Abstract
Background
The growth guidance (GG) method for treatment of early onset scoliosis has as its primary goal the restoration of apical spinal alignment, facilitating normal spinal growth to achieve a suitable adult thoracic height.
Purpose
To evaluate whether GG surgical treatment achieves comparable thoracic and spinal height to distraction-based treatment (DBT) in idiopathic early onset scoliosis (I-EOS) patients. We hypothesized that GG would prove superior to DBT at the time of definitive fusion surgery.
Methods
All I-EOS patients who underwent GG at a single center were reviewed. T1–L1 and T1–S1 heights were measured using the traditional coronal method as well as the Halifax sagittal spinal length (SSL) technique. The same measurements were obtained from a comparable control group obtained from a multi-center pediatric early onset scoliosis database who underwent treatment with traditional growing rods (TGR) or magnetically controlled growing rods (MCGR).
Results
Of the I-EOS patients who underwent GG 2004–2019, 15 patients underwent final fusion after GG completion, with a mean 5.5 years of GG treatment prior to fusion (range 2.0–11.4 years). Mean age at GG implantation was 8.4 years (range 2.0–11.7 years); 7 were male and 8 female. GG patients experienced a mean coronal thoracic height increase of 6.2 cm during treatment through final fusion, and a mean coronal spinal height increase of 8.8 cm. At the time of final fusion, GG patients achieved greater significant mean increases than DBT patients by 2.9 cm in coronal thoracic height (p = 0.0023), 4.5 cm in coronal spinal height (p = 0.001), and 4.0 cm in SSL spinal height (p = 0.01). No GG patient concluded treatment with a thoracic height less than 18 cm in either coronal or sagittal plane.
Conclusions
Not only did 100% of GG patients reach minimum thoracic height of 18 cm at time of final fusion, but GG also proved to be superior to distraction-based constructs in a comparison cohort on 3 of 4 spinal elongation measures.
Level of evidence.
3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of early onset scoliosis (EOS) continues to be one of the most significant challenges in pediatric orthopaedics. Various strategies for growth-preserving spinal correction exist, but without strong consensus on which techniques are most effective for each type of EOS patients. Within the classification subtypes of EOS, idiopathic EOS (I-EOS) patients are more homogeneous in that they typically do not have significant medical comorbidities or concomitant musculoskeletal deformities (El-Hawary and Akbarnia, [1]). However, I-EOS patients arguably have the highest functional demands to achieve successful treatment, in that they are fully ambulatory and have normal pulmonary demands. Treatment thereby must utilize implants that accommodate normal childhood movement demands while also maximizing thoracic height and pulmonary development (Skaggs DL et al., [2]).
Distraction-based techniques (DBT) have been the mainstay of surgical I-EOS treatment (El-Hawary et al., [7]). These include traditional growing rods (TGR), vertical expandable prosthetic titanium rib (VEPTR), or the more recent development of magnetically controlled growing rods (MCGR). The constant between these options, however, is multiple return trips to the operating room or multiple, time-sensitive clinic visits for lengthening.
Growth guidance (GG) is an alternative treatment strategy that seeks to avoid these downsides of distraction-based EOS treatment. The primary advantage of GG is that it allows for continued spinal elongation without repeat rod lengthening or additional surgical interventions. GG harnesses the child’s spinal growth to achieve spinal elongation, using specially designed screws that allow for sliding of the rod at the proximal and distal ends of the construct for growth around a selective fusion at the apex of the deformity (Morell and McCarthy, [5]).
There are conflicting reports in the literature regarding the relative effectiveness of DBT and GG in terms of achieving sufficient thoracic height at the completion of treatment (Morell and McCarthy, [5]; Skaggs DL et al., [2]; Nazareth et al., [9]). Most of these studies had heterogeneous cohorts of EOS patients, only evaluated coronal height measurements, and had varying time endpoints for determining spinal growth. The purpose of this study was to evaluate in detail the changes in thoracic (T1–T12) and spinal (T1–S1) heights specifically of I-EOS patients in both the coronal and sagittal planes, using the final fusion as a common endpoint of treatment. We hypothesized that GG would prove superior to DBT at the time of definitive fusion surgery in terms of achieving thoracic and spinal elongation.
Methods
After institutional review board approval, a retrospective analysis was completed of all patients with early onset scoliosis at a single institution who underwent the guided growth (GG) procedure from 2004–2020. Patients with I-EOS were then selected as a cohort, as these patients were felt to have the greatest functional demands on the implants, highest expectation for normal body proportions and pulmonary function, and the least heterogeneity in spinal anatomy and medical comorbidities.
For each subject in the idiopathic diagnosis group, radiographs were obtained from four distinct time periods; pre-operative, immediately post-operative from GG, 2 years post-operative from GG, and immediately post-operative from final fusion. Patient were excluded from the analysis if they had not yet undergone final fusion, were lost to follow up before 2 years, or had an index procedure prior to GG. Radiographs were voided of identifying information and were uploaded to a surgical planning software site, Surgimap (Nemaris Inc., Globus Medical Inc., Audubon, PA). Surgimap software allows for the creation of a database of radiographs and contains measuring tools to obtain a variety of spinal parameters.
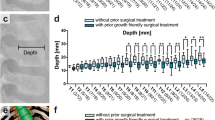
For each radiograph, thoracic spinal height (T1–T12) and total spinal height (T1–S1) were measured in the coronal plane of a standing PA full-length radiograph. Because the coronal measurements do not account for the effect of kyphosis and lordosis on true spinal length, sagittal spine length (SSL) was also calculated for each radiograph using the validated Halifax methodology. A series of multiple points were selected to create a best-fit line on the lateral standing full-length film for the thoracic length (T1–T12) and the total spinal length (T1–S1) (Spurway et al., [6])(Fig. 1).
The multi-center Pediatric Spine Study Group (PSSG) database was used to identify a similar cohort of patients who underwent DBT, who met the following inclusion criteria and for which a complete set of radiographs was available. Inclusion criteria for DBT cohort were diagnosis of I-EOS, treatment with either TGR or MCGR distraction-based constructs, age < 10 years at index procedure, and completion of treatment with final fusion. TGR and MCGR patients were both included in the DBT cohort, as these surgeries are conceptually similar in mechanism of spinal elongation; there is published precedent for analysis of these patients as a single DBT group (Doany et al., [11]; Tahir et al., [12]). Patients were excluded if they had undergone a prior surgical intervention before index DBT. Identical radiograph time points and measurements were utilized with the DBT cohort as was done with the GG cohort.
Data were summarized by group using means and standard deviations (SDs) for continuous variables, and using numbers and proportions for categorical variables. The study group treated with guided growth (n = 15) was compared to the control group treated with TGR and MCGR (n = 39) for differences in patient characteristics as follows. Continuous characteristics were compared using Student’s t test if variances were roughly equal, Welch’s t test if they were unequal, and the Kruskal–Wallis test if data were non-normally distributed. Categorical characteristics were compared with Pearson’s chi-square test if all cell counts had expected value ≥ 5, or with the Fisher exact test otherwise. Groups were also compared for differences in thoracic height and spinal height during the pre-operative study period, at the 2 year follow-up, and at final fusion using Welch’s t test (i.e., without confounder adjustment). Finally, the GG cohort was compared to the DBT cohort for evidence of efficacy, both at the 2 year follow-up and at final fusion, using unequal-variance ANCOVA with Satterthwaite’s degrees-of-freedom procedure. At each post-operative time, the efficacy outcome in each ANCOVA model was the post-operative value of thoracic height (either coronal or sagittal) or of spinal height (either coronal or sagittal). The class variable in each ANCOVA model was Cohort, which was allowed to have unequal variances. The two continuous confounders in each ANCOVA model were (A) the subject’s pre-operative value of the efficacy outcome, and (B) the subject’s age at first surgery. SAS v9.4 software (SAS Institute Inc., Cary, NC, USA) was employed for all analysis procedures, and a two-sided p < 0.05 significance level was utilized for all statistical hypothesis tests.
Results
126 GG cases were performed at our institution from 2004 to 2020; of these, 37 were categorized as I-EOS. Of these 37 I-EOS patients, 30 had returned for 2 year follow-up (mean 7.0 years, range 2.4–15.4 years), with 15 having completed their guided growth and undergone final fusion. Patients in this cohort had a mean pre-operative age of 8.5 years, a mean pre-operative coronal curve magnitude of 63 degrees, and thoracic kyphosis of 44 degrees. In the GG cohort, 7 patients were male and 8 female. Their immediate post-operative coronal curve magnitude was 19.8 degrees with a thoracic kyphosis of 30 degrees. The immediate post-operative curve magnitude was not available for the DBT cohort (Table 1).
The DBT cohort consisted of 39 patients, 35 with TGR and 4 with MCGR. Patients in this cohort had a mean age at initial surgery of 7.2 years, a mean pre-operative coronal curve magnitude of 74 degrees, and a mean thoracic kyphosis of 49 degrees. Thirteen were male and 26 female (Table 1). When comparing the pre-operative mean thoracic and spinal heights in the coronal and sagittal planes, there were no significant differences between the GG and DBT cohorts (Table 2).
The average number of operations was 4.3 in the GG cohort and 9.0 in the DBT cohort (p < 0.001; Table 1). When patients from the two procedures were compared to each other for height differences at the 2 year follow-up (Table 2), GG patients had larger sagittal thoracic and spinal heights, with statistical significance after confounder adjustment for pre-operative height and age at first surgery. Specifically, the GG cohort in the sagittal plane was 2.0 cm taller in thoracic height (p = 0.045) and 3.1 cm taller in spinal height (p = 0.036) compared to the DBT cohort. When viewed in the coronal plane, the 2 year group differences in thoracic height and spinal height were both 1 cm larger for GG compared to DBT, although they did not attain statistical significance (Table 2).
At the time of final fusion, GG patients enjoyed both noticeably taller means and noticeably narrower SDs on all four radiological height measures than did DBT patients (Table 2). On three of the four measures, the difference in means was statistically significant both before and after adjusting for pre-operative height and age at first surgery. Thoracic height in the coronal plane had means of 25.2 cm for GG versus 21.8 cm for DBT, yielding an unadjusted difference of 3.4 cm (p = 0.0021) plus an ANCOVA-adjusted difference of 2.9 cm (p = 0.0023), both of which favored GG (Table 2). Likewise, spinal height in the coronal plane had means of 41.3 cm for GG versus 36.1 cm for DBT, yielding a difference of 5.2 cm (p = 0.0004) before adjustment and 4.5 cm (p = 0.0010) after ANCOVA adjustment (Table 2). Spinal height in the sagittal plane showed a similar increase with GG compared to DBT, the raw and ANCOVA-adjusted differences being 4.9 cm (p = 0.0030) and 4.0 cm (p = 0.0112), respectively (Table 2).
Overall, GG patients experienced a mean coronal thoracic height increase of 6.2 cm during treatment through final fusion, and a mean coronal spinal height increase of 8.8 cm. DBT patients finished treatment with a mean coronal thoracic height increase of 4.2 cm, and a mean coronal spinal height increase of 6 cm (Table 2). All GG patients concluded treatment with a thoracic height of at least 18 cm, while only 85% (33/39) of the DBT patients reached this threshold at final fusion.
Discussion
The purpose of this study was to evaluate in detail whether GG achieves thoracic and spinal heights comparable to traditional distraction-based methods for treating I-EOS patients. We employed the traditional coronal measurements, as well as the validated SSL measurement technique. Sagittal height measurements have not been previously published for the GG population. At time of final fusion after undergoing GG, patients had a mean thoracic height of 25.2 cm in the coronal plane and 26.8 cm in the sagittal plane, which is well above the minimum thoracic height to avoid thoracic insufficiency syndrome (Karol et al., [3]; Skaggs DL et al., [2]; Tis et al., [4], Theologis et al., [8]). All of our GG patients successfully surpassed the often-quoted goal minimum thoracic height of 18 cm, and while the utility of this threshold value continues to be debated, we believe that GG does not compromise the potential for an I-EOS patient to reach an adequate and proportional chest size (Johnston et al., [13]).
Not only did the GG patients enjoy taller thoracic and spinal heights than did the distraction-based patients by the time of final fusion, but also those height benefits with GG persisted after ANCOVA-adjusting for pre-operative heights and age at first surgery. Including these two confounders in each ANCOVA model has the effect of adjusting all patients’ post-operative heights to the values they would have had if the patients had started with equal pre-operative heights and equal ages at first surgery. For this reason, the ANCOVA-adjusted group difference in post-operative heights is equivalent to (and interpretable as) the ANCOVA-adjusted group difference in the amounts by which each procedure increased the average post-operative height measure from its pre-operative value. By this interpretation, the GG procedure was superior to the DBT procedure on three of the four height measures. Finally, the standard deviations in thoracic and spinal heights were uniformly narrower in GG patients compared to DBT patients at the time of final fusion. This fact indicates that the results obtained after GG may be more reliable than those obtained after DBT.
As EOS is quite heterogeneous, the previous studies have included a variety of etiologies. This study chose to focus on idiopathic EOS to evaluate a more homogenous population. Another strength of this study was the length of post-operative follow-up. The average follow-up was 8.6 years with all patients except one reaching the 4 year follow-up time point.
It has previously been hypothesized that the limited fusion and avoidance of submuscular dissection allows for more remaining flexibility in GG patients at the time of final fusion, in contrast to TGR patients (Morell and McCarthy, [5]). Even if there is residual deformity, this retained flexibility can then be leveraged for additional deformity correction at final fusion. We observed that the 15 GG patients had thoracic- and spinal-height increases of 2.6 cm and 4.4 cm, respectively, in the coronal plane from the 2 year follow-up to final fusion. This was in contrast to coronal-plane thoracic- and spinal-height increases of 1.0 cm and 1.7 cm among the 27 evaluable DBT patients over the same treatment interval. Moreover, we believe that the apical derotation and coronal correction achieved at the index GG surgery allows for spinal elongation to occur along, or close to, the coronal plumbline of the body, rather than off-axis.
Nazareth et al. reported on coronal thoracic and spinal height increase in a separate population of GG patients. They studied 20 GG cases, of which only 3 were I-EOS patients. The authors identified that the mean thoracic height increase from pre-operative measurements to final pre-fusion follow-up was 4.2 cm, and that mean spinal height increase was 7.3 cm. Both of these mean values are less than what we identified. Importantly, their study did not include post-fusion measurements or a DBT control group. We believe that a crucial aspect of the GG procedure is the flexibility retained in the spine at the time of final fusion that allows for further height increase, and that this fact should be reflected in the overall analysis of the procedure’s effectiveness. Moreover, the Nazareth et al.’s GG patient cohort was heterogeneous in terms of scoliosis diagnosis. The authors’ experience is that the surgical technique and expected outcomes for use of GG in neuromuscular, syndromic, and congenital EOS patients differs significantly from I-EOS, and at this point, GG should not be reasonably studied by considering all these different groups as one patient population.
The values we obtained for DBT spinal elongation are consistent with the previous reports. Glotzbecker et al. reported a mean coronal thoracic height increase of 2.0 cm after 5 years of TGR treatment in 41 EOS patients (Glozbecker et al., [10]). We measured 3.7 cm of mean coronal thoracic height increase for DBT patients over the entire course of treatment. Tahir et al. identified a mean coronal spinal height increase of 6.9 cm in 43 EOS patients, through final fusion. They subanalyzed TGR and MCGR patients and found no significant difference in final T1-S1 coronal height between these two distraction treatment strategies (Tahir et al., [12]). We identified a mean spinal height increase over the course of treatment of 6.0 cm in our DBT cohort.
Limitations of this study include its retrospective nature. The GG patients were from a single center and are a small sample size. The DBT patients were from multiple centers, and we do not have details on the decision for TGR versus MCGR in those patients. When comparing the two procedures, there were slight differences in the study populations. The GG patients were older, which was adjusted for in the analysis, and had slightly smaller pre-operative curvature when compared to DBT patients. Other aspects of the GG procedure, including deformity correction and complications, have been previously described; the goal of this study is not to re-state those results.
GG meets several other criteria listed in the SRS Growing Spine Committees goals (Skaggs DL et al., [2]). The committee states that treatment should minimize burden on patient and families. GG requires fewer trips to the doctor, as it does not require in-clinic lengthening. For many rural families, who travel a great distance to be seen by specialists, this can alleviate a significant amount of stress related to transport and time away from work and school. Additionally, GG requires fewer surgical interventions. The GG patients in this study had an average of 4 surgical interventions overall, with an average of only 3 interventions (range: 2–5) after excluding one patient (16 surgeries) who was converted to TGR. In contrast, TGR patients typically require ten lengthening surgeries to achieve sufficient spinal height (El-Hawary et al., [7]). Finally, if GG patients do not return for regular follow-up, which the reality of the practice of medicine today, they have less risk of negative impact as they simply continue to grow along the rods. This is in contrast to patients with magnetic or traditional growing rods who could experience significant complications if they do not return for regularly scheduled time-sensitive appointments.
In conclusion, though both treatment modalities achieve thoracic and spinal growth, GG achieves significantly larger increases in coronal thoracic and spinal height, and sagittal spinal height at the time of final fusion when compared to DBT.
References
El-Hawary R, Akbarnia BA (2015) Early onset scoliosis-time for consensus. Spine Deform 3(2):105–106
Skaggs DL, Guillaume T, El-Hawary R et al (2015) Early onset scoliosis consensus statement, srs growing spine committee, 2015. Spine Deform 3:107
Karol LA, Johnston C, Mladenov K et al (2008) Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Jt Surg Am 90:1272–1281
Tis JE, Karlin LI, Akbarnia BA et al (2012) Early onset scoliosis modern treatment and results. J Pediatric Orthop 32:647–657
McCarthy R, Morell S (2016) New developments in the treatment of early onset spinal deformity: role of the Shilla growth guidance system. Med Devices: Evid Res 9:241–246
Spurway AJ, Chukwunyerenwa CK, Kishta WE et al (2016) Sagittal spine length measurements: a novel technique to assess growth of the spine. Spine Deform 4:331–337
El-Hawary et al (2020) Distraction-based surgeries increase thoracic sagittal spine length after ten lengthening surgeries for patients with idiopathic early onset scoliosis. Spine Deform 8:303–309
Theologis AA, Smith J, Kerstein M, Gregory JR, Luhmann SJ (2019) Normative data of pulmonary function tests and radiographic measures of chest development in children without spinal deformity: is a t1–t12 height of 22 cm adequate? Spine Deform 7:857–864. https://doi.org/10.1016/j.jspd.2019.01.010
Nazareth A, Skaggs DL, Illingworth KD, Parent S, Shah SA, Sanders JO, Andras LM, Growing Spine Study Group (2020) Growth guidance constructs with apical fusion and sliding pedicle screws (SHILLA) results in approximately 1/3rd of normal T1–S1 growth. Spine Deform. 8:531–535. https://doi.org/10.1007/s43390-020-00076-7
Glotzbecker MP, Gold M, Miller P, Akbarnia BA, Johnston C, Sanchez Perez Grueso F, Shah SA, Emans J (2014) Distraction-based treatment maintains predicted thoracic dimensions in early-onset scoliosis. Spine Deform 2(3):203–207. https://doi.org/10.1016/j.jspd.2014.03.001
Doany ME, Olgun ZD, Kinikli GI, Bekmez S, Kocyigit A, Demirkiran G, Karaagaoglu AE, Yazici M (2018) Health-related quality of life in early-onset scoliosis patients treated surgically: eosq scores in traditional growing rod versus magnetically controlled growing rods. Spine (Phila Pa1976). 43:148–153. https://doi.org/10.1097/BRS.0000000000002274
Tahir M, Mehta D, Sandhu C, Jones M, Gardner A, Mehta JS (2022) A comparison of the post-fusion outcome of patients with early onset scoliosis treated with traditional and magnetically controlled growing rods. Bone Jt J 104:257–264. https://doi.org/10.1302/0301-620X.104B2.BJJ-2021-1198.R1
Johnston CE, Karol LA, Thornberg D, Jo C, Eamara P (2021) The 18-cm thoracic-height threshold and pulmonary function in non-neuromuscular early-onset scoliosis: a reassessment. JB JS Open Access 6(21):00093. https://doi.org/10.2106/JBJS.OA.21.00093
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Cornaghie: Data Collection. Data analysis. Writing—original draft preparation, approval of final version of manuscript, agree to be accountable for the work. Bumpass: Writing—editing, data collection, approval of final version, agree to be accountable for the work. McCarthy: Study conception, data collection, approval of final version, agree to be accountable for the work. Siegel: Statistical analysis, writing—original draft preparation, approval of final version, agree to be accountable for work. Roeder: Data Collection, approval of final version of manuscript, agree to be accountable for the work.
Corresponding author
Ethics declarations
Conflict of interest
Authors M. Cornaghie, L. Roeder, and E.R. Siegel have no financial interests to disclose. Author D. Bumpass has received a consulting and speaking fee from Medtronic. Author R. McCarthy has received a consulting and speaking fee from Medtronic and OrthoPediatrics.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of the University of Arkansas approved this study.
Informed consent
Informed consent was exempted due to the type of research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cornaghie, M., Bumpass, D., Roeder, L. et al. Spinal height for growth guidance treatment in early onset idiopathic scoliosis: analysis through final surgical treatment. Spine Deform 12, 1485–1491 (2024). https://doi.org/10.1007/s43390-024-00891-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-024-00891-2