Abstract
Background/Objectives:
There is limited evidence that prominent calorie labelling on out-of-home meals helps consumers reduce calorie intakes and avoid weight gain, but no evidence on its effects on macro- and micro-nutrients. The objective of this study was to assess the impact of prominent calorie labelling on energy, macro- and micro-nutrients.
Subjects/Methods:
Young adults in a catered residential setting were observed when choosing main meals over three study periods in fixed order in this observational study. Period 1: with calorie labels (20 weeks); period 2: without calorie labels (10 weeks); period 3: with calorie labels plus information on estimated energy requirements (10 weeks). Nutrient contents of meal choices were analysed from food composition tables.
Results:
Energy, 4 macronutrients and 19 micronutrients levels were derived from 4200 meals chosen by 120 subjects over 40 weeks. Means (s.d. or Median) for key macro- and micro-nutrients were for period 1: energy=658 (94) kcal, fat=31 (8.6) g, saturated fat=10.5 (2.7) g, B12=2.5 (1.7) μg, folate=119 (46.8) μg, vitamin C=80.0 (42) mg, Ca=278 (129) mg, Na=1230 (119) mg, Fe=22 (10) g, Se=19 (10.1) μg, I=34 (10.1) μg, period 2: energy=723 (87) kcal, fat=35 (7.6) g, saturated fat=12 (2.7) g, B12=3.4 (1.7) μg, Folate=182 (13.3) μg, vitamin C=87.0 (49.7) mg, Ca=379 (149) mg, Na=1352 (114) mg, Fe=41.6 (14) g, Se=26 (10.3) μg, I=38.0 (18.4) μg, period 3: energy=578 (109) kcal, fat=27.3 (9.1) g, saturated fat=8.5 (2.7) g, B12=2.2 (0.5) μg, Folate=90 (50.8) μg, vitamin C=75.0 (34) mg, Ca=277 (119) mg, Na=1205 (99) mg, Fe=14.5 (10.9) g, Se=15.0 (10) μg, I=32.0 (18.4) μg. All macro- and micro-nutrients, except for B1, vitamin C, vitamin E and Ca were significantly different between the three periods (P<0.001), but all mean intakes remained above recommended levels.
Conclusions:
Calorie labelling resulted in reductions in calories, fat and saturated fat contents of the meals chosen, without compromising micronutrient consumptions.
Similar content being viewed by others
Introduction
Obesity prevalence has been increasing worldwide,1 along with increases in food available out-of-home2 and increasing portion sizes.3 In US 33% more food is consumed out-of-home than in 1970,4 and this pattern is following internationally.5 Food out-of-home is usually of poorer nutrition quality and higher in calories in both independent6 and chain restaurants,7 and customers find it hard to estimate the calorie content of the food on offer.8 Calorie labelling has therefore been suggested as a tool to help raise awareness of the calorie content of food and to help customers to choose less calories.
Calorie labelling was firstly proposed in 2006 by New York City’s Health Department for chain restaurants with more than 15 outlets.9 The restaurant association opposed move and filled lawsuits twice in attempts to prevent its implementation. Alisson, on behalf of the restaurant association, argued that calorie labelling could actually have the opposite effects of those intended, with customers ordering more calories.10 The legislation was passed and implemented in 2008 and in 2011 calorie labelling became part of the Affordable Care Act.11 In the same year, New South Wales in Australia passed similar legislation, requiring the provision of calorie information and of average adult daily energy intake in large multiple food outlets.12 Other states in both US and Australia are considering similar legislation. In UK, the Department of Health ‘Responsibility Deal’ encourages food outlet companies to sign up to a voluntary scheme to provide calorie information.13
Current evidence suggests that calorie labelling overall is ineffective in reducing the calories bought/chosen by customers, but for those who actually see the labels it can lead to a significant reduction of 124 kcal/meal or snack.14 There are long-standing concerns over ‘calorie-counting’, and that if calorie labelling leads to a reduction in calories purchased, it may lead to unfavourable intakes of other macro- and micro-nutrients. Providing only calorie information may mask a poor nutritional profile of a food item and mislead the consumers in terms of its healthfulness.
Of all the studies conducted since introduction of calorie labelling legislation in the US, only one, Elbel et al.,15 has examined nutrients other than energy. They reported no significant differences in calories, fat, sodium and sugar chosen by customers in New York City food outlets before and after the introduction of calorie labelling.15
The present study assessed the effect on macro- and micro-nutrients, chosen in main-meal selections by young adults, of prominent calorie labelling in a catered residential setting that led to reduced calorie intakes and avoidance of weight gain over 40 weeks.
Materials and methods
This study was reviewed and approved by the ethics committee of the Medical Veterinary and Life Sciences College of the University of Glasgow, and conducted in 2013–2014.
Setting
The study was conducted in a residential university student hall of residence accommodating 120 students. All residents are provided with breakfast and dinner every day for the 40-week academic year, from a rotating 5-week menu cycle, included within a fixed accommodation charge. The present study involved only the evening main meals.
Menu
Three-course evening meals provided a choice of three different main-course dishes, varied daily, from which students were allowed to choose one. They could also choose one starter, one dessert and a piece of fruit, or two pieces of fruit, or a piece of fruit and a small pot of yogurt. The recipes and options within the 5-week menu cycle remained unchanged during the entire study.
The menu had been developed over time by the catering staff, without any expert nutritional guidance, reducing food costs and wastage being the main catering criteria. All meals were prepared and cooked on-site by the hall’s catering staff. Recipes, including ingredient lists, for all dishes served in the hall, were available for analysis for the researchers, but not provided to students. Portions of the meat and fish meal components were fixed (110 g/portion) and serving of the other meal components was carried out using standard utensils. Nutrient contents of meals chosen from the usual menu were analysed using nutrient analysis software (WinDiets, Aberdeen, UK, 2010) as recommended by the Department of Health for England Guidelines for voluntary calorie labelling in catering outlets.16
Study periods
There were three separate study periods during the 40-week study duration, which covered the entire residential academic year.
Period 1: For 20 weeks (September 2012–January 2013), calorie contents per portion for each component of the evening meal were shown each day, in bold text on 5.4 × 9.9 cm laminated cards, which also included the university coat of arms, both on the main hall notice board and at the of meal self-serving point.
Period 2: For 10 weeks (February–March 2013), calorie labels were removed from display.
Period 3: For a 10-week period (April–June 2013), in addition to calorie contents, estimated daily energy requirements were presented in front of the foods, for males and females aged 18–34 years old, based on the Schofield equations, assuming a physical activity level of 1.4 and for a range of weights (50–100 kg). The common single current energy requirement recommendation of 2000 kcal/day for women and 2500 kcal/day for men is an overestimation for many young adults. Therefore, we provided energy requirements for males and females, for the specific age group, and for a variety of body weights, in an attempt to help young adults realise approximately how much energy they need and how energy requirements vary with body weight. The estimated daily energy requirements of young adults were provided as A4 size posters in the dining room, one for males and one for females.
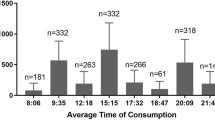
Data collection
During the year 2012–2013, the selections of meal components made by the first 100 students served on selected days, were observed and recorded manually. The principal researcher (CKN) attended the evening meal serving on 14 days on each 5-week menu cycle (one cycle with calorie information, one cycle with no calorie information and one cycle with calorie information and daily energy requirements; 42 days in total). The researcher stood just behind the food on offer in order to have immediate contact with both the participants and catering staff. The cutoff of 100 students was set in case the range of choices could be reduced for subsequent students, once the most popular choices had been served. In the event, however, there was no occasion when meal options ran out before the first 100 students had been served on the days when meal serving was observed and choices recorded. Food wastage was not possible to be measured.
Analyses of choices
An access database was constructed with all the available meal options for the 5-week menu cycle and their nutritional analysis. Meals observed during the three study periods were entered in the database and 4200 meal combinations were logged in, in total. After checking for normalcy, mean values and s.d. or median and interquartile ranges were reported.
Statistical analysis
One-way analysis of cariance was performed to determine whether there were any differences between the mean total number of calories, grams of fat and grams of saturated fat and all other micronutrients, in the three time periods for male and female participants. Regression analyses then explored the relationships between the nutrient density and energy density. Regression analyses were performed for all the meal components in order to examine relationships between calorie content and macronutrients and micronutrient contents.
Results
The ranges of calories, fat and saturated fat contents of each course of the menu on offer, from which students could choose their meals, were: starters: 18–399 kcal, fat 0.5–27.3 g, saturated fat 0.2–24.5 g; main courses: 105–885 kcal, fat 7.5–56.7 g, saturated fat 2.5–25.8 g; desserts: 114–694 kcal, fat 8–55.5 g, saturated fat 2.0–34.5 g.
Subjects
Most of the 120 resident young adults ate their evening meal in the hall restaurant on most days, because they had pre-paid for meals. Their characteristics at baseline were gathered by an online questionnaire, not linked with the current study. Residents’ characteristics at baseline were: mean age=19.1 (s.d. 0.9) years, weight=66.1 (s.d. 11.6) kg, body mass index=22.3 (SD3.3) kg/m2.
Meal choices made during the three study periods
Data were collected on the first 100 subjects to choose their main meals on 42 days, providing a total of 4200 meal choices for analysis, of which 1454 meals had been chosen by males and 2746 by females.
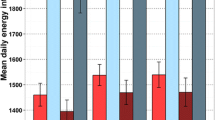
Mean (s.d.) or, where non-normally distributed, median (interquartile) values for energy and all macro- and micro-nutrients chosen during the three study periods are presented in Table 1 and Figures 1, 2, 3.
Energy
The mean number of calories chosen by young adults over 14 days was; period 1: 658 (s.d. 95) kcal, period 2: 722 (s.d. 87) kcal, period 3: 578 (s.d. 107) kcal. Energy expressed in calories was significantly different between the three study periods tested with analysis of variance, P<0.001. That was the case when analysed separately for both males and females.
Period 1 versus period 2 (calorie labelling versus no calorie labelling). Paired t-test showed significant increase of the energy content of meals from period 1 to period 2 (P=0.001). The increase was also significant for both males and females (P=0.03 and P=0.05, respectively).
Period 2 versus period 3 (no calorie labelling versus calorie labelling and energy requirements). Paired t-test showed significant decrease of the energy content of meals from period 2 to period 3 (P=0.002). The decrease was also significant for both males and females
Macronutrients
The mean grams of fat, saturated fat, protein and carbohydrate chosen by young adults over 14 days was; period 1: fat=31 (s.d. 8.6) g, saturated fat=11.4 (s.d. 2.7) g, protein=24.4 (s.d. 10.3) g, carbohydrate=45.6 (s.d. 14.3) g; period 2: fat=34.7 (s.d. 7.8) g, saturated fat=11.9 (s.d. 2.7) g, protein=25.7 (s.d. 10.4) g, carbohydrate=46.4 (s.d. 14.9) g; period 3: fat=26.9 (s.d. 9.1) g, saturated fat=8.4 (s.d. 2.6) g, protein=22.7 (s.d. 10.1) g, carbohydrate=40.2 (s.d. 11.9) g.
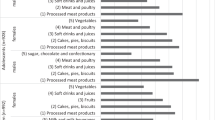
Micronutrients
The mean μg/mg of main micronutrients chosen by young adults over 14 days was; period 1: B12=2.5 (1.7) μg, folate=119 (46.8) μg, vitamin C=80.0 (42) mg, Ca=278 (129) mg, Na=1230 (119) mg, Fe=22 (10) g, Se=19 (10.1) μg, I=34 (10.1) μg; period 2: B12=3.4 (1.7) μg, Folate=182 (13.3) μg, vitamin C=87.0 (49.7) mg, Ca=379 (149) mg, Na=1352 (114) mg, Fe=41.6 (14) g, Se=26 (10.3) μg, I=38.0 (18.4) μg; period 3: B12=2.2 (0.5) μg, Folate=90 (50.8) μg, vitamin C=75.0 (34) mg, Ca=277 (119) mg, Na=1205 (99) mg, Fe=14.5 (10.9) g, Se=15.0 (10) μg, I=32.0 (18.4) μg. All macronutrients (Table 1) but thiamine, vitamin E, vitamin C and calcium were significantly different between the three study periods tested with analysis of variance, P<0.001
Relationship of calorie content with the content of other nutrients
Multiple regression analysis showed strong linear relationships between calorie and fat content (r2=0.901, P<0.01) and between calorie and saturated fat content (r2=0.709, P<0.01). For protein and carbohydrate, the relationship with calorie content was weaker but still significant (protein and kcal: r2=0.505, P=0.05, carbohydrate and kcal: r2=0.408, P=0.05, Figure 4).
Key micronutrients in meals did not correlate with calorie content. The correlation coefficient for calories and Fe was r2=0.141 and for calories and Iodine r2=0.354, neither statistically significant. Calorie content was, however, correlated with Ca (r2= 0.535, P=0.01) with Na (r2=0.526, P=0.01), and folate (r2=0.419, P=0.05, Figure 5).
Discussion
This is the first study to examine the effects of calorie labelling on micro- and micro-nutrients over a prolonged period of time, and in free living subjects without any interference from researchers. Our results indicate that prominent calorie labelling was successful in reducing the amount of all macro- and micro-nutrients except for thiamine, vitamin E, vitamin C and Calcium chosen by young adults. The calorie content of the meals chosen by young adults was also reduced and we have already reported an abolition of the usual weight gain experienced by young adults over the 40-week academic year.17 The mean reduction of 144 kcal/meal associated with calorie labelling, between periods 2 and 3 resulted in young adults achieving the target of 600 kcal/meal based on 2000 kcal diet during period three18 (a meal should consist of 30% of daily energy requirements based suggested from Food Standards Agency). Although calorie labelling led to desired reduction in calories and macronutrients, and prevented weight gain, the reduction in micronutrients did not result in inadequate intakes for any micronutrients, as all those were well above the recommended levels.
The notion that modern diet is energy dense, but nutrient poor, is generally accepted. Nutritional quality of meals is best expressed as nutrient content per unit energy, for example, mg per 1000 kcal. The nutrients that form the basis for human health are protein, energy, vitamin A and carotene, vitamin D, vitamin E, thiamine, riboflavin, niacin, vitamin B6, vitamin B12, folate, vitamin C, antioxidants, calcium, iron, zinc, selenium, magnesium and iodine.19 Some nutrients are provided in great amounts by a limited number of common foods rich in the specific nutrient, such as vitamin C in fruit, calcium and iodine in dairy products, whereas other nutrients are provided more uniformly in many foods, such as Mg and most trace elements. Calorie labelling led to a reduction in macronutrients (fat, saturated fat, carbohydrate and protein) and there were small, proportionate reductions in most of the micronutrients (except for thiamine, Ca, vitamin E and vitamin C).
There has been widespread concern among dietitians and public health experts that ‘calorie-labelling’ of individual foods cannot capture alone the complexity of nutrition, may ignore other nutrients, and aggravate the already nutritionally poor diets of overweight and obese people.20 The present study is, therefore, valuable in showing that calorie content correlates strongly with the fat, saturated fat and sodium content, hence, when a customer is choosing a food item lower in calories then this item is likely to contain less fat and saturated fat, too. Public Health programmes have tended to try to tackle several elements of diet quality simultaneously, which has to some extend caused confusion, and led to over-complex messages with relatively little population benefit. It is confusing and generally unhelpful to ordinary consumers to try to present detailed micronutrient compositions of individual foods, because their nutrient consumptions depend on the quantitative proportions of different foods within the overall diet. Current nutrition information in the form of boxes with nutritional information on the products have had little impact and tend to favour more educated customers.21 Although it is true that improving fat, saturated fat, carbohydrate, protein, sodium and sugar would benefit chronic disease risks, all these nutrients are outweighed by the ill-effects of the increasing obesity levels around the world. Hence, there is an argument for trying to get the calories right before getting involved in more complicated messages.
The format of the calorie labelling used in this study was different to the one used by chain restaurants in US, UK and Australia. The only country that provides some rules regarding the format of the labels is the US. The rule only requires calorie labels to be the in same font size as the font used for the price or the font used for the food item, whichever is the smallest. It seems that the key to the success of calorie labelling is visibility14, 22, 23, 24 but ironically the US rule requires calorie labels to match the font size of the smallest element, which is usually the price for obvious reasons. We used labels that could not be missed because of their size and placement, that is, directly in front of each food item.
There are of course limitations incurred by study design, which should prompt caution in extrapolating our results. Using subjects in a catered residential setting was immensely valuable, allowing a rare opportunity for detailed data collection, but we had access only to one site, so a randomised design was not possible. Furthermore, similar studies in other settings would be reassuring, but they are hard to design and agreements with caterers are difficult to obtain. We only included young adults of normal body mass index, so our results may not be applicable to other age groups or to those that are already overweight or obese. However, young adulthood is critical period for rapid weight gain, and obesity development in both the US25 and the UK.26 Our fixed-order design may have resulted in relatively conservative results. Period 2 was 10 weeks without calorie labelling, but we did not introduce any ‘washout period’ which may not have allowed calorie choices to return to true baseline. There was a significant increase in the mean number of calories chosen during this period but we cannot be sure if there would be an even higher increase should the participants had a washout period.
Conclusions
Prominent calorie labelling can lead to significant reductions in calories, fat, saturated fat and sodium content of the meals chosen by young adults. Although calorie labelling also led to a significant reduction in most micronutrients, intake of those was not impaired as most of them were well above the recommended levels. Providing simple nutrition information in the form of calorie labelling seems to be sufficient for preventing weight gain and reduce fat and saturated fat intake. Wider adoption of calorie labelling in all businesses providing food, irrespective of their size and setting guidelines/legislation on the formatting and placement of calorie labels should be the next steps in public health policies.
References
World Health Organization (WHO) 2014: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 10 April 2015).
Unites States Department of Agriculture Economic Service Research (USDA) http://www.ers.usda.gov/topics/food-choices-health/food-consumption-demand/food-away-from-home.aspx (accessed on 10 April 2015).
Young LR, Nestle M . The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002; 92: 246–249.
Lin B-H, Guthrie J, Frazao E Nutrient contribution of food away from home. In: Frazao E (ed.) America's Eating Habits: Changes and Consequences, vol 750. US Dept of Agriculture, Economic Research Service: Washington, DC, USA, 1999.
Department for Environment, Food and Rural Affairs. Family Food https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/193804/familyfood-2011report.pdf (accessed on 23 August 2014).
Urban LE, Lichtenstein AH, Gary CE, Fierstein JL, Equi A, Kussmaul C, Dallal GE, Roberts SB . The energy content of restaurant foods without stated calorie information. JAMA Intern Med 2013; 173: 1292–1299.
Scourboutakos MJ, Semnani-Azad Z, L’Abbe MR . Restaurant meals: almost a full day’s worth of calories, fats, and sodium. JAMA Intern Med 2013; 100: 6–23.
Block JP, Condon SK, Kleinman K, Mullen J, Linakis S, Rifas-Shiman S, Gillman MW . Consumers' estimation of calorie content at fast food restaurants: cross sectional observational study. Br Med J 2013; 346: f2907.
Farley TA, Caffarelli A, Bassett MT, Silver L, Frieden TR . New York City‘s flight over calorie labelling. Health Affair 2009; 28: w1098–w1109.
New York State Rest Assoc v New York City Bd of Health, Declaration of David B. Allison, PhD, No. 08 Civ 1000 (RJH) (SDNY 2008).
US Food and Drug administration (FDA). Menu and Vending Machines labelling requirements 2015: http://www.fda.gov/Food/IngredientsPackagingLabeling/LabelingNutrition/ucm217762.htm (accessed on 10 April 2015).
Foods Standards Australia and New Zealand. Labelling http://www.foodstandards.gov.au/industry/labelling/pages/default.aspx (accessed on 10 April 2015).
Department of Health. Responsibility Deal https://responsibilitydeal.dh.gov.uk/ (accessed on 10 April 2015).
Nikolaou CK, Hankey CR, Lean MEJ . Calorie-labelling: Does it impact on calorie purchase in catering outlets and the views of young adults? Inter J Obes 2015; 39: 542–545.
Elbel B, Kersh R, Brescoll VL, Dixon B . Calorie-labeling and food choices: A first look at the effects on low-income people in New York city. Health Affair 2009; 10: 1377.
Department of Health. Technical guidance on voluntary calorie labelling for catering businesses 2011 http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publichealth/Publichealthresponsibilitydeal/BecomingaResponsibilityDealpartner/DH_126217 (accessed on 10 April 2015).
Nikolaou CK, Hankey CR, Lean MEJ . Preventing weight gain with calorie labelling. Obesity (Silver Spring) 2014; 22: 2277–2283.
Food Standards Agency. FSA nutrient and food based guidelines for UK institutions http://www.food.gov.uk/multimedia/pdfs/nutguideuk.pdf.
World Health Organization (WHO) Dietary Recommendations/Nutritional requirements http://www.who.int/nutrition/topics/nutrecomm/en/ (accessed on 10 April 2015).
Ludwig DS, Brownell KD . Public health amid scientific uncertainty: The case of restaurant calorie-labelling regulations. JAMA 2009; 302: 434–435.
Grunert KG, Wills JM . A review of European research on consumer response to nutrition information on food labels. J Public Health 2007; 15: 385–399.
News From the Centers for Disease Control and Prevention. Restaurant Customers Do Use Calorie Information on Menus. JAMA 2014; 312: 883.
Berman M, Lavizzo-Marey R . Obesity prevention in the information age: Caloric information at the point of purchase. JAMA 2008; 300: 433–435.
Blumenthal K, Volpp KG . Enhancing the effectiveness of food labeling in restaurants. JAMA 2010; 303: 553–554.
Lewis CE, Jacobs DR, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, Williams OD . Weight gain continues in the 1990 s: 10-year trends in weight and overweight from the CARDIA study. Am J Epidemiol 2010; 151: 1172–1181.
Lean MEJ, Katsarou C, McLoone P, Morrison DS . Changes in BMI and waist circumference in Scottish adults: use of repeated cross-sectional surveys to explore multiple age groups and birth-cohorts. Int J Obes 2013; 37: 800–808.
Acknowledgements
We would like to thank the catering staff for assisting us in the conducting of this study. CKN conceived the idea, carried out the study, collected and analysed the data, written and reviewed the manuscript, CRH reviewed the manuscript, MEJL conceived the idea, analysed the data, wrote and reviewed the manuscript. CKN received a scholarship from the State Scholarship Foundation of Greece.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nikolaou, C., Hankey, C. & Lean, M. Effects of calorie labelling on macro- and micro-nutrients in main-meal choices made by young adults. Eur J Clin Nutr 70, 386–392 (2016). https://doi.org/10.1038/ejcn.2015.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.175
- Springer Nature Limited
This article is cited by
-
Large-scale regionalised LCA shows that plant-based fat spreads have a lower climate, land occupation and water scarcity impact than dairy butter
The International Journal of Life Cycle Assessment (2020)