Abstract
Background/Objectives:
High salt intake is a well-recognized risk factor of osteoporosis for its modulating effect on calcium metabolism. To understand the effect of dietary sodium on bone turnover, we evaluated the association between urinary sodium excretion and bone turnover markers in Korean postmenopausal women with low bone mass.
Subjects/Methods:
A retrospective review of medical records at a single institution identified 537 postmenopausal women who were first diagnosed with osteopenia or osteoporosis between 2008 and 2013. Subjects were stratified by low (<2 g/day, n=77), moderate (2–4.4 g/day, n=354) and high (⩾4.4 g/day, n=106) sodium excretion. A 24-h urine was collected to estimate sodium, calcium and creatinine. Bone turnover markers and calciotropic hormones were measured in serum. Bone mineral density (BMD) was assessed using dual-energy X-ray absorptiometry.
Results:
Sodium intake was positively associated with urinary sodium excretion (P=0.006, r=0.29). Bone turnover markers were significantly higher in the moderate-to-high urinary sodium excretion group (⩾2 g/day) than in the low urinary sodium excretion group (<2 g/day); CTX-I (C-telopeptides of type I collagen) was 21.3% higher (P=0.001) and osteocalcin (OC) was 15.7% higher (P=0.004). Calciotropic hormones and BMD were not significantly different across the sodium excretion groups.
Conclusions:
High urinary sodium excretion (⩾2 g/day) increased bone turnover markers in Korean postmenopausal women, suggesting that excessive sodium intake might accelerate bone turnover.
Similar content being viewed by others
Introduction
According to the 2011 Korea National Health and Nutrition Examination Survey (KNHANES V-2), the average daily sodium intake is 6172 mg for males and 4172 mg/day for females.1 However, World Health Organization (WHO) recommends that adults consume <2000 mg of sodium per day.2 Public health implications of high sodium intake have largely focused on cardiovascular end points but have not sufficiently examined other organ systems such as the skeletal system.
The prevalence of osteoporosis among Korean women over 50 years old is 38.7%3 and is substantively higher than the prevalence of 10% reported by the 2010 and 2012 National Center for Health Statistics in the United States4, 5 and the prevalence of 30% in five European countries (France, Germany, UK, Italy and Spain).6 One of the important factors leading to this difference could be excessive daily sodium intake among Korean women.
Although the role of calcium in the prevention and treatment of osteoporosis is well established, less emphasis has been placed on factors that may modulate calcium metabolism—such as, sodium.7, 8 The higher sodium intake among Korean women may contribute to their higher rates of osteoporosis because a high-sodium diet induces hypercalciuria and contributes to a negative calcium balance, even with a high-calcium diet.9 Even though the increased mobilization of calcium stores with high sodium intake may contribute to osteoporosis,10 there are some controversies; one study shows that sodium excretion has no effect on bone mass,11 and others suggest a negative correlation between sodium excretion and bone mass.12, 13 Moreover, the association between dietary sodium intake and bone turnover markers has not been studied extensively. One study shows no effect of high sodium intake on serum osteocalcin (OC) or serum C-telopeptides of type I collagen (CTX-I), although reducing sodium intake decreases serum OC by approximately 3%.14 Laura et al. also report that serum propeptide of type I collagen, a bone formation marker, is significantly decreased with a low-sodium diet.15 Because the effect of excessive sodium intake on bone turnover has not been well established, we aimed to assess changes of bone turnover markers according to the amount of urinary sodium excretion, which is closely associated with dietary sodium intake in Korean postmenopausal women with low bone mass.
Materials and methods
Subjects
We reviewed the medical records retrospectively. Postmenopausal women who were at least 1 year past menopause were included. Participants were first diagnosed with osteopenia or osteoporosis at the health promotion center of the Samsung Medical Center (Seoul, Korea), which is used for medical checkups in the general population, and were subsequently referred to the Division of Endocrinology and Metabolism between March 2010 and March 2013. Dietary sodium and calcium consumption was assessed in 86 subjects using a modified food frequency questionnaire (FFQ) based on the one used in the KNHANES. We classified these subjects as the confirmation group, in which we intended to confirm the correlation between dietary sodium intake and urinary sodium excretion. After analyzing this association in the confirmation group, we selected the verification group retrospectively to assess the association between urinary sodium excretion and bone turnover markers. The subjects in the verification group were first diagnosed with osteopenia or osteoporosis at the outpatient clinic of the Department of Endocrinology and Metabolism between March 2008 and March 2013. This population included individuals who visit health promotion center for medical checkups from the general population and subsequently referred and who were referred from the outpatient department of another division. A total of 833 subjects were initially selected for the verification group. Subjects with history of kidney transplantation, primary hyperparathyroidism and rheumatoid arthritis were excluded. Subjects were also excluded if they had taken corticosteroids, estrogen, supplemental calcium, anticonvulsant agents, diuretics such as thiazide within 6 months of the study, bisphosphonates, parathyroid hormone and antihormonal agents for cancer therapy (such as breast cancer). Patients with an estimated glomerular filtration rate <60 ml/min/1.73 m2 (according to Modification of Diet in Renal Disease study equation) were also excluded. After exclusion, a total of 537 subjects were analyzed as the verification group, which consisted of Korean women between 41 and 86 years who were at least 1 year past menopause and serum follicle-stimulating hormone levels were >40 mIU/ml. Among them, 68 patients had cessation of menstruation after hysterectomy. This study was approved by the Institutional Review Board at the Samsung Medical Center.
Measurements
Bone formation and resorption biomarkers, calciotropic hormones, such as intact parathyroid hormone and serum 25-hydroxyvitamin D (D2+D3), and baseline serum electrolyte, calcium, phosphorus, magnesium and creatinine were retrospectively obtained from electronic medical records. Blood samples were collected in the morning after an overnight fast of >8 h. All blood samples were obtained at the first visit to the outpatient clinic and before the commencement of osteoporosis or osteopenia treatment. Serum OC, a marker of bone formation, and serum CTX-I, a marker of bone resorption, were measured by electrochemiluminescence immunoassay (Roche Modular Analytics E170 (Roche Diagnostics, Mannheim, Germany)). In our laboratory, the interassay coefficient of variation ranged from 1.8 to 2.3% for OC and 2.6 to 2.9% for CTX-I. Serum bone alkaline phosphatase (ALP), a marker of bone formation, was measured by ELISA (Ostase Bone specific alkaline phosphatase EIA, Immunodiagnostic Systems, IDS, Boldon, UK) and had an interassay coefficient of variation of 3.7–6.4%. Serum parathyroid hormone (PTH) was measured by radioimmunoassay (kit from CIS bio, Automatic Gamma Counter GAMMA-10 2.0, Codolet, France) and had an interassay coefficient of variation of 9.5–11.5%. Serum 25-hydroxyvitamin D was measured by LC-MS/MS (Agilent 6460 triple-quadrupole mass spectrometer (Agilent Technologies, Inc., Santa Clara, CA, USA)) and had an interassay coefficient of variation of 2.8–3.4% for D2 and 3.0% for D3. Baseline bone mineral density (BMD) was measured by dual-energy X-ray absorptiometry using either Lunar Prodigy Advance (448 patients) or Hologic Delphi W (89 patients). In accordance with WHO criteria, osteopenia was defined as a T-score between −1 and −2.5 and osteoporosis as a T-score of <−2.5 for the lumbar spine, femur neck or total hip. The different measurement devices for BMD were adjusted for in the regression analysis of urine sodium excretion and BMD. Current smoking status, coffee intake and age of menopause were obtained by self-report questionnaires.
Assessment of dietary sodium intake in the confirmation group
All subjects in the confirmation group completed the modified FFQ during a health-care examination at the health promotion center on the basis of dietary intake over the previous 3 months. The modified FFQ was composed of 71 questions that assessed consumption frequency of 63 food items in 11 food groups. The detailed contents of food groups and frequency of servings were the same as the FFQ used in the KNHANES.16 The ‘modified FFQ’ was used in the Samsung Medical Center to promote better understanding and easier recall of food groups and consumption frequency.
Assessment of sodium excretion
Before the administration of medications for osteoporosis or osteopenia, 24-h urine samples were collected from all patients to estimate urinary sodium, calcium and creatinine excretion. Urine sodium was measured using an ion-selective electrode, calcium was measured using ocresolphthalein complexone method and creatinine was measured by the Jaffe method using the COBAS Integra 800 (Roche Diagnostics). We classified subjects into low (<2 g/day), moderate (2–4.4 g/day) and high sodium excretion groups (⩾4.4 g/day). Cutoff point of the lower sodium level was chosen on the basis of the recommended daily sodium amount by WHO.2 Cutoff point of the upper sodium level to delineate between the moderate and high sodium excretion was chosen on the basis of a recent study on sodium intervention.9
Statistical analysis
Statistical analyses were performed using SPSS statistics 21.0 (SPSS, Inc. Chicago, IL, USA). Kruskal–Wallis tests were used to analyze the differences in age, years since menopause (YSM), mean urinary calcium excretion and calciotropic hormones across the urinary sodium excretion groups. Mann–Whitney tests were used to compare between pairs of groups when appropriate. Bone turnover markers including serum OC, CTX-I and bone ALP across the urinary sodium excretion groups were assessed using one-way analysis of variance. Bonferroni correction was used in the post hoc analysis of the between-group comparisons to account for the number of comparisons performed. An analysis-of-covariance model, including bone turnover markers, urinary sodium excretion and the interaction between the two, was fit to assess the heterogeneity of bone turnover markers levels across YSM duration.17, 18, 19 All other data, which were parametrically distributed and expressed as means and standard deviation (s.d.), were analyzed using analysis of variance. A P-value<0.05 was considered statistically significant.
Results
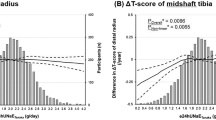
Table 1 shows the baseline characteristics of our study population. Among the 86 subjects in the confirmation group, the average daily sodium and calcium intakes were 3465 and 813 mg. Linear correlation between the amount of daily sodium intake (mg/day) and urinary sodium excretion (mg/day) was statistically significant (P=0.006, r=0.29). Patients in the verification group (n=537) were stratified into low (n=77), moderate (n=354) and high urinary sodium excretion group (n=106). Age, YSM, body weight, body mass index, smoking status and coffee intake were similar across these three groups. Baseline sodium excretion/creatinine ratio (mg/g Cr) (P<0.001) and calcium excretion/creatinine ratio (mg/g Cr) (P=0.004) were higher in the moderate and high urinary sodium excretion groups compared with the low urinary sodium excretion group (Table 2), and the correlation between these two variables was statistically significant (P<0.001, r=0.202, data not shown). The intact PTH (P=0.21) and 25-hydroxyvitamin D (P=0.794) were similar across the groups (Table 2). Average baseline serum markers of bone formation and bone resorption were significantly different across the three urinary sodium excretion groups (CTX-I; P=0.003, OC; P=0.001, bone ALP; P=0.025; Table 3). Specifically, serum CTX-I was higher in the moderate and high urinary sodium excretion groups, respectively, than in the low urinary sodium excretion group (P=0.001 and P=0.01, respectively), as were serum OC (P=0.001 and P=0.043, respectively) and serum bone ALP (P=0.015 and P=0.009, respectively) (Figure 1). Serum CTX-I was 21.3% higher (P=0.001), serum OC was 15.7% higher (P=0.004) and serum bone ALP was 9.5% higher (P=0.174) in individuals with sodium excretion ⩾2 g/day than in those with <2 g/day (Figure 2). Differences in bone turnover markers were maintained even after adjustment for duration of YSM (P=0.002 for CTX-1 and P=0.006 for OC; Table 3). BMD of the lumbar spine (LS; P=0.296), femoral neck (FN; P=0.969) and total hip (TH; P=0.419) were not different among the urinary sodium excretion groups (Table 4). Urinary sodium excretion and BMD were not significantly associated after adjustment for body weight, YSM, age and BMD device (Lunar versus Hologic) (LS; P=0.743, FN; P=0.299, TH; P=0.155, data not shown).
Baseline bone turnover markers according to urinary sodium excretion amount. Bars represent the means and SE. *Differences across the three urinary sodium excretion groups, P<0.05; by analysis of variance test. †Low vs moderate, P=0.001; low vs high, P=0.01; moderate vs high, P=0.526; ‡low vs moderate, P=0.001; low vs high, P=0.043; moderate vs high, P=0.086. §low vs moderate, P=0.015; low vs high, P=0.009; moderate vs high, P=0.601. (By Mann–Whitney test, significant differences P<0.017 applied by Bonferroni’s correction.)
Discussion
Although the WHO recommends that adults consume <2000 mg of sodium per day,2 the 2011 data from Korea National Health and Nutrition Examination Survey (KNHANES V-2) show that the average Korean adult intakes 5158 mg sodium per day,1 which is much higher compared with the 3436 mg reported in the United States,20 3900–4200 mg in Central Europe and Middle East/North Africa and 3400–3800 mg in Western Europe and Australia/New Zealand.21 Actually, most Korean food and condiments are high in salt. Despite recommendations to reduce sodium intake,2, 22 salt consumption still exceeds physiologic need for sodium. This excessive intake of sodium is associated with adverse clinical outcomes and has been a significant health issue worldwide.23
Our analysis of the confirmation group confirmed the positive correlation between dietary sodium intake (mg/day) and urinary sodium excretion (mg/day) (P=0.006). The quantity of sodium in a 24-h urine specimen is similar to the quantity of sodium ingested in the absence of hydration disorders or a large change in volume load.24 The correlation coefficient we found was similar to that of a previous study on sodium and calcium intake in postmenopausal women.13 We observed a significant increasing urinary calcium excretion in excessive urinary sodium excretion groups (⩾2 g/day, P=0.004), which supports observations from cross-sectional and cohort studies.12, 25, 26, 27 We then analyzed baseline levels of serum bone turnover markers in postmenopausal women (verification group) stratified by urinary sodium excretion amount (low, moderate and high).
The major finding of our study was that serum bone turnover markers were significantly higher in the excessive urinary sodium excretion group (⩾2 g/day) than in the low urinary sodium excretion group (<2 g/day) (Figure 2). High bone turnover markers in postmenopausal women might indicate rapid bone loss. A previous study shows that serum bone ALP levels were 28% higher and serum OC was 21% higher in postmenopausal women with rapid bone loss than in those with slow bone loss.28 The study also shows that odds of rapid bone loss are 1.8–2.0 times higher for each s.d. that the bone ALP and OC are away from the mean. Gerdhem et al.29 report that bone resorption markers, including serum CTX-I, are consistently higher in women who have sustained at least one fracture than in those without any history of fracture, and individuals with high serum CTX-I were 2.15 times more likely to sustain at least one fracture (95% confidence interval, 1.41–3.28). As demonstrated in these recent studies, biochemical markers of bone formation and resorption are strongly associated with rapid bone loss and higher levels increase the probability of rapid bone loss. In particular, serum CTX-I, which was significantly higher in both the moderate and high urinary sodium excretion group (⩾2 g/day) in our study, is considered one of the most accurate predictors of fracture risk.30, 31 Biochemical markers may provide a representative indication of overall skeletal bone loss and may predict fracture risk earlier and more accurately than measured rates of change in BMD at a single skeletal site.28, 32, 33, 34 Moreover, evaluation of rapid bone loss through serial estimations of BMD is time-consuming in clinical settings, whereas increased bone turnover markers may indicate increasing fracture risk in a more timely manner independent of current BMD.28, 32, 35, 36, 37, 38, 39, 40 We demonstrated that excessive urinary sodium excretion (⩾2 g/day) increased bone turnover markers; hence, we could suggest that excessive dietary sodium intake may accelerate bone turnover rate and can predict rapid bone loss.
The correlation between bone turnover markers and sodium intake in previous studies is inconsistent so far. Although low sodium intake has been thought to decrease bone turnover markers, no published data have shown that high sodium intake increases them. In addition, no studies have investigated the effects of excessive sodium intake on bone turnover markers in patients with low bone mass. Teucher et al.9 report that the bone resorption markers, serum pyridinoline and deoxypyridinoline, are significantly increased only with low-calcium diets (P<0.05) and are not significantly changed with a low-sodium intervention diet. Conversely, Laura et al. report that serum propeptide of type I collagen is significantly lower with a low-sodium diet.15 Another study shows that high sodium intake does not affect serum OC and CTX-I, although reducing sodium intake decreases the serum OC by about 3% (P<0.01).14
Biochemical markers were not significantly different between the moderate (2–4.4 g/day) and high urinary sodium excretion groups (⩾4.4 g/day), suggesting that dietary sodium intake above the current WHO recommendation level has negative effects on bone metabolism by accelerating the rate of bone turnover. However, there might be no further increase in bone turnover markers as urinary sodium excretion increased above the 2 g/day.
In our study, calciotropic hormones, including intact PTH and 25-hydroxyvitamin D, were not different across the three urinary sodium excretion groups. Some studies suggest that PTH and calcitriol increase with higher urinary sodium excretion to compensate for urinary calcium losses,14, 41, 42 although the relationship between PTH and urinary sodium excretion is controversial, especially in postmenopausal women. The increase in PTH and calcitriol with salt loading is observed in young adults but not in postmenopausal women, indicating a lack of adaptation to high salt intake in older women.43, 44 Furthermore, postmenopausal women do not increase calcium absorption, which may be due to impairments in calcitriol synthesis,45 intestinal resistance to 1,25-dihydroxycholecalciferol46 or loss of estrogen.47 These findings from previous studies may explain the lack of differences in calciotropic hormones across the urinary sodium excretion groups in our study.
BMD was not different across the urinary sodium excretion groups in our study. A single 24-h urinary sodium excretion measurement likely does not reflect the long-term dietary habits and may not be accurate for analyzing the association between dietary sodium intake and BMD. In addition, we could not analyze serial BMD measurements to assess the response according to urinary sodium excretion amount, which may be a more accurate assessment of bone status in response to dietary sodium intake compared with the single BMD measurement.
Our study had some limitations. We collected only one 24-h urine sample to estimate sodium and calcium excretion. Multiple 24-h urine samples give a more accurate estimate of sodium intake because they better reflect their usual diet over a long period of time.48 We analyzed the correlation between sodium intake and the 24-h urinary sodium excretion in the confirmation group to compensate for this limitation and directly confirm the association between intake and excretion. The subjects in the verification group who had either osteopenia or osteoporosis were started on calcium and vitamin D supplements or bisphosphonate agents after the first visit to our clinic. Because the subjects needed prompt treatment, we were unable to follow-up the changes of bone turnover markers and BMDs. Finally, this is a single-center-designed study, and thus the results could not be generalized to the overall population.
In conclusion, high urinary sodium excretion (⩾2 g/day) was associated with increased bone turnover markers in Korean postmenopausal women, suggesting that excessive sodium intake might accelerate bone turnover rate. Additional long-term trials, including assessment of serial BMDs and fracture incidences, are needed to confirm the effect of high-sodium diet on bone health.
References
Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Korea Centers for Disease Control and Prevention: Seoul, Korea, 2012.
Guideline: Sodium Intake for Adults and Children. World Health Organization: Geneva, Switzerland, 2012.
Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3). Korea Centers for Disease Control and Prevention: Seoul, Korea, 2010.
Centers for Disease Control and Prevention Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005–2008 [cited by 2014 May 10]. Available from http://www.cdc.gov/nchs/data/databriefs/db93.htm.
Centers for Disease Control and Prevention Healthy people 2010 final review. Arthritis, osteoporosis, and chronic back conditions (accessed on 10 May 2014). Available from www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review_focus_area_02.pdf.
Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O'Malley CD . Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos 2014; 9: 182.
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE . Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 1997; 337: 670–676.
Dawson-Hughes B . Calcium and vitamin D nutritional needs of elderly women. J Nutr 1996; 126: 1165S–1167S.
Teucher B, Dainty JR, Spinks CA, Majsak-Newman G, Berry DJ, Hoogewerff JA et al. Sodium and bone health: impact of moderately high and low salt intakes on calcium metabolism in postmenopausal women. J Bone Miner Res 2008; 23: 1477–1485.
Zarkadas M, Gougeon-Reyburn R, Marliss EB, Block E, Alton-Mackey M . Sodium chloride supplementation and urinary calcium excretion in postmenopausal women. Am J Clin Nutr 1989; 50: 1088–1094.
Dawson-Hughes B, Fowler SE, Dalsky G, Gallagher C . Sodium excretion influences calcium homeostasis in elderly men and women. J Nutr 1996; 126: 2107–2112.
Nordin BE, Need AG, Morris HA, Horowitz M . The nature and significance of the relationship between urinary sodium and urinary calcium in women. J Nutr 1993; 123: 1615–1622.
Devine A, Criddle RA, Dick IM, Kerr DA, Prince RL . A longitudinal study of the effect of sodium and calcium intakes on regional bone density in postmenopausal women. Am J Clin Nutr 1995; 62: 740–745.
Lin PH, Ginty F, Appel LJ, Aickin M, Bohannon A, Garnero P et al. The DASH diet and sodium reduction improve markers of bone turnover and calcium metabolism in adults. J Nutr 2003; 133: 3130–3136.
Carbone LD, Barrow KD, Bush AJ, Boatright MD, Michelson JA, Pitts KA et al. Effects of a low sodium diet on bone metabolism. J Bone Miner Metab 2005; 23: 506–513.
Ministry of Health & Welfare, Korea Centers for Disease Control and Prevention Korea Health Statistics 2007: Korea National Health and Nutrition Examination Survey (KNHANES IV-1). Korea Centers for Disease Control and Prevention: Seoul, Korea, 2008.
Garnero P, Sornay-Rendu E, Chapuy MC, Delmas PD . Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J Bone Miner Res 1996; 11: 337–349.
Garnero P, Mulleman D, Munoz F, Sornay-Rendu E, Delmas PD . Long-term variability of markers of bone turnover in postmenopausal women and implications for their clinical use: the OFELY study. J Bone Miner Res 2003; 18: 1789–1794.
Chaki O, Yoshikata I, Kikuchi R, Nakayama M, Uchiyama Y, Hirahara F et al. The predictive value of biochemical markers of bone turnover for bone mineral density in postmenopausal Japanese women. J Bone Miner Res 2000; 15: 1537–1544.
Centers for Disease Control and Prevention (CDC). Sodium intake among adults - United States, 2005-2006. MMWR Morb Mortal Wkly Rep 2010; 59: 746–749.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013; 3: e003733.
Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 2012; 126: 2880–2889.
Kotchen TA, Cowley AW Jr, Frohlich ED . Salt in health and disease—a delicate balance. N Engl J Med 2013; 368: 1229–1237.
Audran M, Legrand E . Hypercalciuria. Joint Bone Spine 2000; 67: 509–515.
Sabto J, Powell MJ, Breidahl MJ, Gurr FW . Influence of urinary sodium on calcium excretion in normal individuals. A redefinition of hypercalciuria. Med J Aust 1984; 140: 354–356.
Jones G, Beard T, Parameswaran V, Greenaway T, von Witt R . A population-based study of the relationship between salt intake, bone resorption and bone mass. Eur J Clin Nutr 1997; 51: 561–565.
Shortt C, Madden A, Flynn A, Morrissey PA . Influence of dietary sodium intake on urinary calcium excretion in selected Irish individuals. Eur J Clin Nutr 1988; 42: 595–603.
Ross PD, Knowlton W . Rapid bone loss is associated with increased levels of biochemical markers. J Bone Miner Res 1998; 13: 297–302.
Gerdhem P, Ivaska KK, Alatalo SL, Halleen JM, Hellman J, Isaksson A et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res 2004; 19: 386–393.
Garnero P . Markers of bone turnover for the prediction of fracture risk. Osteoporos Int 2000; 11: S55–S65.
Johnell O, Oden A, De Laet C, Garnero P, Delmas PD, Kanis JA . Biochemical indices of bone turnover and the assessment of fracture probability. Osteoporos Int 2002; 13: 523–526.
Vasikaran S, Eastell R, Bruyere O, Foldes AJ, Garnero P, Griesmacher A et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 2011; 22: 391–420.
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD . Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 2002; 87: 1586–1592.
Delmas PD, Seeman E . Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with anti-resorptive therapy. Bone 2004; 34: 599–604.
Biver E, Chopin F, Coiffier G, Brentano TF, Bouvard B, Garnero P et al. Bone turnover markers for osteoporotic status assessment? A systematic review of their diagnosis value at baseline in osteoporosis. Joint Bone Spine 2012; 79: 20–25.
Szulc P, Delmas PD . Biochemical markers of bone turnover: potential use in the investigation and management of postmenopausal osteoporosis. Osteoporos Int 2008; 19: 1683–1704.
Garnero P, Hausherr E, Chapuy MC, Marcelli C, Grandjean H, Muller C et al. Markers of bone resorption predict hip fracture in elderly women: the EPIDOS Prospective Study. J Bone Miner Res 1996; 11: 1531–1538.
van Daele PL, Seibel MJ, Burger H, Hofman A, Grobbee DE, van Leeuwen JP et al. Case-control analysis of bone resorption markers, disability, and hip fracture risk: the Rotterdam study. BMJ 1996; 312: 482–483.
Akesson K, Ljunghall S, Jonsson B, Sernbo I, Johnell O, Gardsell P et al. Assessment of biochemical markers of bone metabolism in relation to the occurrence of fracture: a retrospective and prospective population-based study of women. J Bone Miner Res 1995; 10: 1823–1829.
Szulc P, Chapuy MC, Meunier PJ, Delmas PD . Serum undercarboxylated osteocalcin is a marker of the risk of hip fracture: a three year follow-up study. Bone 1996; 18: 487–488.
Zemel MB, Bedford BA, Standley PR, Sowers JR . Saline infusion causes rapid increase in parathyroid hormone and intracellular calcium levels. Am J Hypertens 1989; 2: 185–187.
Breslau NA, McGuire JL, Zerwekh JE, Pak CY . The role of dietary sodium on renal excretion and intestinal absorption of calcium and on vitamin D metabolism. J Clin Endocrinol Metab 1982; 55: 369–373.
Jacobs MJ, Breslau PJ, Greep JM, Lemmens HA . Clinical and rheological studies in patients with intermittent claudication. Atherosclerosis 1985; 55: 331–337.
McParland BE, Goulding A, Campbell AJ . Dietary salt affects biochemical markers of resorption and formation of bone in elderly women. BMJ 1989; 299: 834–835.
Prince R, Devine A, Dick I, Criddle A, Kerr D, Kent N et al. The effects of calcium supplementation (milk powder or tablets) and exercise on bone density in postmenopausal women. J Bone Miner Res 1995; 10: 1068–1075.
Pattanaungkul S, Riggs BL, Yergey AL, Vieira NE, O'Fallon WM, Khosla S . Relationship of intestinal calcium absorption to 1,25-dihydroxyvitamin D [1,25(OH)2D] levels in young versus elderly women: evidence for age-related intestinal resistance to 1,25(OH)2D action. J Clin Endocrinol Metab 2000; 85: 4023–4027.
Heaney RP, Recker RR, Stegman MR, Moy AJ . Calcium absorption in women: relationships to calcium intake, estrogen status, and age. J Bone Miner Res 1989; 4: 469–475.
Massey LK, Whiting SJ . Dietary salt, urinary calcium, and bone loss. J Bone Miner Res 1996; 11: 731–736.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, S., Joung, J., Cho, Y. et al. Effect of high dietary sodium on bone turnover markers and urinary calcium excretion in Korean postmenopausal women with low bone mass. Eur J Clin Nutr 69, 361–366 (2015). https://doi.org/10.1038/ejcn.2014.284
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.284
- Springer Nature Limited
This article is cited by
-
Spironolactone reduces biochemical markers of bone turnover in postmenopausal women with primary aldosteronism
Endocrine (2020)
-
High dietary sodium intake is associated with low bone mass in postmenopausal women: Korea National Health and Nutrition Examination Survey, 2008–2011
Osteoporosis International (2017)
-
Adherence to the 2006 American Heart Association’s Diet and Lifestyle Recommendations for cardiovascular disease risk reduction is associated with bone mineral density in older Chinese
Osteoporosis International (2017)