Abstract
Objectives
Electric scooters (e-scooters) have contributed to a rise in injury burden and emergency department (ED) utilization since their local introduction 3 years ago. This study is a novel collaboration between the City of Calgary’s Department of Transportation and emergency medicine researchers to better understand the nature and frequencies of e-scooter injuries. It quantifies the incidence and characteristics of e-scooter related injuries treated in Calgary EDs/urgent care centres (UCCs).
Methods
Administrative data from electronic medical records of all patients presenting to Adult Emergency Departments and one Urgent Care Centre in Calgary with an e-scooter related injury between July 8, 2019, and Oct 1, 2019, and May 22, 2020, and September 30, 2020 were collected. Additional data were obtained from paper EMS reports. Descriptive statistics were used to characterize injury-specific variables and comparisons were drawn between ED visits for other transportation modalities.
Results
1272 ED/urgent care visits were attributed to an e-scooter related incident. The majority of incidents occurred between 20:00 and 24:00 (47%). Most injuries occurred to the lower limb (54.8%), followed by facial injuries (42.9%). The overwhelming majority of injuries happened to the e-scooter drivers (97.6%). E-scooter injuries made up approximately 15% of all trauma presentations to Calgary area adult EDs during the e-scooter season and 1 in 1400 e-scooter rides resulted in a visit to an ED/UCC.
Conclusions
Traumatic ED visits related to e-scooter use represent an increasing burden of preventable injuries. This study identified specific characteristics to focus future education and public policy efforts on.
Résumé
Objectifs
Les scooters électriques (e-scooters) ont contribué à une augmentation du fardeau des blessures et de l’utilisation des services d’urgence (SU) depuis leur introduction locale il y a trois ans. Cette étude est une nouvelle collaboration entre le Département des transports de la Ville de Calgary et des chercheurs en médecine d’urgence afin de mieux comprendre la nature et la fréquence des blessures causées par le scooter électrique. Il quantifie l'incidence et les caractéristiques des blessures liées aux scooters électriques traitées dans les services d'urgence/soins d’urgence de Calgary.
Méthodes
Données administratives provenant des dossiers médicaux électroniques de tous les patients se présentant aux services d'urgence pour adultes et à un centre de soins d'urgence de Calgary avec une blessure liée à un scooter électrique entre le 8 juillet 2019 et le 1er octobre 2019 et entre le 22 mai 2020 et le 30 septembre 2020. Des données supplémentaires ont été obtenues à partir des rapports papier des SMU. Des statistiques descriptives ont été utilisées pour caractériser les variables spécifiques aux blessures et des comparaisons ont été établies entre les visites aux urgences pour les autres modes de transport.
Résultats
1 272 visites aux urgences ou aux soins d'urgence ont été attribuées à un incident lié à un scooter électrique. La majorité des incidents se sont produits entre 20 h 00 et 24 h 00 (47 %). La plupart des blessures se sont produites au niveau des membres inférieurs (54,8 %), suivies des blessures au visage (42,9 %). La grande majorité des blessures sont survenues chez les conducteurs de scooters électriques (97,6 %). Les blessures liées aux scooters électriques représentent environ 3,5 % de toutes les présentations de traumatismes dans les services d'urgence pour adultes de la région de Calgary et 1 sur 1 400 trajets en scooter électrique a entraîné l'admission dans un service d'urgence.
Conclusions
Les visites aux urgences traumatiques liées à l'utilisation des scooters électriques représentent une charge croissante de blessures évitables. Cette étude a identifié des caractéristiques spécifiques sur lesquelles il convient de concentrer les efforts futurs en matière d'éducation et de politique publique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known about the topic? |
Micromobility services such as shared electric scooter (e-scooter) companies are a new phenomenon that is changing the nature and frequency of traumatic transportation related injuries in the ED. |
What did this study ask? |
What is the current impact of e-scooter related injuries on healthcare resource utilization (ED visits, lab work and imaging, need for surgical intervention and hospital admission) and how does this compare to other forms of transportation-related injuries? |
What did this study find? |
E-scooters made up a small but important subset of all traumas presenting to Calgary ED/UCCs during the e-scooter season with most injuries involving the head and lower extremity. Most e-scooter riders did not report wearing a helmet. |
Why does this study matter to clinicians? |
While e-scooter injuries remain relatively uncommon compared to injuries from motor vehicle collisions, this topic is directly relevant to clinicians as this mode of transportation increases and as the majority of these injuries are possibly preventable. |
Introduction
Micromobility services such as Electric scooter (e-scooter) share companies are a new phenomenon that have, in their short 3 year history, proven to create disruptive alternate form of short-distance travel [1]. Since their first launch in Santa Monica, California in 2017, these businesses have spread to over 120 countries and have seen astounding profits. Lime and Bird are two of the largest e-scooter share companies in North America, and have been valued at more than $1.1 billion and $2 billion, respectively [2]. The share systems are intended to provide an alternative to motorized vehicles and bicycles and as a solution to the ‘last mile’ problem of a travel distance too short to drive but seems too long to walk. They are marketed as a convenient and cleaner alternative to personal automobiles [3]. In the summer of 2019, Lime and Bird launched their e-scooter share systems in Calgary, Alberta and continued to operate through the summer of 2020.
E-scooter’s contribution to injury and healthcare costs has been of rising concern. A rapid review of the impact of e-scooters on local healthcare resources reported significant injuries to upper and lower extremities as well as head injuries, facial fractures and lacerations/abrasions [1]. E-scooter critics have noted that they seem to be too fast for sidewalks, but not safe enough to be ridden on the street [4]. What’s more, most studies show that the vast majority of injured riders were not using a helmet [5]. Additionally, injuries sustained by e-scooter falls tend to require imaging and sometimes surgery and/or admission, incurring substantial cost to healthcare systems. This study is a unique partnership between the University of Calgary’s Department of Emergency Medicine at the Cumming School of Medicine and the City of Calgary’s Transportation Department. It aims to determine the rate and description of injury from e-scooter use and health resource utilization in addition to describing the incidence and characteristics of severe injuries transported by Emergency Medical Services (EMS).
Methods
Study design and time period
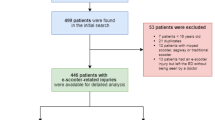
This study reviews administrative data from electronic medical records of all patients presenting to Adult Emergency Departments and one Urgent Care Centre in Calgary with an e-scooter related injury between July 8, 2019, and Oct 1, 2019, and May 22, 2020, and September 30, 2020 (246 days). An additional detailed chart review of paper medical records was conducted of patients who arrived via emergency medical services with the term “scooter” (and/or “mobility scooter, push scooter, e-scooter, motorized scooter, lime scooter, green scooter, rented scooter”) included in the triage note to understand the characteristics and behaviours of e-scooter operators who may have sustained more severe injuries and necessitated an EMS activation and transfer to an ED. One research assistant reviewed each paper chart in the secure Health Records Office and transcribed de-identified data onto the Case Report Form. We excluded charts that were obviously not an e-scooter (ie. mobility scooter), anyone less than 18 years of age or charts that were missing an EMS report in the paper chart. Ethics approval was provided by the University of Calgary’s Conjoint Health Research Ethics Board.
Data analysis
Demographic data and independent variables are reported in frequencies and analyzed as categorical variables using chi-square for strength of association.
Results
According to City of Calgary Department of Transportation estimates, 1.87 million E-scooters trips were made among 200,000 unique riders during the two-year City of Calgary E-scooter Pilot project. During this time, 1272 ED/urgent care visits were attributed to an e-scooter related incident, resulting in a rate of injury requiring an ED or urgent care visit of 1 ride in every 1400 e-scooter journey (Table 1) and an incidence of 0.95 injuries per 1000 residents. E-scooters made up 15% of all traumas presenting to Calgary ED/UCCs during the e-scooter season and were responsible for no fatalities or ICU admissions compared to other transportation modalities. In comparison, bicycle-related injuries, motor vehicle collisions and motorcycle-related injuries made up 43%, 33% and 9% of ED visits, respectively, during that same time period (Table 1).
The average age of an injured e-scooter rider was 34 years (18–67) and the majority were male (52%). Two patients were given the highest Canadian Triage and Acuity Scale (CTAS) for a closed head injury with skull, jaw and orbital fractures while the other was brought by EMS after being impaled by his e-scooter while riding.
The majority of all-comer e-scooter patients were triaged as CTAS 3 and 4. The most common anatomical injury among all e-scooter riders was a lower limb injury such as hip fractures, tibial/fibula fractures, ankle fractures, ligamentous injuries or lacerations, followed by upper limb injuries including hand and forearm fractures and head injuries, ranging from minor lacerations to facial bone fractures, mandibular fractures and orbital floor fractures. Over half of patients underwent diagnostic imaging in the ED. The most common imaging study was a radiograph (826, 64%) or computed tomography (169, 13%). 87 (7%) patients were admitted, and 94 (7%) patients underwent surgery within 30 days of their initial ED presentation. 1153 patients were discharged, one patient left against medical advice and 31 left before being assessed by an emergency physician.
The demographic and injury characteristics of patients with severe injuries that necessitated EMS transport to EDs/UCCs are presented in Table 2. Detailed chart reviews of these patients revealed that most injuries occurred between 20h00 and 24h00 and occurred on sidewalks and roadways. Of the 75 EMS transported injuries, 69 (92%) were drivers, at least 2 (3%) were passengers and 4 were pedestrians (non-riders: two people were hit while walking on sidewalk, one tripped over a parked e-scooter and one injury involved a cyclist). One excluded record included a person assaulted with a parked e-scooter. The two most common mechanisms of injury described by EMS reports were only using one hand or having one foot on the e-scooter while in motion or “losing control” when encountering a hazard in the built environment such as riding over gravel, potholes or transitioning over a curb. Of the EMS patients where alcohol intoxication was suspected, 28 had detectable levels of alcohol based on serum testing in the ED. Only three patients were documented as wearing a helmet (Fig. 1).
Discussion
To our knowledge, this is the first Canadian study to identify and explore the injury patterns and healthcare resource utilization after accidents involving e-scooters.
Interpretation of findings
While uncommon, e-scooter injuries are relevant as the majority of these injuries are likely preventable. A substantial proportion of injuries associated with e-scooter use are head injuries and cranio-facial injuries, with incidences in the literature reported to be as high as 40% and 58%, respectively [1, 6]. Our study attempted to capture helmet use by patient self-report; however, the majority of study records did not contain information about helmet use. A 2021 systematic review by Public Health Ontario also found that helmet use was rarely documented and, when it was, that helmet use was infrequent [5]. Knowing whether helmets were available and/or used would help inform future injury prevention strategies, specifically with respect to head and cranio-facial injuries [7, 8].
A unique mechanism of injury recorded in our study was related to the physical design/use of the e-scooter itself. Calgary saw a particularly high incidence of ankle injuries, specifically skin lacerations to the medial malleolus, resulting from a bolt on the back wheel of one company’s e-scooter frequently catching the rider’s right ankle when they propelled themselves forward.
Comparison to previous studies
Previous studies have documented the presence of serum alcohol levels as a variable associated with patient presentations for e-scooter injury. Between 4.8 and 33% of injuries were related to alcohol use according to a 2021 literature review conducted by Public Health Ontario [5]. Our study relied on clinician assessment and laboratory investigations ordered at the clinician’s discretion to quantify serum alcohol levels. Clinicians suspected alcohol as a contributing factor in 84 patients in our study, with 50 (4%) patients having a blood alcohol level above zero. We did not obtain information on illicit substances that may have been consumed prior to using an e-scooter.
People injured while operating electric scooters represent a relatively high proportion of health resource utilization. While our study reported an admission rate of 6%, previous studies report admission rates between 5.8 and 28.5% with between 7 and 25.4% requiring operative care after their mishaps. Additionally, a study by Allen et al. showed that 91% of those injured required imaging including plain film, CT scan, and MRI [9]. The same study found that 51.6% of injured riders were transported by EMS. A study by Beck et al. also found that, of those who required imaging, 78% received plain films and 24% received MRI scans, with 7% of those injured being transported by EMS[10].
Strengths and limitations
This study is limited by its reliance on administrative data and the use of the triage note to identify eligible ED/UCC visits. It is possible that our search term was over-inclusive and may have included a small number of mobility scooters that are not specifically e-scooters. Our data and conclusion were also limited by the use of EMS activation as a proxy for severity of illness. Lastly, this study was not designed to identify any risk factors for injuries.
Clinical implications
E-scooter use is on the rise in Calgary and, with it, we expect to see a rise in e-scooter related injuries. Being aware of common injury patterns as well as how to prevent them informs triage and resource utilization considerations and empowers clinicians in patient centred discussions about injury prevention.
Research implications
While this study was not designed to offer a thorough analysis of the harms of e-scooter use relative to the benefits of e-scooter use, future research could focus on the public health implications of micromobility services such as shared electric scooters, as in the case of cycling studies where the harms and benefits of use are better understood. Future studies should also look at comparing rates of injury among e-scooters to those among motorcycles, bicycles and cars, taking into account the larger distances travelled and accidents related to motorized vehicles that do not result in ED visits. Collaborations with private scooter companies would be beneficial to further understand operator behaviours and risk factors associated with e-scooter injury.
Conclusion
While providing a convenient and presumably enjoyable alternative to long walks or shorter drives, electric scooter share systems have also introduced an additional injury burden and resulted in increased utilization of emergency department and urgent care resources during the e-scooter season. The evidence thus far shows an array of injury types associated with e-scooter use. Furthermore, e-scooter injuries have proven to increase hospital admission rates, surgeries, imaging use, and EMS activation. Some of these injuries may have been prevented with the use of helmets and the avoidance of alcohol. Our study provides insight into injury patters and e-scooter user behavior and has contributed unique information to the development to City of Calgary public policy for e-scooter use.
References
Trivedi B, Kesterke MJ, Bhattacharjee R, Weber W, Mynar K, Reddy LV. Craniofacial injuries seen with the introduction of bicycle-share electric scooters in an urban setting. J Oral Maxillofac Surg. 2019;77(11):2292–7.
Lime. About us. Available from: https://www.li.me/about-us.
Laker L. Welcome, watch or ban: how should cities deal with electric scooters? The Guardian 2019: Available from: https://www.theguardian.com/cities/2019/jun/18/welcome-watch-or-ban-how-should-cities-deal-with-electric-scooters [Cited May 10, 2020]
Man Killed in Electric Scooter Crash in Washington DC. BBC. 2019: Available from: https://www.bbc.com/news/world-us-canada-45596449 [Cited May 10, 2019.]
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Berenbaum E. E-scooter injuries. Toronto: Queen’s Printer for Ontario; 2021.
Trivedi TK, Liu C, Antonio ALM, et al. Injuries associated with standing electric scooter use. JAMA Netw Open. 2019;2(1): e187381. https://doi.org/10.1001/jamanetworkopen.2018.7381.
Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev. 2000;2: CD001855.
Hagel BE, Yanchar NL, Beno S, Cyr C, Scott JW, Zelman M. Bicycle helmet use in Canada: the need for legislation to reduce the risk of head injury. Paediatrics Child Health (Canada). 2013;18(9):475–80.
Allen JR, English KC, Rix K, Brown CVR, Ziebell CM, Brown LH. 262 Epidemiology of Dockless electric rental scooter injuries. Ann Emerg Med. 2019;74(4):103.
Beck S, Barker L, Chan A, Stanbridge S. Emergency Department impact following the introduction of an electric scooter sharing service. Emerg Med Aust. 2019;32(3):409–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sheikh, M., Islam, A., Kroeker, N. et al. Electric scooter related injuries in Calgary emergency departments. Can J Emerg Med 24, 735–741 (2022). https://doi.org/10.1007/s43678-022-00378-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00378-x