Abstract
This review aims to provide a brief introduction to kaempferol with respect to its various therapeutic properties such as anticancer, antioxidant, anti-proliferative, pro-apoptotic, anti-diabetic, anti-inflammatory, and immunomodulatory properties. It also intends to review the various possible nanoformulations that can be designed for the targeted delivery of kaempferol to various tissues. Nanoformulation has been employed to enhance the solubility and bioavailability of poorly soluble and bioavailable phytochemicals like kaempferol. The various nanoformulation methods employed to effectively deliver kaempferol are nanoemulsions, nanomatrixes, nanoparticles, nanostructured lipid carriers, gold nanoparticles, nanocomplexes, and other magnetic nanoparticles. In this review article, it is emphasised that kaempferol has multiple therapeutic properties that target a diverse number of diseases and exhibit a specific mechanism of action for each target. The various nanoformulations of kaempferol were significantly better than the free kaempferol drug delivery system. They were better absorbed into the body, showed better target delivery, and had an improved bioavailability. Nanoformulated kaempferol had a better therapeutic action against certain cancer cell lines and several diseases which it aimed to target. It was realised that kaempferol can be further explored as a potential drug for treatment purposes for several chronic diseases. Therapeutic action against different ailments makes it a versatile phytochemical drug. To further increase its potential to be used in the field of medicine, kaempferol can be nanoformulated in ways such as a nanoemulsion and nanocomplex, among the most important approaches. Thus, the prospects and the possible effective drug delivery for kaempferol are discussed and emphasised here.
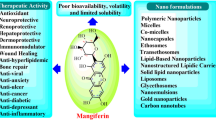
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Herbal drugs have been an integral part of many Asian cultures and are much sought after due to their lesser unwanted side effects (Ghasemian et al. 2016). Newer technologies for studying and establishing various toxicology studies for herbal medicine have been on a rise. Chemicals present in herbs possess a wide range of therapeutic properties that can be further explored and studied, so that they can be effectively used for various disease therapies.
Flavonoids present in plants are known to possess many therapeutic properties which if further studied and researched thoroughly and extensively can help us in developing many lifesaving drugs. Multiple in vitro and in vivo studies have been done to study the effects of flavonoids in treating different types of cancer (Kashyap et al. 2017). One such remarkable polyphenol is kaempferol (3,5,7-trihydroxy-2-(4-hydroxyphenyl)-4H-chromen-4one), a type of flavonol, which is mostly found in foods like broccoli, kale, tea, cabbage, apples, grapes, leeks, and tomatoes (Kashyap et al. 2017).
Kaempferol (1) is biosynthesized by condensing 4-coumaroyl-CoA with tripropionyl-CoA with chalcone synthase as a catalyst (Ren et al. 2019). It exhibits a host of therapeutic activities such as anti-inflammatory, anti-diabetic, anticancer, immunomodulatory, antioxidant, anti-proliferative, and pro-apoptotic activities that have been used to cure various types of cancer of the bladder, breast, lung, colon, pancreas, prostate, cervical, and ovary (Imran et al. 2019). It has been observed to cure systemic sclerosis occurring in skin fibrosis, renal diseases such as diabetic nephropathy, and inflammation due to rheumatoid arthritis and promote osteoblast survival to promote bone formation (Kashyap et al. 2017). Kaempferol undergoes transformation in the small intestine and liver via absorption and metabolism and is converted to sulfosuccinate-conjugated and glucuronides and to 4-methylphenol, phloroglucinol in the large intestine. The process is followed by excretion from all these sites.

Nanotechnology is one of the most studied and explored novel drug development strategies to provide an improved and competent drug delivery system (Gatadi et al. 2021). Nanomedicine has been an efficient way of designing drugs that have poor aqueous solubility. This involves reducing the toxicity of the drug, improving the aqueous solubility and bioavailability, better pharmacological action, possible prevention of degradation, and a wider reach of the drug at the desired site (Gunasekaran et al. 2014).
Most of the potential anticancer drugs are present in the biopharmaceutical classification system class IV; i.e. they have both poor solubility and poor permeability. Thus, it is hard to formulate and administer such drugs to the patients. Formulating such molecules or drugs into a nanoformulation and using certain biodegradable polymers like chitosan have significantly improved their bioavailability and solubility. The main drawback of kaempferol is its poor aqueous solubility leading to poor bioavailability. In order to combat this problem, the present article focuses on the different types of nanoformulations such as nanoemulsion, nanocomplexes, nanostructured lipid carriers, nanomatrix, and gold nanoparticles that have been used to deliver kaempferol to the target sites by enhancing its bioavailability.
Search Strategies
A systematic search in the literature was performed in Pub-Med, PubChem, Science Direct, Google Scholar, Scopus, and Medline academic databases. A search of kaempferol was done using terms such as ‘physicochemical properties’, ‘potential anticancer mechanisms of kaempferol’, ‘therapeutic properties of kaempferol’, ‘treatment of hyperglycemia’, ‘toxicological potential’, ‘bioavailability’, ‘aqueous solubility’, ‘anti-apoptotic effect’, ‘anti-oxidant effect’, ‘nanoformulation’, ‘nanoformulation strategies for kaempferol’, ‘nanoformulation of phytochemicals’, ‘nanoemulsion of kaempferol’, ‘nanomatrix of kaempferol’, ‘kaempferol gold nanoparticles’, and ‘kaempferol magnetic nanoparticles’. Along with this, in this present review, all the studies done with respect to the potential therapeutic properties and nanoformulation strategies of kaempferol will be reviewed.
Discussion
Physicochemical Properties
Kaempferol has a hydrophobic property, due to the presence of its diphenylpropane structure (Ren et al. 2019). This hydrophobic structure limits its solubility in aqueous media. This in turn affects its overall bioavailability in the human body. The compound kaempferol, with a molecular weight of 286.24, is soluble in solvents such as acetic acid, alkalies, ethanol, and acetone. The solubility of kaempferol in water is limited to 440 mg/l at 25 °C. The LogP value that is the partition coefficient of kaempferol is estimated to be 2.0. It is a yellow solid which is crystalline in nature and has a melting point in the range of 276–278 °C As it belongs to the class of flavones, kaempferol has a lipophilic structure, thus limiting its oral bioavailability (PubChem 2022).
Bioavailability and Absorption
Kaempferol, despite its wide range of health benefits like anti-inflammatory, potential anticancer, and antioxidant properties, is lipophilic in nature and is best absorbed through passive and facilitated diffusion as well as active transport. Its oral bioavailability is in the range of nanograms to micrograms per millilitre (Alam et al. 2020). Kaempferol exhibits low aqueous solubility that impairs its chemical stability and biological effects. For this reason, it is formulated using nanocarriers such as lecithin—a vegetable-based phospholipid or chitosan, or into nanoemulsions by size reduction, which improve its aqueous solubility and enhance its stability against free radicals in a controlled manner, thereby increasing its absorption and overall bioavailability (Ilk et al. 2017).
Toxicology
In in vitro studies conducted, it was seen that kaempferol reduces the cellular uptake and bioavailability of folic acid in iron-deficient patients; hence, it is contraindicated with them. It is also said to interfere with the bioavailability of etoposide; hence, it is not administered to cancer patients on etoposide therapy. The toxicological potential of kaempferol has been a topic of conflict among researchers. It was observed that studies proved kaempferol to be anti-mutagenic while some researches proved it to be genotoxic. The mutagenic effect of kaempferol is said to be induced by the CYP 1 A1 enzyme that converts kaempferol to genotoxic guercetin. It has been discovered that kaempferol exhibits antioxidant effects when it reduces the free radicals it donates to a hydrogen atom to form a phenoxyl radical. When a second radical reacts with the phenoxyl radical, it acts as an antioxidant. If this phenoxyl radical reacts with an oxygen species, in that case, kaempferol acts as a pro-oxidant (Alam et al. 2020).
Therapeutic Activities
Kaempferol (1) is responsible for controlling several mechanisms that lead to the proliferation of cancer cells. Kaempferol, an ordinary flavonol, is found to be potentially cytotoxic to cancer cells and regulates tumour progression with different mechanisms (Govindaraju et al. 2019). It regulates the process in cellular signal transduction pathways involved in metastasis, angiogenesis, and apoptosis (Rajendran et al. 2014). The wide range of therapeutic activities of kaempferol is depicted in Fig. 1.
Potential Anticancer Activity
Breast Cancer
The current therapy for breast cancer includes surgery, radiotherapy, and medicines—anti-angiogenesis, anti-oestrogen, aromatase inhibitors, monoclonal antibody drugs, and other drugs. But they exhibit fatal side effects like cardiac failure, pulmonary fibrosis, ototoxicity, hepatotoxicity, fertility issues, and nephrotoxicity. According to animal studies, flavonoids like KMF exhibit a therapeutic effect as a chemotherapy drug for breast cancer. Figure 2 illustrates the various mechanisms of action of kaempferol against the target cells in breast cancer. In triple-negative breast cancer cells MDA-MD-231, kaempferol induced apoptosis, DNA damage, and complete destruction of tumour cells by causing the arrest of the G1 phase. Kaempferol leads to the cleavage of caspase-3 and caspase-9 (Gonçalves et al. 2018). As caspase 3 regulates the growth of tumour surviving cells, its deficiency causes the cells that were resistant to therapeutic antineoplastic agents to no longer be able to repopulate (Huang et al. 2011). In MCF 7 breast cancer cells, the Crabtree effect states that high levels of glucose accelerate their cell proliferation (Zhu and Xue 2019); upon treatment with kaempferol, the glucose uptake of MCF breast cancer cells is effectively inhibited, causing a decline in cell proliferation and viability. Thus, kaempferol was found to be the most potent inhibitor of 3-HDG uptake. It revealed cytotoxic and anti-proliferative properties that were mimicked by low glucose concentrations. It also induced an increase in extracellular lactate levels due to the inhibition of MCT-1-mediated lactate cellular uptake, resulting in cell death (Azevedo et al. 2015).
Oestrogen-positive receptors play a vital role in the proliferation of breast cancer. Kaempferol led to a dose- and time-dependent decrease in the expression of the progesterone receptor and prevented the oestradiol-induced cell proliferation in MCF-7 cells. It was effective on ER both positive and negative receptors (Hung 2004).
The expression of PARP (poly ADP ribose polymerase), a cutting substrate of caspase, plays an important role in the repair of damaged DNA. Its cleavage leads to cellular disassembly. Kaempferol induced this cleavage upon treatment for 24 h, thereby proving its anti-proliferative activity on MCF 7 cells in a dose-dependent manner.
Kaempferol caused the downregulation of anti-apoptotic protein Bcl2 and caused the induction of pro-apoptotic protein BaX, which are involved in DNA repair (Yi et al. 2016).
Epithelial mesenchymal transition is considered to play a vital role in the development of breast cancer, which can resist chemotherapy, leading to failure of the treatment. Triclosan, when administered along with kaempferol, leads to restoration in the morphology from mesenchymal to epithelial type and significant reduction in the migration and invasion of MCF-7 cells. It suppressed the triclosan-induced expression of EMT and metastasis-promoting markers (Lee et al. 2017). Kaempferol also repressed the endogenous oestrogen and triclosan–induced proliferation of MCF-7 cells (Wang et al. 2019).
Rho-A and Rho-C and their signalling pathways play a vital role in the migration and division of MCF 7 cells. Rho-C is involved in increased tumour motility and metastasis. Kaempferol in reduced concentration inhibits the migration and invasion of MCF-7 cells via blocking these pathways (Guan et al. 2020).
Elevated levels of matrix-metalloproteinase (MMPs) are found to contribute to tumour progression. MMP-3 plays a pivotal role in the degradation and remodelling of ECM, tumour cell invasion, and metastasis. Kaempferol inhibits the caseinolytic activity of MMP3 and breast cancer invasion (Phromnoi et al. 2009).
The nuclear factor erythroid derived 2 (NRF-2) pathway is involved in the transformation of oncogenes. It regulates the antioxidant enzymes like NADPH and phase II detoxifying enzymes. Kaempferol is a potent NRF2 inducer that upregulated its expression and inhibited the NRF-2-dependent carcinogenesis transformation (Yang et al. 2017).
Lung Cancer
Non-small cell lung cancer exhibits a poor prognosis, making it a leading cause of cancer-related death each year. The metastasis of the lung cancer cells contributes to the aggressiveness of NSCLC. Thus, identification of the factors leading to lung metastasis and studying the underlying molecular mechanisms is the key approach for lung cancer therapy.
TGF-β1 induces metastasis by promoting EMT in the later stages of cancer. The molecular mechanism of TGF-β1–induced EMT signifies the crucial role of the Smad 3 signalling pathway. The inhibition or depletion of Smad 3 terminates TGF-β1 induction of EMT. Smad 3 is a transcriptional activator of E-cadherin repressors and a key mediator of the TGF-β signalling pathway. KC was observed to completely abolish TGF-beta 1–mediated repression of E-cadherin in a dose-dependent manner. The TGF-β1–induced EMT marker expression was also significantly reduced.
Transforming growth factor-β1 (TGF β1) induces metastasis of A-549 cells by promoting EMT in the later stages of cancer. Inhibition of SMAD3, a key mediator of the TGF-β1 pathway, leads to the termination of TGF-β1–induced EMT. Treatment with kaempferol ceased the TGF-β1–mediated repression of E-cadherin in a dose-dependent manner; it also reduced the TGF-β1–induced EMT marker expression significantly.
The binding of oestrogen to the oestrogen receptors located on the A549 cells leads to the progression of lung cancer. ERRα enhances migration and invasion of A-549 cells by inducing EMT. Kaempferol antagonises ERR-α and ERR-γ activity, leading to the inhibition of EMT-induced migration of A549 lung cancer cells (Huang et al. 2011).
FGF-1 is an inducer of FGFR1 phosphorylation in A459 cells that activated MM26 that increased cancer invasiveness. Kaempferol is said to inhibit the FGFR pathway, leading to the cessation of FGF1-stimulated MMP26 activation, thereby inhibiting the metastasis of A459 cells caused by MMP26 activation (Hu et al. 2014).
TBF-β1 increases the MMP2 secretion and MMP2 gene promoter activities. This upregulation of MMP2 leads to the destruction of the ECM and basement membrane, thereby promoting the invasion of A549 cells. Kaempferol inhibited the activities of TBF- β1, causing an EMT accompanied by invasion of A-549 lung cancer cells.
The PI3K pathway causes transformation of A459 cells from epithelial to mesenchymal type. Kaempferol caused the inhibition of oncogene transformation of A459 cells from epithelial to mesenchymal type through the suppression of the phosphatidylinositol 3-kinase (PI3K) activity. Activator protein 1 that led to the enhancement of the PI3K pathway was also suppressed by kaempferol (Lee et al. 2010).
The phosphates and tensin homologues chromosome (PTEN) is a tumour-suppressing gene that is frequently deleted or mutated in lung cancer. Kaempferol causes the upregulation of PTEN, the tumour-suppressing gene, leading to the inhibition of AKT activation, thereby suppressing migration and invasion of A549 cells.
These results provide for an innovative regulatory mechanism for kaempferol (1) to inhibit the metastasis of lung cancer, thereby accelerating its application as an antineoplastic drug and an anti-tumour agent (Jo et al. 2015).
Colon Cancer
Colon cancer is mainly related to a sedentary lifestyle including an unhealthy diet, too little exercise, use of contraceptives, alcohol, smoking, and harmful environmental factors that contribute to the increased body mass index (Tarasiuk et al. 2018). It develops as a result of uncontrolled cell growth within the large intestine, caecum, rectum, and colon. Tumour necrosis factor–related apoptosis–inducing ligand (TRAIL) is a protein that functions as a ligand and interacts with specific pro-apoptotic receptors such as the death receptor 5 (DR5 or called TRAIL-R2) and DR4 (also called TRAIL-R1). This interaction between TRAIL and DR5 leads to the formation of a complex that activates caspase-8 and caspase-3. This activation results in the destruction of many substrates resulting in the apoptosis of the SW480 colon cells. It was observed that KMF sensitises the colon cells SW480 to the TRAIL-induced apoptosis due to induction of DR5 (Yoshida et al. 2008). A graphical description of this process of inhibition is depicted in Fig. 3.
Cervical Cancer
In the present scenario, human cervical cancer imposes a huge threat to women’s health and is responsible for over 300,000 deaths worldwide (Cohen et al. 2019). Defects in the apoptotic pathways are a major reason for disease pathogenesis and resistance to medicines. Thus, a potential pro-apoptotic and ageing agent can be used for its treatment. In HeLa cervical cancer cells, kaempferol (1) effectively caused the apoptosis of HeLa cells by the upregulation of pro-apoptotic genes, namely p53, p21, BaX, caspase3, and caspase 9 (Alonso-Castro et al. 2013). It also caused the downregulation of the survival genes, specifically Bcl-2, AKT, and PI3K. It also reduces the expression of the telomerase gene and induces cellular ageing. This cytotoxic effect was more pronounced against the neoplastic HeLa cervical cancer cell lines than in the normal human fibroblast cells, thus proving it as a safe chemotherapeutic agent (Kashafi et al. 2017). The anti-proliferative action on SiHa cell lines would increase with an increase in the administration of kaempferol in a concentration-dependent manner. The mitochondrial membrane is responsible for the energy supply, cell signalling, cell death, and differentiation. Thus, it contributes to the proliferation of normal as well as cancer cells. Disruption of this membrane would lead to apoptosis of SiHa cells (Tu et al. 2016).
Pancreatic Cancer
Over 80% of cases are diagnosed in humans between 60 and 80 years of age (Ghadirian et al. 2003). The epidermal growth factor receptor (EGFR) is a transmembrane tyrosine kinase type of receptor that is activated in many epithelial tumours that is responsible for pancreatic tumour progression (Mendelsohn and Baselga 2006). The main goal of the study conducted by Lee et al. (2017) was to determine the mechanism of kaempferol on pancreatic cells. It was observed that this flavonol inhibited the proliferation of pancreatic cells and induced apoptosis (Zhang et al. 2008). It also acts by decreasing the phosphorylation of the EGFR pathway, thereby inhibiting the aggressive growth and migratory activity of these cells (Lee and Kim 2016).
Liver Cancer
The liver is one of the most prone organs to metastasis of cancer cells and accounts for the fifth most common malignancy in the world and is more common in men. The major tumour causatives include hepatitis B and C virus, alcohol consumption, and viral infection. Smoking and exposure to aflatoxin, a mycotoxin that contaminates peanuts, is said to cause mutation in the tumour-suppressor gene p53. The risk of hepatocellular carcinoma increases with diabetes and obesity that are linked with insulin resistance (Kulanthaivel et al. 2012). Aflatoxins, a type of mycotoxin, is derived from the secondary metabolism of the fungi belonging to the genus Aspergillus. AFB1 is a mycotoxin found commonly in grains and cereals and is said to be involved in the development of hepatocellular carcinoma (Ferreira et al. 2019). The administration of kaempferol reduces the extent of peroxidation. It decreases the activity of phase II biotransformation enzymes and increases the activity of phase I enzymes. It was also shown to increases the levels of enzymic and non-enzymic antioxidants thereby inhibiting lipid peroxidation. Thus, kaempferol reduced the formation of free radicals and their scavenging activity, due to its antioxidant property.
Prostate Cancer
A diagnosis of prostate cancer is done by analysing the serum prostate-specific antigen, digital rectal examination, magnetic resonance imaging, and biopsy. The rate of survival is as high as 90% for a well-differentiated localised prostate cancer (Lavery et al. 2016). Prostate cancer cells exhibit slow growth and have a low rate of mutation, which makes them a potential candidate for immunotherapy. Granulocyte-macrophage colony-stimulating factor (GM-CSF) is an immunomodulator protein produced by prostate cancer 3 (PC-3) cells. Kaempferol acts by increasing the production of GM-CSF in a concentration-dependent manner, without affecting the mRNA levels. It modulated the chemotaxis of dendritic cells, responsible for the tumouricidal action depicted in Fig. 4. It also led to an increase in the extracellular and intracellular calcium ion levels.
Ovarian Cancer
Ovarian tumours are a heterogeneous group of neoplasms, divided into various subgroups, based on their cytological and histological characteristics (Mahalaxmi and Santhy 2017). Cisplatin, being the most commonly used therapeutic agent for the treatment of ovarian cancer, comes with a major drawback, that of the risk of the development of resistance to cisplatin being too high. By increasing the dosage, one can overcome the resistance, but it will lead to toxicity in the non-tumorigenic cells. Thus, the cells were first treated with cisplatin, and further were subjected to KMF.
Kaempferol (1) synergises the anticancer effect of cisplatin on ovarian cancer cells, by upregulating the pro-apoptotic gene CDKN1A and downregulating the pro-oncogene cMyc mRNA, thus suppressing the proliferation of cancer cells. It also inhibits the ABCC6 gene that was responsible for reducing the intracellular cisplatin levels (Luo et al. 2010). Kaempferol decreases the levels of Bcl-xl protein, a pro-oncogene, in ovarian cancer cells, while the pro-apoptotic genes BaX, BaD, and p53 were upregulated. Thus, kaempferol activates the intrinsic apoptotic pathway and causes the death of the ovarian cancer cells (Luo et al. 2011).
Vascular endothelial growth factor (VEGF) is an important positive factor that regulates angiogenesis. Found in ovarian tumours, its gene expression is modulated by growth factors, oncogenes, hypoxia, and hormones. Luo et al. (2009) studied the effect of kaempferol on angiogenesis and VEGF gene expression regulated by the HIF-1, proliferator activated receptor gamma coactivator 1 α (PPARGC1A), and oestrogen related receptor α (ESRRA) pathways on ovarian cancer cells. No significant change was seen in levels of PPARGC1A mRNA. But the ESSRA mRNA levels were inhibited to 62% in the OVCAR cell lines in a concentration-dependent manner (Luo et al. 2009). Therefore, the angiogenesis due to VEGF positive regulation in ovarian cancer cells OVCAR was inhibited by KMF.
Bladder Cancer
Bladder cancer is associated with classic symptoms of painless haematuria occurring in most patients, with the rest experiencing microhaematuria. It is 3–4 times more frequent in men than in women, mainly due to the higher exposure of men towards tobacco smoking and aromatic amines (Pelucchi and Negri 2017).
The anti-proliferative activity of kaempferol on the bladder cancer EJ cell line was studied by Feng Xie et al. (2013). The phosphates and tensin homologue (PTEN) on the 10th chromosome is supposed to be a potent tumour-suppressor gene required for the regulation of the PI3/Akt pathway (PI3K, phosphatidylinositol 3-kinase, and Akt protein kinase B). It acts by hydrolysing the 3-phosphate group of PIP3 (phosphatidylinositol (3,4,5)-trisphosphate), thereby converting it to its active form PIP2, causing inhibition of its anti-proliferative effects. Deletion or mutation of PTEN causes activation of the Akt pathway, which leads to regulation of survival and growth responses of tumour cells (Sfakianos et al. 2014). A loss in the functionality of the PTEN gene was noticed in EJ cells of the bladder which was responsible for the development of resistance to the therapy. PTEN is involved in the proliferation and apoptosis of EJ cells through the dephosphorylation of PIP3 (phosphatidylinositol (3,4,5)-triphosphate) and inhibition of the Akt protein kinase B signalling pathway. EJ cancer cells were treated with different doses of kaempferol, and the result showed that KMF increases the PTEN expression and stimulates the apoptosis in these cells, and also inhibits Akt phosphorylation leading to a decrease in the cancer cell proliferation (Xie et al. 2013).
Anti-diabetic Effect
Diabetic nephropathy is a microvascular complication in patients suffering from diabetes and accounts for 30–47% of the end-stage kidney disorders (Sharma et al. 2017). One of the key indicators of diabetic nephropathy is hyperglycaemia. Most drugs used for lowering blood glucose levels have turned out to be highly toxic, thus limiting its use. The rhomboide protease (Rho) GTPase family of proteins is composed of monomeric G-proteins that take part in regulating the various cellular functions; their hydrolytic activity is affected by the Rho regulators. High levels of glucose were found to activate Rho-A in the renal mesangial and tubular epithelial cells of patients with diabetes. This study was conducted on rats by Lee et al. (2010) with the aim of investigating what effect kaempferol displays on the renal tubular epithelial cells under hyperglycaemic conditions. Upon treatment with kaempferol in a concentration-dependent manner, the observations are summarised in Fig. 5 (Sharma et al. 2019). Thus, in conclusion, the probable mechanism of action of kaempferol (1) to slow down the diabetes progression and the complications related to it was that it worked as a Rho-A inhibitor and it acts by inhibiting the activation of Rho kinase.
Skin Fibrosis
Skin fibrosis is the accumulation of extracellular matrix in the dermis that results in dysfunction and altered architecture of the dermis (Do and Eming 2016). Epithelial cells are said to be majorly involved in the development of skin fibrosis. A study conducted to examine the effect of kaempferol (1) on skin fibrosis in the bleomycin-induced fibrosis mice model was performed in vivo. The mice model was divided into two groups; one was treated with KMF and the other was the control. The cells treated with bleomycin had increased ROS production due to oxidative stress, leading to several damages such as enhanced platelet activation and upregulation of adhesion molecules or secretion of inflammatory cytokines (Sekiguchi et al. 2019). Kaempferol suppresses the progression of skin fibrosis and the infiltration of inflammatory cells in the bleomycin-treated mice model, thereby showing anti-inflammatory activity. It also exerts its antioxidant effect by suppressing ROS production. In addition, it exerts an anti-apoptotic effect by reducing the activity of caspase 3.
Bone Loss
It is a condition where the new formation of the bone does not keep up with the old bone removal. It is a consequence of rheumatoid arthritis. It occurs locally as well as systemically, affecting the inflamed joints, leading to osteopenia and overt osteoporosis. There is an increased risk of fractures, especially in geriatrics (Orsolini et al. 2019). One of the causes of bone loss was found to be elevated levels of endogenous glucocorticoids and stress conditions. Decreased bone mass and its mineral density with an increase in risk of fractures involve excess glucocorticoids (GCs). The excess GC production leads to osteoporosis (Yang et al. 2020). A study was conducted on rats with the aim of examining the effect of kaempferol on bone loss and osteoblast survival. By studying the changes in the bone and tissue volume, strengthening of the trabecular network, and increased survival of osteoblast, kaempferol proves to be a potential agent to treat osteoporosis (Adhikary et al. 2018).
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic and systemic autoimmune response towards various joints with an unknown cause, progressive disability, systemic complications, and early death. But due to advanced knowledge, pathogenesis has helped to develop various drugs for its treatment (Alam et al. 2017). The p38 mitogen activated protein kinase (MAPK) pathway contributes to the process of induction of chronic inflammation in rheumatoid arthritis. The disease is mainly characterised by the involvement of various macrophages and fibroblast-like synoviocytes, causing the inflammation of the synovial membrane (Liu et al. 2017). Kaempferol is said to improve the condition of various autoimmune diseases (Rajendran et al. 2014). Kaempferol was administrated in TNF-activated MAPK-induced fibroblast-like synoviocytes, incubated for a day, and stimulated with TNF again in order to enhance the activation of the MAPK pathway. Kaempferol significantly suppressed the TNF-activated MAPK pathway, which reduced the migration of synoviocytes (Pan et al. 2018). Thereby, these results suggest the anti-invasive and anti-migratory effect of kaempferol on fibroblast-like synoviocytes.
Nanoformulation Strategies
Nanoformulated particles in general have various properties like the ability to cross tissue barriers, healing wounds, and killing toxic cells (Gatadi et al. 2021). Even after possessing a wide range of therapeutic properties, kaempferol (1) has low water solubility and bioavailability which prevented its use in cancer therapy. The chances of giving less activity in vivo are more for some plant metabolites, such as kaempferol, that have low solubility. Thus, the concept of nanoformulation originated, where permeability and solubility of hydrophobic compounds can be enhanced. To make the most out of the naturally derived flavonol kaempferol in targeting specific cancer cells and to show their full therapeutic potential, kaempferol can be administered by using nanotechnology, as illustrated in Fig. 6. Various nanoformulations for kaempferol can be used in targeting cancer cells like glioma cells, ovarian cells, and human prostate cancer cells, or for efficient ocular drug delivery or even for better oral drug delivery for treating diseases like diabetes, cancer, and various neurodegenerative diseases. Nanoformulation is the latest and most advanced technique of kaempferol administration for therapeutic purposes and better patient compliance.
Approaches
Nanoemulsion
The need for the preparation of kaempferol-loaded nanoemulsions arises to provide a better administration strategy like that of the intranasal route (Colombo et al. 2018). This route can be effectively used to administer the drug to the brain. Phytochemicals like kaempferol have poor aqueous solubility and thus have poor bioavailability and absorption which acts as a disadvantage in delivering drugs to the brain as they find it difficult to cross the blood-brain barrier. Nanoemulsions due to their small size can deliver the drug like kaempferol via the intranasal route to the brain efficiently (Bonferoni et al. 2019). This nanoemulsion of kaempferol can increase the absorption and thus increase the bioavailability of the drug in the targeted region. This system even has the potential to prevent any sort of chemical degradation of the drug. One of the studied nanoemulsion systems is a mucoadhesive nanoemulsion of kaempferol specifically designed to target the glioma cell lines in the brain of a rat. This study used high-pressure homogenisation to prepare the nanoemulsions, such as pressure valve homogenizers, ultra-sonicators, and micro-fluidisers that use a high force or pressure to suspend the dispersed particles (Aswathanarayan and Vittal 2019). A high-energy method was used to get the mucoadhesive property chitosan as it is known to have a bio-adhesive nature and increases permeability in the nasal region. The tests were conducted by comparing kaempferol nanoemulsion, free kaempferol, and kaempferol-loaded mucoadhesive nanoemulsions. This particular formulation helps to enhance the apoptosis of glioma cell lines thus acting as a potential treatment strategy for cancer via the nose route to the brain (Colombo et al. 2018).
Nanoparticles
They are classified as liposomes, albumin bound, dendrimers, polymeric, iron oxide, quantum dots, and gold (metals) (Wang and Wang 2014; Radjabian and Abetz 2020). These nanoparticles help in size controlling, site-targeted therapy, and better drug loading and release. Polyethylene glycol (PEG)–coated polymeric nanoparticles are the ones commonly used (Mohanraj and Chen 2007). A study was conducted on ovarian cancer cell viability to test the potency and effectiveness of kaempferol nanoparticles. Polyethylene-oxide-polypropylene-oxide-polyethylene oxide (PEO-PPO-PEO), poly-DL-lactic acid co-glycolic acid (PLGA), PLGA-polyethyleneimine (PEI), chitosan, and poly-amidoamine dendrimer (PAMAM) nanoparticles were studied by incorporating kaempferol via the nanoprecipitation method. The PEO-PPO-PEO kaempferol particles showed a better and great inhibitory effect on the ovarian cancer cell line (A2780/CP70) than others. On another ovarian cancer cell line (OVCAR-3), yet again, the PEO-PPO-PEO KMF nanoparticles showed better cell viability. Even folate-targeted kaempferol can be incorporated into the PEO-PPO-PEO nanoparticles to target only the overexpressing cancer cell lines. Apart from kaempferol PEO-PPO-PEO and PLGA, nanoparticles showed a better inhibitory response on all the abovementioned cancer cell lines (Luo et al. 2012).
Kaempferol-loaded lecithin/chitosan nanoparticles were prepared to test their antifungal action. This nanoformulation was prepared by the interaction between kaempferol, lecithin, and chitosan. The tests showed that kaempferol-lecithin-chitosan nanoparticles showed better antioxidant activity compared to free kaempferol due to reasons like better solubility of the drug. The antifungal action of the kaempferol-loaded lecithin/chitosan nanoparticle system was tested and found to be better than free kaempferol as it interferes with the cell wall, synthesis of DNA and RNA, and hyphal extension of Fusarium oxysporium. This strong inhibition was possible due to their greater surface area and their size (Ilk et al. 2017). Thus, these nanoparticles have a good potential for ovarian cancer cell–targeted therapy and for possible antifungal action.
Nanocomplexes
Nanocomplexes have proven to have a great potential in targeting brain tumours by incorporating doxorubicin and 5-fluorouracil to have a controlled release (Di Martino et al. 2017). Ocular surface inflammation and oxidative stresses are known to be the major symptoms of most eye diseases. Compared to conventional eye drops, the nanoformulation of ophthalmic agents has been known to have better penetration capacity, better solubility, and better residing time in the cornea. In a recently conducted study, a nanocomplex of polyvinylpyrrolidone (PVP) 17PF-kaempferol was prepared by a simple thin-film hydration method. There are two grades of approved PVP available, 12PF and 17PF, and amongst these, 17PF showed better complexing capacity. PVP has a good property of solubilising poorly soluble phytochemicals as well as forming hydrogen-hydrogen bonds with them which in turn makes the preparation more stable. The 17PF-kaempferol nanocomplex ocular solution was found to have better corneal permeability, antioxidant action, and good complexing efficacy. This was due to its ultra-nano-size (8.628 ± 0.066 nm). All the safety aspects of the drug were verified, and it showed 17PF-kaempferol to have a good eye tolerance and also showed cell cytotoxicity. This nanocomplex solution showed 3600 times improved water solubility for kaempferol. The end result of healed alkali burns on the cornea showed better and enhanced anti-inflammatory and antioxidant power with the administration of this kaempferol nanoformulation (Zhang et al. 2020).
Nanostructured Lipid Carriers
The nanostructured lipid carriers (NLCs) help in enhancing the aqueous solubility and permeation of the drug in the body. According to Subramaniam et al. (2020), optimisation of NLC is the main factor that determines the nature of the drug. As NLC has liquid lipids, the drug solubility is enhanced by increased entrapping; also, they have good oral bioavailability. They are also capable of handling both hydrophilic and hydrophobic drugs as well as have the capacity to release drugs in a sustained manner (Poonia et al. 2016). In a previously conducted experiment, oral delivery of kaempferol was checked via NLC of N-trimethyl chitosan (TMC, surface-modified). The only drawback of using chitosan was its instability in basic pH, i.e., exceeding the range of 5.5–6.5. Therefore, TMC was used in this experiment as it is highly water soluble and has better stability in a neutral environment. Decyclic acid and palmitic acid were grafted onto the kaempferol-loaded N-trimethyl chitosan chloride NLC. Kaempferol was emulsified and went under ultra-sonication to form the loaded NLC. In the next step, chitosan went under amination to form TMC which then was condensed with the two aliphatic acids and grafted onto the kaempferol-loaded NLC. It was concluded that there was an accelerated release of drugs from the DA-TMC-KNLC. PA-TMC-KNLC showed sustained-release action. In Caco-2 cells, these nanoparticles showed increased and better cell drug delivery (Du et al. 2019).
Gold Nanoparticles
Metals have often shown efficient properties in multiple biomedical studies (Pissuwan 2017; Srinivas Raghavan et al. 2015). Gold nanoparticles have proven to be useful in treating various cancer models (Manju and Sreenivasan 2010). Gold nanoparticles in their colloidal form have been prepared to target tumour necrosis factor (TNF) in mice (Chandran and Thomas 2015). In this study, gold nanoparticles were synthesised with loaded kaempferol to study their potential anticancer effect on the MCF-7 cancer cell line by their antioxidant action. The kaempferol used was derived from a Lotus species, Fabaceae, and a suitable colloid form was made with AuNP using HAuCl4. Size and shape were tuned and modified accordingly, and wine-red colloidal AuNP with kaempferol was formed. pH was the main basis of the colloidal stability of AuNPs with kaempferol glucoside. AuNP showed the maximum free radical scavenging activity while in higher concentrations showing mild cytotoxicity in MCF-7 cell lines. This even proved the efficacy of these nanoparticles in destroying cancer cell lines and behaving as a potential anticancer agent (Oueslati et al. 2020). Another similar study indicated a higher toxicity in breast cancer cell lines by K-AuNP at lower concentrations, showing its capability as an anti-breast cancer agent also acting as an antiangiogenic agent by inhibiting VEGF-induced angiogenesis (Kondath et al. 2014).
Nanomatrix
Entrapping phytochemicals in nanomatrix has been previously studied for curcumin-loaded zinc oxide (Perera et al. 2020). Layer-by-layer (LbL) polyelectrolyte nanomatrix type of encapsulation was designed to load kaempferol in an inorganic CaCO3 template (Kumar et al. 2012). Previously, studies showed the effectiveness of kaempferol as an anti-osteoclastogenic agent (Trivedi et al. 2008). This effect is thought to be due to its antioxidant properties (Imran et al. 2019). In this experiment, the differentiating factor is this unique delivery of kaempferol along with calcium from CaCO3 (core particle) which is a calcium supplement. CaCO3 was prepared by colloidal crystallisation, and later, its dried form was incubated with kaempferol. Later, they were centrifuged and then the LbL assembly was prepared. After various tests and analytical studies, it was found that the plasma bioavailability of kaempferol with this nanomatrix formulation was quite high. Also, this nanomatrix had higher mineralised nodule formation in OVx rats. In OCN and Col1 (osteogenic genes), the miRNA levels were significantly high after being treated with the kaempferol-loaded CaCO3 nanomatrix. This study even showed that this nanomatrix inhibited the bone turnover rate. Micro-architecture was restored by this nanomatrix and also was sustained in a better way (Kumar et al. 2012).
Other Magnetic Nanoformulations
Graphene quantum dots (GQDs) were used in experiments to visualise kaempferol content. In another experiment, by using the mini-emulsion polymerisation method, magnetic fluorescent microspheres (MFMs) were prepared which included Fe3O4, KMF, and ferrofluids. This model of nanoformulation is also called a bifunctional drug delivery system as it allows both real-time visualisation of kaempferol (drug) release and external manipulation with a magnetic field by an imaging technique. The results for the experiment were as follows: Thermogravimetric analysis showed that they had a strong magnetic sensitivity in the presence of an outer magnetic field due to higher magnetite content. According to UV analysis, kaempferol release was sustained and slow from the MFMs at various pH levels. On conducting a cytotoxicity assay, it was seen that as the concentration of kaempferol increased, the number of viable Hela cells diminished. Hence, it was shown that these magnetic nanostructures have a great anticancer potential for Hela cell lines (Zhang et al. 2017).
A dual drug delivery system for kaempferol along with paclitaxel was prepared using magnetic fluorescent nanocomposites. Fe3O4 ferrofluids were prepared by the chemical co-precipitation technique, and a magnetic microsphere was prepared in a mixture of ferrofluids and BSA later collected with magnets. Kaempferol was loaded into this microsphere. Then GQDs with paclitaxel (PTX) were prepared as a suspension, and the loaded GQD was made. The magnetic microsphere with kaempferol was added to the GQD-paclitaxel solution and ultrasonically dispersed, and after some time, it was collected using magnets, washed, and dried. The results of the analysis showed that kaempferol was successfully loaded onto the microsphere and also showed the presence of paclitaxel loading onto the GQDs. MFMs were proven to have good dispersibility and a spherical structure. This nanocomposite showed a slow sustained-release effect of the drug and could even inhibit the growth of Hela cells (Zhang et al. 2018).
Perspectives and Future Directions
Plants, being easily available, inexpensive, and high in flavonoid content, have been used in herbal and conventional therapy to treat diseases and health conditions. Studies conducted by the researches report that kaempferol in a dose-dependent manner has led to the inhibition of the proliferation and metastasis of cancer cells of the lung, prostate, cervix, bladder, liver, pancreas, ovaries, breast, and the colon, as well as exhibits an anti-diabetic effect in hyperglycemic patients. Thus, the administration of kaempferol and the discovery of new nanoformulations to further increase its bioavailability and aqueous solubility, than the already-existing nanocarriers, is a potential field of research. With an increase in the awareness of environmentally sound and consumer-friendly extraction processes, based on green chemistry, the need for newer methods of extraction of kaempferol is in focus.
Kaempferol, in various nanostructures such as nanomatrix, nanoemulsion, and gold nanoparticle, has shown its capacity as a nanoformulated drug, to effectively target disease sites, with enhanced solubility and increased bioavailability. But high costs associated with nanotechnology and developing this drug as a nanomedicine on an industrial scale, and lack of continuous persistent research on this compound, can be seen as a hurdle. Thus, with the help of the pre-existing research on nanoformulation strategies for kaempferol, the upcoming, newer and advanced nanoformulation techniques can have a well-established base to potentially introduce this drug into the market. Further research on the toxicology studies, and nanoformulation of kaempferol, can potentially bring this drug at a larger scale, from bench to bed, for manufacturing it and bringing forth it as a therapeutic drug to the patients.
Conclusion
The benefits of using herbal drugs and components derived from medicinal plants are numerous. Owing to a shift in lifestyle across the globe, people are preferring naturally derived organic food and medicines. Several flavonoids derived from dietary sources such as tomatoes, grapes, apples, and broccoli, among others, have exhibited their efficacy in combating multiple health issues. The dietary flavonoid kaempferol is abundantly found in a variety of vegetables and fruits. A large number of preclinical studies have confirmed the role of kaempferol in the prevention and treatment of a broad range of cancers such as breast, lung, cervical, ovarian, prostate, pancreatic, liver, colon, and bladder cancer, due to its anti-proliferative, pro-apoptotic, and anti-migratory activities that lead to the inhibition of mechanisms and cycles leading to the growth of the cancerous cells. It can also be used as a potent anti-diabetic, in the treatment of skin fibrosis, and in promoting osteoblast survival, exhibiting its anti-inflammatory, antioxidant, and immunomodulatory activities. In order to improve the aqueous solubility and bioavailability of kaempferol, designing an appropriate nano-drug delivery system promoting high patient compliance is crucial. Out of the above-discussed nanoformulations, nanoemulsions, NLC, graphene quantum dots, and metal-based nanoparticles, such as the gold nanoparticle, can be seen as the ones having the most potential. The toxicological studies must be further conducted with respect to kaempferol to establish its safety completely. Further research can definitely push this phytochemical into commercial use for the treatment of various diseases. The different experiments mentioned in this article provide a great insight on the various activities of kaempferol, on how different nanoformulations can be designed for different target sites and various types of cancer. Hence, nanoformulation and its targeted therapeutic advantages provide a bright future for kaempferol in the area of clinical medicine.
References
Adhikary S, Choudhary D, Ahmad N, Karvande A, Kumar A, Banala VT, Mishra PR, Trivedi R (2018) Dietary flavonoid kaempferol inhibits glucocorticoid-induced bone loss by promoting osteoblast survival. Nutrition 53:64–76. https://doi.org/10.1016/j.nut.2017.12.003
Alam J, Jantan I, Bukhari SNA (2017) Rheumatoid arthritis: recent advances on its etiology, role of cytokines and pharmacotherapy. Biomed Pharmacother 92:615–633. https://doi.org/10.1016/j.biopha.2017.05.055
Alam W, Khan H, Shah MA, Cauli O, Saso L (2020) Kaempferol as a dietary anti-inflammatory agent: current therapeutic standing. Molecules 25:4073. https://doi.org/10.3390/molecules25184073
Alonso-Castro AJ, Ortiz-Sánchez E, García-Regalado A, Ruiz G, Núñez-Martínez JM, González-Sánchez I, Quintanar-Jurado V, Morales-Sánchez E, Dominguez F, López-Toledo G, Cerbón MA, García-Carrancá A (2013) Kaempferitrin induces apoptosis via intrinsic pathway in HeLa cells and exerts antitumor effects. J Ethnopharmacol 145:476–489. https://doi.org/10.1016/j.jep.2012.11.016
Aswathanarayan JB, Vittal RR (2019) Nanoemulsions and their potential applications in food industry. Front Sustain Food Syst 3:95. https://doi.org/10.3389/fsufs.2019.00095
Azevedo C, Correia-Branco A, Araújo JR, Guimarães JT, Keating E, Martel F (2015) The chemopreventive effect of the dietary compound kaempferol on the MCF-7 human breast cancer cell line is dependent on inhibition of glucose cellular uptake. Nutr Cancer 67:504–513. https://doi.org/10.1080/01635581.2015.1002625
Bonferoni MC, Rossi S, Sandri G, Ferrari F, Gavini E, Rassu G, Giunchedi P (2019) Nanoemulsions for “nose-to-brain” drug delivery. Pharmaceutics 11:84. https://doi.org/10.3390/pharmaceutics11020084
Chandran PR, Thomas RT (2015) Gold nanoparticles in cancer drug delivery. In: Thomas S, Grohens Y, Ninan N, Nanotechnology applications for tissue engineering. Elsevier Inc., pp. 221-237. doi: https://doi.org/10.1016/B978-0-323-32889-0.00014-5
Cohen PA, Jhingran A, Oaknin A, Denny L (2019) Cervical cancer. Lancet 393:169–182. https://doi.org/10.1016/S0140-6736(18)32470-X
Colombo M, Figueiró F, de Fraga DA, Teixeira HF, Battastini AMO, Koester LS (2018) Kaempferol-loaded mucoadhesive nanoemulsion for intranasal administration reduces glioma growth in vitro. Int J Pharm 543:214–223. https://doi.org/10.1016/j.ijpharm.2018.03.055
Di Martino A, Kucharczyk P, Capakova Z, Humpolicek P, Sedlarik V (2017) Chitosan-based nanocomplexes for simultaneous loading, burst reduction and controlled release of doxorubicin and 5-fluorouracil. Int J Biol Macromol 102:613–624. https://doi.org/10.1016/j.ijbiomac.2017.04.004
Do NN, Eming SA (2016) Skin fibrosis: models and mechanisms. Curr Res Transl Med 64:185–193. https://doi.org/10.1016/j.retram.2016.06.003
Du Q, Chen J, Yan G, Lyu F, Huang J, Ren J, Di L (2019) Comparison of different aliphatic acid grafted N-trimethyl chitosan surface-modified nanostructured lipid carriers for improved oral kaempferol delivery. Int J Pharm 568:118506. https://doi.org/10.1016/j.ijpharm.2019.118506
Ferreira RG, Cardoso MV, de Souza Furtado KM, Espíndola KMM, Amorim RP, Monteiro MC (2019) Epigenetic alterations caused by aflatoxin b1: a public health risk in the induction of hepatocellular carcinoma. Transl Res 204:51–71. https://doi.org/10.1016/j.trsl.2018.09.001
Gatadi S, Madhavi YV, Nanduri S (2021) Nanoparticle drug conjugates treating microbial and viral infections: a review. J Mol Struct 1228:129750. https://doi.org/10.1016/j.molstruc.2020.129750
Ghadirian P, Lynch HT, Krewski D (2003) Epidemiology of pancreatic cancer: an overview. Cancer Detect Prev 27:87–93. https://doi.org/10.1016/S0361-090X(03)00002-3
Ghasemian M, Owlia S, Owlia MB (2016) Review of anti-inflammatory herbal medicines. Adv Pharmacol Sci 2016:9130979. https://doi.org/10.1155/2016/9130979
Gonçalves H, Guerra MR, Duarte Cintra JR, Fayer VA, Brum IV, Teixeira MTB (2018) Survival study of yriple-negative and non–triple-negative breast cancer in a Brazilian cohort. Clin Med Insights Oncol 12:1179554918790563. https://doi.org/10.1177/1179554918790563
Govindaraju S, Roshini A, Lee MH, Yun K (2019) Kaempferol conjugated gold nanoclusters enabled efficient for potential anticancer therapeutics to A549 lung cancer cells. Int J Nanomed 14:5147–5157. https://doi.org/10.2147/IJN.S209773
Guan X, Guan X, Dong C, Jiao Z (2020) Rho GTPases and related signaling complexes in cell migration and invasion. Exp Cell Res 388:111824. https://doi.org/10.1016/j.yexcr.2020.111824
Gunasekaran T, Haile T, Nigusse T, Dhanaraju MD (2014) Nanotechnology : an effective tool for enhancing bioavailability and bioactivity of phytomedicine. Asian Pac J Trop Biomed 4:S1–S7. https://doi.org/10.12980/APJTB.4.2014C980
Hu M, Xiang F-X, He Y-F (2014) Are cancer stem cells the sole source of tumor? J Huazhong Univ Sci Technol [Med Sci] 34:621–625. https://doi.org/10.1007/s11596-014-1327-8
Huang Q, Li F, Liu X, Li W, Shi W, Liu F-F, O’Sullivan B, He Z, Peng Y, Tan A-C, Zhou L, Shen J, Han G, Wang X-J, Thorburn J, Thorburn A, Jimeno A, Raben D, Bedford JS, Li C-Y (2011) Caspase 3-mediated stimulation of tumor cell repopulation during cancer radiotherapy. Nat Med 17:860–866. https://doi.org/10.1038/nm.2385
Hung H (2004) Inhibition of estrogen receptor alpha expression and function in MCF-7 cells by kaempferol. J Cell Physiol 198:197–208. https://doi.org/10.1002/jcp.10398
Ilk S, Saglam N, Özgen M (2017) Kaempferol loaded lecithin/chitosan nanoparticles: preparation, characterization, and their potential applications as a sustainable antifungal agent. Artif Cells Nanomed Biotechnol 45:907–916. https://doi.org/10.1080/21691401.2016.1192040
Imran M, Salehi B, Sharifi-Rad J, Aslam Gondal T, Saeed F, Imran A, Shahbaz M, Tsouh Fokou PV, Umair Arshad M, Khan H, Guerreiro SG (2019) Kaempferol: a key emphasis to its potential anticancer potential. Molecules 24:2277. https://doi.org/10.3390/molecules24122277
Jo E, Park SJ, Choi YS, Jeon W-K, Kim B-C (2015) Kaempferol suppresses transforming growth factor-β1-induced epithelial-to-mesenchymal transition and migration of A549 lung cancer cells by inhibiting Akt1-mediated phosphorylation of Smad3 at threonine-179. Neoplasia 17:525–537. https://doi.org/10.1016/j.neo.2015.06.004
Kashafi E, Moradzadeh M, Mohamadkhani A, Erfanian S (2017) Kaempferol increases apoptosis in human cervical cancer HeLa cells via PI3K/AKT and telomerase pathways. Biomed Pharmacother 89:573–577. https://doi.org/10.1016/j.biopha.2017.02.061
Kashyap D, Sharma A, Tuli HS et al (2017) Kaempferol – a dietary potential anticancer molecule with multiple mechanisms of action: recent trends and advancements. J Funct Foods 30:203–219. https://doi.org/10.1016/j.jff.2017.01.022
Kondath S, Raghavan BS, Anantanarayanan R, Rajaram R (2014) Synthesis and characterisation of morin reduced gold nanoparticles and its cytotoxicity in MCF-7 cells. Chem Biol Interact 224:78–88. https://doi.org/10.1016/j.cbi.2014.09.025
Kulanthaivel L, Srinivasan P, Shanmugam V (2012) Therapeutic efficacy of kaempferol against AFB 1 induced experimental hepatocarcinogenesis with reference to lipid peroxidation, antioxidants and biotransformation enzymes. Biomed Prev Nutr 2:252–259. https://doi.org/10.1016/j.bionut.2012.04.002
Kumar A, Gupta GK, Khedgikar V, Gautam J, Kushwaha P, Changkija B, Nagar GK, Gupta V, Verma A, Dwivedi AK, Chattopadhyay N, Mishra PR, Trivedi R (2012) In vivo efficacy studies of layer-by-layer nano-matrix bearing kaempferol for the conditions of osteoporosis: a study in ovariectomized rat model. Eur J Pharm Biopharm 82:508–517. https://doi.org/10.1016/j.ejpb.2012.08.001
Lavery A, Kirby RS, Chowdhury S (2016) Prostate cancer. Medicine 44:47–51. https://doi.org/10.1016/j.mpmed.2015.10.001
Lee J, Kim JH (2016) Kaempferol inhibits pancreatic cancer cell growth and migration through the blockade of EGFR-related pathway in vitro. PLoS ONE 11:e0155264. https://doi.org/10.1371/journal.pone.0155264
Lee KM, Lee DE, Seo SK, Hwang MK, Heo Y-S, Lee KW, Lee HJ (2010) Phosphatidylinositol 3-kinase, a novel target molecule for the inhibitory effects of kaempferol on neoplastic cell transformation. 31:1338–1343. https://doi.org/10.1093/carcin/bgq102
Lee GA, Choi KC, Hwang KA (2017) Kaempferol, a phytoestrogen, suppressed triclosan-induced epithelial-mesenchymal transition and metastatic-related behaviors of MCF-7 breast cancer cells. Environ Toxicol Pharmacol 49:48–57. https://doi.org/10.1016/j.etap.2016.11.016
Liu Q, Xiao XH, Hu LB, Jie H-Y, Wang Y, Ye W-C, Li M-M, Liu Z (2017) Anhuienoside C ameliorates collagen-induced arthritis through inhibition of MAPK and NF-κB signaling pathways. Front Pharmacol 8:299. https://doi.org/10.3389/fphar.2017.00299
Luo H, Rankin GO, Liu L, Daddysman MK, Jiang B-H, Chen YC (2009) Kaempferol inhibits angiogenesis and VEGF expression through both HIF dependent and independent pathways in human ovarian cancer cells. Nutr Cancer 61:554–563. https://doi.org/10.1080/01635580802666281
Luo H, Daddysman MK, Rankin GO, Jiang B-H, Chen YC (2010) Kaempferol enhances cisplatin’s effect on ovarian cancer cells through promoting apoptosis caused by down regulation of cMyc. Cancer Cell Int 10:16. https://doi.org/10.1186/1475-2867-10-16
Luo H, Rankin GO, Li Z, DePriest L, Chen YC (2011) Kaempferol induces apoptosis in ovarian cancer cells through activating p53 in the intrinsic pathway. Food Chem 128:513–519. https://doi.org/10.1016/j.foodchem.2011.03.073
Luo H, Jiang B, Li B, Li Z, Jiang B-H, Chen YC (2012) Kaempferol nanoparticles achieve strong and selective inhibition of ovarian cancer cell viability. Int J Nanomed 7:3951–3959. https://doi.org/10.2147/IJN.S33670
Mahalaxmi I, Santhy KS (2017) An overview about mitochondrial DNA mutations in ovarian cancer. Alexandria J Med 53:307–310. https://doi.org/10.1016/j.ajme.2017.05.014
Manju S, Sreenivasan K (2010) Functionalised nanoparticles for targeted drug delivery. In: Sharma CP (ed) Biointegration. Med Implant Mater Sci Des Elsevier, pp 267–297. https://doi.org/10.1533/9781845699802.2.267
Mendelsohn J, Baselga J (2006) Epidermal growth factor receptor targeting in cancer. Semin Oncol 33:369–385. https://doi.org/10.1053/j.seminoncol.2006.04.003
Mohanraj VJ, Chen Y (2007) Nanoparticles - a review. Trop J Pharm Res 5:561–573. https://doi.org/10.4314/tjpr.v5i1.14634
Orsolini G, Fassio A, Rossini M, Adami G, Giollo A, Caimmi C, Idolazzi L, Viapiana O, Gatti D (2019) Effects of biological and targeted synthetic DMARDs on bone loss in rheumatoid arthritis. Pharmacol Res 147:104354. https://doi.org/10.1016/j.phrs.2019.104354
Oueslati MH, Ben TL, Harrath AH (2020) Catalytic, antioxidant and potential anticancer activities of gold nanoparticles synthesized by kaempferol glucoside from Lotus leguminosae. Arab J Chem 13:3112–3122. https://doi.org/10.1016/j.arabjc.2018.09.003
Pan D, Li N, Liu Y, Xu Q, Liu Q, You Y, Wei Z, Jiang Y, Liu M, Guo T, Cai X, Liu X, Wang Q, Liu M, Lei X, Zhang M, Zhao X, Lin C (2018) Kaempferol inhibits the migration and invasion of rheumatoid arthritis fibroblast-like synoviocytes by blocking activation of the MAPK pathway. Int Immunopharmacol 55:174–182. https://doi.org/10.1016/j.intimp.2017.12.011
Pelucchi C, Negri E (2017) Bladder cancer. In: International encyclopedia of public health. Elsevier Inc., pp 233–238. https://doi.org/10.1016/B978-0-12-803678-5.00035-7
Perera WPTD, Dissanayake RK, Ranatunga UI, Hettiarachchi NM, Perera KDC, Unagolla JM, De Silva RT, Pahalagedara LR (2020) Curcumin loaded zinc oxide nanoparticles for activity-enhanced antibacterial and potential anticancer applications. RSC Adv 10:30785–30795. https://doi.org/10.1039/d0ra05755j
Phromnoi K, Yodkeeree S, Anuchapreeda S, Limtrakul P (2009) Inhibition of MMP-3 activity and invasion of the MDA-MB-231 human invasive breast carcinoma cell line by bioflavonoids. Acta Pharmacol Sin 30:1169–1176. https://doi.org/10.1038/aps.2009.107
Pissuwan D (2017) Monitoring and tracking metallic nanobiomaterials in vivo. In: Narayan RJ (ed) Monitoring and evaluation of biomaterials and their performance in vivo, pp 135–149. https://doi.org/10.1016/B978-0-08-100603-0.00007-9
Poonia N, Kharb R, Lather V, Pandita D (2016) Nanostructured lipid carriers: versatile oral delivery vehicle. Futur Sci OA:2. https://doi.org/10.4155/fsoa-2016-0030
PubChem (2022) National Center for Biotechnology Information, PubChem Compound Summary for CID 5280863, Kaempferol. https://pubchem.ncbi.nlm.nih.gov/compound/Kaempferol. Accessed 27 May 2022
Radjabian M, Abetz V (2020) Advanced porous polymer membranes from self-assembling block copolymers. Prog Polym Sci 102:101219. https://doi.org/10.1016/j.progpolymsci.2020.101219
Rajendran P, Rengarajan T, Nandakumar N, Palaniswami R, Nishigaki Y, Nishigaki I (2014) Kaempferol, a potential cytostatic and cure for inflammatory disorders. Eur J Med Chem 86:103–112. https://doi.org/10.1016/j.ejmech.2014.08.011
Ren J, Lu Y, Qian Y, Chen B, Wu T, Ji G (2019) Recent progress regarding kaempferol for the treatment of various diseases. Exp Ther Med 18:2759–2776. https://doi.org/10.3892/etm.2019.7886
Sekiguchi A, Motegi S, Fujiwara C, Yamazaki S, Inoue Y, Uchiyama A, Akai R, Iwawaki T, Ishikawa (2019) Inhibitory effect of kaempferol on skin fi brosis in systemic sclerosis by the suppression of oxidative stress. J Dermatol Sci 96:8–17. https://doi.org/10.1016/j.jdermsci.2019.08.004
Sfakianos JP, Gellert LL, Maschino A, Gotto GT, Kim PH, Al-Ahmadie H, Bochner BH (2014) The role of PTEN tumor suppressor pathway staining in carcinoma in situ of the bladder. Urol Oncol Semin Orig Investig 32:657–662. https://doi.org/10.1016/j.urolonc.2014.02.003
Sharma D, Bhattacharya P, Kalia K, Tiwari V (2017) Diabetic nephropathy: new insights into established therapeutic paradigms and novel molecular targets. Diabetes Res Clin Pract 128:91–108. https://doi.org/10.1016/j.diabres.2017.04.010
Sharma D, Gondaliya P, Tiwari V, Kalia K (2019) Kaempferol attenuates diabetic nephropathy by inhibiting RhoA/Rho-kinase mediated inflammatory signalling. Biomed Pharmacother 109:1610–1619. https://doi.org/10.1016/j.biopha.2018.10.195
Srinivas Raghavan B, Kondath S, Anantanarayanan R, Rajaram R (2015) Kaempferol mediated synthesis of gold nanoparticles and their cytotoxic effects on MCF-7 cancer cell line. Process Biochem 50:1966–1976. https://doi.org/10.1016/j.procbio.2015.08.003
Subramaniam B, Siddik ZH, Nagoor NH (2020) Optimization of nanostructured lipid carriers: understanding the types, designs, and parameters in the process of formulations. J Nanoparticle Res 22:141. https://doi.org/10.1007/s11051-020-04848-0
Tarasiuk A, Mosińska P, Fichna J (2018) The mechanisms linking obesity to colon cancer: an overview. Obes Res Clin Pract 12:251–259. https://doi.org/10.1016/j.orcp.2018.01.005
Trivedi R, Kumar S, Kumar A, Siddiqui JA, Swarnkar G, Gupta V, Kendurker A, Dwivedi AK, Romero JR, Chattopadhyay N (2008) Kaempferol has osteogenic effect in ovariectomized adult Sprague-Dawley rats. Mol Cell Endocrinol 289:85–93. https://doi.org/10.1016/j.mce.2008.02.027
Tu LY, Bai HH, Cai JY, Deng SP (2016) The mechanism of kaempferol induced apoptosis and inhibited proliferation in human cervical cancer SiHa cell: from macro to nano. Scanning 38:644–653. https://doi.org/10.1002/sca.21312
Wang EC, Wang AZ (2014) Nanoparticles and their applications in cell and molecular biology. Integr Biol 6:9–26. https://doi.org/10.1039/c3ib40165k
Wang X, Yang Y, An Y, Fang G (2019) The mechanism of potential anticancer action and potential clinical use of kaempferol in the treatment of breast cancer. Biomed Pharmacother 117:109086. https://doi.org/10.1016/j.biopha.2019.109086
Xie F, Su M, Qiu W, Zhang M, Guo Z, Su B, Liu J, Li X, Zhou L (2013) Kaempferol promotes apoptosis in human bladder cancer cells by inducing the tumor suppressor, PTEN. Int J Mol Sci 14:21215–21226. https://doi.org/10.3390/ijms141121215
Yang Y, Wang Y, Wang T, Jiang X, Wang L (2017) Screening active components of modified Xiaoyao powder as NRF2 agonists. Cell Biochem Funct 35:518–526. https://doi.org/10.1002/cbf.3309
Yang J, Li J, Cui X, Li W, Xue Y, Shang P, Zhang H (2020) Blocking glucocorticoid signaling in osteoblasts and osteocytes prevents mechanical unloading-induced cortical bone loss. Bone 130:115108. https://doi.org/10.1016/j.bone.2019.115108
Yi X, Zuo J, Tan C, Xian S, Luo C, Chen S, Yu L, Luo Y (2016) Kaempferol, a flavonoid compound from gynura medica induced apoptosis and growth inhibition in MCF-7 breast cancer cell. Afr J Tradit Complement Altern Med 13:210–215. https://doi.org/10.21010/ajtcam.v13i4.27
Yoshida T, Konishi M, Horinaka M, Yasuda T, Goda AE, Taniguchi H, Yano K, Wakada M, Sakai T (2008) Kaempferol sensitizes colon cancer cells to TRAIL-induced apoptosis. Biochem Biophys Res Co 375:129–133. https://doi.org/10.1016/j.bbrc.2008.07.131
Zhang Y, Chen AY, Li M, Chen C, Yao Q (2008) Ginkgo biloba extract kaempferol inhibits cell proliferation and induces apoptosis in pancreatic cancer cells. J Surg Res 148:17–23. https://doi.org/10.1016/j.jss.2008.02.036
Zhang X, Xu M, Zhang Z, Hao L, Wang S, Jiang W (2017) Preparation and characterization of magnetic fluorescent microspheres for delivery of kaempferol. Mater Technol 32:125–130. https://doi.org/10.1080/10667857.2016.1157913
Zhang X, Pan Q, Hao L, Lin Q, Tian X, Zhang Z, Wang S, Wang H (2018) Preparation of magnetic fluorescent dual-drug nanocomposites for codelivery of kaempferol and paclitaxel. J Wuhan Univ Technol Mater Sci Ed 33:256–262. https://doi.org/10.1007/s11595-018-1814-z
Zhang F, Li R, Yan M, Li Q, Li Y, Wu X (2020) Ultra-small nanocomplexes based on polyvinylpyrrolidone K-17PF: a potential nanoplatform for the ocular delivery of kaempferol. Eur J Pharm Sci 147:105289. https://doi.org/10.1016/j.ejps.2020.105289
Zhu L, Xue L (2019) Kaempferol suppresses proliferation and induces cell cycle arrest, apoptosis, and DNA damage in breast cancer cells. Oncol Res 27:629–634. https://doi.org/10.3727/096504018X15228018559434
Author information
Authors and Affiliations
Contributions
The data collection using academic databases, designing of schematic diagrams and flowcharts using the BioRender application, and study conception for the potential clinical uses of kaempferol were done by AT and RK; they include collection of data on the therapeutic effects of kaempferol; its mechanism of action in the treatment of cancer of the breast, lung, colon, liver, pancreas, ovaries, prostate, and bladder; its exhibition of anti-diabetic activity in hyperglycaemic patients; and its treatment of skin fibrosis and bone loss. The data collection and use of academic databases, the designing and sketching of schematic diagrams using the Adobe Illustrator and BioRender applications, and study conception regarding the nanoformulation strategies of kaempferol were done by AT and LC, which include collection of data on nanoemulsions, nanoparticles, nanocomplexes, nanostructured lipid carriers, gold nanoparticles, nanomatrixes, and other magnetic nanoformulations.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chandekar, L., Katgeri, R. & Takke, A. The Potential Clinical Uses and Nanoformulation Strategies of Kaempferol, a Dietary Flavonoid. Rev. Bras. Farmacogn. 32, 693–707 (2022). https://doi.org/10.1007/s43450-022-00290-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43450-022-00290-6