Abstract
Salmonella is an important poultry pathogen with zoonotic potential. Being a foodborne pathogen, Salmonella-contaminated poultry products can act as the major source of infection in humans. In India, limited studies have addressed the diversity of Salmonella strains of poultry origin. This study represented 26 strains belonging to Salmonella serovars Typhimurium, Infantis, Virchow, Kentucky, and Agona. The strains were tested for resistance to 14 different antimicrobial agents using the Kirby-Bauer disk-diffusion assay. The presence of the invA, hilA, agfA, lpfA, sopE, and spvC virulence genes was assessed by polymerase chain reaction (PCR), and the genetic diversity was assessed by Enterobacterial Repetitive Intergenic Consensus Polymerase Chain Reaction (ERIC-PCR). The highest resistance to tetracycline (n = 17; 65.38%) followed by nalidixic acid (n = 16; 61.53%) was detected among the strains. Among the strains (n = 17) phenotypically resistant to tetracycline, 94% (n = 16) were also positive for the tetA gene. Based on the presence of virulence genes, the strains were characterized into three virulence profiles (PI, P2, and P3). Among the investigated virulence genes, invA, hilA, agfA, and lpfA were present in all strains. The sopE gene was mostly associated with serovars Virchow (n = 3; 100%) and Typhimurium (n = 8; 80%), whereas spvC gene was exclusive for two Typhimurium strains that lacked sopE gene. ERIC-PCR profiling indicated clusters correlating their serovar, geographical, and farm origins. These results demonstrate that Salmonella isolates with a wide genetic range, antibiotic resistance, and virulence characteristics can colonize poultry. The presence of such strains is crucial for both food safety and public health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Each year, diarrheal diseases impact an estimated 550 million people worldwide and are thought to be the cause of 33 million fatalities. In India, Salmonella is one of the most frequent pathogens for gastrointestinal and systemic diseases [1, 2]. Approximately 2600 serovars of Salmonella enterica subsp. enterica (Salmonella enterica) have been reported, which cause enteric infections in both animals and humans [3, 4]. Non-typhoidal Salmonella (NTS) associated with many food products, poultry meat and eggs, is recognized as a potent zoonotic pathogen linked with foodborne transmission [5,6,7]. Salmonella spp. serovars are equipped with various mechanisms to invade and counter the oxidative stress within the cells. They also harbor diverse virulence factors resulting in enteric and systemic clinical manifestations in the host [8,9,10,11]. In the recent years, emergence of virulent multidrug-resistant (MDR) isolates of Salmonella has become a matter of serious public health concern [11].
A recent study reported the predominance of serovars Typhimurium, Infantis, Kentucky, Gallinarum, and Virchow in Indian poultry (2005–2019) [12]. A comparative study on poultry Salmonella strains representing 17 states (2011–2016) also involving the major egg-producing and consumer states reported Typhimurium, Gallinarum, and Enteritidis as the predominant serovars [13]. With an overall Salmonella prevalence of 3.5%, the predominant serovars reported were Enteritidis (68.1%) and Typhimurium (31.8%) from poultry and poultry products from Karnataka state. The study also reported 72.7% isolates as MDR (≥3 antimicrobial class) with the highest resistance was observed for polymyxin-B (81.8%) followed by nalidixic acid (72.7%) [14]. The emergence of serovar Agona among poultry farms in addition to commonly reported serovars was recently reported from the union territory of Jammu and Kashmir [15]. The use of antibiotic growth promoters (AGP) in poultry feed is unregulated in India. Testing of antimicrobial residues in 70 chicken meat samples meant for human consumption in New Delhi, India, indicated 40% positivity, with the predominant ones indicated were norfloxacin (20%), ciprofloxacin (14.3%), doxycycline (14.3%), oxytetracycline (11.4%), and chlortetracycline (1.4%) [16].
DNA-based fingerprinting techniques such as Enterobacterial Repetitive Intergenic Consensus PCR (ERIC-PCR) are rapid and sensitive assays and can be easily performed in small-scale laboratories [17]. Hence, many researchers have attempted genotyping of Salmonella isolates to infer their persistence and spread in different geographical regions [18, 19]. Thus, continuous monitoring of the emergence and spread of virulent AMR Salmonella serovars is essential to prepare for establishing preventive and control strategies. Despite the high prevalence of salmonellosis in India, there are limited reports on the detailed characterization of Salmonella strains associated with poultry. Considering these facts, the present study was envisaged to study AMR, virulence, and genotypic characteristics of Salmonella strains recovered from poultry in India during the last four years.
Materials and methods
Bacterial strains and serotyping
Twenty-six (n=26) Salmonella strains maintained at the repository of National Salmonella Centre-Veterinary (NSC-Vet), Indian Veterinary Research Institute were used in the present study. The strains were recovered from poultry (broilers) during a period ranging from 2019 to 2022 recovered from four different states viz., Uttar Pradesh, Uttarakhand, Andaman and Nicobar Islands, and Jammu and Kashmir, India. Among these, n = 12 strains were also reported in a previous study from Jammu and Kashmir, India [15]. The strains were revived using brain heart infusion (BHI) broth after incubation for 12–18 h at 37 °C following the sub-culturing on Hektoen Enteric (HE) agar. Green-colored colonies with black centers were presumptively identified as Salmonella strains and were subsequently sub-cultured on nutrient agar for downstream analysis. Further, biochemical characterization was carried out using catalase, triple sugar iron, urease, citrate, and motility indole lysine (MIL) tests. Salmonella serotyping was performed using agglutination test and specific antisera (SSI Diagnostica A/S, Denmark) according to the White-Kauffmann Le-minor (WKL) scheme [20]. Molecular serotyping of the strains was also performed using serovar-specific PCR as described earlier [12]. The genomic DNA was extracted using QIAamp DNA Mini Kit (Qiagen, USA). All PCR assays in the present study were carried out in 25 μL reaction mixture containing 2.5 μL of DNA template, 12.5 μL of 2x master mix (DreamTaq Green PCR Master Mix, Thermo Scientific™), 0.5 μL each of forward and reverse primers (10 pmol/μL), and nuclease-free water to make up the volume. The primers, amplicon lengths, and annealing temperatures used for molecular serotyping PCR are mentioned in Supplementary Table 1. The amplified PCR products were electrophoresed on 2% agarose gels containing ethidium bromide and visualized using the UV gel documentation system (Alpha Imager, Germany).
Antimicrobial susceptibility testing
The antibiotic susceptibility testing was performed using the Kirby-Bauer disk diffusion method [21] as per the Clinical and Laboratory Standards Institute guidelines [22]. Fourteen (n = 14) antimicrobial agents (Himedia, India) were tested at the following concentrations: cefotaxime + clavulanic acid (CEC, 30/10 μg), ceftazidime (CAZ, 10 μg), ceftazidime + clavulanic acid (CAC, 30/10 μg), streptomycin (S, 10 μg), levofloxacin (LE, 5 μg), ciprofloxacin (CIP, 5 μg), nitrofurantoin (NIT, 300 μg), tetracycline (TE, 30 μg), doripenem (DOR, 10 μg), ertapenem (ERT, 10 μg), meropenem (MER, 10 μg), imipenem (IMP, 10 μg), nalidixic acid (NA, 30 μg), kanamycin (K, 30 μg), amoxicillin/clavulanic acid (AMC, 30, 20/10), aztreonam (AT, 30 μg), trimethoprim-sulphathoxazole/co-trimoxazole (COT, 25 μg), and trimethoprim (TR, 5 μg). The extended spectrum beta-lactamase (ESBL) production in the Salmonella strains was determined by double disk diffusion test [23]. Escherichia coli strain ATCC 25922 and Klebsiella pneumoniae strain ATCC 700603 were used as the quality control strains. The zone of inhibition around the antibiotic disks was measured in mm and compared with the CLSI clinical break points (CLSI, 2018).
For genotypic resistance profiling, resistance genes were selected against antibiotics for which maximum strains were showing resistance. Molecular detection was carried out using polymerase chain reaction targeting the resistance genes like qnrA, qnrB, qnrC, qnrD, qnrS, Ib-cr, and qepA for quinolones [24,25,26,27,28], tetA, tetB, and tetC genes for tetracycline [29], and dfrA gene for trimethoprim [30]. The genomic DNA extracted using QIAamp DNA Mini Kit (Qiagen, USA) was used as the template DNA. PCR conditions and product visualization were carried out as mentioned in earlier section. The primers, amplicon lengths, and annealing temperatures used for PCR are mentioned in Supplementary Table 1.
Virulence profiling
The Salmonella strains were investigated by PCR for the presence of virulence genes using standard PCR protocols. Uniplex PCR targeting six virulence genes invA, agfA, lpfA, hilA, sopE, and spvC were performed. [31,32,33,34,35]. PCR conditions and product visualization were carried out as mentioned in the earlier section. The primers, amplicon lengths, and annealing temperatures used for PCR are mentioned in Supplementary Table 1.
ERIC profiling
Genotyping of the Salmonella strains was performed by Enterobacterial Repetitive Intergenic Consensus (ERIC) PCR using the primer pairs ERIC-F (5′-ATG TAA GCT CCT GGG GAT TCA C-3′) and ERIC-R (5′-AAG TAA GTG ACT GGG GTG AGC G-3′) [36]. The cycling conditions were as follows: initial denaturation at 95 °C for 7 min, followed by 30 cycles of denaturation at 90 °C for 30 s, annealing at 52 °C for 1 min, and extension at 65 °C for 8 min, and a final extension at 65 °C for 16 min [37]. The PCR products were separated using 2% agarose containing ethidium bromide. After electrophoresis, the gel images were captured and profiles were assigned manually.
Results
Bacterial strains and serotyping
Based on both the conventional and molecular serotyping, the strains were confirmed as belonging to the serovars Typhimurium (10/26), Infantis (5/26), Virchow (3/26), Kentucky (4/26), and Agona (4/26). The details of strains with respect to their serovar, host, source, farm, year of isolation, and geographical locations are shown in Supplementary Table 2.
Antimicrobial susceptibility testing
Twenty out of 26 strains (76.9%) were resistant to ≥1 of the tested antimicrobial drugs. The antimicrobial resistance profiles obtained for the strains are shown in Table 1. The antibiotic sensitivity testing (ABST) results revealed most of the strains resistant to tetracycline (TE) (n = 17/26; 65.38%) followed by nalidixic acid (NA) (n = 16/26; 61.53%) and trimethoprim (TR) (n = 8/26; 30.76%). In the present study, 61.53% (n = 16/26) of the strains were MDR isolates. None of the strains (0%; n = 26/26) were susceptible for all antibiotics, whereas 15.38% (n = 4/26) was resistant to one antibiotic, and another 15.38% (n = 4/26) was resistant to two different antibiotic classes. All the strains belonging to the serovars Infantis (5/5) and Virchow (3/3) were 100% MDR, whereas 75% (3/4) among Kentucky strains was MDR. However, only one Salmonella Typhimurium strain (n = 1/10; 10%) was identified as MDR. The two strains representing the serovar Infantis and one Typhimurium strain exhibited resistance to maximum numbers [6] of antimicrobial drugs, whereas the remaining Typhimurium strains were susceptible to most of the antimicrobial drugs. All strains except one representing serovars Kentucky (n = 3) and all Agona strains (n = 4) were resistant to levofloxacin, whereas among them 6 were resistant to ciprofloxacin. None of the Salmonella strains were identified as ESBL producers based on the double disk diffusion assay. Other than this, amoxicillin/clavulanic acid (AMC) resistance was exclusive to serovar Kentucky strains, and CIP resistance was exclusive to serovar Agona and Kentucky strains, whereas NIT resistance was predominant for serovar Infantis strains and K resistance predominant for serovar Infantis and Kentucky strains. All the above mentioned resistance profiles were also observed within strains belonging to the same geographical location (Jammu and Kashmir) and in most cases represented the same farms. On the other hand, the two Typhimurium strains representing two different farms from the same region differed for their AMR profiles. The serovar-wise resistance profiles are shown in Fig. 1A.
Antimicrobial resistance and virulence pattern among Salmonella strains: serovar wise antimicrobial resistance (A) and virulence genes (B) are shown in the form of a bar diagram. The occurrence of viulence and AMR is represented as percentage calculated by considering each serovar seperately The number of strains respresenting each serovar was Typhimurium - 10, Infantis - 5, Kentucky - 4, Virchow - 3 and Agona - 4
Out of the 26 Salmonella strains, 17 were resistant to TE in the disk diffusion assay. In accordance with the phenotypic assay, 16 out of the 17 tetracycline-resistant Salmonella strains (94.44%) were positive for the tetA (tetracycline efflux pump) gene. Thus, a good correlation between the phenotypic and genotypic expression of TE resistance was observed among the Salmonella strains. On the other hand, among the quinolone (levofloxacin and ciprofloxacin) (7/26; 26.92%) and trimethoprim (n = 8; 30.76%) resistant strains, corresponding resistant genes were not detected based on the genes targeted.
Virulence profiling
All the Salmonella strains were screened for the presence of virulence-associated genes, namely, invA, hilA, agfA, lpfA, sopE, and spvC. All the strains were found to carry a minimum of 3 virulence genes. The prevalence of virulence genes varied among strains. The highest prevalence was observed for invA, hilA, agfA, and lpfA (100%; n = 26/26). Strain wise distribution of virulence genes is shown in Table 2. Serovar wise distribution of virulence genes is shown in Fig. 1B. The strains were categorized into 3 virulence profiles based on the presence of virulence genes. Strains of profile P1 were having genes representing invA, agfA, hilA, and lpfA; P2 had virulence genes invA, agfA, hilA, lpfA, and sopE; P3 had virulence genes inv A, agfA, hilA, lpfA, and spvC. The frequency of occurrence of the virulence profile among the strains was P1 (50%), P2 (42.3%), and P3 (7.6%). The strains of the serovars Infantis (n = 5), Agona (n = 4), and Kentucky (n = 4) exhibited P1 virulence profile, whereas Salmonella Virchow (n = 3) showed P2 virulence profile. On the other hand, the strains of Typhimurium serovars (n = 10) manifested both P2 and P3 virulence profile. Out of the 10 Salmonella Typhimurium strains, 8 showed P2 profile and the 2 exhibited P3 profile. Salmonella serovars Infantis and Agona having the same geographical origin (Jammu and Kashmir) revealed similarity in virulence profile. Salmonella Kentucky (n = 4) strains from two different origins (Uttarakhand and Andaman and Nicobar Island) exhibited similar virulence profile. All the strains representing serovars Infantis, Kentucky, and Agona did not show the presence of spvC and sopE genes. Eight strains representing serovar Typhimuirum and three strains representing serovar Virchow harbored sopE gene, whereas spvC gene was unique to two Typhimurium strains isolated from suspected clinical cases from poultry.
ERIC profiling
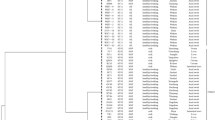
PCR fingerprints of 26 Salmonella strains were obtained by ERIC-PCR. The ERIC-PCR profile was used to infer the genetic relatedness among isolates and to correlate with their serovar and geographical/farm origins. Strains with similar ERIC PCR fingerprints were assigned unique profile numbers (P1 to P10). In general, the strains representing the same serovar and belonging to same farm clustered together. The profile P1 represented Agona, P2 and P3 represented Kentucky, P4 and P5 represented Virchow and Infantis, P7–P10 represented Typhimurium strains. Two strains originating from the same geographical region (Jammu and Kashmir) within the serovar Kentucky formed a closely related cluster, whereas another strain belonging to a different geographical origin (Andaman and Nicobar Islands) formed separate cluster. Strains representing serovar Typhimurium represented 4 profiles, with two profiles (P9 and P10) representing strains from the same geographical origins (Uttarakhand). The remaining two strains from the same geographical origins (Uttar Pradesh) represented unique profiles (P7 and P8), but were isolated from different farms. The genetic diversity analysis of Salmonella strains using ERIC-PCR fingerprints along with the serovar information and geographical locations is depicted in Fig. 2.
Discussion
Salmonellosis is a significant threat to public health worldwide. Globally, an estimated 93 million enteric infections occur annually because of non-typhoidal Salmonella (NTS) infections, causing 155,000 deaths [38]. NTS-associated infection is considered to be a neglected emerging enteric infection in India [39]. Unhygienic practices during the slaughtering of animals, improper handling, and transportation of raw meat all increase the likelihood of contamination of meat products with NTS [40]. The pathogenic potential and AMR of Salmonella can change over time and hence need to be routinely investigated for implementing appropriate control measures. Considering these facts, in the present study, a total of twenty-six Salmonella strains of poultry origin were subjected to antimicrobial susceptibility testing, virulence profiling, and strain typing based on ERIC-PCR profiling.
Among all, 20 strains (76.92%) were found to be resistant to at least one antimicrobial drug. The highest number of strains was resistant to tetracycline (TE) (65.38%). Earlier studies reported TE resistance ranging from 36.3 to 100% for Salmonella strains associated with poultry in India [41,42,43,44]. Resistance to tetracycline associated with broiler chicken from other countries like South Africa (93%) and Brazil (83%) was also reported in similar ranges [45]. Among all tetracycline resistance mechanisms, efflux pump tet gene classes A and B are recognized as the most common genes associated with resistance in Salmonella [46]. In the present study, tetA was found to be present in 94% of the resistant isolates. Significant association of tetA gene (56% to 100%) for tetracycline resistance in poultry Salmonella strains has been reported in India [41, 43, 44].
Treatment regime using fluoroquinolones may fail in patients infected with Salmonella spp. resistant to nalidixic acid (NA) [47, 48]. The present study identified nalidixic acid resistance among 61.53% of the isolates. Corroborating resistance percentage (56.25%) was reported by an earlier study on poultry associated Salmonella in Rajasthan, India [42]. Strains representing different geographical origin strains were also indicated with time-dependent changes (90.63 to 46.43% from 1990 to 2017) in their susceptibility pattern for NA [41].
The current study detected both trimethoprim and co-trimoxazole (COT) resistance in 34 % and ciprofloxacin (CIP) resistance in 23.07% strains. An earlier study reported 25.00% and 15.62% strains resistant to trimethoprim and ciprofloxacin, respectively, among a total of 32 strains [42]. However, none of the resistant strains were positive for respective AMR genes targeted by PCR in the study. Thus, it may be assumed that the phenotypic resistance may be mediated by point mutations or other mechanisms that are not explored in the study.
Presently, there is no national database or surveillance data for estimating the use of antimicrobials in health and veterinary sectors in India [49]. The antimicrobial drugs of choice for the treatment of human NTS infections are chloramphenicol, ampicillin, trimethoprim-sulphamethoxazole (cotrimoxazole), fluoroquinolones, and extended spectrum cephalosporins [41, 50]. However, antibiotic growth promoters (AGP) often included in animal feeds to promote growth can contribute to development of AMR bacteria. The AGPs reported for common use in Indian poultry sector are oxytetracycline, chlortetracycline, bacitracin, furazolidone, enrofloxacin, cephalosporins, ciprofloxacin, and tylosin [51]. Thus, the higher resistance for TE, NA, and CIP observed in the study correlates the possibility of high AGP usage in chicken. A high probability of resistance to NA, CIP, and TE in bacteria associated with Indian poultry sector was reported earlier based on studies in E. coli [52].
With respect to serovar association to any particular antibiotic resistance, we observed K, NIT, CIP, and AMC resistance associated to certain serovars such as Infantis, Agona, and Kentucky. In most cases, the strain represented the same farms and hence indicates these AMR profiles can be influenced by farm level managements including the source of poultry stock procurement to the antimicrobial usages within farm. Antimicrobial usage (AMU) pattern at farm levels correlating with high levels of resistance to the same antibiotic in Salmonella was reported in a recent study [53].
A 19-year spanning research study (2000 to 2018) conducted in India unveiled the slow emerging trends of antimicrobial resistance patterns associated with NTS serovars isolated from human feces [50]. A study involving 271 Salmonella isolates representing the period 1990 to 2017 from poultry, farm animals, and environmental sources similarly indicated a rise in antibiotic resistance for most of the tested antibiotics except cephalosporins and carbapenems [41]. All these factors emphasize the importance of NTS serovars and associated AMR risks in all sectors.
Salmonella serovars during the course of time can lose or acquire virulence factors as a result of adaptation to new hosts or environments [54]. In the present study, the presence of six virulence genes was investigated. None of the Salmonella strains was found to harbor all 6 virulence genes, whereas all the strains harbored the invA, hilA, agfA, and lpfA genes. Among these, invA and hilA genes are part of the Salmonella pathogenicity island 1 (SPI-1) and hence are required for host epithelial cell invasion in pathogenic Salmonella. On the other hand, aggregative fimbriae (agfA) and long polar fimbriae (lpf) are reported for involvement in colonization and virulence [55]. The agfA gene is associated with adhesion and biofilm formation [56], whereas lpfA gene is involved in adhesion to surfaces and epithelial cells, an essential prior stage of biofilm formation [57]. This hence indicates the essentiality of these genes for the survival of Salmonella in poultry gastrointestinal tracts and associated environments. Similar ubiquitous presence of invA, hilA, agfA, and lpf genes among all the involved poultry strains representing serovar Typhimurium and Enteritidis was reported by earlier studies [11, 54, 57].
In the present study, the sopE gene was detected in 11 (42%) and the spvC gene was detected in two (6.79%) strains. The spv (Salmonella plasmid virulence) operon is a highly conserved region that attenuates intestinal inflammation, promotes bacterial dissemination, and results in systemic infection [58]. In the present study, the presence of these genes in serovar Typhimurium strains isolated from clinical cases probably indicates their role in the septicemic manifestation of disease. Salmonella outer proteins (Sop) encoded by sop genes are the effector molecules of type-III secretion system (TTSS) which are involved in the early stages of Salmonella infection. Several isoforms of the sop genes have been identified (sopA–sopE) [59]. For the study strains, sopE gene was unique to all the Salmonella Virchow strains [3] and to those Salmonella Typhimurium strains [5] lacking the spvC gene. Similar variation among Salmonella Typhimurium strains with respect to carriage of spvC and spoE genes was reported from poultry strains in earlier studies [60]. The possible reason could be that the association of these genes differs within the genome as the spvC gene is a plasmid-borne virulence gene, whereas spoE gene is a prophage-related virulence gene [61].
In the present study, ERIC profiles indicated strain clustering correlating their serovar and geographical/farm origins. A unique profile mostly involved strains representing a particular serovar. Exceptions were observed for serovar Typhimurium and Kentucky were strains represented multiple profiles. In most cases, a different profile was observed when the strain had a different geographical or farm origin. Multiple ERIC profiles [5] within a single serovar are reported while involving 22 strains of serovar Gallinarum. The strains involved in a single profile were also belonging to different geographical locations and years of isolation [62]. Similarly, ERIC profiling of 45 poultry Salmonella isolates representing six serovars was indicated with 8 major profiles correlating their serovar and host origins, whereas 6 strains had unique profiles and remained unclustered in phylogeny. Among these, serovars Kentucky and Enteritidis strains were also involved in unrelated clusters [63]. This hence indicates strains representing a particular serovar usually cluster together, but often can also be represented in multiple clusters or form unique clusters.
Conclusion
To conclude, the present study characterized 26 strains of Salmonella belonging to serovars Typhimurium, Virchow, Kentucky, Infantis, and Agona. The strains exhibiting both MDR phenotype and maximum virulence genes may have the potential to evolve into a dominant clone with high zoonotic potential. Salmonellosis in humans due to such strain may overwhelm the current therapeutic regimes resulting in high treatment costs and fatality. The genetic diversity among the strains regardless of the serovars further necessitates continuous monitoring and surveillance of Salmonella strains among the poultry industry.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- NTS:
-
Non-typhoidal Salmonella
- ERIC-PCR:
-
Enterobacterial Repetitive Intergenic Consensus PCR
- AMR:
-
Antimicrobial resistance
- MDR:
-
Multidrug-resistant
References
Jain P, Chowdhury G, Samajpati S, Basak S, Ganai A, Samanta S, Okamoto K, Mukhopadhyay AK, Dutta S (2020) Characterization of non-typhoidal Salmonella isolates from children with acute gastroenteritis, Kolkata, India, during 2000-2016. Braz J Microbiol 51(2):613–627. https://doi.org/10.1007/s42770-019-00213-z
Mahindroo J, Thanh DP, Nguyen TNT, Mohan B, Thakur S, Baker S, Taneja N (2019) Endemic fluoroquinolone-resistant Salmonella enterica serovar Kentucky ST198 in northern India. Microb Genom. https://doi.org/10.1099/mgen.0.000275
Guibourdenche M, Roggentin P, Mikoleit M, Fields PI, Bockemühl J, Grimont PA, Weill FX (2010) Supplement 2003-2007 (No. 47) to the White-Kauffmann-Le Minor scheme. ResMicrobiol 161(1):26–29. https://doi.org/10.1016/j.resmic.2009.10.002
Jajere SM (2019) A review of Salmonella enterica with particular focus on the pathogenicity and virulence factors, host specificity and antimicrobial resistance including multidrug resistance. VetWorld 12(4):504–521. https://doi.org/10.14202/vetworld.2019.504-521
Bhardwaj DK, Taneja NK, Taneja P, Patel P (2022) Phenotypic and genotypic characterization of multi-drug resistant, biofilm forming, human invasive strain of Salmonella Typhimurium SMC25 isolated from poultry meat in India. Microb Pathog 173(Pt A):105830. https://doi.org/10.1016/j.micpath.2022.105830
Haubert L, Maia DSV, Rauber Würfel SDF, Vaniel C, da Silva WP (2022) Virulence genes and sanitizers resistance in Salmonella isolates from eggs in southern Brazil. J Food Sci Technol 59(3). https://doi.org/10.1007/s13197-021-05113-5
Li S, He Y, Mann DA et al (2021) Global spread of Salmonella Enteritidis via centralized sourcing and international trade of poultry breeding stocks. Nat Commun 12:5109. https://doi.org/10.1038/s41467-021-25319-7
Cai LL, Xie YT, Hu HJ, Xu XL, Wang HH, Zhou GH (2023) A small RNA, SaaS, promotes Salmonella pathogenicity by regulating invasion, intracellular growth, and virulence factors. Microbiology Spectrum 11(1):e02938–e02922. https://doi.org/10.1128/spectrum.02938-22
Choi J, Groisman EA (2016) Acidic pH sensing in the bacterial cytoplasm is required for Salmonella virulence. Mol Microbiol 101(6):1024–1038. https://doi.org/10.1111/mmi.13439
Masud S, van der Burg L, Storm L, Prajsnar TK, Meijer AH (2019) Rubicon-dependent Lc3 recruitment to Salmonella-containing phagosomes is a host defense mechanism triggered independently from major bacterial virulence factors. Front Cell Infect Microbiol 2(9):279. https://doi.org/10.3389/fcimb.2019.00279
Siddiky NA, Sarker MS, Khan MSR, Begum R, Kabir ME, Karim MR, Rahman MT, Mahmud A, Samad MA (2021) Virulence and antimicrobial resistance profiles of Salmonella enterica serovars isolated from chicken at wet markets in Dhaka, Bangladesh. Microorganisms 9(5):952. https://doi.org/10.3390/microorganisms9050952
Mohanapriya HA, Anbazhagan S, Khawaskar D, Jayakumar V, Lalrinzuala MV, Himani KM, Sophia I, Mariappan AK, Abhishek VKN, Sinha DK, Chaudhuri P, Chaturvedi VK, Singh BR, Thomas P (2023) Development and validation of multiplex PCR based molecular serotyping of Salmonella serovars associated with poultryinIndia. J Microbiol Methods 207:106710. https://doi.org/10.1016/j.mimet.2023.106710
Kumar Y, Singh V, Kumar G, Gupta NK, Tahlan AK (2019) Serovar diversity of Salmonella among poultry. Indian J Med Res 150:92–95. https://doi.org/10.4103/ijmr.ijmr_1798_17
Shivaning Karabasanavar N, Benakabhat Madhavaprasad C, Agalagandi Gopalakrishna S, Hiremath J, Shivanagowda Patil G, Barbuddhe B (2020) Prevalence of Salmonella serotypes S. Enteritidis and S. Typhimurium in poultry and poultry products. J Food Saf 40:e12852. https://doi.org/10.1111/jfs.12852
Singh A, Singh M, Malik MA, Padha S (2023) Is there a shift in Salmonella diversity among poultry in Northern India? Avian Dis 67(1):108–113. https://doi.org/10.1111/jfs.12852
Ramakant Sahu, Poornima Saxena (2014) Antibiotica in Meat, Investigator Center fo Science Envairoment pollution Monitoring Laboratory, New Delhi - 110062
Versalovic J, Koeuth T, Lupski R (1991a) Distribution of repetitive DNA sequences in eubacteria and application to finger printing of bacterial genomes. Nucleic Acids Res 19(24):6823–6831. https://doi.org/10.1093/nar/19.24.6823
Soares LSG, Casella T, Kawagoe EK, Benetti Filho V, Omori WP, Nogueira MCL, Wagner G, de Oliveira RR, Stahlhofer SR, Ferreira FA, Tondo EC (2023) Phenotypic and genotypic characterization of antibiotic resistance of Salmonella Heidelberg in the south of Brazil. Int J Food Microbiol 391:110151. https://doi.org/10.1016/j.ijfoodmicro.2023.110151
Xu Z, Wang M, Wang C, Zhou C, Liang J, Gu G, Wang M, Wei P (2021) The emergence of extended-spectrum β-lactamase (ESBL)-producing Salmonella London isolates from human patients, retail meats and chickens in southern China and the evaluation of the potential risk factors of Salmonella London. Food Control 128:108187. https://doi.org/10.1016/j.foodcont.2021.108187
Grimont PA, Weill FX, (2007) Antigenic formulae of the Salmonella serovars. WHO collaborating centre for reference and research on Salmonella, vol 9, pp. 1–166
Bauer AW, Kirby WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 45(4):493–496
CLSI (2018) Performance standards for antimicrobial susceptibility testing, 28th edn. CLSI supplement M100. Clinical and Laboratory Standards Institute, Wayne
Akpaka PE, Vaillant A, Wilson C, Jayaratne P (2021) Extended spectrum beta-lactamase (ESBL) produced by Gram-negative bacteria in Trinidad and Tobago. Int J Microbiol 2021. https://doi.org/10.1155/2021/5582755
Cattoir V, Poirel L, Rotimi V, Soussy CJ, Nordmann P (2007) Multiplex PCR for detection of plasmid-mediated quinolone resistance qnr genes in ESBL-producing enterobacterial isolates. J Antimicrob Chemother 60(2):394–397. https://doi.org/10.1093/jac/dkm204
Cavaco LM, Hasman H, Xia S, Aarestrup FM (2009) qnrD, a novel gene conferring transferable quinolone resistance in Salmonella enterica serovar Kentucky and Bovismorbificans strains of human origin. Antimicrob Agents Chemother 53(2):603–608. https://doi.org/10.1128/aac.00997-08
Ciesielczuk H, Hornsey M, Choi V, Woodford N, Wareham DW (2013) Development and evaluation of a multiplex PCR for eight plasmid-mediated quinolone-resistance determinants. J Med Microbiol 62(12):1823–1827. https://doi.org/10.1099/jmm.0.064428-0
Wareham DW, Umoren I, Khanna P, Gordon NC (2010) Allele-specific polymerase chain reaction (PCR) for rapid detection of the aac (6′)-Ib-cr quinolone resistance gene. Int J Antimicrob Agents 36(5):476–477. https://doi.org/10.1016/j.ijantimicag.2010.07.012
Yamane K, Wachino JI, Suzuki S, Arakawa Y (2008) Plasmid-mediated qepA gene among Escherichia coli clinical isolates from Japan. Antimicrob Agents Chemother 52(4):1564–1566. https://doi.org/10.1128/aac.01137-07
Fonseca EL, Mykytczuk OL, Asensi MD, Reis EM, Ferraz LR, Paula FL, Ng LK, Rodrigues DP (2006) Clonality and antimicrobial resistance gene profiles of multidrug-resistant Salmonella enterica serovar Infantis isolates from four public hospitals in Rio de Janeiro. Brazil J Clin Microbiol 44(8):2767–2772. https://doi.org/10.1128/jcm.01916-05
Huovinen P, Sundström L, Swedberg G, Sköld OJAA (1995) Trimethoprim and sulfonamide resistance. Antimicrob Agents Chemother 39(2):279–289. https://doi.org/10.1128/aac.39.2.279
Bäumler AJ, Heffron F (1995) Identification and sequence analysis of lpfABCDE, a putative fimbrial operon of Salmonella Typhimurium. J Bacteriol 177(8):2087–2097. https://doi.org/10.1128/jb.177.8.2087-2097.1995
Chiu CH, Ou JT (1996) Rapid identification of Salmonella serovars in feces by specific detection of virulence genes, invA and spvC, by an enrichment broth culture-multiplex PCR combination assay. J Clin Microbiol 34(10):2619–2622. https://doi.org/10.1128/jcm.34.10.2619-2622.1996
Guo X, Chen J, Beuchat LR, Brackett RE (2000) PCR detection of Salmonella enterica serotype Montevideo in and on raw tomatoes using primers derived from hilA. Appl Environ Microbiol 66(12):5248–5252. https://doi.org/10.1128/AEM.66.12.5248-5252.2000
Prager R, Rabsch W, Streckel W, Voigt W, Tietze E, Tschäpe H (2003) Molecular properties of Salmonella enterica serotype Paratyphi B distinguish between its systemic and its enteric pathovars. J Clin Microbiol 41(9):4270–4278. https://doi.org/10.1128/jcm.41.9.4270-4278.2003
Swamy SC, Barnhart HM, Lee MD, Dreesen DW (1996) Virulence determinants invA and spvC in salmonellae isolated from poultry products, wastewater, and human sources. Appl Environ Microbiol 62(10):3768–3771. https://doi.org/10.1128/aem.62.10.3768-3771.1996
Versalovic J, Koeuth T, Lupski R (1991b) Distribution of repetitive DNA sequences in eubacteria and application to fingerpriting of bacterial genomes. Nucleic Acids Res 19(24):6823–6831. https://doi.org/10.1093/nar/19.24.6823
Kim JS, Lee GG, Park JS, Jung YH, Kwak HS, Kim SB, Nam YS, Kwon ST (2007) A novel multiplex PCR assay for rapid and simultaneous detection of five pathogenic bacteria: Escherichia coli O157:H7, Salmonella, Staphylococcus aureus, Listeria monocytogenes, and Vibrio parahaemolyticus. J Food Prot 70(7):1656–1662. https://doi.org/10.4315/0362-028x-70.7.1656
Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, Jones TF, Fazil A, Hoekstra RM, International Collaboration on Enteric Disease “Burden of Illness” Studies (2010) The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis 50(6):882–889
Kumar S, Kumar Y, Kumar G, Kumar G, Tahlan AK (2022) Non-typhoidal Salmonella infections across India: emergence of a neglected group of enteric pathogens. J Taibah Univ Med Sci 17(5):747–754. https://doi.org/10.1016/j.jtumed.2019.03.003
Eng S-K, Pusparajah P, Mutalib N-SA, Ser H-L, Chan K-G, Lee L-H (2015) Salmonella: a review on pathogenesis, epidemiology and antibiotic resistance. Front Life Sci 8(3):284–293. https://doi.org/10.1080/21553769.2015.1051243
Inbaraj S, Agrawal RK, Thomas P, Mohan C, Agarwal RKS, Verma MR, Chaudhuri P (2022) Antimicrobial resistance in Indian isolates of non typhoidal Salmonella of livestock, poultry and environmental origin from 1990 to 2017. Comp Immunol Microbiol Infect Dis 80:101719. https://doi.org/10.1016/j.cimid.2021.101719
Mir IA, Kashyap SK, Maherchandani S (2015) Isolation, serotype diversity and antibiogram of Salmonella enterica isolated from different species of poultry in India. Asian Pac J Trop Biomed 5(7):561–567. https://doi.org/10.1016/j.apjtb.2015.03.010
Sharma J, Kumar D, Hussain S, Pathak A, Shukla M, Kumar VP, Anisha PN, Rautela R, Upadhyay AK, Singh SP (2019) Prevalence, antimicrobial resistance and virulence genes characterization of nontyphoidal Salmonella isolated from retail chicken meat shops in Northern India. Food Control 102:104–111. https://doi.org/10.1016/j.foodcont.2019.01.021
Waghamare RN, Paturkar AM, Vaidya VM, Zende RJ, Dubal ZN, Dwivedi A, Gaikwad RV (2018) Phenotypic and genotypic drug resistance profile of Salmonella serovars isolated from poultry farm and processing units located in and around Mumbai city, India. Veterinary world 11(12):1682. https://doi.org/10.14202/vetworld.2018.1682-1688
Zishiri OT, Mkhize N, Mukaratirwa S (2016) Prevalence of virulence and antimicrobial resistance genes in Salmonella spp. isolated from commercial chickens and human clinical isolates from South Africa and Brazil. Onderstepoort J Vet Res 83(1):1–11. https://doi.org/10.4102/ojvr.v83i1.1067
Pavelquesi SLS, de Oliveira Ferreira ACA, Rodrigues ARM, de Souza Silva CM, Orsi DC, da Silva ICR (2021) Presence of tetracycline and sulfonamide resistance genes in Salmonella spp.: literature review. Antibiotics (Basel, Switzerland) 10. https://doi.org/10.3390/antibiotics10111314
Dimitrov T, Udo EE, Albaksami O, Kilani AA, Shehab E-DMR (2007) Ciprofloxacin treatment failure in a case of typhoid fever caused by Salmonella enterica serotype Paratyphi A with reduced susceptibility to ciprofloxacin. J Med Microbiol 56(2):277–279. https://doi.org/10.1099/jmm.0.46773-0
Stevenson JE, Gay K, Barrett TJ, Medalla F, Chiller TM, Angulo FJ (2007) Increase in nalidixic acid resistance among non-typhi Salmonella enterica isolates in the United States from 1996 to 2003. Antimicrob Agents Chemother 51(1):195–197. https://doi.org/10.1128/aac.00222-06
Kumar SG, Adithan C, Harish BN, Sujatha S, Roy G, Malini A (2013) Antimicrobial resistance in India: a review. J Nat Sci Biol Med 4(2):286–291. https://doi.org/10.4103/0976-9668.116970
Jacob JJ, Solaimalai D, Muthuirulandi Sethuvel DP, Rachel T, Jeslin P, Anandan S, Veeraraghavan B (2020) A nineteen-year report of serotype and antimicrobial susceptibility of enteric non-typhoidal Salmonella from humans in Southern India: changing facades of taxonomy and resistance trend. Gut Pathog 23(12):49. https://doi.org/10.1186/s13099-020-00388-z
Bangera SR, Umakanth S, Chowdhury G, Saha RN, Mukhopadhyay AK, Ballal M (2019) Poultry: a receptacle for non-typhoidal Salmonellae and antimicrobial resistance. Iran J Microbiol 11:31–38
Brower CH, Mandal S, Hayer S, Sran M, Zehra A, Patel SJ, Kaur R, Chatterjee L, Mishra S, Das BR, Singh P, Singh R, Gill JPS, Laxminarayan R (2017) The prevalence of extended-spectrum beta-lactamase-producing multidrug-resistant Escherichia coli in poultry chickens and variation according to farming practices in Punjab. India Environ Health Perspect 125:077015
Jibril AH, Okeke IN, Dalsgaard A, Olsen JE (2021) Association between antimicrobial usage and resistance in Salmonella from poultry farms in Nigeria. BMC Vet Res 17(1):234. https://doi.org/10.1186/s12917-021-02938-2
Borges KA, Furian TQ, Borsoi A, Moraes HL, Salle CT, Nascimento VP (2013) Detection of virulence-associated genes in Salmonella Enteritidis isolates from chicken in South of Brazil. Pesqui Vet Bras 33:1416–1422. https://doi.org/10.1590/S0100-736X2013001200004
Wagner C, Hensel M (2011) Adhesive mechanisms of Salmonella enterica. Bacterial Adhesion: Chem, Biol Phys:17–34. https://doi.org/10.1007/978-94-007-0940-9_2
Yoo AY, Yu JE, Yoo H, Lee TH, Lee WH, Oh JI, Kang HY (2013) Role of sigma factor E in regulation of Salmonella Agf expression. Biochem Biophys Res Commun 430(1):131–136. https://doi.org/10.1016/j.bbrc.2012.11.025
Mendonça EP, Melo RT, Oliveira MR, Monteiro GP, Peres PA, Fonseca BB, Giombelli A, Rossi DA (2020) Characteristics of virulence, resistance and genetic diversity of strains of Salmonella Infantis isolated from broiler chicken in Brazil. Pesqui Vet Bras 40:29–38. https://doi.org/10.1590/1678-5150-pvb-5546
Zuo L, Zhou L, Wu C, Wang Y, Li Y, Huang R, Wu S (2020) Salmonella spvC gene inhibits pyroptosis and intestinal inflammation to aggravate systemic infection in mice. Front Microbiol 11:562491. https://doi.org/10.3389/fmicb.2020.562491
Choudhury M, Borah P, Sarma HK, Barkalita LM, Deka NK, Hussain I, Hussain MI (2016) Multiplex-PCR assay for detection of some major virulence genes of Salmonella enterica serovars from diverse sources. Curr Sci 111(7):1252–1258. https://doi.org/10.2307/24909136
Kumar N, Mohan K, Georges K, Dziva F, Adesiyun AA (2021) Occurrence of virulence and resistance genes in Salmonella in cloacae of slaughtered chickens and ducks at pluck shops in Trinidad. J Food Prot 84(1):39–46. https://doi.org/10.4315/JFP-20-203
Proroga YTR, Mancusi A, Peruzy MF et al (2019) Characterization of Salmonella Typhimurium and its monophasic variant 1,4, [5],12:i:- isolated from different sources. Folia Microbiol 64:711–718. https://doi.org/10.1007/s12223-019-00683-6
de Souza AI, de Freitas Neto OC, Batista DF, Estupinan AL, de Almeida AM, Barrow PA, Berchieri A (2015) ERIC-PCR genotyping of field isolates of Salmonella enterica subsp. enterica serovar Gallinarum biovars Gallinarum and Pullorum. Avian pathol : J WVPA 44:475–479. https://doi.org/10.1080/03079457.2015.1086975
Fendri I, Ben Hassena A, Grosset N, Barkallah M, Khannous L, Chuat V, Gautier M, Gdoura R (2013) Genetic diversity of food-isolated Salmonella strains through pulsed field gel electrophoresis (PFGE) and enterobacterial repetitive intergenic consensus (ERIC-PCR). PLoS One 8:e81315. https://doi.org/10.1371/journal.pone.0081315
Code availability
Not applicable.
Funding
Financial support received from Director, ICAR-IVRI, Izatnagar is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
DG and PT conceptualized and designed the study. DG, YMI, and AS carried out strain isolation and culturing. AKM carried out postmortem examination and sampling. DG, LP, SI and SN carried out AMR studies and virulence profiling. AB and PT carried out serotyping. SK generated ERIC profiles. PT and VC supervised the study. DG, LP, MS, PD, and PT wrote the manuscript. All authors contributed to manuscript revision and read and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval
Not applicable as animal experiments were not conducted for this research. All sample collections were made after approval and as per the guidelines of the Institutional Animal Ethics Committee, ICAR-IVRI.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: David Germano Gonçalves Schwarz
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geyi, D., Thomas, P., Prakasan, L. et al. Salmonella enterica serovars linked with poultry in India: antibiotic resistance profiles and carriage of virulence genes. Braz J Microbiol 55, 969–979 (2024). https://doi.org/10.1007/s42770-024-01252-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-024-01252-x