Abstract
Background/Objectives:
Although loss of fat-free mass (FFM) and reduced muscle strength are highly prevalent in chronic obstructive pulmonary disease (COPD), only few data are available on the relationships of handgrip strength (HGS) and respiratory muscle strength with body composition in such disease. In particular, we aimed to assess whether raw bioelectrical impedance (BIA) variables were independent predictors of muscle strength in COPD patients, possibly more significant than anthropometric variables and BIA-based estimates of FFM.
Subjects/Methods:
Two hundred and thirty-seven COPD patients (161 males and 76 females) underwent respiratory, anthropometric, BIA, HGS and respiratory muscle strength (maximum inspiratory or expiratory pressure=MIP and MEP) measurements. Bioimpedance index (BI index=height square/whole-body impedance) and phase angle (PhA) were considered as raw BIA variables. FFM was estimated using three disease-specific BIA equations.
Results:
In COPD patients a stronger correlation was observed between HGS and PhA compared to the ones with anthropometric variables or FFM estimates. Multiple regression analysis showed that combining BI index and PhA (plus age in male patients) accounted for 50.2% and 42.6% of the variance in HGS in male and female patients, respectively. Similarly, BI index and PhA emerged as predictors of both MIP and MEP in males, while in females MIP was related only to PhA and MEP only to BI index.
Conclusions:
Raw BIA variables are independent and valuable predictors of HGS and respiratory muscle strength in COPD patients. BI index and PhA could provide useful information for evaluating body composition and better assessing muscle strength and physical fitness in COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic respiratory disease with several important extra-pulmonary consequences; in particular, loss of fat-free mass (FFM) and decreased muscle strength are highly prevalent in these patients.1, 2 Low FFM may have adverse effects on health status,3 increasing the frequency or severity of disease exacerbations, and being a strong predictor of mortality.4, 5 In the clinical setting, FFM is very frequently assessed by using bioelectrical impedance analysis (BIA). In such a case body composition is estimated by means of predictive equations which include BIA variables and frequently also variables such as age and weight.6 Alternatively, the use of directly-measured raw BIA variables, such as phase angle (PhA) or impedance ratio (IR=the ratio between impedance and Z at higher frequencies and Z at lower frequencies), has gained attention because they are thought to be a proxy of water distribution (extracellular/intracellular water ratio), body cell mass (BCM) and cellular integrity.6, 7, 8, 9, 10, 11, 12, 13, 14 Preliminary data in COPD showed that PhA significantly decreased across COPD stages.15 Furthermore, it was found to be positively correlated with body mass index (BMI) and negatively with age and disease severity.8
Decreased muscle strength is also common in COPD,1 possibly due to a number of specific reasons such as deconditioning, inflammation, malnutrition, oxidative stress, hypoxemia, in addition to the loss of muscle mass.2 Low limb muscle strength (usually evaluated by isometric knee extension strength) is reduced by 20–30% in COPD patients,2 and is considered to be a strong predictor of both exercise capacity and mortality.16 Similarly, handgrip strength (HGS) was found to be lower in COPD patients,17, 18, 19, 20, 21 being inversely associated with their quality of life and mortality.22, 23
Although the evaluation of both body composition and muscle strength is recommended for defining different nutritional phenotypes,5 only a few studies24, 25, 26, 27, 28, 29 have so far evaluated the relationships between upper limb muscle strength and body composition in COPD, showing lower HGS in patients with depleted FFM,25, 26 and an inverse association with BIA-based FFM.27, 28 With regard to raw BIA variables, a direct correlation between lower limb muscle strength and PhA was reported,8 with only preliminary results on HGS.11 On the other hand, to the best of our knowledge there is a scarcity of data on the relationship between respiratory muscle strength and body composition,30, 31, 32 and no mention of raw BIA variables.
Based on this background, the aim of this study was to assess the relationship between HGS and BIA in COPD patients. In particular, we hypothesized that raw BIA variables are stronger predictors of HGS than general characteristics of patients or BIA-based estimates of FFM. Similarly, we also evaluated whether BIA could be effective in predicting respiratory muscle strength.
Materials and methods
Patients with COPD, consecutively admitted to the Pulmonary Rehabilitation Section of Clinic Center S.p.A (Naples, Italy) from March 2013 to May 2016, were assessed for eligibility. Inclusion criteria were both genders and a diagnosis of COPD according to the latest Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.33 Exclusion criteria were related to diagnosis of known respiratory disorders other than COPD, known history of significant inflammatory disease other than COPD and a COPD exacerbation within 4 weeks of enrollment. The Ethics Committee of the ‘Federico II’ University of Naples approved the research protocol and all patients gave informed consent to participate to the study.
Lung function
All patients performed a baseline post-bronchodilator spirometry and body plethysmography (QBOX COSMED, Albano Laziale, Rome, Italy) according to American Thoracic Society (ATS)/European Respiratory Society (ERS) standardization.34 Forced expiratory volume in 1 s (FEV1) was assessed in accordance with the latest GOLD guidelines.35 Patients were classified into four stages according to GOLD criteria as follows: GOLD stage I (mild) if FEV1% predicted ⩾80; GOLD stage II (moderate) if 50⩾FEV1% predicted >80; GOLD stage III (severe) if 30⩾FEV1% predicted >50 and GOLD stage IV (very severe) if FEV1% predicted <30.
Body composition
Body weight and body height were measured to the nearest 0.1 kg and 0.5 cm respectively, using a mechanical column scale (SECA 711; Hamburg, Germany) and a stadiometer (SECA 220; Hamburg, Germany), and BMI was calculated as body weight/height.2 Body composition and single-frequency BIA (SF-BIA) were assessed at 50 kHz using a Human Im-Touch analyzer (DS Medica S.r.l., Milan, Italy), in standardized conditions (i.e. ambient temperature between 23 and 25 °C, fast >3 h, empty bladder, supine position for at least 10 min before starting the measurement), In addition, after cleaning skin surface, patients were asked to lay with legs and arms slightly abducted at 30°, so there was no contact between the extremities and trunk.
A standard tetrapolar technique was used, with measuring electrodes placed on the anterior surface of the wrist and ankle, and injecting electrodes placed on the dorsal surface of the hand and the foot, respectively. Z, resistance and PhA were measured for both dominant and non-dominant sides injecting an imperceptible electrical current of 800 mA. Bioelectrical impedance index (BI index) was calculated as height squared divided by Z, being a raw BIA variable directly related to FFM.36 As BIA-based estimates of body composition, FFM and FFM index (FFMI kg/m2=FFM/height2) were estimated from resistance using three disease-specific BIA equations.37, 38, 39 Fat mass (FM) was calculated as body weight minus FFM.
Muscle strength
HGS, a proxy of overall muscle strength,40 was measured at baseline with a digital dynamometer (Dynex, MD systems, Inc., Westerville, OH, USA). Three measurements were taken for each body sides (dominant and non-dominant) and the maximum values were considered for statistical analysis.41 Mean value of the two body sides was indicated as whole-body HGS (or HGS). Low HGS was defined according to the European Working Group on Sarcopenia in Older People (EWGSOP) as follows: <30 kg in males and <20 kg in females.
Respiratory muscle strength was measured as maximum inspiratory pressures (MIP) and maximum expiratory pressures (MEP), according to the method described by Black and Hyatt.42 Measurements were obtained in the sitting position with MicroRPM (CareFusion, Hoechberg, Germany).
Other measurements
Breathlessness was measured using the Medical Research Council (MRC) dyspnea scale.43 A composite prognostic index based on BMI, airflow obstruction, dyspnea, and exercise capacity (BODE index),44 was used as proxy of global disease severity.
Statistical analysis
Whole-body data for Z, BI index, PhA and HGS were obtained by calculating the mean of dominant and non-dominant sides. Values were reported as mean±s.d. unless otherwise specified. Comparisons between groups were conducted by analysis of variance (ANOVA). Pearson correlation coefficient was used to evaluate the association between variables. Multiple regression analysis was applied in order to identify the best predictors of HGS, MIP and MEP. Three sets of variables were considered: general characteristics of patients (age, height, weight and BMI, plus FEV1 measured); BIA-based estimates of body composition (FFM and FM) plus age; raw BIA variables (BI index and PhA) plus age.
Results
Two hundred and thirty-seven patients (161 males and 76 females) with stable COPD were studied. General characteristics of patients were shown in Table 1. Male patients had higher HGS (+51.1%), MIP (+18.5%) and MEP (+11.0%) than female patients. When using the EWGSOP criteria,45 low HGS was found in 63.4% and 71.1% of male and female COPD patients, respectively. The majority of patients had moderate to severe impaired lung function: 3.4% of patients were classified in GOLD stage I, 30.4% in GOLD stage II, 39.7% in GOLD stage III and 26.6% in GOLD stage IV. With respect to BODE index, 26.6% patients had a score between 1 and 5 points and 73.4% between 6 and 10 points.
Concerning body composition, whichever of the three predictive equations was used, FFM and FFMI were significantly higher and percentage of FM lower in males compared to females (Table 1). In both genders, mean FFM (and, consequently, FFMI) was the highest when the Rutten equation was used and the lowest when the Kyle equation was used.
SF-BIA data
BI index was significantly lower by about 23.3% in females (Table 1), while PhA was higher in males (by 6.0%). In a multivariate analysis, age (P<0.001), BMI (P<0.05) and FEV1 measured (P<0.001) emerged all as predictors of PhA in males (adjusted R2=0.220, P<0.001), whereas height and weight did not. On the contrary, in females, the only significant predictor was FEV1 measured (adjusted R2=0.049, P<0.05).
An inverse correlation between PhA and BODE index was observed both in males (r=−0.343, P<0.001) and females (r=−0.358, P<0.01), whereas a marked decline across GOLD stages was observed only in males (5.37±0.89, 5.00±0.92 and 4.82±0.99 degrees in stages I/II, III and IV, respectively).
Relationship between muscle strength and body composition
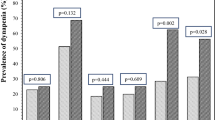
First, we evaluated the association of PhA with a number of variables of interest (Table 2). There was a more evident correlation of HGS with age, anthropometric variables, and BIA estimates of FFM in males than females. The association with HGS was weaker for FFMI, independently of the equation used (data not shown). In both genders, raw BIA variables, and especially PhA (Figure 1), were more strictly correlated with HGS than the other variables (with the exception of height in females). With respect to respiratory muscle strength, as shown in Table 2, there was in both genders a significant association of MIP or MEP with BIA estimates of FFM, and also with PhA (for MEP only in males).
Multiple regression analysis was applied on different sets of independent variables in order to identify the best predictors of HGS. First, demographic and anthropometric variables (plus FEV1) were considered. In males, age, height, weight, BMI and FEV1 entered the model (P<0.01 or less) with an adjusted R2 of 0.333, whereas in females the only predictor was height (age, weight, BMI and FEV1 were excluded), with an adjusted R2 of 0.280.
As a second step, with respect to BIA-based estimates of body composition, FFM, FM and age all emerged as significant predictors of HGS, except for the Steiner equation in females (data not shown). FFM was also a predictor of MIP in both genders and MEP in males, whichever predictive equation was chosen, whereas this correlation was significant in females only for Rutten equation (data not shown).
Finally, when raw BIA variables were included in the model (Table 3), combining BI index and PhA (plus age in male patients) accounted for 50.2 and 42.6% of the variance in HGS in male and female patients, respectively. In both genders HGS was almost 3 kg higher for every one degree increase in PhA. Similarly, as shown in Table 3, BI index and PhA emerged as predictors of both MIP and MEP in males, while in females MIP was related only to PhA and MEP only to BI index.
Discussion
The main finding of the present study is that in COPD patients raw BIA variables are significant predictors of muscle strength. HGS, MIP and MEP are more strictly related to BI index and PhA compared to general characteristics of patients and BIA-based FFM.
Different metabolic phenotypes characterized by low FFM and decreased muscle strength (for example, sarcopenia and sarcopenic obesity) may be observed in COPD patients,5 being associated with decreased physical activity, exercise intolerance, poor quality of life, and higher morbidity and mortality.2, 23 In the clinical setting, FFM is often estimated through predictive equations based on BIA variables. Raw BIA variables (BI index and PhA) have also been receiving attention,6, 10, 46, 47 because they are considered as a proxy of FFM, water distribution, BCM and cellular integrity.14, 18, 48 The few data available in the literature have shown that in COPD patients PhA was higher in males,8, 15, 49 being correlated negatively with age and positively with BMI and FEV1,8 and significantly decreased across COPD stages.15 We extend these observations by showing, in a multivariate analysis, that age and BMI are predictors of PhA in males, but not in females. In addition, it should be noted that underweight male patients (BMI<21 kg/m2) have lower values of PhA compared to those with a higher BMI (4.49±0.98 degrees vs 5.10±0.90 degrees; P<0.001). Indeed, no difference was found in underweight female patients compared to those with a normal weight.
Low muscle strength, which is another feature of muscle dysfunction and a major systemic consequence of COPD,2 is commonly diagnosed in the clinical setting by measuring HGS.5 In COPD patients HGS has been found to be reduced,17, 18, 19, 20, 21 being inversely associated with their quality of life and mortality.22, 23 A few studies have also provided limited data on the relationship between muscle strength and body composition in COPD (none as primary endpoint), showing that patients with depleted FFM had lower HGS.25, 26, 27, 28 In addition, regarding raw BIA variables, an association between quadriceps strength and PhA was found in a recent single study.8 Taking into consideration the scarcity of data in the literature, this is the first study to deal with evaluating in COPD the relationship of HGS and respiratory muscle strength with raw BIA variables, as compared with a number of other selected variables, such as general characteristics and BIA-based estimates of body composition. Simple correlation shows that HGS is more strongly related to raw BIA data (in particular, to PhA) than other selected variables. More interestingly, in a multivariate analysis raw BIA variables emerged as significant predictors of HGS, while FEV1 did not. HGS directly increases by 2.83 kg for each degree of PhA at 50 kHz, in males and 3.09 kg in females. These results are consistent with previous studies on old patients with cancer50 or elderly people at risk of sarcopenia.48
Respiratory muscle strength is another functional measure with prognostic potential in COPD patients.51 Many COPD patients show a reduction in the strength of respiratory muscles,52, 53 with a prevalence of 20–45% in patients with a stable disease,53 and 80–90% in patients with frequent exacerbations.54 While previous studies have found in COPD that respiratory muscle strength was positively correlated to FFMI55 and lower in underweight patients,56 to the best of our knowledge no data are available on the relationships of MIP and MEP with raw BIA variables. In good agreement with a previous study showing an association between MIP and PhA in cancer patients,57 we found positive correlations of respiratory muscle strength with BI index and PhA, which were stronger than the ones observed with other potential predictors (anthropometrics and BIA-based estimates of FFM). A possible explanation could be the reduced mass of the diaphragm muscle and chest wall or reduced mechanical efficiency of the respiratory muscles in COPD patients with poorer body composition.58
Overall, the relationship of HGS, MIP and MEP with raw BIA variables in COPD patients can be explained first of all considering that BI index is usually considered as a proxy of FFM. In addition, our results suggest that PhA may provide some useful information on intrinsic characteristics of FFM related to muscle strength, possibly because it reflects BCM or some cellular abnormalities due to malnutrition.
Some limitations of the study must be acknowledged. First, this is a single-center study, which, however, included COPD patients referred for a pulmonary rehabilitation program from several hospitals and chest physicians of Campania region in Southern Italy (5 850 850 residents). Second, since these data were not available, we are not able to compare BIA variables with body composition estimates obtained with dual energy X-ray absorptiometry or other reference techniques. However, this is the first study that describes in COPD the relationships of muscle strength with raw BIA variables and other variables commonly used in the clinical setting.
In conclusion, based on these results, it can be concluded that raw BIA variables (BI index and PhA) are independent predictors of muscle strength in COPD patients, more strongly associated to HGS and respiratory muscle strength than BIA-based estimates of FFM or anthropometric parameters. The assessment of BI index and PhA could provide useful information for evaluating body composition and better assessing muscle strength and physical fitness in COPD. Longitudinal studies are needed to test whether raw BIA variables may help predicting risk of functional decline in these patients.
References
Nyberg A, Saey D, Maltais F . Why and how limb muscle mass and function should be measured in patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc 2015; 12: 1269–1277.
Maltais F, Decramer M, Casaburi R, Barreiro E, Burelle Y, Debigarè R et al. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014; 189: e15–e62.
Shoup R, Dalsky G, Warner S, Davies M, Connors M, Khan M et al. Body composition and health-related quality of life in patients with obstructive airways disease. Eur Respir J 1997; 10: 1576–1580.
Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF . Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr 2005; 82: 53–59.
Schols AM, Ferreira IM, Franssen FM, Gosker HR, Janssens W, Muscaritoli M et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J 2014; 44: 1504–1520.
Earthman CP . Body composition tools for assessment of adult malnutrition at the bedside: a tutorial on research considerations and clinical applications. J Parenter Enteral Nutr 2015; 39: 787–822.
Earthman C, Traughber D, Dobratz J, Howell W . Bioimpedance spectroscopy for clinical assessment of fluid distribution and body cell mass. Nutr Clin Pract 2007; 22: 389–405.
Maddocks M, Kon SS, Jones SE, Canavan JL, Nolan CM, Higginson IJ et al. Bioelectrical impedance phase angle relates to function, disease severity and prognosis in stable chronic obstructive pulmonary disease. Clin Nutr 2015; 34: 1245–1250.
Norman K, Stobaus N, Zocher D, Bosy-Westphal A, Szramek A, Scheufele R et al. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am J Clin Nutr 2010; 92: 612–619.
Mulasi U, Kuchnia AJ, Cole AJ, Earthman CP . Bioimpedance at the bedside: current applications, limitations, and opportunities. Nutr Clin Pract 2015; 30: 180–193.
de Blasio F, Santaniello MG, De Blasio F, Miracco Berlingieri G, Bellofiore B, Scalfi L . BIoelectrical impedance analysis (bia) in the assessment of muscular function in patients suffering from copd. Chest 2014; 145: 468A–468A.
de Blasio F, de Blasio F, Miracco Berlingieri G, Bianco A, La Greca M, Franssen FM et al. Evaluation of body composition in COPD patients using multifrequency bioelectrical impedance analysis. Int J Chron Obstruct Pulmon Dis 2016; 11: 2419–2426.
Baumgartner RN, Chumlea WC, Roche AF . Bioelectric impedance phase angle and body composition. Am J Clin Nutr 1988; 48: 16–23.
Gonzalez MC, Barbosa-Silva TG, Bielemann RM, Gallagher D, Heymsfield SB . Phase angle and its determinants in healthy subjects: influence of body composition. Am J Clin Nutr 2016; 103: 712–716.
Abbatecola AM, Fumagalli A, Spazzafumo L, Betti V, Misuraca C, Corsonello A et al. Body composition markers in older persons with COPD. Age Ageing 2014; 43: 548–553.
Swallow EB, Reyes D, Hopkinson NS, Man WD, Porcher R, Cetti EJ et al. Quadriceps strength predicts mortality in patients with moderate to severe chronic obstructive pulmonary disease. Thorax 2007; 62: 115–120.
Cortopassi F, Celli B, Divo M, Pinto-Plata V . Longitudinal changes in handgrip strength, hyperinflation, and 6-minute walk distance in patients with COPD and a control group. Chest 2015; 148: 986–994.
Gosselink R, Troosters T, Decramer M . Peripheral muscle weakness contributes to exercise limitation in COPD. Am J Respir Crit Care Med 1996; 153: 976–980.
Shah S, Nahar P, Vaidya S, Salvi S . Upper limb muscle strength & endurance in chronic obstructive pulmonary disease. Indian J Med Res 2013; 138: 492–496.
Heijdra YF, Pinto-Plata V, Frants R, Rassulo J, Kenney L, Celli BR . Muscle strength and exercise kinetics in COPD patients with a normal fat-free mass index are comparable to control subjects. Chest 2003; 124: 75–82.
Pleguezuelos E, Esquinas C, Moreno E, Guirao L, Ortiz J, Garcia-Alsina J et al. Muscular Dysfunction in COPD: Systemic Effect or Deconditioning? Lung 2016; 194: 249–257.
Puhan MA, Siebeling L, Zoller M, Muggensturm P, ter Riet G . Simple functional performance tests and mortality in COPD. Eur Respir J 2013; 42: 956–963.
Burtin C, Ter Riet G, Puhan MA, Waschki B, Garcia-Aymerich J, Pinto-Plata V et al. Handgrip weakness and mortality risk in COPD: a multicentre analysis. Thorax 2016; 71: 86–87.
Engelen MP, Schols AM, Baken WC, Wesseling GJ, Wouters EF . Nutritional depletion in relation to respiratory and peripheral skeletal muscle function in out-patients with COPD. Eur Respir J 1994; 7: 1793–1797.
Mostert R, Goris A, Weling-Scheepers C, Wouters EF, Schols AM . Tissue depletion and health related quality of life in patients with chronic obstructive pulmonary disease. Respir Med 2000; 94: 859–867.
Yilmaz D, Capan N, Canbakan S, Besler HT . Dietary intake of patients with moderate to severe COPD in relation to fat-free mass index: a cross-sectional study. Nutr J 2015; 14: 35.
Vermeeren MA, Creutzberg EC, Schols AM, Postma DS, Pieters WR, Roldaan AC et al. Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med 2006; 100: 1349–1355.
Kurosaki H, Ishii T, Motohashi N, Motegi T, Yamada K, Kudoh S et al. Extent of emphysema on HRCT affects loss of fat-free mass and fat mass in COPD. Intern Med 2009; 48: 41–48.
Hillman CM, Heinecke EL, Hii JW, Cecins NM, Jenkins SC, Eastwood PR . Relationship between body composition, peripheral muscle strength and functional exercise capacity in patients with severe chronic obstructive pulmonary disease. Intern Med J 2012; 42: 578–581.
Kyle UG, Janssens JP, Rochat T, Raguso CA, Pichard C . Body composition in patients with chronic hypercapnic respiratory failure. Respir Med 2006; 100: 244–252.
Gologanu D, Ionita D, Gartonea T, Stanescu C, Bogdan MA . Body composition in patients with chronic obstructive pulmonary disease. Maedica 2014; 9: 25–32.
Nishimura Y, Tsutsumi M, Nakata H, Tsunenari T, Maeda H, Yokoyama M . Relationship between respiratory muscle strength and lean body mass in men with COPD. Chest 1995; 107: 1232–1236.
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. Available from http://goldcopd.org.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338.
Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013; 187: 347–365.
Heitmann BL . Impedance: a valid method in assessment of body composition? Eur J Clin Nutr 1994; 48: 228–240.
Rutten EP, Spruit MA, Wouters EF . Critical view on diagnosing muscle wasting by single-frequency bio-electrical impedance in COPD. Respir Med 2010; 104: 91–98.
Steiner MC, Barton RL, Singh SJ, Morgan MD . Bedside methods versus dual energy X-ray absorptiometry for body composition measurement in COPD. Eur Respir J 2002; 19: 626–631.
Kyle UG, Pichard C, Rochat T, Slosman DO, Fitting JW, Thiebaud D . New bioelectrical impedance formula for patients with respiratory insufficiency: comparison to dual-energy X-ray absorptiometry. Eur Respir J 1998; 12: 960–966.
Ling CH, Taekema D, de Craen AJ, Gussekloo J, Westendorp RG, Maier AB . Handgrip strength and mortality in the oldest old population: the Leiden 85-plus study. CMAJ 2010; 182: 429–435.
Vaz M, Thangam S, Prabhu A, Shetty PS . Maximal voluntary contraction as a functional indicator of adult chronic undernutrition. Br J Nutr 1996; 76: 9–15.
Black LF, Hyatt RE . Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969; 99: 696–702.
Fletcher CM, Elmes PC, Fairbairn AS, Wood CH . The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J 1959; 2: 257–266.
Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350: 1005–1012.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010; 39: 412–423.
Norman K, Stobaus N, Pirlich M, Bosy-Westphal A . Bioelectrical phase angle and impedance vector analysis—clinical relevance and applicability of impedance parameters. Clin Nutr 2012; 31: 854–861.
Elia M . Body composition by whole-body bioelectrical impedance and prediction of clinically relevant outcomes: overvalued or underused? Eur J Clin Nutr 2013; 67: S60–S70.
Basile C, Della-Morte D, Cacciatore F, Gargiulo G, Galizia G, Roselli M et al. Phase angle as bioelectrical marker to identify elderly patients at risk of sarcopenia. Exp Gerontol 2014; 58: 43–46.
de Blasio F, Santaniello MG, de Blasio F, Berlingieri GM, Bellofiore B, Scalfi L . Bioelectrical impedance analysis (BIA) in the assessment of muscular function in patients suffering from COPD. Chest 2014; 145: 468A.
Norman K, Wirth R, Neubauer M, Eckardt R, Stobaus N . The bioimpedance phase angle predicts low muscle strength, impaired quality of life, and increased mortality in old patients with cancer. J Am Med Dir Assoc 2015; 16: 117–122.
Hodgev VA, Kostianev SS . Maximal inspiratory pressure predicts mortality in patients with chronic obstructive pulmonary disease in a five-year follow-up. Folia Med 2006; 48: 36–41.
Gea J, Agusti A, Roca J . Pathophysiology of muscle dysfunction in COPD. J Appl Physiol (1985) 2013; 114: 1222–1234.
Polkey MI, Kyroussis D, Hamnegard CH, Mills GH, Green M, Moxham J . Diaphragm strength in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1996; 154: 1310–1317.
Vilaró J, Ramirez-Sarmiento A, Martínez-Llorens JM, Mendoza T, Alvarez M, Sánchez-Cayado N et al. Global muscle dysfunction as a risk factor of readmission to hospital due to COPD exacerbations. Respir Med 2010; 104: 1896–1902.
Luo Y, Zhou L, Li Y, Guo S, Li X, Zheng J et al. Fat-free mass index for evaluating the nutritional status and disease severity in COPD. Respir Care 2016; 61: 680–688.
Sabino PG, Silva BM, Brunetto AF . Nutritional status is related to fat-free mass, exercise capacity and inspiratory strength in severe chronic obstructive pulmonary disease patients. Clinics 2010; 65: 599–605.
Hui D, Bansal S, Morgado M, Dev R, Chisholm G, Bruera E . Phase angle for prognostication of survival in patients with advanced cancer: preliminary findings. Cancer 2014; 120: 2207–2214.
Ferreira IM, Brooks D, White J, Goldstein R . Nutritional supplementation for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 12: Cd000998.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
LS designed the research. FdB, MGS and FrdB conducted the research. FdB and LS analyzed the data and performed statistical analysis, which was reviewed by FMEF, LL, AB and GM. FdB and LS produced a first draft of the manuscript and had primary responsibility for final content. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
de Blasio, F., Santaniello, M., de Blasio, F. et al. Raw BIA variables are predictors of muscle strength in patients with chronic obstructive pulmonary disease. Eur J Clin Nutr 71, 1336–1340 (2017). https://doi.org/10.1038/ejcn.2017.147
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2017.147
- Springer Nature Limited
This article is cited by
-
Association of phase angle with sarcopenia and muscle function in patients with COPD: a case-control study
BMC Pulmonary Medicine (2024)
-
Association of phase angle with sarcopenia in chronic musculoskeletal pain patients: a retrospective study
Journal of Orthopaedic Surgery and Research (2023)
-
Phase angle in assessment and monitoring treatment of individuals with respiratory disease
Reviews in Endocrine and Metabolic Disorders (2023)
-
Phase angle (PhA) in overweight and obesity: evidence of applicability from diagnosis to weight changes in obesity treatment
Reviews in Endocrine and Metabolic Disorders (2023)
-
Dynapenia is highly prevalent in older patients with advanced idiopathic pulmonary fibrosis
Scientific Reports (2021)