdette HL, Whitaker RC . A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics 2005; 116: 657–662.
Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE . Neighborhood environment and physical activity among youth: a review. Am J Prev Med 2011; 41: 442–455.
Christian H, Giles-Corti B, Knuiman M, Timperio A, Foster S . The influence of the built environment, social environment and health behaviors on body mass index. Results from RESIDE. Prev Med 2011; 53: 57–60.
Eccles JS . The development of children ages 6 to 14. Fut Child 1999; 9: 30–44.
Chandola T . The fear of crime and area differences in health. Health Place 2001; 7: 105–116.
Goodman E, Whitaker RC . A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 2002; 110: 497–504.
Hill TD, Ross CE, Angel RJ . Neighborhood disorder, psychophysiological distress, and health. J Health Soc Behav 2005; 46: 170–186.
Lambert M, Van Hulst A, O'Loughlin J, Tremblay A, Barnett TA, Charron H et al. Cohort profile: the Quebec Adipose and Lifestyle Investigation in youth cohort. Int J Epidemiol 2011; 41: 1533–1544.
Lubans DR, Hesketh K, Cliff D, Barnett L, Salmon J, Dollman J et al. A systematic review of the validity and reliability of sedentary behaviour measures used with children and adolescents. Obes Rev 2011; 12: 781–799.
Chaput J-P, Saunders TJ, Mathieu M-È, Henderson M, Tremblay MS, O'Loughlin J et al. Combined associations between moderate to vigorous physical activity and sedentary behaviour with cardiometabolic risk factors in children. Appl Physiol Nutr Metab 2013; 38: 477–483.
Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012; 307: 704–712.
Gullone E . The development of normal fear: a century of research. Clin Psychol Rev 2000; 20: 429–451.
Côté-Lussier C, Jackson J, Kestens Y, Henderson M, Barnett T . A child’s view: social and physical environmental features differentially predict parent and child perceived neighborhood safety. J Urban Health 2015; 92: 10–23.
Cutting TM, Fisher JO, Grimm-Thomas K, Birch LL . Like mother, like daughter: familial patterns of overweight are mediated by mothers' dietary disinhibition. Am J Clin Nutr 1999; 69: 608–613.
Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN . Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004; 158: 342–347.
Warren R . Parental mediation of children's television viewing in low-income families. J Commun 2005; 55: 847–863.
Byrne BM . Structural Equation Modeling with Mplus: Basic Concepts, Applications, and Programming. Routledge: New York, NY, USA, 2013.
Salmon J, Timperio A, Telford A, Carver A, Crawford D . Association of family environment with children's television viewing and with low level of physical activity. Obes Res 2005; 13: 1939–1951.
Dössegger A, Ruch N, Jimmy G, Braun-Fahrländer C, Mäder U, Hänggi J et al. Reactivity to accelerometer measurement of children and adolescents. Med Sci Sports Exerc 2014; 46: 1140–1146.
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M . Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008; 40: 181.
Anderson SE, Economos CD, Must A . Active play and screen time in US children aged 4 to 11 years in relation to sociodemographic and weight status characteristics: a nationally representative cross-sectional analysis. BMC Public Health 2008; 8: 366.
Timperio A, Crawford D, Telford A, Salmon J . Perceptions about the local neighborhood and walking and cycling among children. Prev Med 2004; 38: 39–47.
Lorenc T, Clayton S, Neary D, Whitehead M, Petticrew M, Thomson H et al. Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health Place 2012; 18: 757–765.
Duncan SC, Seeley JR, Gau JM, Strycker LA, Farmer RF . A latent growth model of adolescent physical activity as a function of depressive symptoms. Ment Health Phys Act 2012; 5: 57–65.
Stavrakakis N, de Jonge P, Ormel J, Oldehinkel AJ . Bidirectional prospective associations between physical activity and depressive symptoms. The TRAILS Study. J Adolesc Health 2012; 50: 503–508.
Pantazis C . 'Fear of crime’, vulnerability and poverty. Br J Criminol 2000; 40: 414–436.
Lovasi GS, Hutson MA, Guerra M, Neckerman KM . Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009; 31: 7–20.
Jackson J, Stafford M . Public health and fear of crime a prospective cohort study. Br J Criminol 2009; 49: 832–847.
Van Hulst A, Gauvin L, Kestens Y, Barnett T . Neighborhood built and social environment characteristics: a multilevel analysis of associations with obesity among children and their parents. Int J Obes (Lond) 2013; 37: 1328–1335.
Public Health Agency of Canada. Tips to Get Active: Physical Activity Tips for Children (5–11 years). Available at: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/pa-ap/05paap-eng.php Accessed 5 June 2015.
Austin DM, Furr LA, Spine M . The effects of neighborhood conditions on perceptions of safety. J Crim Justice 2002; 30: 417–427.
Jackson J . Experience and expression social and cultural significance in the fear of crime. Br J Criminol 2004; 44: 946–966.
Kuo FE, Bacaicoa M, Sullivan WC . Transforming inner-city landscapes trees, sense of safety, and preference. Environ Behav 1998; 30: 28–59.
Boreham C, Riddoch C . The physical activity, fitness and health of children. J Sports Sci 2001; 19: 915–929.
Acknowledgements
We acknowledge the funding agencies of the QUALITY cohort: the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada and the Fonds de la recherche en santé du Québec. Dr Marie Lambert (July 1952–February 2012), pediatric geneticist and researcher, initiated the QUALITY cohort. Her leadership and devotion to QUALITY will always be remembered and appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Côté-Lussier, C., Mathieu, MÈ. & Barnett, T. Independent associations between child and parent perceived neighborhood safety, child screen time, physical activity and BMI: a structural equation modeling approach. Int J Obes 39, 1475–1481 (2015). https://doi.org/10.1038/ijo.2015.98
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.98
- Springer Nature Limited
This article is cited by
-
Association between built environments and weight status: evidence from longitudinal data of 9589 Australian children
International Journal of Obesity (2022)
-
Reciprocal relationships between employment status and psychological symptoms: findings from the Building a New Life in Australia study
Social Psychiatry and Psychiatric Epidemiology (2022)