Abstract
Background
Surgical management of adolescent idiopathic scoliosis (AIS) and Scheuermann’s kyphosis (SK) may be associated with several complications including extended length of stay and unplanned reoperations. Several studies have previously compared postoperative complications and functional outcomes for AIS and SK patients with mixed results. However, a meta-analysis compiling the literature on this topic is lacking.
Methods
Following the PRISMA guidelines, PubMed, Cochrane, and Google Scholar (pages 1–20) were accessed and explored until April 2024. The extracted data consisted of complications (overall and surgical-site infections [SSI]), readmissions, reoperations, and Scoliosis Research Society-22 (SRS-22) score. Mean differences (MD) with 95% CI were used for continuous data and odds ratio (OR) was utilized for dichotomous data were calculated across studies.
Results
Seven retrospective articles were included in the meta-analysis, including 4866 patients, with 399 in the SK group and 4467 in the AIS group. SK patients were found to have statistically significantly higher rates of overall complications (OR = 5.41; 95% CI 3.69–7.93, p < .001), SSI (OR = 11.30; 95% CI 6.14–20.82, p < .001), readmissions (OR = 2.81; 95% CI 1.21–6.53, p = 0.02), and reoperations (OR = 7.40; 95% CI 4.76–11.51, p < .001) than AIS patients. However, they had similar SRS-22 scores postoperatively (MD = −0.06; 95% CI −0.16 to 0.04, p = 0.26) despite the SK group having lower SRS-22 scores preoperatively (MD = −0.30; 95% CI −0.42 to −0.18, p < .001).
Conclusion
In this meta-analysis of studies comparing spinal deformity surgery outcomes in AIS and SK patients, SK was associated with more complications, readmissions, and reoperations. SK did have equivalent SRS-22 scores postoperatively to AIS patients, highlighting the benefit of surgical treatment despite higher complication rates. This data may help inform healthcare institutions, payors, and quality monitoring organizations who examine outcomes of pediatric and adult spinal deformity surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common cause of scoliosis, affecting 2–4% of adolescents, with incidence rates ranging between 0.47% and 5.2% [1,2,3,4,5]. AIS is characterized as a curvature of the spine with a Cobb angle greater than 10° with vertebral rotation [6]. While the pathophysiology of AIS is largely unknown, contributing factors include genetic polymorphisms, hormone and signaling peptide dysregulation, environmental triggers, such as diet and exercise, and physiological deficiencies in bone and muscle tissue surrounding the spine [1].
Scheuermann’s kyphosis (SK), also known as Scheuermann’s disease, is the second most common developmental disorder in patients with a spinal deformity after AIS [7, 8]. This type of kyphosis develops in early adolescence with a reported prevalence ranging from 0.4 to 8.3% [8,9,10,11]. Definitions of SK vary, but the current widely accepted diagnostic criterion is the wedging of three adjacent vertebral bodies by at least 5° [12]. Similar to AIS, a detailed understanding of the etiology of SK is limited, though genetic roots, altered spinal biomechanics, and abnormal tissue composition have been increasingly investigated [13].
AIS, SK, and other spinal diseases have major impacts on quality of life for children and adolescents [14, 15]. In fact, these two spinal conditions are different, reaching the threshold for operative management at different stages being earlier in SK. Surgical treatments of these conditions have advanced over the last few decades, but several complications that necessitate extended length of stay (LOS) and unplanned reoperation still remain [16,17,18,19,20,21]. Specifically, studies report a 9.2% 2-year revision risk following primary pediatric spinal deformity surgery, and extended LOS rates of up to 91% for SK and 59% for idiopathic deformities [17, 22]. On the other hand, Sarwahi et al. reported similar revision rates and infection rates between AIS and SK [22]. Several studies have compared postoperative complications and quality of life data for AIS and SK patients with differing results [22,23,24]. However, no prior meta-analysis has compiled literatures comparing the surgical outcomes of these two etiologies. As such, the purpose of this meta-analysis was to compare the outcomes of spinal deformity surgery in AIS and SK patients to help inform healthcare quality monitoring efforts.
Materials and methods
Search strategy
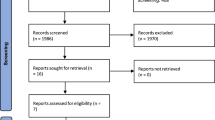
Following the PRISMA guidelines, PubMed, Cochrane, and Google Scholar (pages 1–20) were accessed and explored until April 2024 using the following keywords “Scheuermann”, “AIS” and “idiopathic scoliosis” to find articles comparing SK and AIS patients undergoing spinal deformity surgery. Additional articles were added by going through reference lists from articles. One author extracted the data, and another confirmed the choice of the included articles. The process is summarized in the PRISMA flowchart (Fig. 1).
Articles were included if they consisted of comparative studies, comparing SK to AIS patients undergoing spinal deformity surgery. Comparative articles with nonrelevant outcomes, as well as non-comparative articles were excluded.
Data extraction
Eligibility of the included studies were determined by two reviewers independently. The extracted data consisted of complications [overall complications, and surgical-site infections (SSI)], readmissions, reoperations, and patient-reported outcome measures (PROMs) [Scoliosis Research Society-22 score (SRS-22)]. If present, differences between the investigators were resolved by a third independent reviewer. No software tools were used to aid with data extraction, it was doing manually on an excel sheet.
Risk-of-bias assessment
The ROBINS-I tool was used to assess the risk of bias in the included non-randomized studies by two authors independently [25]. Studies were evaluated for their confounding bias, selection bias, classification bias, bias due to deviation from interventions, bias due to missing data, bias in outcomes measurements, and bias in the selection of reported results and were graded to have a low, moderate, serious, or critical risk. If the study had a moderate, serious, or critical risk of bias in at least one of the domains, it will be classified as having an overall moderate, serious or critical risk of bias respectively. It is considered to have a low risk of bias if all the evaluated domains had a low risk of bias. Studies were excluded if they had a critical risk of bias.
Statistical analysis
Review Manager 5.4 (The Cochrane Collaboration, 2020) was implemented for the statistical analysis. Mean differences (MD) with 95% CI were used for continuous data while odds ratio (OR) was utilized for dichotomous data. Heterogeneity was evaluated by Q tests and I2 statistics. If considerable heterogeneity was indicated by p ≤ 0.05 or I2 > 50%, random-effects model was used. Otherwise, the fixed-effect model was implemented. A statistically significant result is shown by p ≤ 0.05.
Results
Characteristics of the included studies
Seven retrospective articles from 5 cohorts met the inclusion criteria [15, 17,18,19, 22,23,24]. These studies included 4866 patients, with 399 in the SK group and 4467 in the AIS group. The main characteristics of the included studies are summarized in Table 1.
Adverse events
Overall complications
Four studies including 3573 patients reported data about overall complications (294 in the SK group and 3279 in the AIS group). SK patients had a statistically significantly higher rate of complications than AIS patients (odds ratio = 5.41; 95% CI 3.69–7.93, p < 0.001, Fig. 2A).
SSI
Three studies including 2974 patients reported data about SSI (260 in the SK group and 2714 in the AIS group). SK patients had a statistically significantly higher rate of SSI than AIS patients (odds ratio = 11.30; 95% CI 6.14–20.82, p < 0.001, Fig. 2B).
Readmission
Two studies including 1354 patients reported data about overall complications (97 in the SK group and 1257 in the AIS group). SK patients had a statistically significantly higher rate of readmissions than AIS patients (Odds Ratio = 2.81; 95% CI 1.21–6.53, p = 0.02, Fig. 2C).
Reoperations
Three studies including 2974 patients reported data about reoperations (260 in the SK group and 2714 in the AIS group). SK patients had a statistically significantly higher rate of reoperations than AIS patients (odds ratio = 7.40; 95% CI 4.76–11.51, p < 0.001, Fig. 2D).
PROMs
Two studies including 2175 patients reported data about SRS-22 (187 in the SK group and 1988 in the AIS group). A lower pre-operative score was shown in SK patients (mean difference = −0.30; 95% CI −0.42 to −0.18, p < 0.001, Fig. 3A). However, no statistically significant difference was shown between the two groups postoperatively (mean difference = −0.06; 95% CI −0.16 to 0.04, p = 0.26, Fig. 3B).
Discussion
Previous studies have investigated outcomes of spine surgery between SK and AIS patients. This meta-analysis was conducted with the objective of offering more definitive data regarding the difference in outcomes between these two patient populations. The results of this meta-analysis revealed that SK patients have a higher rate of post-operative SSI, overall complications, readmission, and reoperations. However, both AIS and SK have similar PROMs post-operatively despite SK patients having lower scores pre-operatively highlighting the life-changing effects of kyphosis correction. In all the analyzed outcomes, the heterogeneity assessed using I2 was below the threshold of 50% making the studies only mildly heterogeneous without affecting the results of this meta-analysis.
SK patients were shown to have five times more post-operative complications, 11 times more the SSI, 3 times more readmission, and seven times more reoperations. These higher adverse events may be attributable to several causes. Patients with SK may require more extensive surgery including longer instrumentation and increased use of osteotomies, thus increasing operative time and mitigating positive outcomes in patients managed by surgeons with limited experiences in those procedures [18, 26, 27]. In addition, the higher rate of SSI could be result of the proximal extent of the dissection needed at the base of the neck (C7, T1, T2 upper instrumented vertebrae) in SK patients as this area is prone to contamination due to the difficulty of intraoperative draping [23]. Furthermore, the cantilever forces required to correct the kyphosis on top of the pull-out forces at both extremities of the construct may ultimately increase the risk of implant failure [28,29,30,31,32]. This notion is supported by the fact that the main etiology for reoperation in SK patients was shown to be implant failure [18]. Carefully choosing fusion levels, choosing the best upper instrumented level, proper rod contouring, and avoiding overcorrection are crucial to preventing these issues [31]. Furthermore, because of their low prevalence, SK patients are either underrepresented in many cohort studies or the focus of small single-center research, which leads to a large variation in the surgical threshold and strategy [33,34,35,36]. As a result, caring for these individuals is frequently seen as a judgment test. Therefore, creating a more standardized national strategy could decrease the adverse events seen in these patients. Nevertheless, educating SK patients pre-operatively on the higher post-operative risks is important. Furthermore, additional research on the management of SK may help reduce post-operative risks and aid in the understanding of this entity.
Patients with SK had similar post-operative SRS-22 total scores compared to AIS patients despite having lower pre-operative scores. Previous research has demonstrated that, in comparison to age- and sex-matched controls, SK patients report feeling more self-conscious about their appearance preoperatively. They also note lower self-image domain scores than both AIS patients and normal controls. The self-image domain of the SRS, in fact, is most strongly correlated with kyphosis magnitude when compared to other SRS domains [37,38,39]. This could explain why SK patients require more invasive surgeries, thus leading the higher rates of post-operative adverse events. However, one must note that only two studies (including 187 in the SK group and 1988 in the AIS group) were included in the PROMs analysis as other studies did not report the values of SRS-22 scores.
Despite this study comparing surgical outcomes of between AIS and SK, one should note that these 2 conditions are fundamentally different, often reaching the threshold for surgical intervention at distinct stages in pediatric spinal deformity centers, being earlier in SK. The unequal weighting in favor of AIS in the analyzed studies reflects the higher incidence of AIS, potentially leading to an underestimation of the complexities associated with SK surgeries. This disparity might result in oversimplification of SK as a uniplanar deformity, miscalculations in surgical strategies, and a skewed approach influenced by the more routine AIS procedures, thereby increasing the risk of postoperative complications. Additionally, SK surgeries generally involve more extensive procedures extending into the lumbar spine, unlike many AIS surgeries. The complexity and extent of SK surgeries naturally lead to higher complication rates, which may not have been appropriately accounted for in our comparisons.
Strengths and limitations
While this meta-analysis is the first to compare the outcomes of posterior fusion in AIS and SK, it has several potential limitations. Only comparative studies were included which limited the number of studies included in the overall analysis. Moreover, the included studies were of retrospective nature limiting the level of evidence of this meta-analysis. The low number of studies in some outcome analysis may limit the generalizability of these findings. Furthermore, the variability in study designs, and surgical techniques, and the potential publication bias among the included studies may have introduced heterogeneity into our analysis, which could have influenced the interpretation of results and the validity of our conclusions. In addition, the pooling of these studies and the missing granularity in their results restricted us from doing sub-analyses based on the demographics and potential confounding factors of the patients. Finally, the limited availability of long-term follow-up data in some studies may have restricted our ability to assess the durability of outcomes over time.
Conclusion
In this meta-analysis of studies comparing spinal deformity surgery outcomes in AIS and SK patients, SK was associated with more complications, readmissions, and reoperations. However, they had similar postoperative SRS-22 scores despite having lower preoperative scores. These results highlight the differences between surgical treatment of SK and AIS, which may help inform efforts to monitoring quality and outcomes of spinal deformity surgery. Future studies following AIS and SK patients prospectively are required in order to provide a higher level of evidence to the existing body of literature.
References
Kikanloo SR, Tarpada SP, Cho W (2019) Etiology of adolescent idiopathic scoliosis: a literature review. Asian Spine J 13:519–26. https://doi.org/10.31616/asj.2018.0096
Thomas JJ, Stans AA, Milbrandt TA, Kremers HM, Shaughnessy WJ, Larson AN (2021) Trends in incidence of adolescent idiopathic scoliosis: a modern US population-based study. J Pediatr Orthop 41:327–332. https://doi.org/10.1097/BPO.0000000000001808
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7:3–9. https://doi.org/10.1007/s11832-012-0457-4
Fong DYT, Cheung KMC, Wong Y-W, Wan Y-Y, Lee C-F, Lam T-P et al (2015) A population-based cohort study of 394,401 children followed for 10 years exhibits sustained effectiveness of scoliosis screening. Spine J 15:825–833. https://doi.org/10.1016/j.spinee.2015.01.019
Ohrt-Nissen S, Hallager DW, Henriksen JL, Gehrchen M, Dahl B (2016) Curve magnitude in patients referred for evaluation of adolescent idiopathic scoliosis: five years’ experience from a system without school screening. Spine Deform 4:120–124. https://doi.org/10.1016/j.jspd.2015.10.001
Addai D, Zarkos J, Bowey AJ (2020) Current concepts in the diagnosis and management of adolescent idiopathic scoliosis. Child’s Nerv Syst 36:1111–1119. https://doi.org/10.1007/s00381-020-04608-4
Bezalel T, Carmeli E, Kalichman L (2019) Scheuermann’s disease: radiographic pathomorphology and association with clinical features. Asian Spine J 13:86–95. https://doi.org/10.31616/asj.2018.0025
Sebaaly A, Farjallah S, Kharrat K, Kreichati G, Daher M (2022) Scheuermann’s kyphosis: update on pathophysiology and surgical treatment. EFORT Open Rev 7:782–791. https://doi.org/10.1530/EOR-22-0063
Daniels AH, Jurgensmeier D, McKee J, Harrison MW, D’Amato CR (2009) Acute celiac artery compression syndrome after surgical correction of Scheuermann kyphosis. Spine 34:E149-52. https://doi.org/10.1097/BRS.0b013e3181918f05
Ali RM, Green DW, Patel TC (1999) Scheuermannʼs kyphosis. Curr Opin Pediatr 11:66–69. https://doi.org/10.1097/00008480-199902000-00014
Suominen EN, Saarinen AJ, Syvänen J, Diarbakerli E, Helenius L, Gerdhem P et al (2022) Health-related quality of life outcomes in adolescent Scheuermann’s kyphosis patients treated with posterior spinal fusion: a comparison with age- and sex-matched controls. J Child Orthop 16:290–296. https://doi.org/10.1177/18632521221106384
Palazzo C, Sailhan F, Revel M (2014) Scheuermann’s disease: an update. Jt Bone Spine 81:209–214. https://doi.org/10.1016/j.jbspin.2013.11.012
O’Donnell JM, Wu W, Youn A, Mann A, Swarup I (2023) Scheuermann kyphosis: current concepts and management. Curr Rev Musculoskelet Med 16:521–530. https://doi.org/10.1007/s12178-023-09861-z
Sebaaly A, Daher M, Salameh B, Ghoul A, George S, Roukoz S (2022) Congenital scoliosis: a narrative review and proposal of a treatment algorithm. EFORT Open Rev 7:318–327. https://doi.org/10.1530/EOR-21-0121
Tsirikos AI, García-Martínez S (2023) Long-term health-related quality of life (QOL) after paediatric spinal deformity surgery and comparison with the general population. J Clin Med. https://doi.org/10.3390/jcm12227142
Roberts SB, Tsirikos AI (2022) paediatric spinal deformity surgery: complications and their management. Healthcare 10:2519. https://doi.org/10.3390/healthcare10122519
Fruergaard S, Ohrt-nissen S, Pitter FT, Høy K, Lindberg-larsen M, Eiskjær S et al (2021) Length of stay, readmission, and mortality after primary surgery for pediatric spinal deformities: a 10-year nationwide cohort study. Spine J 21:653–663. https://doi.org/10.1016/j.spinee.2021.01.004
Fruergaard S, Ohrt-nissen S, Pitter FT, Høy K, Lindberg-larsen M, Eiskjær S et al (2021) Revision risk after pediatric spinal deformity surgery: a nationwide study with 2-year follow-up. Spine J 21:642–652. https://doi.org/10.1016/j.spinee.2020.12.002
Jain A, Puvanesarajah V, Menga EN, Sponseller PD (2015) Unplanned hospital readmissions and reoperations after pediatric spinal fusion surgery. Spine 40:856–62. https://doi.org/10.1097/BRS.0000000000000857
Aoun M, Daher M, Bizdikian A-J, Kreichati G, Kharrat K, Sebaaly A (2024) Implant density in adolescent idiopathic scoliosis: a meta-analysis of clinical and radiological outcomes. Spine Deform. https://doi.org/10.1007/s43390-024-00860-9
Daher M, Aoun M, Kreichati G, Kharrat K, Sebaaly A (2024) Hybrid vs all pedicle screws constructs in adolescent idiopathic scoliosis: a metaanalysis of clinical and radiological outcomes. Spine Deform. https://doi.org/10.1007/s43390-024-00886-z
Sarwahi V, Hasan S, Koutsogiannis P, Dzaugis P, Vora R, Molloy S et al (2022) Scheuermann kyphosis patients have a similar revision and infection rate to adolescent idiopathic scoliosis patients. Spine 47:E290-5. https://doi.org/10.1097/BRS.0000000000004233
Lonner BS, Toombs CS, Guss M, Braaksma B, Shah SA, Samdani A et al (2015) Complications in operative scheuermann kyphosis. Spine 40:305–11. https://doi.org/10.1097/BRS.0000000000000757
Toombs C, Lonner B, Shah S, Samdani A, Cahill P, Shufflebarger H et al (2018) Quality of life improvement following surgery in adolescent spinal deformity patients: a comparison between scheuermann kyphosis and adolescent idiopathic scoliosis*. Spine Deform 6:676–683. https://doi.org/10.1016/j.jspd.2018.04.009
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Daniels AH, Daher M, Singh M, Balmaceno-Criss M, Lafage R, Diebo BG et al (2023) The case for operative efficiency in adult spinal deformity surgery: impact of operative time on complications, length of stay, alignment, fusion rates, and patient reported outcomes. Spine. https://doi.org/10.1097/BRS.0000000000004873
Coe JD, Smith JS, Berven S, Arlet V, Donaldson W, Hanson D et al (2010) Complications of spinal fusion for Scheuermann kyphosis. Spine 35:99–103. https://doi.org/10.1097/BRS.0b013e3181c47f0f
Gong Y, Yuan L, He M, Yu M, Zeng Y, Liu X et al (2019) Comparison between stable sagittal vertebra and first lordotic vertebra instrumentation for prevention of distal junctional kyphosis in Scheuermann disease: systematic review and meta-analysis. Clin Spine Surg 32:330–336. https://doi.org/10.1097/BSD.0000000000000792
Lonner BS, Newton P, Betz R, Scharf C, O’Brien M, Sponseller P et al (2007) Operative management of Scheuermannʼs kyphosis in 78 patients. Spine 32:2644–52. https://doi.org/10.1097/BRS.0b013e31815a5238
Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD (2006) Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. J Am Acad Child Adolesc Psychiatry 45:512–519
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: Minimum five-year follow-up. Spine 34:729–34. https://doi.org/10.1097/BRS.0b013e3181ae2ab2
Horn SR, Poorman GW, Tishelman JC, Bortz CA, Segreto FA, Moon JY et al (2019) Trends in treatment of Scheuermann kyphosis: a study of 1,070 cases from 2003 to 2012. Spine Deform 7:100–106. https://doi.org/10.1016/j.jspd.2018.06.004
Jain A, Sponseller PD, Kebaish KM, Mesfin A (2015) National trends in spinal fusion surgery for Scheuermann kyphosis. Spine Deform 3:52–56. https://doi.org/10.1016/j.jspd.2014.06.009
Lee SS, Lenke LG, Kuklo TR, Valenté L, Bridwell KH, Sides B et al (2006) Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine 31:2316–21. https://doi.org/10.1097/01.brs.0000238977.36165.b8
Koller H, Juliane Z, Umstaetter M, Meier O, Schmidt R, Hitzl W (2014) Surgical treatment of Scheuermann’s kyphosis using a combined antero-posterior strategy and pedicle screw constructs: efficacy, radiographic and clinical outcomes in 111 cases. Eur Spine J 23:180–191. https://doi.org/10.1007/s00586-013-2894-2
Polly DW, Ledonio CGT, Diamond B, Labelle H, Sucato DJ, Hresko MT et al (2019) What are the indications for spinal fusion surgery in Scheuermann kyphosis? J Pediatr Orthop 39:217–221. https://doi.org/10.1097/BPO.0000000000000931
Petcharaporn M, Pawelek J, Bastrom T, Lonner B, Newton PO (2007) The relationship between thoracic hyperkyphosis and the Scoliosis Research Society outcomes instrument. Spine 32:2226–31. https://doi.org/10.1097/BRS.0b013e31814b1bef
Murray PM, Weinstein SL, Spratt KF (1993) The natural history and long-term follow-up of Scheuermann kyphosis. J Bone Joint Surg Am 75:236–248. https://doi.org/10.2106/00004623-199302000-00011
Lonner B, Yoo A, Terran JS, Sponseller P, Samdani A, Betz R et al (2013) Effect of spinal deformity on adolescent quality of Life. Spine 38:1049–55. https://doi.org/10.1097/BRS.0b013e3182893c01
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
MD: data acquisition, writing original draft, approved the version to be submitted, accountable for all aspects of the work. RR: data acquisition, writing original draft, approved the version to be submitted, accountable for all aspects of the work. MS: data acquisition, writing original draft, approved the version to be submitted, accountable for all aspects of the work. JN: data acquisition, writing original draft, approved the version to be submitted, accountable for all aspects of the work. CI: data acquisition, writing original draft, approved the version to be submitted, accountable for all aspects of the work. BGD: interpretation of data, review, editing, approved the version to be submitted, accountable for all aspects of the work. AHD: interpretation of data, review, editing, and supervision, approved the version to be submitted, accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
BGD reports the following: receives consulting fees from Clariance, SpineArt, and SpineVision. AHD discloses the following, receives royalties from Spineart and Stryker, consulting fees from Medtornic, research support from Alphatec, Medtronic, and Orthofix, and Fellowship support from Medtronic. Remaining authors do not report any conflict.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Daher, M., Rasquinha, R., Singh, M. et al. Spinal deformity surgery in Scheuermann’s kyphosis versus adolescent idiopathic scoliosis: meta-analysis of complications and clinical outcomes. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00967-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00967-z