Abstract
Background
The Schatzker classification system for tibial plateau fractures is one of the most commonly used systems. However, there has been controversy if a Schatzker III type fracture truly exists by their original definition. We aimed to correlate the radiographic and CT images of type III fractures, describe the additional propagating fracture patterns and determine if these fractures do exist by their original description.
Methods
This multicenter retrospective cohort observational study included patients with tibial plateau fractures across five trauma centers over 9 years were identified. All X-rays and CT scans were assessed. Two independent fellowship trained, Orthopaedic trauma surgeons reviewed all knee X-rays and classified them according to the Schatzker system. The CTs were subsequently reviewed and the fractures were reclassified based on CT findings.
Results
569 Tibial plateau fractures in 566 patients were analyzed. All X-ray classified Schatzker III fractures were reclassified to a Schatzker II type after review of CT scans by both assessors independently as there were always at least two or more fracture lines propagating from the depressed fragment to the lateral cortex in all cases. The interobserver variability as assessed by the kappa correlation coefficient (κ) for X-rays and CT-based classifications were κ = 0.274 and κ = 0.906, respectively. The majority of cases had two lateral cortical breaks (83.8%). In addition, the depression occurred mostly in the anterolateral and posterolateral positions (60.3%) of the lateral tibial plateau.
Conclusion
This study did not support the existence of true Schatzker Type III fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fractures comprise of approximately 1–1.2% of all fractures [1,2,3] and its incidence is 10.3 per 100,000 people annually [2]. Although there are around 38 classification systems for tibial plateau fractures described in literature [4], the 2 most commonly used are the AO/OTA and Schatzker systems [3, 5] with some authors suggesting that the Schatzker classification is the most widely adopted [1, 4].
Schatzker first described the six category classification system for tibial plateau fractures in his original paper published in 1974 [6]. Schatzker et al. revisited the classification system in 1979, based on a series of standard AP and lateral X-rays of 94 patients with tibial plateau fractures [7]. In this original classification system, a type III fracture was defined as a pure depression of the central articular surface of the lateral tibial plateau without a lateral wedge and with the lateral cortex intact.
With the increasing use of CT and MRI scans, it has been noted that the incidence of type III fractures is much lower with some authors suggesting that type III fractures may not exist due to the presence of occult fractures over the lateral cortex on advanced imaging [8,9,10]. However, there has not been any dedicated study to date investigating this claim as well as to describe the various complex fracture patterns that may be derived on CT imaging from X-ray identified type III fractures.
This paper aims to evaluate CT images of Xray-diagnosed Schatzker III fractures, to see if they truly exist. A secondary objective is to describe the fracture patterns and how they contribute to the misclassification of these fractures.
Methods
A multicenter retrospective cohort observational study was performed. Patients were identified across 5 trauma centers in the country over a period of 9 years from January 2008 to February 2017. This research was approved by the national ethics review board (NHG DSRB Ref: 2016/00741).
Keyword searches were performed on patient data that was retrieved from each institutions’ digital Pictures Archiving and Communicating System as well as the online operative records systems. This method of search ensured that all patients with tibial plateau fractures who had received either non-surgical or surgical management, regardless of initial radiographs or treatment that was performed at another institution, would be included in the study. A total of 740 patients were identified. All inpatient plain radiographs and CT scans for these 740 patients were screened by the first author. Patients with injuries other than tibial plateau fractures, those with existing hardware or periprosthetic/peri-implant fractures and those with missing or inadequate preoperative X-rays or CT imaging were excluded from the analysis.
The remaining patients’ plain radiographs were then reviewed by the first author again, and were classified according to the Schatzker system. Radiographs showing Schatzker III and equivocal Schatzker II/III fractures were compiled, randomized and presented to 2 blinded independent assessors separately, both of whom were fellowship trained Orthopaedic trauma consultants with at least 5 years of experience. The assessors reviewed all X-rays and reclassified the tibial plateau fractures according to the Schatzker classification. Corresponding CT images were then reviewed on another date and the fractures were reclassified again by the assessors.
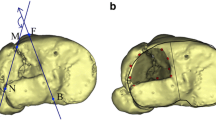
For fractures where either one or both assessors had classified as type III on plain X-rays and were identified as type II after CT review, further analysis was performed. For these cases, the position of the lateral plateau depression and the point at which the fracture exited the lateral cortex was noted. An imaginary line was drawn between the two tibial spines dividing the tibial plateau into the medial and lateral plateaus as per Kfuri and Schatzker’s description [11]. Subsequently, the lateral tibial plateau was divided into equal quadrants. Any fracture depression which had more than 50% of its largest cross sectional area in the predominant quadrant was labelled accordingly: anterolateral (AL), posterolateral (PL), anteromedial (AM) and posteromedial (PM) (Fig. 1). If the depression was largely lateral to the mid-sagittal line and had equal representation on the AL and PL quadrant, it was labelled as ‘lateral’ and if the depression was largely medial to the mid-sagittal line and was equally present on the AM and PM quadrants, it was ‘medial’. Similarly, if the depression was largely anterior to the mid-coronal line with equal representation on the AM and AL quadrants, it was ‘anterior’ and if the depression was largely posterior to the mid-coronal line with equal representation in the PM and PL quadrants, it was ‘posterior’. If the area of depression was equally represented in all four quadrants, it was ‘central’ (Fig. 2). The lateral tibial plateau was also divided into 12 equal parts to delineate a clock face and the position of the fracture exiting through the lateral cortex was noted accordingly (Fig. 3). The fracture lines in the right leg would exit from the 6 to 12 o’clock positions (i.e. 6, 7, 8, 9, 10, 11, 12) while that in the left leg would exit from the 12 to 6 o’clock positions (i.e. 12, 1, 2, 3, 4, 5, 6).
CT division of lateral plateau into quadrants. A The blue line dividing the medial and lateral tibial plateaus. The green line (mid coronal) and orange line (mid sagittal) dividing the lateral tibial plateau into four equal quadrants. B This case illustrates an anterior position of the depressed segment as it is in the anterior half of the lateral tibial plateau with equal distribution in the AL and AM quadrants
Clockface description of fracture lines exiting at the cortex. A The clockface delineating the pattern of facture lines exiting through the lateral cortex. Cases illustrating fracture lines, exiting the 2 and 4 o’clock positions (B), 10 and 7 o’clock positions (C), and 2, 4 and 6 o’clock positions (D)
Statistical methods
For continuous variables, the descriptive statistics were presented in frequencies, minimum, maximum, mean [standard deviation (SD)] and median [interquartile range (IQR)]. Inter-observer reliability was assessed by the kappa correlation coefficient (κ) as proposed by Cohen [12]. Interpretation of kappa coefficients and levels of agreement between assessors were determined by the levels of clinical agreement for diagnosis described by McHugh [13]: (κ) 0.0–0.20 (none), 0.21–0.39 (minimal), 0.40–0.59 (weak), 0.60–0.79 (moderate), 0.80–0.90 (strong) and > 0.9 (almost perfect).
Results
Out of the 740 patients who were identified during the study period, 569 tibial plateau fractures in 566 patients were finally included in the study as depicted in the patient flow chat (Fig. 4). There were 390 males (68.5%) and 176 females (31.5%) with an age range from 15 to 99 with a mean age of 49 (SD 15.3) and median age of 48 (IQR 22) years. The mean and median age of males was 45 (SD 13.2) and 44 (IQR 17) years, respectively, while that in females was 56 (SD 16.9) and 60 (IQR 23) years, respectively. 116 tibial plateau fractures were identified as Schatzker III and equivocal for Schatzker II/III by the first author.
The 2 senior assessors then independently analyzed the plain radiographs of the 116 fractures and classified them to the Schatzker system. The first assessor identified 47 Schatzker II fractures (40.5%), 66 Schatzker III fractures (56.9%), 1 Schatzker I fracture (0.862%) and 2 fractures that were unclassifiable under the Schatzker system (1.72%). The second observer identified 87 Schatzker II (75.0%) and 29 Schatzker III fractures (25.0%) (Table 1). Based on plain radiograph classification by the 2 assessors, the incidence of type III fractures in the 569 fractures included in the study was 11.6% and 5.1% respectively. The Cohen’s kappa (κ) evaluating the inter-observer reliability for X-ray interpretation suggested minimal agreement (κ = 0.274).
There were 68 cases that were identified by either one or both of the assessors to be type III fractures. Of these, these were 31 males and 37 females with an age range from 20 to 81 with a mean age of 52.4 (SD 15.9) and median age of 54 (IQR 26) years. Although there were less males than females, there was no significant difference in the mean and median age of patients who sustained type III fractures as compared to the rest of the population.
After review of corresponding CT images of 116 fractures, the assessors independently found the same 10 cases each, to be equivocal and subsequently reached a consensus for a final classification. Based on CT imaging, the first assessor identified 110 (94.8%) Schatzker II fractures, 5 Schatzker V fractures (4.31%) and 1 (0.862%) Schatzker I fracture (previously graded as radiographically non-Schatzker classifiable). The second assessor independently identified 111 Schatzker II fractures (95.7%) and the same 5 cases of Schatzker V fractures as the first assessor (Table 1). All previously X-ray classified Schatzker III fractures were reclassified on review of CT images to Schatzker II by both assessors independently. Cohen’s kappa (κ) of the CT images suggested almost perfect agreement (κ = 0.906). Some illustrative cases where a type III fracture identified on X-ray being reclassified to a type II after CT analysis are shown in Fig. 5.
68 cases were identified where either one or both assessors had classified the fracture as a type III on X-ray and were subsequently re-classified as type II after CT analysis. All 68 cases were noted to have at least 2 breaks in the lateral cortex. There were 22 PL (32.4%), 19 AL (27.9%), 9 lateral (13.2%), 2 anterior (2.94%), 3 posterior (4.41%) and 13 central (19.1%) depressions noted. There were no AM, PM or medial depressions noted over the lateral tibial plateau. There were 57 cases with 2 lateral cortical breaks (83.8%), 7 cases with 3 breaks (10.3%), 1 case with 4 and 5 breaks respectively (1.47% each) and 2 cases with 6 breaks (2.94%). The majority of all anterior fracture lines (56 out of 58 or 96.6%) exited from the 10–11 (right limb) and 1–2 (left limb) o’clock positions over the lateral tibial plateau, while the majority of posterior fracture lines (80 out of 90 or 88.9%) exited at the 7–8 (right limb) and 4–5 (left limb) o’clock positions. For those PL fractures with only 2 lateral cortical breaks, the majority of cases (13 out of 19 or 68.4%) had both cortical breaks exiting posteriorly whereas this was not the case for AL fractures where only 2 out of 18 cases (11.1%) had both cortical breaks exiting anteriorly. The summary of the above findings is presented in Tables 2 and 3.
87.2% of the lateral cortical breaks occurred in the AL (1–2 and 10–11 o’clock) and PL (4–5 and 7–8 o’clock) positions while 60.3% of the depressions also occurred in the AL and PL quadrants of the lateral tibial plateau. For PL depressed fractures, 69.4% of all cortical breaks occurred in the 4–5 and 7–8 o’clock positions. 56.4% of cortical breaks occurred in the 1–2 and 10–11 o’clock positions in AL depression fractures. In central depressions, 38.9% of breaks occurred in the 1–2 and 10–11 o’clock positions while almost a similar number of breaks (41.7%) occurred in the 4–5 and 7–8 o’clock positions. All cortical breaks in lateral depressions were found anterolaterally over the 1–2 and 10–11 o’clock positions and posterolaterally over the 4–5 and 7–8 o’clock positions. The summary of these findings is presented in Table 2.
Discussion
The Schatzker classification system for tibial plateau fractures is widely used by orthopedic surgeons to assess the initial injury, plan management, and predict prognosis [14]. Although Schatzker et al. [7] commented that the incidence of type III fractures was 36% and the most common fracture type in their series, there has been evidence that this is much lower with incidence of type III fractures reported between 3 and 11% of all tibial plateau fractures making them in fact, among the least common fracture type [15,16,17,18,19]. In our paper, the plain radiographic incidence of type III fractures was also low at 11.6% and 5.1%, respectively, as classified by the two independent assessors, in keeping with existing literature. Some authors have also commented that pure depressed lateral tibial plateau fractures may not actually exist [8,9,10].
In an MRI analysis of 103 tibial plateau fractures, Gardner et al. [9] found that there was no true Schatzker III fracture in their series. The authors noted that there was often a fracture line that occurred posteriorly in the sagittal plane of the MRI scans of previously X-ray classified Schatzker III type fractures. In a series of 45 tibial plateau fractures where plain radiographs, 2D and 3D CT images were compared, Doornberg et al. [8] commented that 3 out of the 6 assessors did not classify any depressed articular fractures of the lateral plateau as Schatzker type III as they always found that the lateral cortex was never intact. These fractures had been classified as type II instead. In a CT analysis of 514 tibial plateau fractures, Hua et al. [20] commented that the first 200 cases yielded no type III fractures. The authors commented that only after more data collection and a deeper understanding of the CT images, did they note that type III fractures exist but only account for a very small proportion (4 of 514, 0.78%). In their paper, the authors did not elaborate on the additional data that were collected and how the CT scans were analyzed for them to derive the incidence of type III fractures as 0.78% of their series. Our paper is the first study in literature dedicated to exclusively and methodically investigate the true occurrence of type III fractures.
In our study of 569 tibial plateau fractures, we found no fractures with a pure depression of the lateral tibial plateau. In the CT analysis of all the fractures determined as Schatzker III type on plain radiographs, there was always a fracture line propagating from the depressed fragment that extended to the lateral cortex. Albeit this fracture extension not being clearly seen in 10 cases, with careful review by the assessors, these fracture lines were more accurately detected on the CT axial cuts. Tibial plateau fractures occurred most commonly over the AL and PL quadrants (60.3%) followed by central depressions (19.1%). PL depressed fractures had majority (69.4%) of the cortical breaks occurring at the PL position (4–5 and 7–8 o’clock) while AL depressed fracture had most (56.4%) of that occurring at the AL position (1–2 and 10–11 o’clock). The occurrence of AL and PL positions of cortical breaks were almost similar in centrally depressed fractures. We hypothesize that it is because the majority of fracture lines occur in planes diagonal to the pure coronal or sagittal planes, that they are not apparent on plain radiographs and are best appreciated only on CT axial cuts. This is in contradistinction to the MRI findings in Gardner et al.’s study which were described in the sagittal plane [9].
Some authors subclassify type III fractures into those with a lateral tibial plateau depression (type IIIA) and those with a central depression (type IIIB) [14, 21]. The AO/OTA classification has also subdivided depressed lateral tibial plateau fractures (41B2.1) as having qualifications of being either AL, PL or central based on the quadrants stipulated by Kfuri et al. [11, 22]. In our series, we did not find any depression that was in the AM, PM or medial zones as defined in our paper suggesting that true centrally depressed fractures as stated by AO/OTA and other authors may not exist.
Though having its limitations, the popularity of the use of the Schatzker system is attributed by its familiarity and ease of use [1, 3]. A major limitation of the Schatzker classification is that it only addresses fracture lines in the sagittal plane [1]. CT has become the standard for pre-operative evaluation of tibial plateau fractures due to the need for accurate assessment of fracture displacement and depression which otherwise could frequently be misrepresented on plain radiographs [14]. The addition of 2D and 3D CT reconstructions have helped further improve inter-observer reliability of the Schatzker system, with kappa coefficients of up to 0.75 and 0.85 respectively [1, 3]. Literature also suggests that the Schatzker fracture classification, treatment plans and surgical approaches were changed with the addition of CT as compared to plain radiographs [8, 23, 24]. Our data are in keeping with existing evidence [4] that the interobserver reliability increases significantly when using CTs (κ = 0.906) as compared to only using X-rays (κ = 0.274).
The Schatzker classification was originally described based on plain radiographs. The increasing use of CT scans with three-dimensional reconstruction to classify fracture patterns introduces additional information into a system which was not developed for such [4]. Thus it is important to consider this when attempting to classify a tibial plateau fracture using the Schatzker system on a CT scan. This critique applies to our paper as well. However according to Schatzker’s original definition of a type III fracture which is that of a pure depression of the lateral tibial plateau with the lateral cortex intact, the use of CT imaging has proven that this type of fracture may not exist. Luo et al. [25], Chang et al. [26] and Krause et al. [27], more recently, have introduced their own CT classification systems which allow assessment of fractures in the axial plane which was previously not possible using plain radiographs. Acknowledging the drawbacks of plain X-rays and the original Schatzker classification system, Kfuri and Schatzker [11] revisited this and using additional information from CT scans, extended the original Schatzker system to add the third dimension to appreciate the architecture of the fracture and its spatial topography. However, the authors continue to mention that the extended system allows for pure depressed fractures to be identified by its precise location and if the rim is intact, presuming that such fractures exist.
Most authors recommend that in pure joint depressed fractures, the intact rim does not allow direct exposure and visualizing of the depressed fragments. Reduction is, therefore, achieved indirectly via instruments introduced to elevate the depressed segment through the creation of a metaphyseal window, and a buttress plate is often not necessary as the intact rim buttresses against further displacement [11, 28]. Our series shows that there is a lateral cortical break in all type III fractures and theoretically, this window can be used to access the main depressed fragment. However, we note that the majority of the breaks (57.7%) were in the posterolateral cortex where many surgeons would not choose to create their metaphyseal window due to the access difficulties arising from the fibula. Many of the lateral cortical breaks we noted on CT scans were also small and undisplaced which may not change the approach of fixation. Although our paper provides new information on Schatzker III fractures, further research is required to conclude if surgical strategies may change based on this new information.
Our large series is the first study to investigate the true occurrence of type III tibial plateau fractures. Scans were independently assessed by two experienced surgeons and a high degree of concordance was achieved. A drawback of this paper was that although the two assessors were independent for most part of the assessment, the equivocal nature of some CT scans required them to reach a consensus for a final accurate classification. Although this could have been overcome by higher quality CT and finer cuts, we were constrained by the retrospective nature of the study. Additionally, further research based on the complex fracture patterns brought to light from the results of this study, may need to be conducted to derive if this new information would clinically change surgical approach and management of type III fractures.
This study has shown that there is always a lateral cortical break seen on CT scans in all X-ray classified Schatzker III type fractures thus converting them by definition, to a Schatzker II type fracture. We found no true Schatzker III type fracture, suggesting that such fractures may not exist. The majority of our depressed fractures were located over the AL and PL quadrant of the lateral plateau and the corresponding lateral cortical breaks noted were over the AL and PL positions respectively. Despite this new CT information distinguishing type III to II fractures, further research is required to conclude if surgical strategies may change based on this new information.
Data availability
This is not applicable for this article.
References
Mthethwa, J., & Chikate, A. (2018). A review of the management of tibial plateau fractures. Musculoskeletal Surgery, 102(2), 119–127.
Elsøe, R., Larsen, P., Nielsen, N., Swenne, J., Rasmussen, S., & Østgaard, S. (2015). Population-based epidemiology of tibial plateau fractures. Orthopedics, 38, e780–e786.
Zeltser, D. W., & Leopold, S. S. (2013). Classifications in brief: Schatzker classification of tibial plateau fractures. Clinical Orthopaedics and Related Research, 471(2), 371–374.
Millar, S. C., Arnold, J. B., Thewlis, D., Fraysse, F., & Solomon, L. B. (2018). A systematic literature review of tibial plateau fractures: What classifications are used and how reliable and useful are they? Injury, 49(3), 473–490.
Marsh, J.L. (2000). Tibial Plateau Fractures. In: Obrant, K. (eds) Management of Fractures in Severely Osteoporotic Bone. Springer, London. https://doi.org/10.1007/978-1-4471-3825-9_21.
Schatzker, J. (1974). Compression in the surgical treatment of fractures of the tibia. Clinical Orthopaedics and Related Research®, 105, 220–239.
Schatzker, J., Mcbroom, R., & Bruce, D. (1979). The tibial plateau fracture: The Toronto experience 1968–1975. Clinical Orthopaedics and Related Research®, 138, 94–104.
Doornberg, J. N., Rademakers, M. V., van den Bekerom, M. P., Kerkhoffs, G. M., Ahn, J., Steller, EPh., et al. (2011). Two-dimensional and three-dimensional computed tomography for the classification and characterisation of tibial plateau fractures. Injury, 42(12), 1416–1425.
Gardner, M. J., Yacoubian, S., Geller, D., Suk, M., Mintz, D., Potter, H., et al. (2005). The incidence of soft tissue injury in operative tibial plateau fractures: A magnetic resonance imaging analysis of 103 patients. Journal of Orthopaedic Trauma, 19(2), 79–84.
Browner, B. D. (2009). Skeletal trauma: Basic science, management, and reconstruction. Elsevier Health Sciences.
Kfuri, M., & Schatzker, J. (2018). Revisiting the Schatzker classification of tibial plateau fractures. Injury, 49(12), 2252–2263.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46.
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276–282.
Markhardt, B. K., Gross, J. M., & Monu, J. (2009). Schatzker classification of tibial plateau fractures: Use of CT and MR imaging improves assessment. Radiographics, 29(2), 585–597.
Rademakers, M. V., Kerkhoffs, G. M. M. J., Sierevelt, I. N., Raaymakers, E. L. F. B., & Marti, R. K. (2007). Operative treatment of 109 tibial plateau fractures: Five- to 27-year follow-up results. Journal of Orthopaedic Trauma, 21(1), 5–10.
Zhang, B.-B., Sun, H., Zhan, Y., He, Q.-F., Zhu, Y., Wang, Y.-K., et al. (2019). Reliability and repeatability of tibial plateau fracture assessment with an injury mechanism-based concept. Bone & Joint Research, 8(8), 357–366.
Yang, G., Zhai, Q., Zhu, Y., Sun, H., Putnis, S., & Luo, C. (2013). The incidence of posterior tibial plateau fracture: An investigation of 525 fractures by using a CT-based classification system. Archives of Orthopaedic and Trauma Surgery, 133(7), 929–934.
Lv, H., Zhang, Q., Chen, W., Song, Z., Zheng, Z., & Zhang, Y. (2020). Epidemiological study of tibial plateau fractures combined with intercondylar eminence fractures. Orthopaedic Surgery, 12(2), 561–569.
e Albuquerque, R. P., Hara, R., Prado, J., Schiavo, L., Giordano, V., & do Amaral, N. P. (2013). Epidemiological study on tibial plateau fractures at a level I trauma center. Acta Ortopédica Brasileira, 21(2), 109–115.
Hua, K., Jiang, X., Zha, Y., Chen, C., Zhang, B., & Mao, Y. (2019). Retrospective analysis of 514 cases of tibial plateau fractures based on morphology and injury mechanism. Journal of Orthopaedic Surgery and Research, 14(1), 267.
Canale, S. T., & Beaty, J. H. (2012). Campbell’s operative orthopaedics e-book. Elsevier Health Sciences.
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D., & Kellam, J. F. (2018). Fracture and dislocation classification compendium—2018. Journal of Orthopaedic Trauma, 32, S1–S10.
Chan, P. S., Klimkiewicz, J. J., Luchetti, W. T., Esterhai, J. L., Kneeland, J. B., Dalinka, M. K., et al. (1997). Impact of CT scan on treatment plan and fracture classification of tibial plateau fractures. Journal of Orthopaedic Trauma, 11(7), 484–489.
Castiglia, M. T., Nogueira-Barbosa, M. H., Messias, A. M. V., Salim, R., Fogagnolo, F., Schatzker, J., et al. (2018). The impact of computed tomography on decision making in tibial plateau fractures. The Journal of Knee Surgery, 31(10), 1007–1014.
Luo, C.-F., Sun, H., Zhang, B., & Zeng, B.-F. (2010). Three-column fixation for complex tibial plateau fractures. Journal of Orthopaedic Trauma, 24(11), 683–692.
Chang, S.-M., Hu, S.-J., Zhang, Y.-Q., Yao, M.-W., Ma, Z., Wang, X., et al. (2014). A surgical protocol for bicondylar four-quadrant tibial plateau fractures. International Orthopaedics, 38(12), 2559–2564.
Krause, M., Preiss, A., Müller, G., Madert, J., Fehske, K., Neumann, M. V., et al. (2016). Intra-articular tibial plateau fracture characteristics according to the “Ten segment classification.” Injury, 47(11), 2551–2557.
Schatzker, J. (2005). Fractures of the Tibial Plateau. In: The Rationale of Operative Fracture Care. Springer, Berlin, Heidelberg. https://doi.org/10.1007/3-540-27708-0_19.
Acknowledgements
This manuscript was prepared by the Singapore Orthopaedic Research CollaborativE (SORCE), c/o Kumaran Rasappan and Ernest Beng Kee Kwek.
Case contributors: Ernest B. K. Kwek (Woodlands Health Campus/Tan Tock Seng Hospital), Ivan T. H. Chua (Tan Tock Seng Hospital), Yong Ren (Farrer Park Hospital/Khoo Teck Puat Hospital), Merng Koon Wong (Sengkang General Hospital/Singapore General Hospital), Kein Boon Poon (Sengkang General Hospital/Changi General Hospital), Andy K.S. Yeo (Changi General Hospital), Yongsheng Chen (Ng Teng Fong General Hospital), Fareed H. Y. Kagda (Ng Teng Fong General Hospital).
Funding
No external funding or grants were received for any aspect of this work. The authors have not sought any writing assistance for the production of the paper.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed equally in the literature review, manuscript writing and review and approved the version submitted for publication. KR is the corresponding author of this study and as such, take responsibility for the integrity of the data in the study and the accuracy of the content provided. KR had full access to all the data in the study and had the final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no financial and personal conflicts of interest in this work.
Ethical Standard Statement
This research complies with the principles laid down in the Declaration of Helsinki and has been approved by our institution’s ethics review committee (National Healthcare Group Domain Specific Review Board—NHG DSRB Ref: 2016/00741). This retrospective study only involved collection of Xrays and CT scan images of patients. Throughout which, all collected data remained anonymous through deidentification.
Informed Consent
According to the national law and our institution’s ethics review board, informed consent from patients for data collected during this study period for a nature of such a study was not required and thus consent was not collected from the patients of this study.
Location Where Work was Performed
The collection of data for this manuscript was done in the respective institutions across Singapore. The compilation and analysis of data as well as the preparation of the first draft of the manuscript was done in Tan Tock Seng Hospital, Singapore (Address: 11 Jln Tan Tock Seng, Singapore 308433).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the “Singapore Orthopaedic Research CollaborativE (SORCE)” are listed in the Acknowledgements section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rasappan, K., Lim, M.J., Chua, I.T.H. et al. Does the Schatzker III Tibial Plateau Fracture Exist?. JOIO 57, 1891–1900 (2023). https://doi.org/10.1007/s43465-023-01001-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-01001-6