Abstract
Glucagon-like peptide-1 (GLP-1) agonists play a crucial role in treating type 2 diabetes mellitus and obesity by providing glycemic control and aiding weight management. Despite their widespread use, concerns about serious adverse events have prompted extensive research. This review aims to describe the current understanding of serious adverse events associated with GLP-1 agonists. A comprehensive search of PubMed, Google Scholar and Embase databases was performed starting from 2010. Studies reporting evidence of an association between GLP-1 agonists and serious adverse events from 22 articles (5 case reports, 5 randomized controlled trials (RCTs), 9 real-world data cohort analyses, 2 meta-analyses and 1 systematic review and meta-analysis) were included and categorized by the type of adverse event. While some studies reported risks, including anaphylaxis, cardiovascular, gastrointestinal, psychiatric and thyroid-related events, others found no significant associations. The evidence remains mixed, necessitating further research to fully understand the safety profile of GLP-1 agonists and inform clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glucagon-like peptide-1 (GLP-1) receptor agonists have revolutionized the management of type 2 diabetes mellitus (T2DM) and obesity, offering glycemic control, weight loss, and cardiovascular benefits [1,2,3]. Despite their clinical efficacy and widespread use, concerns regarding serious adverse events (SAEs) have garnered significant attention within the public and medical community, prompting extensive research [1]. A serious adverse event related to a drug is defined as “any untoward medical occurrence that, at any dose, results in death, or is life-threatening, or requires hospitalization or prolongation of existing hospitalization, or is a congenital anomaly or birth defect [4].
A review of the literature reveals a spectrum of serious adverse events linked to GLP-1 agonist use [1]. Numerous observational studies and meta-analyses have reported conflicting findings regarding the association between GLP-1 agonists and serious adverse events involving the cardiovascular [5], gastrointestinal (GIT) system [6], skin [7], and mental health [8]. In contrast, others find no significant association [9, 10]. Similarly, concerns regarding thyroid safety have prompted regulatory scrutiny and ongoing research efforts to elucidate the actual risk profile of GLP-1 agonists [11]. Because clinical trials for GLP-1 agonists have short durations, rare and serious adverse events may not be adequately recognized. This review aims to describe the current understanding of serious adverse events associated with GLP-1 agonists.
Materials and methods
This review gathered recent and pertinent literature concerning serious adverse events linked with GLP-1 agonists. Utilizing PubMed, Google Scholar and Embase databases, it conducted comprehensive searches on hypersensitivity reactions, cardiovascular adverse events, pancreatitis, thyroid malignancies, bowel obstruction, and psychiatric adverse events, as they were identified previously as serious adverse events associated with GLP-1 agonist treatment [1, 5,6,7,8].
Eligibility, inclusion and exclusion criteria
Readily accessible English peer-reviewed articles published from 1 January 2010 until 10 February 2024 were included, incorporating evidence from randomized controlled trials (RCTs), observational studies, meta-analyses, case reports, and regulatory documentation. Studies reporting evidence of an association between GLP-1 agonists and serious adverse events were included and categorized by the type of adverse event. The findings and practice recommendations derived from these studies were summarized in a table. Additionally, studies that did not report an association between GLP-1 agonists and serious adverse events were discussed in a relevant section to provide an overview of these studies.
Results
This review synthesized evidence of GLP-1 agonists associated with serious adverse events from 22 articles: 5 case reports, 5 randomized controlled trials (RCTs), 9 real-world data analyses, 2 meta-analyses and 1 systematic review and meta-analysis Table 1. While some studies (n = 22) suggest links between GLP-1 agonists and serious adverse events, several evidences support their safety and effectiveness. Interpretations of the findings and practice recommendations derived from these articles were summarized (Table 1).
Hypersensitivity reactions
There are concerns regarding the potential association of GLP-1 agonists with anaphylactic reactions, which represent rare yet potentially life-threatening adverse events [1]. Exenatide has been linked to urticarial rash, shortness of breath, and anaphylaxis, while delayed injection site reactions were noted with liraglutide and delayed urticaria-like rash with dulaglutide [12,13,14].
Furthermore, a multisite population-based cohort study analysis revealed a modest increase in the risk of anaphylactic reaction with GLP-1 agonists compared to DPP-4 inhibitors and a 38% increased risk compared to sodium-glucose cotransporter-2 (SGLT2) inhibitors. These findings suggest a potential association between GLP-1 agonists and anaphylactic reactions; however, warranting further investigation [15].
Due to limited evidence in the literature, a standardized protocol for testing patients sensitized to one or more GLP-1 agonists is needed. Therefore, it is appropriate to consider an alternative non-GLP-1 receptor agonist glucose-lowering agent for individuals with a history of hypersensitivity reactions to any GLP-1 receptor agonist [16].
Of note, patients allergic to exenatide and lixisenatide subsequently tolerated the human GLP-1 analog, liraglutide. Additionally, there was a reported case of a patient sensitized to liraglutide who tolerated semaglutide, suggesting that alternative GLP-1 agonists within the same class could be considered [17].
Thyroid malignancies
Animal studies have fueled anxieties, demonstrating that GLP-1 agonists promote thyroid C-cell proliferation and hyperplasia in rodents, potentially leading to increased calcitonin production [18].
Several proposed mechanisms attempt to explain this observed C-cell proliferation, including direct GLP-1 receptor activation, which indirectly stimulates C-cell growth by activating other mitogenic pathways; however, translating findings from animal studies to humans requires caution due to interspecies differences in thyroid physiology and GLP-1 receptor distribution [18, 19].
Although GLP-1 agonists may affect thyroid hormone levels, clinical studies have not consistently shown significant alterations in thyroid function. Observational safety studies have produced conflicting results regarding the clinical relevance of pre-clinical findings, with some suggesting a potential link between GLP-1 agonists and thyroid hyperplasia. In contrast, others have found no significant association [19, 20]. RCTs indicated that thyroid cancer occurrence is rare with GLP-1 agonist exposure, while observational studies with higher bias risk yield inconsistent results [20, 21]. Overall, there is no definitive evidence of increased thyroid cancer risk with GLP-1 agonist therapy. These findings can inform clinicians when addressing patient concerns about a potential but unproven link between GLP-1 agonist therapy and thyroid cancer [20, 21].
A Korean study, funded by the government and pharmaceutical companies, utilized data from the Korean National Health Insurance Database (2014–2020). Two cohorts were established to compare GLP-1 agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors with SGLT2 inhibitors. The study revealed that neither GLP-1 agonists nor DPP-4 inhibitors were associated with an increased risk of thyroid cancer compared to SGLT2 inhibitors. Subgroup analyses and sensitivity analyses supported these findings [11].
Another study utilized the French national health care insurance system (SNDS) database to examine the link between GLP-1 agonists and thyroid neoplasms in individuals with type 2 diabetes treated with second-line anti-diabetic drugs from 2006 to 2018. It involved 2,562 case subjects with thyroid cancers and 45,184 control subjects. GLP-1 agonist used for 1–3 years was associated with an increased risk of all thyroid cancer (adjusted hazard ratio [HR] 1.58, 95% CI 1.27–1.95) and medullary thyroid cancer (adjusted HR 1.78, 95% CI 1.04–3.05) [22].
However, the study faced limitations, including potential mis-classification of outcomes and confounders due to coded diagnoses, lack of specific codes for medullary thyroid cancers, and potential misclassification in drug exposure assessment from health care databases and reporting bias [21].
A systematic review and meta-analysis study assessed the association between GLP-1 agonists and six types of thyroid disorders. The study revealed that GLP-1 agonists use was associated with a higher risk of overall thyroid disorders (RR 1.28, 95% CI 1.03–1.60) compared to placebo or other interventions. However, GLP-1 agonists did not significantly impact the occurrence of thyroid cancer, hyperthyroidism, hypothyroidism, thyroiditis, thyroid mass, or a goitre (all RRs close to 1.0 with wide CIs). The study concluded that GLP-1 agonists did not significantly alter the risk of thyroid disorders studied. Nevertheless, due to the low incidence of these disorders, further investigation is warranted to confirm these findings [23].
Another study aimed to assess whether liraglutide, a GLP-1 agonist, is associated with thyroid cancer risk compared to other anti-diabetic medications. The study used data from a US health plan (2010–2014); patients initiating liraglutide or other anti-diabetic drugs were followed for a median of 17 months. While relative risks varied across different comparisons, liraglutide initiators did not show a significantly elevated risk of thyroid cancer after adjusting for latency effects. However, caution is warranted due to potential residual confounding and surveillance bias, highlighting the need for further investigation into the association between liraglutide use and thyroid cancer risk [24].
In the EXSCEL RCT, evaluating the cardiovascular effects of adding once-weekly exenatide to usual care in patients with type 2 diabetes, the total number of patients who developed cancer was similar between the groups (355 in the exenatide group and 361 in the placebo group). The number of patients who had medullary thyroid carcinoma was two in the exenatide group and one in the placebo group. However, more patients in the exenatide group developed thyroid papillary carcinomas compared to the placebo group (10 vs. 4) [25].
Despite lacking conclusive evidence, regulatory bodies such as the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have adopted a precautionary approach. Most GLP-1 agonists carry a black box warning highlighting the potential risk of C-cell thyroid tumors. Additionally, guidelines recommend baseline and periodic monitoring of thyroid function, particularly in patients with pre-existing thyroid conditions or a family history of medullary thyroid carcinoma (MTC) [26].
Large-scale, well-designed studies with long-term follow-up are urgently needed to assess the risk of MTC associated with GLP-1 agonists definitively. Such studies should account for potential confounding factors, including pre-existing thyroid conditions, genetic pre-dispositions, and environmental exposures.
Cardiovascular adverse events
Various GLP-1 agonists have demonstrated a favorable impact on reducing major adverse cardiovascular events (MACE) in patients with type 2 diabetes and obesity, primarily evidenced through industry-sponsored RCTs, where semaglutide reduced the incidence of cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke in high-risk type 2 diabetes patients. At the same time, liraglutide also decreased the occurrence of similar outcomes in this population [3, 27, 28]. The SELECT RCT, involving 17,604 patients with pre-existing cardiovascular disease and overweight or obesity but without diabetes, showed that semaglutide at a dose of 2.4 mg was more effective than placebo in reducing the incidence of death from cardiovascular symptoms, nonfatal myocardial infarction, and non-fatal stroke over an average follow-up period of 39.8 months [28]. However, in the ELIXA RCT, adding lixisenatide to standard care did not change the rate of MACE or other serious adverse events, such as severe hypoglycemia, pancreatitis, and pancreatic neoplasms, compared to placebo [29]. In the STEP-HFpEF RCT, patients with heart failure with preserved ejection fraction (HFpEF) and obesity treated with semaglutide (2.4 mg) experienced more significant reductions in symptoms and physical limitations, improved exercise function, and more significant weight loss than those receiving a placebo [30]. However, further research is warranted to explore the potential risks of heart failure and pro-thrombotic effects as significant cardiovascular adverse events.
Despite the potential beneficial effects of GLP-1 agonists in improving heart failure, as suggested by pre-clinical studies, clinical evidence has indicated that GLP-1 agonist treatment might be linked to adverse heart failure events. For example, such treatment could lead to increased heart rate and reduced left ventricular ejection fraction (LVEF) associated with liraglutide [5].
In a trial involving 241 stable patients with chronic heart failure (LVEF ≤ 45%). Liraglutide 1.8 mg once daily did not significantly impact LVEF change compared to placebo (mean difference: -0.8%, P = 0.24), but it increased heart rate (mean difference: 7 b.p.m., P < 0.0001) and led to more serious cardiac events (10% vs. 3% in placebo, P = 0.04 (Table 1)). The study suggests liraglutide’s safety concerns in chronic heart failure patients despite its neutral effect on systolic function, prompting further investigation across heart failure subgroups. Limitations of this study include potential LVEF estimation variability and the relatively short treatment duration compared to other heart failure therapies [5].
Of note, a systematic review and meta-analysis aimed to synthesize the latest evidence on the cardiovascular benefits and risks of GLP-1 agonists. Eight trials involving 60,080 patients were analyzed, revealing that GLP-1 receptor agonists reduced MACE by 14%, all-cause mortality by 12%, hospital admission for heart failure by 11%, and the composite kidney outcome by 21%, without increasing severe hypoglycemia, retinopathy, or pancreatic adverse effects. The benefits remained consistent across different subgroups. The findings underscore the potential of GLP-1 receptor agonists to mitigate cardiovascular risks and improve kidney outcomes in patients with type 2 diabetes, irrespective of their structural homology [31]. None of the cardiovascular outcomes trials (CVOTs) reported fatal heart failure events or outpatient heart failure exacerbations, except for the REWIND trial [32, 33], which documented urgent heart failure visits without any significant differences between the treatment and control groups [33]. However, confirming the overall risk and benefit of GLP-1 agonists for heart failure has proven challenging, and careful monitoring and individual risk assessment remain crucial, particularly in high-risk patients.
Among type 2 diabetes patients, weekly exenatide did not significantly alter major cardiovascular events compared to placebo; these include fatal or nonfatal myocardial infarction, fatal or non-fatal stroke, and hospitalization for heart failure (EXSCEL trial) [25]. The EXSCEL trial observed a higher mean heart rate in the exenatide group compared to the placebo group [25]. A meta-analysis corroborated an elevated risk of heart failure hospitalization (HFH) associated with GLP-1 agonists in patients with LVEF < 40% (OR 1.49, 95% CI 1.05–2.10). These findings should be interpreted with caution as they are based on a subgroup analysis of the EXSCEL trial, pending further dedicated randomized controlled trials [34].
Gastrointestinal (GIT) adverse events
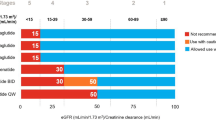
GIT adverse events are the most common with GLP-1 agonists and are the primary reason for treatment discontinuation [1, 3]. Nausea and vomiting, particularly during initiation or dose escalation, are frequent but typically resolve within weeks. However, their recurrence may impact patient adherence and quality of life [1, 3]. Severe GIT symptoms such as vomiting and diarrhea can lead to acute kidney injury [35], especially in patients with pre-existing renal impairment or other risk factors. Caution is advised, especially in patients with moderate to severe chronic kidney disease, as adverse kidney events have been linked to GIT symptoms. Close monitoring and discontinuation of medication may be necessary in cases of acute worsening of kidney function [35, 36].
A clinical guideline was established to address gastrointestinal symptoms associated with GLP-1 agonists, aiming to reduce treatment discontinuation [36]. The guideline recommends several strategies: healthcare providers (HCPs) may adjust the dosing schedule if GIT adverse events occur during the dose-escalation phase; patients experiencing GIT adverse events when advancing to a higher dose should revert to the lower dose for a few days before gradually increasing it; treatment may be temporarily withheld until the resolution of adverse events before resuming [36].
Adverse events involving the gallbladder and biliary ducts
Gallbladder disease, including cholelithiasis (gallstones) and cholecystitis (gallbladder inflammation), is a documented adverse event associated with GLP-1 receptor agonists [37, 38]. The elevated risk of gallbladder or biliary diseases with GLP-1 agonists is likely attributable to their inhibition of gallbladder motility and delayed emptying, resulting from the suppression of cholecystokinin secretion [39]. Furthermore, substantial weight loss in some patients using GLP-1 agonists may contribute to an increased risk of gallbladder disorders [37, 38].
A systematic review of 76 RCTs involving 103,371 patients found that GLP-1 agonists treatment increased the risk of gallbladder or biliary diseases, particularly cholelithiasis, cholecystitis and biliary disease. The risk was higher at higher doses, with more prolonged use, and in weight loss trials [40].
In the SURMOUNT-1 RCT, patients with obesity administered once-weekly tirzepatide at doses of 5 mg, 10 mg or 15 mg exhibited significant and sustained weight loss. The occurrence of cholecystitis and acute cholecystitis was higher in the tirzepatide-treated groups compared to the placebo groups, although the incidence was relatively low (≤ 0.6%). These findings are particularly essential for clinicians managing patients with a history of gallbladder disease [41].
Bowel obstruction
The likelihood of chronic intestinal obstruction in individuals increases gradually over time, with the peak incidence observed 1.6 years after starting GLP-1RA treatment. Nevertheless, typical clinical trials assessing GLP-1 agonists rarely extend beyond one year and studies indicate that constipation remains unaffected by short-term doses of GLP-1 agonists [6, 42, 43].
Initial concerns about increased ileus risk from case reports differ from significant RCT findings for GLP-1 agonists which haven’t shown heightened ileus occurrence. Observational studies hint at potential associations, prompting further investigation, especially regarding individual susceptibility due to pre-existing bowel conditions or electrolyte imbalances [6, 42, 43].
A real-world study using UK Clinical Practice Research Datalink data (2013–2019) compared GLP-1 agonists and DPP-4 inhibitors to SGLT-2 inhibitors regarding the risk of intestinal obstruction. The study found that both GLP-1 agonists and DPP-4 inhibitors posed an elevated risk of intestinal obstruction compared to SGLT-2 inhibitors, with GLP-1 agonists showing a hazard ratio (HR) of 1.69 (95% CI: 1.04–2.74) and DPP-4 inhibitors displaying increased risk after 1.8 years of use [6]. However, limitations such as exposure and outcome mis-classification and residual confounding were noted, warranting cautious interpretation of the findings [6].
In a real-world study from the University of British Columbia, non-diabetic GLP-1 agonist users had a higher risk of bowel obstruction compared to bupropion-naltrexone users (HR, 4.22 [95% CI, 1.02–17.40]) [43]. However, caution is warranted in interpreting findings due to confounding factors such as study population heterogeneity, varying ileus definitions, and short follow-up durations [1, 44]. Factors like pre-existing bowel conditions or co-medications could influence outcomes, while recent abdominal surgery or electrolyte imbalances might increase individual susceptibility to ileus with GLP-1 agonists. Additionally, GLP-1 agonists’ primary action of slowing gastric emptying could contribute to ileus, necessitating further exploration of this delay’s magnitude and long-term impact. Long-term randomized controlled trials assessing the risk of ileus with these drugs are currently lacking [1, 44].
Psychiatric adverse events
Concerns about potential psychiatric adverse events associated with GLP-1 agonists have prompted thorough investigation. An analysis of individual case safety reports summited to the European medication safety database (EudraVigilance) revealed psychiatric adverse symptoms associated with semaglutide, liraglutide, and tirzepatide with depression being the most reported, followed by anxiety and suicidal ideation. Nine deaths, primarily associated with liraglutide (n = 8), along with 11 life-threatening outcomes were reported. The fatal incidents mainly affected men (8 out of 9) and resulted from completed suicidal attempts and depression [8]. Although psychiatric adverse events accounted for only 1.2% of total reports, the severity and fatality of some cases indicate a need for further investigation [8]. The study had limitations including a lack of causality and a lack of denominator.
While the US FDA’s investigations found no clear association between GLP-1 agonists and suicidal thoughts or actions, ongoing scrutiny continues due to the small number of incidents observed. Patients are advised against discontinuing GLP agonists without medical consultation, and healthcare professionals should monitor for mood changes [45]. A retrospective cohort analysis comparing semaglutide with non-GLP-1 agonist medications over six months in overweight or obese patients and those with T2DM revealed lower suicidal ideation risk with semaglutide [10]. However, the short follow-up period poses limitations to the study’s generalizability.
Pancreatitis
Initial suspicions of a link between GLP-1 agonists and pancreatitis emerged from retrospective observational studies, prompting extensive research and discussions on potential mechanisms [46]. A study analyzing adverse event reports associated with sitagliptin and exenatide compared to other medications found a six-fold increase in reported pancreatitis odds ratios for sitagliptin or exenatide [46]. Pancreatic cancer was more frequently reported in patients using these drugs, consistent with case reports and animal studies suggesting an elevated risk of pancreatitis with GLP-1 therapy, leading to an FDA warning [47].
However, a systematic review and meta-analysis of twelve randomized trials involving 36,397 patients found no increased risk of pancreatic cancer with GLP-1 analogs compared to other treatments [48]. However, more extensive and longer-term studies are needed for confirmation and to address concerns about study duration and outcomes.
A meta-analysis examined the link between GLP-1 agonist use and acute pancreatitis and pancreatic cancer, drawing data from seven large-scale cardiovascular outcome trials involving 56,004 patients with T2DM. The analysis, spanning follow-up durations of 1.3 to 5.4 years, found no significant difference in the risk of acute pancreatitis or pancreatic cancer between GLP agonists and the placebo group. Both pooled results and sensitivity analyses did not reveal an increased risk of either condition associated with GLP-1 agonist use in T2DM patients [49].
However, in a real-world data study, GLP-1 agonists were associated with an increased risk of pancreatitis compared with bupropion-naltrexone (adjusted HR, 9.09 [95% CI, 1.25-66.00]). Additionally, the incidence of biliary disease (per 1000 person-years) was 11.7 for semaglutide, 18.6 for liraglutide, and 12.6 for bupropion-naltrexone and 4.6, 7.9 and 1.0, respectively [43].
While randomized controlled trials provide reassurance, isolated occurrences of pancreatitis among GLP-1 agonist users persist. Despite the absence of confirmed causality in most instances, these cases underscore the significance of patients promptly reporting any abdominal discomfort or suspected pancreatitis symptoms to facilitate timely diagnosis and intervention. Physicians should consider various factors, such as underlying pancreatic disorders, pre-existing gallstones, or concomitant medications, which may predispose individuals to pancreatitis [1, 43].
Discussion
This review examined serious adverse events linked to GLP-1 agonists. While some studies reported risks, including anaphylaxis, cardiovascular, gastrointestinal, psychiatric, and thyroid-related events, others found no significant associations. The evidence remains mixed, necessitating further research to fully understand the safety profile of GLP-1 agonists and inform clinical practice.
GLP-1 agonists play a vital role in managing type 2 diabetes mellitus and obesity, offering benefits in glycemic control and weight management [1,2,3]. Understanding serious adverse events associated with GLP-1 agonists demands careful consideration of evidence including study design, patient traits, and confounding factors.
Detecting serious adverse events in clinical trials is ultimately limited by small sample sizes, short durations, and selective participant selection, which restrict the identification of rare or long-term adverse events [50, 51]. Under-reporting due to observer bias, patient reluctance and sponsor influence further complicates detection [52]. Inadequate detection methods and mis-classification of adverse events also present significant challenges. The lack of long-term data in pre-marketing trials necessitates ongoing post-marketing surveillance [53, 54]. Adverse events are often considered secondary objectives, leading to less thorough reporting [55]. Variations in definitions, baseline characteristics, trial durations, routine care and event rates add to the complexity [52, 54]. Therefore, despite its limitations, using real-world data to assess large spontaneous reports is crucial for detecting rare and serious adverse effects not detected in clinical trials [56, 57].
GLP-1 agonists remain incompletely elucidated, with various confounding factors potentially influencing the accurate incidence of these adverse effects. For example, the potential association between GLP-1 agonists and pancreatic inflammation, including pancreatitis, is not well understood. Evidence from pre-clinical studies suggests that GLP-1 agonists may exert deleterious effects on pancreatic tissue. Specifically, administration of GLP-1 agonists such as exenatide in male rats has been associated with chronic pancreatic damage, characterized by pyknosis of acinar cells, increased cytoplasmic vacuolation, widened intercellular spaces, and infiltration of inflammatory cells [58, 59].
While some studies suggest links between GLP-1 agonists and serious adverse events, interpretations are intricate due to disease severity and comorbidities. Clinicians must weigh benefits against potential risks and monitor patients for adverse events. Continuous long-term safety assessments, particularly regarding cumulative effects and susceptibility in specific populations, are imperative. Furthermore, understanding mechanistic interactions, requires robust research and long-term observational studies to inform clinical practice.
Strengths and limitations of this study
This review presents the most recent evidence from the literature, encompassing randomized controlled trials and real-world cohort studies, concerning the potential serious adverse events linked with the emerging T2DM and obesity medications, notably GLP-1 agonists, which are increasingly employed in clinical settings. While this review does not explore causal relationships, it is essential to note that it is not a systematic review and is authored by a single individual. Consequently, it may be subject to selection and reporting biases, which could impact the generalizability of its findings. Nevertheless, it offers valuable insights into the safety of medications increasingly used worldwide for managing common conditions such as diabetes and obesity and may be subject to selection and reporting biases which affect the generalizability of findings. Of note, shedding light on this topic remains crucial, as many severe and rare adverse effects often go unnoticed in clinical trials due to their short duration and lack of specific focus on exploring such occurrences [8].
Despite concerns regarding the serious adverse events associated with GLP-1 agonists, the available evidence generally confirms their safety and efficacy. Clinicians are tasked with evaluating the benefits against potential risks and conducting vigilant monitoring for adverse events in patients [1, 8]. This responsibility should involve a collaborative effort among the medical team, comprising pharmacists and nurses. Patients should also report any unpleasant adverse effects to their treating physicians. Thorough comprehension of pharmacological interventions such as GLP-1 agonists is imperative for proficient management. Further research is warranted to clarify mechanistic pathways and inform evidence-based decision-making in clinical practice, thereby ensuring optimal utilization and patient safety. Key questions, including definitive associations between GLP-1 agonists and serious adverse outcomes and understanding mechanistic interactions, require robust research and long-term observational studies to inform clinical practice.
Conclusion
While some studies suggest links between GLP-1 agonists and serious adverse events, evidence supports their safety and effectiveness. Interpretations are intricate due to disease severity and comorbidities. Clinicians must weigh benefits against potential risks and monitor patients for adverse events. A comprehensive understanding of pharmacological interventions such as GLP-1 agonists is essential for effective management. Further research is needed to elucidate mechanistic pathways and guide evidence-based decision-making in clinical practice ensuring optimal use and patient safety.
Data availability
Data supporting the study’s findings are available from the corresponding author upon reasonable request.
Abbreviations
- T2DM:
-
Ttype 2 Diabetes Mellitus
- SGLT2:
-
Sodium-glucose Cotransporter-2
- DPP-4:
-
Dipeptidyl Peptidase-4
- SELECT trial:
-
Semaglutide Effects on Heart Disease and Stroke in Patients With Overweight or Obesity
- ELIXA trial:
-
Evaluation of LIXisenatide in Acute Coronary Syndrome
- EXSCEL:
-
Exenatide Study of Cardiovascular Event Lowering
- LVEF:
-
Left Ventricular Ejection Fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- STEP-HFpEF:
-
Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity
- SNDS:
-
French National Health Care Insurance System
- HCPs:
-
Healthcare Providers
References
Filippatos TD, Panagiotopoulou TV, Elisaf MS. Adverse effects of GLP-1 receptor agonists. Rev Diabet Stud. 2014 Fall-Winter;11(3–4):202–30.
Heuvelman VD, Van Raalte DH, Smits MM. Cardiovascular effects of glucagon-like peptide 1 receptor agonists: from mechanistic studies in humans to clinical outcomes. Cardiovascular Res. 2020;116(5):916–30.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and Cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22.
Cook D, Lauzier F, Rocha MG, Sayles MJ, Finfer S. Serious adverse events in academic critical care research. CMAJ. 2008;178(9):1181–4.
Jorsal A, Kistorp C, Holmager P, Tougaard RS, Nielsen R, Hänselmann A, et al. Effect of liraglutide, a glucagon-like peptide-1 analogue, on left ventricular function in stable chronic heart failure patients with and without diabetes (LIVE)-a multicentre, double-blind, randomised, placebo-controlled trial. Eur J Heart Fail. 2017;19(1):69–77. https://doi.org/10.1002/ejhf.657.
Faillie JL, Yin H, Yu OHY, Herrero A, Altwegg R, Renoux C, et al. Incretin-based drugs and risk of intestinal obstruction among patients with type 2 diabetes. Clin Pharmacol Ther. 2022;111(1):272–82.
Steveling EH, Winzeler B, Bircher AJ. Systemic allergic reaction to the GLP-1 receptor agonist exenatide. J Pharm Technol. 2014;30(5):182–6.
Tobaiqy M, Elkout H. Psychiatric adverse events associated with semaglutide, liraglutide and tirzepatide: a pharmacovigilance analysis of individual case safety reports submitted to the EudraVigilance database. Int J Clin Pharm. 2024;46(2):488–95. https://doi.org/10.1007/s11096-023-01694-7.
Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. STEP-HFpEF trial committees and investigators. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023;389(12):1069–84.
Wang W, Volkow ND, Berger NA, Davis PB, Kaelber DC, Xu R. Association of semaglutide with risk of suicidal ideation in a real-world cohort. Nat Med. 2024;30(1):168–76.
Bea S, Son H, Bae JH, Cho SW, Shin JY, Cho YM. Risk of thyroid cancer associated with glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in patients with type 2 diabetes: a population-based cohort study. Diabetes Obes Metab. 2024;26(1):108–17.
Pérez E, Martínez-Tadeo J, Callero A, Hernández G, Rodríguez-Plata E, García-Robaina JC. A case report of allergy to exenatide. J Allergy Clin Immunol Pract. 2014;2(6):822–3.
Carvallo A, Silva C, Gastaminza G, D’Amelio C. Delayed hypersensitivity reaction to liraglutide: a case report. J Investig Allergol Clin Immunol. 2020;30(5):367–9.
Bianchi L, Ali Biglu Marash S, Malatesta N, Hansel K, Tramontana M, Stingeni L. Hypersensitivity to glucagon-like peptide-1 receptor agonists: a case of delayed urticaria-like rash to dulaglutide and literature review. JEADV Clin Pract. 2024;3:313–6.
Pradhan R, Patorno E, Tesfaye H, Schneeweiss S, Yin H, Franklin J, et al. Glucagon-like peptide 1 receptor agonists and risk of anaphylactic reaction among patients with type 2 diabetes: a Multisite Population-based Cohort Study. Am J Epidemiol. 2022;191(8):1352–67.
Dungan K, DeSantis A. Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus. In: Post TW, ed. UpToDate. Waltham (MA): UpToDate; 2023: http://www.uptodate.com [Last accessed 20 Feb 2024].
Shetty R, Basheer FT, Poojari PG, Thunga G, Chandran VP, Acharya LD. Adverse drug reactions of GLP-1 agonists: a systematic review of case reports. Diabetes Metab Syndr. 2022;16(3):102427.
Bjerre Knudsen L, Madsen LW, Andersen S, Almholt K, de Boer AS, Drucker DJ, et al. Glucagon-like peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology. 2010;151:1473–86.
Rosol TJ. On-target effects of GLP-1 receptor agonists on thyroid C-cells in rats and mice. Toxicol Pathol. 2013;41(2):303–9. https://doi.org/10.1177/0192623312472402.
De Espinosa AE, Brito JP, McCoy RG, Shao H, Singh Ospina N. Glucagon-like Peptide-1 receptor agonists and thyroid Cancer: a narrative review. Thyroid. 2024;34(4):403–18. https://doi.org/10.1089/thy.2023.0530. Epub 2024 Mar 26.
Thompson CA, Stürmer T, Putting. GLP-1 RAs and thyroid Cancer in Context: additional evidence and remaining doubts. Diabetes Care. 2023;46(2):249–51.
Bezin J, Gouverneur A, Pénichon M, Mathieu C, Garrel R, Hillaire-Buys D, et al. Pariente A, Faillie JL. GLP-1 receptor agonists and the risk of thyroid Cancer. Diabetes Care. 2023;46(2):384–90.
Hu W, Song R, Cheng R, Liu C, Guo R, Tang W, Zhang J, et al. Use of GLP-1 receptor agonists and occurrence of thyroid disorders: a Meta-Analysis of Randomized controlled trials. Front Endocrinol (Lausanne). 2022;13:927859.
Funch D, Mortimer K, Ziyadeh NJ, Seeger D, Zhou J, Ng L, Major-Pedersen E, Bosch-Traberg A, Gydesen H, Dore H, et al. Risk of thyroid Cancer Associated with Use of Liraglutide and other antidiabetic drugs in a US commercially insured Population. Diabetes Metab Syndr Obes. 2021;14:2619–29.
Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, et al. EXSCEL Study Group. Effects of once-weekly Exenatide on Cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228–39. https://doi.org/10.1056/NEJMoa1612917.
Prescribing Information. WEGOVY (semaglutide) injection, for subcutaneous use https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/215256s003lbl.pdf. [Last accessed 20 Feb 2024].
Sattar N, McGuire DK, Pavo I, Weerakkody GJ, Nishiyama H, Wiese RJ, et al. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591–8. https://doi.org/10.1038/s41591-022-01707-4.
Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. SELECT Trial investigators. Semaglutide and Cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389(24):2221–32.
Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Køber LV, et al. ELIXA investigators. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–57. https://doi.org/10.1056/NEJMoa1509225.
Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9(10):653–62.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. REWIND investigators. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–30. https://doi.org/10.1016/S0140-6736(19)31149-3.
Khan MS, Fonarow GC, McGuire DK, Hernandez AF, Vaduganathan M, Rosenstock J, et al. Glucagon-like peptide 1 receptor agonists and heart failure: the need for further evidence generation and practice guidelines optimization. Circulation. 2020;142(12):1205–18. https://doi.org/10.1161/CIRCULATIONAHA.120.045888.
Neves JS, Packer M, Ferreira JP. Increased risk of heart failure hospitalization with GLP-1 receptor agonists in patients with reduced ejection fraction: a Meta-analysis of the EXSCEL and FIGHT trials. J Card Fail. 2023;29(7):1107–9. https://doi.org/10.1016/j.cardfail.2023.03.017.
Leehey DJ, Rahman MA, Borys E, Picken MM, Clise CE. Acute kidney Injury Associated with Semaglutide. Kidney Med. 2021;3(2):282–5.
Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, Castro A, Cebrián-Cuenca A, de Torres-Sánchez A, et al. Recommendations to manage gastrointestinal adverse events in patients treated with Glp-1 receptor agonists: a Multidisciplinary Expert Consensus. J Clin Med. 2022;12(1):145.
Nexøe-Larsen CC, Sørensen PH, Hausner H, Agersnap M, Baekdal M, Brønden A, Gustafsson LN, Sonne DP, Vedtofte L, Vilsbøll T, Knop FK. Effects of liraglutide on gallbladder emptying: A randomized, placebo-controlled trial in adults with overweight or obesity. Diabetes Obes Metab. 2018;20(11):2557–2564. https://doi.org/10.1111/dom.13420. Epub 2018 Jul 10.
Rehfeld JF, Knop FK, Asmar A, Madsbad S, Holst JJ, Asmar M. Cholecystokinin secretion is suppressed by glucagon-like peptide-1: clue to the mechanism of the adverse gallbladder events of GLP-1-derived drugs. Scand J Gastroenterol. 2018;53(12):1429–32. https://doi.org/10.1080/00365521.2018.1530297.
Faillie JL, Yu OH, Yin H, Hillaire-Buys D, Barkun A, Azoulay L. Association of Bile Duct and Gallbladder diseases with the Use of Incretin-based drugs in patients with type 2 diabetes Mellitus. JAMA Intern Med. 2016;176(10):1474–81. https://doi.org/10.1001/jamainternmed.2016.1531.
He L, Wang J, Ping F, Yang N, Huang J, Li Y, et al. Association of Glucagon-Like Peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: a systematic review and Meta-analysis of Randomized clinical trials. JAMA Intern Med. 2022;182(5):513–9. https://doi.org/10.1001/jamainternmed.2022.0338.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. SURMOUNT-1 investigators. Tirzepatide once Weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205–16. https://doi.org/10.1056/NEJMoa2206038.
Lu J, Liu H, Zhou Q, Wang MW, Li Z. A potentially serious adverse effect of GLP-1 receptor agonists. Acta Pharm Sin B. 2023;13(5):2291–3.
Sodhi M, Rezaeianzadeh R, Kezouh A, Etminan M. Risk of gastrointestinal adverse events Associated with Glucagon-Like Peptide-1 receptor agonists for weight loss. JAMA. 2023;330(18):1795–7.
Maselli DB, Camilleri M. Effects of GLP-1 and its analogs on gastric physiology in diabetes Mellitus and obesity. Adv Exp Med Biol. 2021;1307:171–92.
No causal link between GLP-1 RAs and suicidal ideation. Reactions Weekly 1991, 5 (2024). https://doi.org/10.1007/s40278-024-52517-9. https://www.fda.gov/drugs/drug-safety-and-availability/update-fdas-ongoing-evaluation-reports-suicidal-thoughts-or-actions-patients-taking-certain-type. [Last accessed 20 Feb 2024].
Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141(1):150–6. https://doi.org/10.1053/j.gastro.2011.02.018.
Food and drug Administration (FDA). 2016. Drug Safety Communication: FDA investigating reports of possible increased risk of pancreatitis and pre-cancerous findings of the pancreas from incretin mimetic drugs for type 2 diabetes, https://www.fda.gov/Drugs/DrugSafety/ucm343187.htm. [Last accessed 20 Feb 2024].
Pinto LC, Falcetta MR, Rados DV, Leitão CB, Gross JL. Glucagon-like peptide-1 receptor agonists and pancreatic cancer: a meta-analysis with trial sequential analysis. Sci Rep. 2019;9(1):2375. https://doi.org/10.1038/s41598-019-38956-2.
Cao C, Yang S, Zhou Z. GLP-1 receptor agonists and pancreatic safety concerns in type 2 diabetic patients: data from cardiovascular outcome trials. Endocrine. 2020;68(3):518–25. https://doi.org/10.1007/s12020-020-02223-6.
Aronson JK, Ferner RE. Clarification of terminology in drug safety. Drug Saf. 2005;28(10):851–70. https://doi.org/10.2165/00002018-200528100-00003.
Pirmohamed M, Breckenridge AM, Kitteringham NR, Park BK. Adverse drug reactions. BMJ. 1998;316(7140):1295–8. https://doi.org/10.1136/bmj.316.7140.1295.
Ioannidis JP. Adverse events in randomized trials: neglected, restricted, distorted, and silenced. Arch Intern Med. 2009;169(19):1737–9. https://doi.org/10.1001/archinternmed.2009.313.
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–9. https://doi.org/10.1016/S0140-6736(00)02799-9.
Schroll JB, Maund E, Gøtzsche PC. Challenges in coding adverse events in clinical trials: a systematic review. PLoS ONE. 2012;7(7):e41174. https://doi.org/10.1371/journal.pone.0041174.
Loke YK, Derry S. Reporting of adverse drug reactions in randomised controlled trials - a systematic survey. BMC Clin Pharmacol. 2001;1:3. https://doi.org/10.1186/1472-6904-1-3. Epub 2001 Sep 12.
Hersh WR, Weiner MG, Embi PJ, Logan JR, Payne PR, Bernstam EV, et al. Caveats for the use of operational electronic health record data in comparative effectiveness research. Med Care. 2013;51(8 Suppl 3):S30–7. https://doi.org/10.1097/MLR.0b013e31829b1dbd.
Tobaiqy M, Elkout H, MacLure K. Analysis of thrombotic adverse reactions of COVID-19 AstraZeneca Vaccine reported to EudraVigilance Database. Vaccines (Basel). 2021;9(4):393. https://doi.org/10.3390/vaccines9040393.
Lee PH, Stockton MD, Franks AS. Acute pancreatitis associated with liraglutide. Ann Pharmacother. 2011;45(4):e22. https://doi.org/10.1345/aph.1P714.
Yu X, Tang H, Huang L, Yang Y, Tian B, Yu C. Exenatide-induced chronic damage of pancreatic tissue in rats. Pancreas. 2012;41(8):1235–40. https://doi.org/10.1097/MPA.0b013e31824e67a3.
Mondragon A, Davidsson D, Kyriakoudi S, Bertling A, Gomes-Faria R, Cohen P, et al. Divergent effects of liraglutide, exendin-4, and sitagliptin on beta-cell mass and indicators of pancreatitis in a mouse model of hyperglycaemia. PLoS ONE. 2014;9(8):e104873. https://doi.org/10.1371/journal.pone.0104873.
Funding
The author did not receive any funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tobaiqy, M. A review of serious adverse events linked with GLP-1 agonists in type 2 diabetes mellitus and obesity treatment. Pharmacol. Rep 76, 981–990 (2024). https://doi.org/10.1007/s43440-024-00629-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-024-00629-x