Abstract
Background
Obesity, insulin resistance, and hyperandrogenemia are commonly seen in women with polycystic ovary syndrome (PCOS), and these three conditions form a vicious cycle leading to reproductive and metabolic abnormalities. Metformin improves the symptoms of PCOS by increasing insulin sensitivity but is not therapeutically optimal. Recent studies have reported that sodium-glucose co-transporter protein receptor inhibitors improve insulin resistance and reduce the weight of patients with PCOS. We performed a meta-analysis to assess the influence of sodium-glucose co-transporter protein-2 (SGLT2) inhibitors on anthropometric, glycolipid metabolism and reproductive outcomes after therapy of overweight/obese women with PCOS.
Methods
We searched the relevant literature published up to April 2023. Information on the effect of SGLT2 inhibitors on overweight/obese patients with PCOS was extracted independently by two reviewers. Review Manager 5.3 was used for meta-analysis.
Results
Five randomized controlled trials that met our criteria were retrieved. Our meta-analysis demonstrated that in overweight/obese patients with PCOS, SGLT2 inhibitors treatment was significantly superior to metformin treatment in terms of reducing body weight (P = 0.02, I2 = 36%), decreasing dehydroepiandrosterone sulfate concentrations [SMD = -0.42, 95% CI (-0.76, -0.07), I2 = 22%, P = 0.02], and reducing the incidence of nausea [RR = 0.35, 95% CI (0.21, 0.60), I2 = 71%, P = 0.0001].
Conclusions
SGLT2 inhibitors are a possible alternative therapy for treating overweight/obese women with PCOS who do not respond favorably to metformin treatment. However, further large randomized controlled trials and cost-effectiveness analyses are warranted to guide the implementation of SGLT2 inhibitors treatment in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycystic ovary syndrome (PCOS) is a complex reproductive endocrine disorder that affects 4%–21% of women of reproductive age [1]. Its etiology is not fully understood and involves genetic, epigenetic, endocrine, metabolic and environmental factors. PCOS is characterized by hyperandrogenaemia, sporadic ovulation or anovulation and polycystic ovarian changes [2]. A diagnosis of PCOS is established if a patient has at least two of these three symptoms, and other diseases have been excluded. Compared with healthy patients, PCOS patients have a higher risk of infertility, obesity, type 2 diabetes mellitus, hypertension, cardiovascular disease, non-alcoholic fatty liver disease and endometrial cancer [3,4,5,6].
Obesity is present in 30%–60% of PCOS patients, with approximately 95% of such patients experiencing insulin resistance [5, 7, 8]. Insulin resistance can lead to abnormal glucose and lipid metabolism [9], resulting in hyperlipidemia due to low serum concentrations of high-density lipoprotein cholesterol (HDL-C) [10]. Moreover, hyperinsulinaemia reduces the circulating concentrations of sex hormone-binding globulin (SHBG) and increases free testosterone (FT) concentrations. This hormonal imbalance can hinder follicular maturation, leading to irregular menstruation and infertility [11].
Obesity and insulin resistance are major contributors to comorbidities in patients with PCOS. Antidiabetic drugs have been found to effectively enhance insulin activation, leading to weight reduction and alleviation of PCOS symptoms. Among these drugs, metformin is recommended for female patients at a high risk of obesity and metabolic problems [12, 13], and it also alleviates menstrual cycle disorders, anovulation and hyperandrogenaemia [14, 15]. However, metformin requires high doses and is slow acting [16]. There remain deficiencies in the treatment of metabolic abnormalities and management of cardiovascular complications in PCOS patients.
Sodium-glucose co-transporter protein-2 (SGLT2) inhibitors are a novel class of hypoglycaemic agent that have shown clinical efficacy beyond their original indication, extending to diseases such as heart failure and chronic kidney disease [17]. SGLT2 inhibitors primarily block SGLT2 receptors and thereby inhibit glucose and sodium reabsorption in the kidney’s proximal tubules. This enables the excretion of excess glucose in the urine and leads to a reduction in blood glucose concentrations. Additionally, SGLT2 inhibitors decrease gluconeogenesis in the liver, enhance insulin sensitivity and release from pancreatic β-cells [18], reduce fat mass and blood pressure [19], mitigate oxidative damage and inflammation [20] and offer cardiovascular protection [21].
SGLT2 inhibitors have also been investigated in animal and clinical trials for the treatment of PCOS. Although some trials have shown effectiveness, there is a lack of large-scale clinical studies and thus evidence to validate the safety and efficacy of SGLT2 inhibitors for PCOS. Furthermore, they have not been approved or recommended by public consensus or guidelines. To address this gap, we conducted a meta-analysis to assess the impact of SGLT2 inhibitors on glucose metabolism, lipid metabolism and reproductive hormones in PCOS patients, aiming to provide valuable insights for clinical treatment.
Methods
Search Strategy
On 15 April 2023, we searched the literature on PubMed, Embase, the Cochrane Library, the Web of Science, Google Scholar, Scopus, Ovid, the China National Knowledge Infrastructure, the Wanfang, and the Weipu databases without date or language restrictions. Full-text searches were conducted using two main sets of terms: ‘Polycystic Ovary Syndrome’ OR ‘polycystic ovarian syndrome’ OR ‘polycystic ovary’ OR ‘PCOS’ OR ‘polycystic ovary disease’ OR ‘polycystic ovarian disease’ OR ‘ovary polycystic disease’ OR ‘Ovary Syndrome, Polycystic’ OR ‘Syndrome, Polycystic Ovary’ OR ‘Ovarian Syndrome, Polycystic’ OR ‘Stein Leventhal Syndrome’ OR ‘Stein-Leventhal Syndrome’ OR ‘Syndrome, Stein-Leventhal’ OR ‘Sclerocystic Ovarian Degeneration’ OR ‘Ovarian Degeneration, Sclerocystic’ OR ‘Sclerocystic Ovarian Syndrome’ OR ‘Sclerocystic Ovaries’ OR ‘Ovary, Sclerocystic’ OR ‘Sclerocystic Ovary’, ‘Sodium-Glucose Transporter 2 Inhibitors’ OR ‘Sodium Glucose Transporter 2 inhibitors’ OR ‘Sodium-Glucose Transporter 2 inhibitor’ OR ‘Sodium Glucose Transporter 2 inhibitor’ OR ‘SGLT2 inhibitors’ OR ‘SGLT 2 inhibitors’ OR ‘SGLT-2 inhibitors’ OR ‘SGLT2 inhibitor’ OR ‘Inhibitor, SGLT2’ OR ‘Inhibitor, SGLT-2’ OR ‘Gliflozins’ OR ‘Gliflozin’ OR ‘SGLT-2 inhibitor’ OR ‘SGLT 2 inhibitor’ OR ‘SGLT2 inhibitor’ OR ‘sodium glucose cotransporter 2 inhibitors’ OR ‘sodium-glucose cotransporter 2 inhibitors’ OR ‘sodium glucose cotransporter 2 inhibitors’ OR ‘sodium-glucose cotransporter 2 inhibitor’ OR ‘sodium glucose cotransporter 2 inhibitor’ OR ‘dapagliflozin’ OR ‘licogliflozin’ OR ‘canagliflozin’ OR ‘empagliflozin’ OR ‘sotagliflozin’ OR ‘janagliflozin’ OR ‘luseogliflozin’ OR ‘ertugliflozin’ OR ‘tofogliflozin’ OR ‘ipragliflozin’ OR ‘mizagliflozin’ OR ‘remogliflozin’ OR ‘sergliflozin’. The two sets of search terms were linked using ‘AND’. We also searched the reference lists of the extracted articles to identify additional relevant articles.
Inclusion Criteria
The literature included in the meta-analysis comprised randomized controlled trials that were neither blinded nor had language restrictions. The targeted patients were women aged 18–45 who had been diagnosed with PCOS according to the Rotterdam criteria set by the American Society for Reproductive Medicine (ASRM) [22], the PCOS criteria set by the National Institute of Child Health and Human Development (NICHD), or the PCOS criteria of the androgen excess and PCOS Society [23]. In light of the limited available data, we included a control group in our study, and the study conducted by Elkind-Hirsch et al. [24] utilized other anti-hyperglycemic drug treatments as the control group. The primary outcome variables analysed in the studies were weight, body mass index (BMI), waist circumference (WC), fasting blood glucose (FBG), fasting insulin (FINS), homeostasis model assessment of insulin resistance (HOMA-IR), total cholesterol (TC), triglycerides (TG), HDL-C, low-density lipoprotein cholesterol (LDL-C), total testosterone (TT), androstenedione (AD), dehydroepiandrosterone sulfate (DHEAS), free androgen index (FAI), and SHBG.
Exclusion Criteria
We excluded studies that included women with a differential diagnosis of Cushing’s disease, hyperprolactinaemia, 21-hydroxylase deficiency, or androgen-secreting tumours. Additionally, we excluded studies that included women who were pregnant or planning to become pregnant or using hormonal contraceptives or steroids, and studies that did not report efficacy measures or had missing data.
Study Selection
We exported each database search to EndNote X9 to check for duplicates. Two researchers (ZLL and WZ) independently screened and cross-checked the results by reviewing abstracts and full texts. Studies that did not meet the inclusion criteria were excluded. Any disagreements were resolved through discussion and consensus.
Data Extraction
Based on the above criteria, after identifying studies for inclusion in the analysis, data extraction was performed by two researchers (ZLL and WZ) using a standardised data extraction form, and any discrepancies were resolved by discussion to consensus. Data extracted from each study were the trial name, author details, year of publication, study location, mean age of participants, drugs used in the experimental and control groups (including the type and dose), number of participants in each treatment group, diagnostic criteria for PCOS, and treatment duration and outcomes.
Quality Assessment
Two investigators used the Cochrane Collaboration Tool to independently evaluate the risk of bias in randomised trials. The assessment was conducted using Review Manager 5.3 software. Any discrepancies between the investigators were resolved by discussion to consensus.
Statistical Analysis
Due to the limited availability of data on the analysed themes, it was difficult to determine the most suitable statistical methods for reporting effect sizes. As a result, we adjusted our criteria for the control group. The study by Elkind-Hirsch et al. [24] included several groups, and we selected the exenatide treatment group as the control group. Exenatide is a glucagon-like peptide-1 receptor agonist (GLP1-RA) that reduces obesity and decreases insulin resistance in patients with PCOS [25]. Exenatide is as effective and safe as metformin for the treatment of PCOS [26, 27], and thus exenatide treatment was included to increase the population and thus the reliability of the effect size.
We used Review Manager 5.3 software for data analysis and to generate forest plots. Outcome measures that were continuous data are presented as standardised mean differences (SMDs). We used the I2 test to evaluate statistical heterogeneity and regarded an I2 greater than 50% as indicating statistical significance. A random-effects model was used for all analyses, as it yields more conservative estimates. We calculated the corresponding 95% confidence intervals (CIs) and P values, and considered P values less than 0.05 as indicating statistical significance.
A main obstacle in using methodological harmonisation for our analysis was that the included studies used different reporting techniques. Therefore, we extracted the mean difference and standard deviation (SD) of each outcome measure from the included studies before and after drug administration, and compared these for each treatment group. The change in SD was calculated as follows:
where R = 0.5. In addition, the outcome indices in the studies by Jiaqi [28] and Meili [29] were reported with 95% CIs, so we used the following formula for the calculation of SD: SD = √N × (upper confidence interval limit − lower confidence interval limit)/3.92
Sensitivity and Subgroup Analyses
As the control group in one study comprised active controls (other anti-hyperglycaemic drugs), there was a possibility that the effect size of the outcome of interest would be underestimated and thus generate bias. To mitigate this bias, subgroup analyses were conducted by separating the active controls. Additionally, sensitivity analyses were performed by systematically excluding each study to evaluate whether this caused any variations in the combined effect size.
Results
Study Characteristics and Quality Evaluation
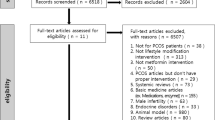
This article is designed according to the PRISMA checklist (S1). A total of 896 articles were obtained from ten databases using first-level and second-level filters based on the specified inclusion and exclusion criteria. After excluding articles with irrelevant titles and abstracts, 10 articles remained. Subsequently, after a thorough full-text examination of the 10 articles, five articles were found to meet the criteria [24, 28,29,30,31]. Figure 1 illustrates the search strategy used to select the articles.
Table 1 presents the characteristics of the included articles, all of which reported randomised controlled trials. Two trials compared an SGLT2 inhibitor group with a metformin group, two trials compared an experimental group receiving a combination of an SGLT2 inhibitor and metformin with a control group receiving only metformin, and one trial compared both an SGLT2 inhibitor group and an SGLT2 inhibitor + metformin group with an exenatide group, which served as a control group Table 2.
The trials included in the systematic review were assessed for the risk of bias, as depicted in Fig. 2. One of trials was deemed to have a high risk of selection bias and reporting bias. In the other four trials, a computer-generated randomised list was used for random sequence generation, as is appropriate. However, none of the three trials provided detailed information regarding the allocation concealment method, resulting in an uncertain risk of selection bias. Four trials were open-label, but the objective nature of the endpoint measures led to a lower risk perception than might otherwise have been the case.
Effect on Weight/BMI/WC
Weight and BMI were reported in all five trials, whereas WC was reported in three trials. A meta-analysis of the trials indicates that treatment with SGLT2 inhibitors yielded reductions in body weight [SMD = -0.06, 95% CI (-0.48, 0.36), I2 = 74%, P = 0.78] (Fig. 3a), BMI [SMD = -0.01, 95% CI (-0.38, 0.35), I2 = 64%, P = 0.94] (Fig. 3b), and WC [SMD = -0.23, 95% CI (-0.56, 0.10), I2 = 32%, P = 0.17] (Fig. 3c) comparable with the control treatments. These differences were not statistically significant. Due to the substantial heterogeneity in weight (P = 0.78, I2 = 74%) and BMI (P = 0.95, I2 = 64%), sensitivity analyses were conducted to evaluate the stability of the data. In a subgroup analysis that excluded the exenatide active control group, the results demonstrated that SGLT2 inhibitor treatment was significantly more effective than metformin treatment in reducing body weight [SMD = -0.35, 95% CI (-0.65, 0.05), I2 = 36%, P = 0.02] (Fig. [8a). Although changes in heterogeneity were observed in the results for BMI (P = 0.16, I2 = 43%), there were no significant variations in the effect size of the results.
Effects on Glucose Metabolism
All of the five trials reported FBG concentration and HOMA-IR, and four articles also reported FINS. However, no statistically significant differences were observed in the changes in FBG [SMD = -0.21, 95% CI (-0.46, 0.05), I2 = 32%, P = 0.12] (Fig. 4a), FINS [SMD = -0.91, 95% CI (-2.40, 0.59), I2 = 97%, P = 0.24] (Fig. 4b), and HOMA-IR [SMD = -0.76, 95% CI (-1.65, 0.14), I2 = 94%, P = 0.10] (Fig. 4c) between the experimental group and the control group. The SGLT2 inhibitor group exhibited comparable effects to the control group in terms of improvements in glucose metabolism. Notably, significant heterogeneity was observed in the results for FINS (P = 0.24, I2 = 97%) and HOMA-IR (P = 0.10, I2 = 94%). Thus, a sensitivity analysis was performed by excluding the study by Zeng et al. and revealed remarkable changes in the heterogeneity in the results for FINS (P = 0.13, I2 = 0%) and HOMA-IR (P = 0.07, I2 = 62%). However, the effect size of the results remained unaffected. This heterogeneity may be attributable to the substantial difference in the sample size of the retrospectively conducted Chinese trial compared with the other included trials, leading to significant heterogeneity in the results. Furthermore, no significant differences in glucose metabolism outcomes were found when comparing SGLT2 inhibitors to metformin in the active control group after excluding them for subgroup analysis.
Effects on Lipid Metabolism
TC, TG, and LDL-C concentrations were reported by all five trials, while HDL-C concentrations were reported by four trials. However, no significant differences were observed in the changes in TC [SMD = 0.08, 95% CI (-0.32, 0.48), I2 = 71%, P = 0.70] (Fig. 5a), TG [SMD = -0.29, 95% CI (-0.75, 0.17), I2 = 78%, P = 0.22] (Fig. 5b), HDL-C [SMD = 0.28, 95% CI (-0.42, 0.97), I2 = 89%, P = 0.44] (Fig. 5c), and LDL-C [SMD = 0.11, 95% CI (-0.17, 0.39), I2 = 42%, P = 0.44] (Fig. 5d) concentrations between the experimental group and the control group. Significant heterogeneity was found in the results for TC (P = 0.70, I2 = 71%), TG (P = 0.22, I2 = 78%), and HDL-C (P = 0.44, I2 = 89%) concentrations. A sensitivity analysis conducted by excluding the study by Zeng et al. revealed changes in the heterogeneity in the results for TC (P = 0.07, I2 = 0%), TG (P = 0.44, I2 = 0%), and HDL-C (P = 0.88, I2 = 0%) concentrations, but there was no significant change in the effect size. Subgroup analysis also yielded non-significant changes in lipid metabolism outcomes.
Effects on Reproduction
TT concentrations were measured in four included trials, while AD and SHBG concentrations were reported in three trials, DHEAS concentrations were estimated in three trials, and FAI% was determined in three trials. Compared with the control group, the SGLT2 inhibitor group showed no improvement in TT concentrations [SMD = -0.10, 95% CI (-0.37, 0.17), I2 = 73%, P = 0.47] (Fig. 6a), FAI% [SMD = 0.02, 95% CI (-0.66, 0.70), I2 = 78%, P = 0.96] (Fig. 6c), SHBG concentrations [SMD = 0.05, 95% CI (-0.28, 0.39), I2 = 0%, P = 0.75] (Fig. 6d), or AD concentrations [SMD = -0.19, 95% CI (-0.52, 0.14), I2 = 0%, P = 0.27] (Fig. 6e), but a significant improvement in DHEAS concentrations [SMD = -0.42, 95% CI (-0.76, -0.07), I2 = 22%, P = 0.02] (Fig. 6b). Statistical heterogeneity was observed in the results for TT concentrations (P = 0.47, I2 = 73%) and FAI% (P = 0.96, I2 = 78%). A sensitivity analysis excluding the study by Elkind-Hirsch et al. revealed a change in the heterogeneity in the results for FAI% (P = 0.49, I2 = 24%). However, a sensitivity analysis for TT concentrations did not show any significant changes in heterogeneity after excluding each study individually. Interestingly, in a subgroup analysis excluding the active control group, DHEAS concentrations after SGLT2 inhibitor treatment [SMD = -0.58, 95% CI (-0.99, -0.18), I2 = 0%, P = 0.005] (Figs. 7 and 8b) remained significantly improved compared with metformin treatment.
Adverse Reactions
Only three trials reported adverse reactions. These were primarily gastrointestinal symptoms, such as nausea, diarrhoea, loss of appetite, vomiting, and abdominal pain. Among these symptoms, nausea was the most common, and its incidence was significantly lower in the SGLT2 inhibitors group than in the control group [RR = 0.35, 95% CI (0.21, 0.60), I2 = 71%, P = 0.0001] (Fig. 7). Additionally, the SGLT2 inhibitors group experienced fewer adverse events than the control group. However, the limited number of included trials and the small sample size in our analysis restrict generalisation of the side effects of SGLT2 inhibitors treatment for PCOS. Future studies with a larger number of patients are necessary to provide a more definitive understanding of these effects.
Discussion
The precise aetiology of PCOS is unknown, and current treatment is based on clinical symptoms and experience. Weight loss is considered an effective treatment for overweight or insulin-resistant patients with PCOS, but they usually show poor compliance, which is necessary for weight control and improvement of insulin resistance through medication. International evidence-based guidelines recommend the use of metformin for patients with PCOS [14]. SGLT2 inhibitors are a novel class of anti-hyperglycaemic drugs that target glucose homeostasis and insulin sensitivity in individuals with diabetes. Notably, numerous large-scale double-blind clinical trials and meta-analyses have demonstrated additional benefits of SGLT2 inhibitors in diabetic patients in terms of cardiovascular mortality [32], stroke occurrence [33] and renal protection [34]. Given the similarities between the key metabolic dysfunctions of PCOS and diabetes, and their shared characteristics, such as obesity, low-grade inflammation, metabolic abnormalities and increased cardiovascular risks [35, 36], it is reasonable to explore the potential benefits of SGLT2 inhibitors in PCOS patients and investigate any complementary mechanisms beyond the improvement of metabolic abnormalities. However, currently, there is insufficient good-quality evidence on the comparative effectiveness and safety of SGLT2 inhibitors versus metformin for PCOS treatment. Therefore, the objective of this meta-analysis was to examine the differences in clinical outcomes between PCOS patients treated with SGLT2 inhibitors or a combination of SGLT2 inhibitors and metformin and those treated with metformin alone.
This study analysed five randomised controlled trials, involving 401 women with PCOS, selected through a rigorous literature search and use of strict inclusion and exclusion criteria to identify high-quality literature for analysis. The meta-analysis results demonstrated that, after 12 to 24 weeks of treatment, the SGLT2 inhibitors group exhibited similar effects to the metformin control group in terms of decreased obesity and improved glucolipid metabolism. However, upon excluding the effect of exenatide from the study by Elkind-Hirsch et al., SGLT2 inhibitors were found to be significantly more effective than metformin in promoting weight loss (P = 0.02, I2 = 36%). This finding suggests that SGLT2 inhibitors therapy provides greater benefits than metformin in terms of reducing obesity symptoms in PCOS patients. Although obesity and insulin resistance are not considered diagnostic criteria for PCOS, they have been linked to various complications, such as type 2 diabetes, cardiovascular disease, infertility and miscarriage [37,38,39]. Moreover, studies conducted on animal models have shown that SGLT2 inhibitors can alleviate obesity symptoms in PCOS. For instance, Pruett et al. reported significant reductions in adiposity, plasma leptin concentrations and blood pressure after 3 weeks of empagliflozin treatment in a dihydrotestosterone-induced female rat model of PCOS [19]. Subsequently, Pruett’s team discovered that SGLT2 inhibitors improved mitochondrial function and decreased oxidative stress in white adiposity, contributing to a reduction in obesity symptoms in an animal model of PCOS [40]. Furthermore, a short-term trial involving obese patients demonstrated a 6% weight loss and an 80% decrease in insulin concentrations after 12 weeks of licogliflozin treatment [41]. In the treatment of female patients with PCOS, a randomised double-blind phase II trial of licogliflozin showed a 70% reduction in hyperinsulinaemia [42]. These findings from animal experiments and clinical studies align with the conclusions of this meta-analysis, supporting the notion that SGLT2 inhibitors can effectively alleviate obesity symptoms in overweight or obese patients with PCOS.
Additionally, this meta-analysis revealed that treatment with SGLT2 inhibitors improved reproductive hormone outcomes in PCOS patients. Specifically, a significant decrease in DHEAS concentrations [SMD = -0.42, 95% CI (-0.76, -0.07), I2 = 22%, P = 0.02] was observed in the SGLT2 inhibitors group relative to the metformin control group, indicating a superior benefit even after excluding the effect of exenatide. However, no significant differences were found in TT, SHBG, FAI, and AD concentrations between the two groups. DHEAS, a hormone made by the adrenal glands through sulfation of dehydroepiandrosterone (DHEA) [43], comprises 51%–73% of DHEAS and its metabolites, which are excreted predominantly through the kidneys [44]. The administration of SGLT2 inhibitors to PCOS patients reduced serum DHEAS concentrations by influencing renal permeability and increasing urinary glucose excretion. Furthermore, it was observed that SGLT2 inhibitors affected DHEAS excretion during PCOS treatment. Increased serum DHEAS concentrations occur in approximately 50% of PCOS patients [45, 46] and are indicative of the formation of androgen, the precursor of DHEAS, in the liver and peripheral tissues [47]. Hyperandrogenism is a prominent characteristic of PCOS, and hyperandrogenaemia contributes to adverse pregnancy outcomes and an increased risk of complications by negatively affecting endometrial tolerance and the developmental capacity of oocytes [48]. A prospective study found that women with PCOS who had hyperandrogenaemia experienced the risk of preterm delivery and preeclampsia [49]. In addition, hyperandrogenaemia, obesity and insulin resistance can interact to form a vicious cycle [50]. Obese patients often have increased insulin concentrations, which stimulate luteinising hormone-induced androgen production while inhibiting the hepatic synthesis of SHBG [51]. The surplus androgens in PCOS patients further contribute to the accumulation of abdominal fat deposition [52]. These alterations can disrupt ovulatory function and lead to menstrual irregularities [53]. Consequently, addressing these factors is crucial for alleviating the symptoms associated with PCOS. In a randomised, double-blind phase II trial of treatments for PCOS, licogliflozin treatment demonstrated significant reductions of up to 70% in hyperinsulinaemia, 19% in androgen concentrations, and 24% in DHEAS concentrations [42]. Similarly, Cai et al. reported a notable advantage over metformin (P = 0.013) where 12 weeks of canagliflozin treatment resulted in a 68.96 µg/dL decrease in DHEAS levels among patients with PCOS [29]. This decrease in DHEAS concentrations not only contributes to a reduction in androgen production but also breaks the vicious cycle of obesity, hyperinsulinaemia and hyperandrogenaemia in PCOS patients. Based on the findings of this meta-analysis and existing clinical studies, it is reasonable to expect improved reproductive outcomes for PCOS patients treated with SGLT2 inhibitors. However, it is important to note that the current number of relevant studies is limited, and further research is warranted to fully elucidate the precise effects of SGLT2 inhibitors in women with PCOS.
Furthermore, regarding adverse reactions, this study found that gastrointestinal discomfort, such as nausea, diarrhoea, loss of appetite, vomiting and abdominal pain, was the most common side effect, with nausea being the predominant symptom. However, the meta-analysis results indicated there were fewer nausea events in the SGLT2 inhibitors treatment group than in the control group [RR = 0.35, 95% CI (0.21, 0.60), I2 = 71%, P = 0.0001]. Additionally, the incidence of other adverse effects was also lower in the SGLT2 inhibitors treatment group than in the control group. These findings highlight the safety advantage of SGLT2 inhibitors in the treatment of PCOS patients.
This meta-analysis had some limitations, as follows. (1) The sample sizes of the control and experimental groups were small. Moreover, there was a large difference in sample events between the one Chinese trial and the other trials, leading to significant heterogeneity in the results. (2) Due to the limited number of clinical studies in this field, a trial that used exenatide as a control treatment for comparison was included. SGLT2 inhibitors monotherapy and SGLT2 inhibitors + metformin combination treatment used in that study were considered as two separate studies in our meta-analysis, according to the inclusion criteria, which might have affected our final results. (3) Few articles were included and thus the final result was not unequivocal. (4) The included experimental groups were SGLT2 inhibitors or SGLT2 inhibitors in combination with metformin, and the final results could not eliminate the potential effects of metformin. (5) The PCOS diagnostic criteria used in the five trials were different from the SGLT2 inhibitors types, and the trial durations as well as the follow-up periods were too short to perform an assessment of ovulation, menstrual frequency and fertility after SGLT2 treatment of women with PCOS. Given these limitations, we look forward to conducting randomised controlled trials or broad sample case–control studies with more rigorous designs and higher quality to validate our results. Furthermore, the results of this meta-analysis may not be applicable to all patients with PCOS, however new treatments are expected. It is our hope that can serve as a reference for the potential clinical application of drugs for the treatment of PCOS.
Conclusion
In conclusion, the available data suggest that SGLT2 inhibitors are comparable with metformin/exenatide in their ability to improve anthropometric measures, glucolipid metabolism and reproductive hormone concentrations in patients with PCOS. Moreover, SGLT2 inhibitors were more effective than metformin in reducing body weight and DHEAS concentrations. As a result, SGLT2 inhibitors represent a potential alternative treatment for overweight/obese women with PCOS who exhibit an inadequate response to metformin. However, the evidence in this study was generated from the literature is limited in both quantity and sample sizes, which renders our findings inconclusive. Therefore, further well-designed studies with larger sample sizes and at multiple centres are required to validate these findings.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Lizneva D. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016;106(1):6–15.
Norman RJ. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97.
Nandi A. Polycystic ovary syndrome. Endocrinol Metab Clin North Am. 2014;43(1):123–47.
Rasquin LI, Anastasopoulou C, Mayrin JV. Polycystic ovarian disease. Treasure Island: StatPearls Publishing; 2023.
Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(5):748–58.
Bagir GS. Body Mass Index below Obesity Threshold Implies Similar Cardiovascular Risk among Various Polycystic Ovary Syndrome Phenotypes. Med Princ Pract. 2016;25(1):61–6.
Wang FF. Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis. Obes Rev. 2018;19(10):1424–45.
Stepto NK. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013;28(3):777–84.
Mahalingaiah S, Diamanti-Kandarakis E. Targets to treat metabolic syndrome in polycystic ovary syndrome. Expert Opin Ther Targets. 2015;19(11):1561–74.
Rubin KH. Development and Risk Factors of Type 2 Diabetes in a Nationwide Population of Women With Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2017;102(10):3848–57.
Li Y. Multi-system reproductive metabolic disorder: significance for the pathogenesis and therapy of polycystic ovary syndrome (PCOS). Life Sci. 2019;228:167–75.
Lashen H. Role of metformin in the management of polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2010;1(3):117–28.
Teede HJ. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–18.
Practice Committee of the American Society for Reproductive Medicine. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline. Fertil Steril. 2017;108(3):426–41.
Dunaif A. Drug insight: insulin-sensitizing drugs in the treatment of polycystic ovary syndrome–a reappraisal. Nat Clin Pract Endocrinol Metab. 2008;4(5):272–83.
Chen X, He S, Wang D. Effects of metformin on body weight in polycystic ovary syndrome patients: model-based meta-analysis. Expert Rev Clin Pharmacol. 2021;14(1):121–30.
Vallon V, Verma S. Effects of SGLT2 Inhibitors on Kidney and Cardiovascular Function. Annu Rev Physiol. 2021;83:503–28.
Marinkovic-Radosevic J. Exploring new treatment options for polycystic ovary syndrome: Review of a novel antidiabetic agent SGLT2 inhibitor. World J Diabetes. 2021;12(7):932–8.
Pruett JE. 2021 Impact of SGLT-2 Inhibition on Cardiometabolic Abnormalities in a Rat Model of Polycystic Ovary Syndrome. Int J Mol Sci. 2021;22(5):2576.
Li X. Sodium Glucose Co-Transporter 2 Inhibitors Ameliorate Endothelium Barrier Dysfunction Induced by Cyclic Stretch through Inhibition of Reactive Oxygen Species. Int J Mol Sci. 2021;22(11):6044.
DeFronzo RA, Norton L, Abdul-Ghani M. Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nat Rev Nephrol. 2017;13(1):11–26.
Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41–7.
Legro RS. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–92.
Elkind-Hirsch KE. Exenatide, Dapagliflozin, or Phentermine/Topiramate Differentially Affect Metabolic Profiles in Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2021;106(10):3019–33.
Htike ZZ. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A systematic review and mixed-treatment comparison analysis. Diabetes Obes Metab. 2017;19(4):524–36.
Han Y, Li Y, He B. GLP-1 receptor agonists versus metformin in PCOS: a systematic review and meta-analysis. Reprod Biomed Online. 2019;39(2):332–42.
Siamashvili M, Davis SN. Update on the effects of GLP-1 receptor agonists for the treatment of polycystic ovary syndrome. Expert Rev Clin Pharmacol. 2021;14(9):1081–9.
Zhang J. Canagliflozin combined with metformin versus metformin monotherapy for endocrine and metabolic profiles in overweight and obese women with polycystic ovary syndrome: A single-center, open-labeled prospective randomized controlled trial. Front Endocrinol (Lausanne). 2022;13:1003238.
Cai M. Efficacy of canagliflozin versus metformin in women with polycystic ovary syndrome: A randomized, open-label, noninferiority trial. Diabetes Obes Metab. 2022;24(2):312–20.
Javed Z. Effects of empagliflozin on metabolic parameters in polycystic ovary syndrome: A randomized controlled study. Clin Endocrinol (Oxf). 2019;90(6):805–13.
Zeng Q, Xu X, Xin L. Effect of canagliflozin combined with metformin on endocrine and metabolic levels in overweight and obese women with polycystic ovary syndrome (in Chinese). Maternal & Child Health Care of China. 2022;37(24):4649–52.
McMurray JJV. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381(21):1995–2008.
Zheng RJ. Association of SGLT2 Inhibitors With Risk of Atrial Fibrillation and Stroke in Patients With and Without Type 2 Diabetes: A Systemic Review and Meta-Analysis of Randomized Controlled Trials. J Cardiovasc Pharmacol. 2022;79(2):e145–52.
Perkovic V. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med. 2019;380(24):2295–306.
Berni TR, Morgan CL, Rees DA. Women with polycystic ovary syndrome have an increased risk of major cardiovascular events: A population study. J Clin Endocrinol Metab. 2021;106(9):e3369–80.
Wekker V. Long-term cardiometabolic disease risk in women with PCOS: a systematic review and meta-analysis. Hum Reprod Update. 2020;26(6):942–60.
Catalano PM. Obesity, insulin resistance, and pregnancy outcome. Reproduction. 2010;140(3):365–71.
Lainez NM, Coss D. obesity, neuroinflammation, and reproductive function. Endocrinology. 2019;160(11):2719–36.
Ormazabal V. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Pruett JE. Mitochondrial function and oxidative stress in white adipose tissue in a rat model of PCOS: effect of SGLT2 inhibition. Biol Sex Differ. 2022;13(1):45.
He YL. The effects of licogliflozin, a dual SGLT1/2 inhibitor, on body weight in obese patients with or without diabetes. Diabetes Obes Metab. 2019;21(6):1311–21.
Tan S. Licogliflozin versus placebo in women with polycystic ovary syndrome: A randomized, double-blind, phase 2 trial. Diabetes Obes Metab. 2021;23(11):2595–9.
Labrie F. Is dehydroepiandrosterone a hormone? J Endocrinol. 2005;187(2):169–96.
Leowattana W. DHEAS as a new diagnostic tool. Clin Chim Acta. 2004;341(1–2):1–15.
Hoffman DI, Klove K, Lobo RA. The prevalence and significance of elevated dehydroepiandrosterone sulfate levels in anovulatory women. Fertil Steril. 1984;42(1):76–81.
Steinberger E, Smith KD, Rodriguez-Rigau LJ. Testosterone, dehydroepiandrosterone, and dehydroepiandrosterone sulfate in hyperandrogenic women. J Clin Endocrinol Metab. 1984;59(3):471–7.
Longcope C. Adrenal and gonadal androgen secretion in normal females. Clin Endocrinol Metab. 1986;15(2):213–28.
Qiao J, Feng HL. Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum Reprod Update. 2011;17(1):17–33.
Naver KV. Increased risk of preterm delivery and pre-eclampsia in women with polycystic ovary syndrome and hyperandrogenaemia. BJOG. 2014;121(5):575–81.
Rachoń D, Teede H. Ovarian function and obesity–interrelationship, impact on women’s reproductive lifespan and treatment options. Mol Cell Endocrinol. 2010;316(2):172–9.
Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020;35:100937.
Escobar-Morreale HF, San Millán JL. Abdominal adiposity and the polycystic ovary syndrome. Trends Endocrinol Metab. 2007;18(7):266–72.
Cena H, Chiovato L, Nappi RE. Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab. 2020;105(8):e2695–709.
Acknowledgements
This systematic review and meta-analysis did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable.
Competing Interests
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, L., Wang, Z., Kong, L. et al. Effect of SGLT2 Inhibitors on Improving Glucolipid Metabolism and Reproductive Hormone Status in Overweight/Obese Women with PCOS: A Systematic Review and Meta-Analysis. Reprod. Sci. 31, 1190–1203 (2024). https://doi.org/10.1007/s43032-023-01415-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01415-5