Abstract
Study design
Retrospective study of a prospectively collected database at one center.
Objectives
Assess the outcomes and complications of adult spinal deformity (ASD) surgery in patients that are 75 years and older compared with patients of 65–75 years of age.
Summary of background data
With increasing amounts of ASD surgery being performed on elderly patients, it is important to assess how age plays a factor in corrective reconstruction surgery.
Methods
Inclusion criteria for the study were all patients ≥ 65 years of age that underwent thoracolumbar deformity correction involving ≥ four levels at a single institution by two surgeons. Patients were divided based on age into 65–74.9 or ≥ 75 groups. Radiographic parameters were measured preoperatively, postoperatively, and at 2 years. The Numeric Rating Scale (NRS) and Oswestry Disability Index (ODI) were collected preoperatively, at 1 year, and 2 years. Comorbidities included were based around the Charlson Comorbidity Index (CCI) and compared to the incidence of complications and need for further surgery.
Results
Both age groups had improvements in their radiographic parameters postoperatively which was maintained at 2 years. Comparing the different age groups with similar comorbidity burden in regard to complications and need for additional surgery yielded no statistically significant difference between groups. Both groups had comparable decreases in NRS and increases in ODI at 2 years.
Conclusions
Analysis of our study population indicates that there is no difference between the outcomes and complications of deformity surgery in patients 75 years and older when compared to a younger elderly population. It also does not appear that a ≥ 3 comorbidity burden has a significant impact on the complications or need for additional surgery in our elderly spinal deformity surgery population.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult spinal deformity (ASD) affects approximately 68% of the elderly population [1]. While only a small proportion of these patients are symptomatic, ASD can be quite debilitating. ASD has been associated with worse health related quality of life (HRQoL) scores when compared to more common chronic conditions such as chronic lung disease, congestive heart failure, diabetes, and ischemic heart disease [2]. Subsequently, as the population continues to age, the prevalence of ASD is increasing and the number of patients seeking treatment continues to grow.
An increasing amount of ASD surgery is being performed [3, 4]. McCarthy et al. reported a four-fold increase in ASD surgery performed on Medicare patients from 2000 to 2010 [3]. Sing et al. found that operative treatment of patients with ASD had increased 3.4 times between 2004 and 2011 in patients equal to or older than 60 years of age [4].
While deformity correction has been shown to result in substantial improvements in quality of life, it comes with the cost of significant morbidity. Several studies have shown that increasing age is associated with an increasing complication rates in adult spine surgery [5,6,7,8]. Despite this, there are several studies that show outcomes can be equivalent in the elderly after ASD surgery [9,10,11]. However, these latter studies have oft set cut-off values of > 65 or > 75 which generalizes outcomes to a larger cluster and limits assessment of outcomes in different age groups within the “elderly” population. Consequently, our goal was to offer a more specific comparative analysis within the elderly population i.e. “young” elderly vs “old” elderly. Therefore, we (1) compared outcomes of patients undergoing ASD surgery at age 65–74.9 versus greater than 75 years of age and (2) evaluated the effect of comorbidity burden on the rates of perioperative complications and need for reoperation in these populations.
Materials and methods
This is a retrospective study utilizing a single surgical practice’s prospectively collected database. Patient data was queried from 2002 to 2016. All patients were operated on by two surgeons with fellowship training in complex spinal deformity. Inclusion criteria for the study were all patients ≥ 65 years of age that underwent thoracolumbar deformity correction involving ≥ four levels with minimum 2-year follow-up. Exclusion criteria included patients < 65 years old, surgery for trauma or tumor, and surgery not specifically to address deformity correction (infection, non-union, adjacent segment degeneration). 176 patients met the final criteria. These 176 patients were then divided into cohorts based on age. 130 patients fell within the 65–74.9-year-old age group. 46 patients fell within the 75 years and older age group.
All patient demographic information was collected. All patient comorbidities were additionally noted. Comorbidity burden was calculated utilizing the Charlson Comorbidity Index (CCI). Radiographic parameters including thoracic kyphosis, lumbar lordosis (LL), pelvic tilt, pelvic incidence (PI), sagittal vertical axis (SVA), and coronal balance were measured preoperatively, one year postoperatively, and at two years postoperatively, and at latest follow-up. Complications are tracked by reviewing hospitalization and clinical records of each patient by dedicated research assistants. The full list of complications tracked is extensive and includes variables commonly tracked by often papers cited and the now defunct Spinal Deformity Study Group [14,15,16]. However, in the interest of brevity, many of these were condensed or omitted if not encountered in this study population. PI-LL was additionally calculated for preoperative and post-operative values. The Numeric Rating Scale (NRS) and Oswestry Disability Index (ODI) were collected preoperatively, at 1year, at 2years, and at latest follow-up.
SPSS v24 (IBM Inc., Chicago, IL) statistical software package was used for all analyses. Descriptive statistics were calculated with standard deviations and ranges. Patient characteristics, for both groups were analyzed with the use of Chi square and student t tests. A Chi square test was used for categorical variables, and an independent student t test was used to assess continuous variables. A p < 0.05 was set as our measure of statistical significance.
Results
Patient baseline characteristics
Demographic differences between the two groups are presented in Table 1. The overall mean age of the study population was 72.2 years old (range: 65 to 85). The mean age for the younger group was 70.0 and was 78.5 years for the eldest group (p = 0.001). The 65–74.9 age group had an average BMI of 27.3 whereas the 75 years and older age group had a mean BMI of 24.6 (p = 0.003). There were 102 (78.5%) females and 29 (63.0%) females in the younger and older age groups respectively (p = 0.049). Tobacco use, surgical diagnoses, and surgical characteristics such as length of fusion, previous spine surgery, and type of previous spine surgery were not different amongst the two groups. The mean follow-up was 69.1 months (25–186 mo).
Comorbidities for each group are demonstrated in Table 2. In the 65–74.9 age group, there were 119 (91.5%) patients with two or less comorbidities and 11 (8.5%) patients with three or more comorbidities. In the 75 years and greater age group there were 42 (91.3%) patients with two or less comorbidities and 4 (8.7%) patients with three or more comorbidities. There was no statistical significance in comorbidity burden between groups (p = 0.961).
Radiographic parameters
All pre-operative and postoperative parameters are presented in Table 3. Both groups had improvements in their radiographic parameters when compared to pre-operative measures. These latter differences were maintained at 2 years post-operatively. There were no statistically significant differences between the preoperative and 2-year postoperative parameters between the age groups.
Patient reported outcome measures
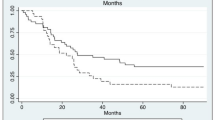
There was no difference in preoperative NRS and ODI scores between the two age groups (p = 0.055 and p = 0.162 respectively). The 2-year scores were also no different between the two groups (p = 0.307 and p = 0.311, respectively). Similarly, when comparing age groups, no difference in NRS scores were noted at 2 years (65–74.9: 2.6, ≥ 75: 2.5, p = 0.608); Fig. 1. Both age groups had a 15.4 improvement in ODI scores at 2-years postop when compared to pre-op scores (p = 0.608); Fig. 2. Within both groups, post-op improvements in NRS and ODI scores were statistically significant.
Clinical complications and need for revision surgery
Complications are listed in Table 4. The overall complication rate in our study was 51.7%. The 65–74.9 age group had an overall complication rate of 48.5% (63 patients) whereas the ≥ 75 group had a complication rate of 60.9% (28 patients) but this was not found to be statistically significant. There were no differences between the two age groups when isolating specific complications. All revision surgeries that were required were spine-related or surgery related. See Table 4 for specifics.
In the 65–74.9 age group, 47.9% with 0–2 comorbidities had a complication whereas 54.5% with ≥ 3 comorbidities had a complication. Additionally, 37.8% of these patients with 0–2 comorbidities required additional surgery compared to 45.5% with ≥ 3 comorbidities. None of these differences met statistical significance.
In the ≥ 75 group, 61.9% with 0–2 comorbidities had a complication whereas 50.0% with ≥ 3 comorbidities had a complication. Furthermore, 38.1% with 0–2 comorbidities required additional surgery compared to 50.0% with ≥ 3 comorbidities. None of these differences met statistical significance.
Discussion
In patients with severe disability and symptoms secondary to their spinal deformity, surgical intervention may be an option to help alleviate some of the disease burden [12]. Bridwell et al. found that surgery provided better outcomes for ASD patients over non-operative treatment when comparing quality of life measures at two years [13]. Research focused on elderly patients specifically found that ASD surgery in 65 years and older patients resulted in less pain and better HRQoL scores when compared to the non-operative cohort [14]. Sciubba et al. reported an improvement in HRQoL measures in patients older than 75 years of age with ASD that underwent surgical reconstruction compared to those treated non-operatively [15].
Though ASD surgery has been shown by many studies to improve outcomes in patients afflicted with severe deformity and symptoms, deformity surgery itself is associated with a high complication rate regardless of age. Sciubba et al. analyzed complication rates for ASD surgery and found an overall rate of 55%, with 18.5% considered as major perioperative complications. Their study had an average of 3.5 year follow-up with an average surgical age of 53.3 years old [16]. Our results showed a 51.7% complication rate which is similar to Sciubba et al. complication rate of 55%. Our study had an average age of 72.2 though, whereas Sciubba et al. study had an average age of 53.3. We did not further extrapolate the complications into minor and major within our study. Jain et al. found a similar 18.1% major medical perioperative complication nearly identical to Sciubba et al. [17]. Soroceanu et al. reported that ~ 27% of patient’s will have at least one complication perioperatively after ASD surgery when including adults of all ages [18]. Both Soroceanu et al. and our study did find a trend towards increasing complication rates with increasing age, but the trend did not meet statistical significance. We did have a higher overall complication rate when compared to Soroceanu et al. but our average age was also much higher than their average of 56.8 years old.
Drazin et al. performed a literature review of 22 different articles on ASD surgery in elderly patients aged 60 years and older with a mean follow-up of three years. They found an overall 38% complication rate with a mean age of 74.2 years [19]. Though our overall complication rate of 51.7% is higher than Drazin et al. study, we also had a much longer mean follow-up of 69.1 months. Lonergan et al. reported a major complication rate of 35% in a patient population ≥ 70 years old with an average age of 76.6 that underwent ASD surgery but found a 95% overall complication rate [20]. The Lonergan et al. study did have a limitation of a study population of only 20 which was much lower than our 176 patients.
One would likely expect that there would be an increased complication rate in the elderly population undergoing ASD surgery, but there is no consensus in the current literature. Worley et al. showed that elderly patients had a higher risk of perioperative complications and mortality compared to patients younger than 65 years old [5]. Another study found a statistically significant trend of increasing complications with increasing decades of life [6]. Drazin et al. reported that a 75 year and older group undergoing ASD surgery had a higher rate of discharge to skilled nursing facilities and higher readmission rates when compared to a 66-74.9 year old age group [7]. Though there was a slight increase in 30 day complication rates in the older population (26.6% vs 21%), this was not statistically significant. Within our study population we did find a trend for increasing complications in the ≥ 75 year old age group but this did not reach statistical significance either. Several other studies have not found an association of increasing complications with age in ASD surgery [11, 21, 22]. Cho et al. did report a non-statistically significant tendency for early complications in patients older than 65 [22]. Sansur et al. also did not find a higher complication rate when comparing groups below or above 65 years of age [21]. Therefore, our results are consistent with several other studies indicating there is not a significant difference between complication rates in the elderly population undergoing ASD surgery.
When discussing ASD surgery, the need for revision surgery should be considered and patients should also be counseled regarding this possibility. Scheer et al. reported a revision operation rate of 17% after ASD surgery with an average of only 1.6 years follow-up in the study population [23]. Another study by Scheer et al. found a slightly higher reoperation rate of 18.8% within two years [24]. In our study, 45 patients (34.6%) in the 65-74.9 year old age group required additional surgery compared to 18 patients (39.1%) in the 75 year and older group. Of these surgeries, however, 26.9% (65–74.9) and 30.4% (> 75) were revision fusions or extensions of fusion. Although our study had higher rates of revision surgeries compared to the two above mentioned Scheer et al. studies, we also had a much longer mean follow-up of 69.1 months. Given that the Scheer et al. studies mentioned above had a mean follow-up of 1.6 and 2 years respectively, postoperative complications such as rod fracture, non-union, proximal junctional kyphosis, and other implant complications may have not had time to present and become an issue within that short follow-up time.
Despite the potential elevated risk for complications in ASD surgery performed on the elderly, Smith et al. reported that elderly patients may do as well or better than younger patients in terms of outcomes [9]. Crawford et al. stated that elderly patients with considerable spinal deformity can obtain as much benefit from ASD surgery when compared to their non-elderly counterparts when comparing outcomes measures between the two groups [10]. Our results further expand this discussion as we found that a ≥ 75-year age group had as good of outcomes as their 65-74.9 year old counterparts. Scheer et al. reported in their study that even though patients 65 years and older had a higher complication rate, the elderly patients had a shorter and improved recovery period when compared to their younger cohorts [25]. In a study by Hassanzadeh et al., elderly patients (≥ 65 years old) achieved equivalent outcomes without an increase in complications compared to a 40-64 year old age group that underwent revision ASD surgery [11]. Lonergan et al. concluded that age alone should not be a deciding factor against surgery for ASD in patients in their 80′s [20]. Our findings echo these latter conclusions.
Drazin et al. reported a mean improvement of ODI by 24.1 and improvement in the VAS of 5.2 in their elderly ASD surgery population [19]. Drazin et al. study results are even more drastic than our ASD surgery study population where we found a 15.4 improvement in the ODI in both of our age groups. We had a 2.6 and 2.5 improvement in the NRS scores in the 65-74.9 and 75 and greater age groups respectively. Our study population had lower preoperative NRS and ODI scores compared to Drazin et al. study. These lower scores in our study population indicate that our patients had less preoperative disability and may explain why we did not see as significant of improvement in our outcomes scores when compared to their study. The 15.4 improvement in ODI seen in our study is more consistent with the results seen in Smith et al. study where they reported a 19 point improvement in ODI within the 65-85 year age group [9]. Importantly, all patients in our study had improvements in their sagittal parameters that were maintained at their last radiographic follow-up.
There are some notable limitations with our study. First, although data were pulled from a prospectively collected database, this was nonetheless, a retrospective study. In this context, as we do not routinely follow patients annually past the 2-year follow-up, we were forced to limit our radiographic and outcome measure analyses to 2-years—a substantial proportion of datapoints were simply not available beyond this and would have impeded any meaningful analysis. Further, this consequently resulted in a wide range in follow-up. However, we would argue that it would be unscientific to include patients that were otherwise doing well and simply chose not to follow-up beyond the 2-year mark out of convenience in a separate “lost to follow-up” category. This of course again, is a limitation of a retrospective study, where a strict longer-term follow-up schedule is not mandated as might be in a prospective study. Further, a relatively small sample size may have limited our ability to establish statistical significance in our comparisons. Finally, there may be concern for surgeon selection bias in this particular patient population. However, we would argue that this selection bias should be universally exercised in this patient population and that deformity correction be strictly limited to those that are deemed medically fit for surgery and have failed extensive conservative treatment modalities. In spite of these limitations, our study is consistent with other literature to support that elderly patients can have similar outcomes with no difference in complications. Though our sample size may not be as large as those queried from large databases, our 176 patient population is larger than many other studies on outcomes and complications in elderly ASD surgery and benefits from drawing from only 2 surgeons at a single center [11, 15, 20, 22, 24].
Conclusion
In conclusion, analysis of our study population indicates that there is not a statistically significant difference between the outcomes and complications of deformity surgery in patients 75 years and older when compared to a younger elderly population in the 65-74.9 age range. It also does not appear that a higher comorbidity burden has a significant impact on the complications or the need for additional surgery in our elderly spinal deformity surgery population. Therefore, we believe that ASD surgery in patients 75 years and older is an option in spite of their chronological age, but only in appropriately chosen patients with severe disability due to their deformity.
References
Schwab F, Dubey A, Gamez L, El Fegoun AB, Hwang K, Pagala M et al (2005) Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 30:1082–1085
Pellisé F, Vila-Casademunt A, Ferrer M, Domingo-Sàbat M, Bagó J, Pérez-Grueso FJS et al (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24:3–11. https://doi.org/10.1007/s00586-014-3542-1
McCarthy I, Hostin R, O’Brien M, Saigal R, Ames CP (2013) Health economic analysis of adult deformity surgery. Neurosurg Clin N Am 24:293–304. https://doi.org/10.1016/j.nec.2012.12.005
Sing DC, Berven SH, Burch S, Metz LN (2017) Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J 17:627–635. https://doi.org/10.1016/j.spinee.2016.11.005
Worley N, Marascalchi B, Jalai CM, Yang S, Diebo B, Vira S et al (2016) Predictors of inpatient morbidity and mortality in adult spinal deformity surgery. Eur Spine J 25:819–827. https://doi.org/10.1007/s00586-015-4104-x
Shaw R, Skovrlj B, Cho SK (2016) Association between age and complications in adult scoliosis surgery: an analysis of the scoliosis research society morbidity and mortality database. Spine 41:508–514. https://doi.org/10.1097/BRS.0000000000001239
Drazin D, Al-Khouja L, Lagman C, Ugiliweneza B, Shweikeh F, Johnson JP et al (2016) Scoliosis surgery in the elderly: complications, readmissions, reoperations and mortality. J Clin Neurosci 34:158–161. https://doi.org/10.1016/j.jocn.2016.06.005
Carreon LY, Puno RM, Dimar JR, Glassman SD, Johnson JR (2003) Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 85-A:2089–2092
Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL et al (2011) Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine 36:817–824. https://doi.org/10.1097/BRS.0b013e3181e21783
Crawford CH, Carreon LY, Bridwell KH, Glassman SD (2012) Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 21:2165–2169. https://doi.org/10.1007/s00586-012-2310-3
Hassanzadeh H, Jain A, El Dafrawy MH, Ain MC, Skolasky RL, Kebaish KM (2013) Clinical results and functional outcomes in adult patients after revision surgery for spinal deformity correction: patients younger than 65 years versus 65 years and older. Spine Deform 1:371–376. https://doi.org/10.1016/j.jspd.2013.07.003
Youssef JA, Orndorff DO, Patty CA, Scott MA, Price HL, Hamlin LF et al (2013) Current status of adult spinal deformity. Global Spine J 3:51–62. https://doi.org/10.1055/s-0032-1326950
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP et al (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine 34:2171–2178. https://doi.org/10.1097/BRS.0b013e3181a8fdc8
Li G, Passias P, Kozanek M, Fu E, Wang S, Xia Q et al (2009) Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine 34:2165–2170. https://doi.org/10.1097/BRS.0b013e3181b3ff0c
Sciubba DM, Scheer JK, Yurter A, Smith JS, Lafage V, Klineberg E et al (2016) Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J 25:2433–2441. https://doi.org/10.1007/s00586-015-3759-7
Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR et al (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform 3:575–594. https://doi.org/10.1016/j.jspd.2015.04.005
Jain A, Hassanzadeh H, Puvanesarajah V, Klineberg EO, Sciubba DM, Kelly MP et al (2017) Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine 27:534–539. https://doi.org/10.3171/2017.3.SPINE161011
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI et al (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine 41:1718–1723. https://doi.org/10.1097/BRS.0000000000001636
Drazin D, Shirzadi A, Rosner J, Eboli P, Safee M, Baron EM et al (2011) Complications and outcomes after spinal deformity surgery in the elderly: review of the existing literature and future directions. Neurosurg Focus 31:E3. https://doi.org/10.3171/2011.7.FOCUS11145
Lonergan T, Place H, Taylor P (2016) Acute complications after adult spinal deformity surgery in patients aged 70 years and older. Clin Spine Surg 29:314–317. https://doi.org/10.1097/BSD.0b013e3182764a23
Sansur CA, Smith JS, Coe JD, Glassman SD, Berven SH, Polly DW et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine 36:E593–E597. https://doi.org/10.1097/BRS.0b013e3182059bfd
Cho K-J, Suk S-I, Park S-R, Kim J-H, Kim S-S, Choi W-K et al (2007) Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine 32:2232–2237. https://doi.org/10.1097/BRS.0b013e31814b2d3c
Scheer JK, Tang JA, Smith JS, Klineberg E, Hart RA, Mundis GM et al (2013) Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database: clinical article. J Neurosurg Spine 19:464–470. https://doi.org/10.3171/2013.7.SPINE12901
Scheer JK, Mundis GM, Klineberg E, Hart RA, Deviren V, Burton DC et al (2016) Recovery following adult spinal deformity surgery: the effect of complications and reoperation in 149 patients with 2-year follow-up. Eur Spine J 25:2612–2621. https://doi.org/10.1007/s00586-015-3787-3
Scheer JK, Mundis GM, Klineberg E, Hart RA, Deviren V, Nguyen S et al (2015) Postoperative recovery after adult spinal deformity surgery: comparative analysis of age in 149 patients during 2-year follow-up. Spine 40:1505–1515. https://doi.org/10.1097/BRS.0000000000001062
Funding
This study was self-funded. No corporate or industry funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
ZL, DD, AC, DC, JR, MC: conception/design, ZL, AC: data collection, AC: Data Analysis and interpretation/stats, ZL, DD, AC, DC, JR, MC: Drafting of manuscript, ZL, DD, AC, DC, JR, MC: Manuscript Revision, DC, JR, MC: Supervision/administration, ZL, DD, AC, DC, JR, MC: Approval of Final manuscript
Corresponding author
Ethics declarations
Conflict of interest
MSC reports consulting fees from Orthofix, Stryker, Depuy, SpineWave, and BK; DGC reports royalties from Spinewave and Medtronic, stock ownership in Handel, and consulting fees from U&I and SpineWave; all other others have no relevant financial disclosures.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Sonoran Spine Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. IRB approval was granted at Sonoran Spine Research and Education Foundation.
Informed consent
Informed consent was obtained from patients prior to inclusion in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lovato, Z.R., Deckey, D.G., Chung, A.S. et al. Adult spine deformity surgery in elderly patients: are outcomes worse in patients 75 years and older?. Spine Deform 8, 1353–1359 (2020). https://doi.org/10.1007/s43390-020-00169-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00169-3