Abstract
Opportunistic bacteria and fungi are commonly reported causes of bovine abortion in a small percentage of fetal losses of infectious etiology in cattle. The objective of this study was to characterize the pathological and etiological findings in fetuses aborted due to secondary bacterial and fungal infections submitted for postmortem examination between 2004 and 2019 in the State of Rio Grande do Sul, Brazil. Nineteen cases of bacterial etiology and five cases of fungal etiology were assessed. In cases of bacterial etiology, gross changes were uncommon and two different microscopic patterns were observed: (1) primary bronchopneumonia with occasional dissemination in cases of Staphylococcus sp., Streptococcus sp., and Mannheimia haemolytica infections; and (2) systemic disease with sepsis in cases of Escherichia coli and Listeria sp. infections. Aspergillus sp. was the main fungal agent identified, and cases of mycotic abortion were characterized by placentitis, dermatitis, and pneumonia. Fetal membranes were available for examination in less than half of the submissions (11/24), and placental lesions were observed in all cases. This study reaffirms the importance of postmortem examinations in the determination of causes of fetal loss in cattle and highlights pathological findings commonly observed in fetuses aborted due to sporadic bacterial and fungal agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reproductive diseases, including embryonic and fetal losses, represent major economic limitations in livestock systems worldwide [1,2,3]. Bovine abortion has been associated with a plethora of infectious and non-infectious agents, and the task of reaching a final diagnosis in these cases is commonly challenging [4]. Studies compiling causes of abortion in cattle indicate that diagnostic rates are highly variable. Nevertheless, a final diagnosis is commonly made in around 30–55% of postmortem submissions and most are represented by infectious etiologies [5,6,7,8,9].
Among infectious causes, numerous bacterial agents have been associated with cattle abortion [10] and are classified as primary reproductive pathogens and secondary or opportunistic agents [4]. The first group is represented by bacteria known to lead to primary reproductive disorders such as abortion, and include Brucella abortus, Leptospira sp., Campylobacter sp., and Chlamydophila sp. [4]. The second group is comprised mainly of bacterial agents commonly found in the environment or colonizing the skin, mucous membranes, and gastrointestinal tract of cattle, which under certain circumstances, e.g., hematogenous spread in the dam, may cause placentitis or fetal dissemination, leading to abortion [4]. Common opportunistic bacterial agents include Staphylococcus aureus, Trueperella pyogenes, and Bacillus sp. [7, 10,11,12]. Likewise, fungal agents, including Aspergillus fumigatus, are occasionally described in association with cases of sporadic abortion in cattle [13].
Even though secondary or opportunist bacterial and fungal agents are not major causes of fetal loss in cattle, they are often documented in retrospective studies as relatively common causes of bovine abortion [6,7,8] and may account for around 25% of fetal losses of infectious etiology in the species [7]. This represents a significant number of submissions that are handled by veterinary pathologists and diagnosticians and need to be differentiated from other causes of abortion in cattle, including primary reproductive pathogens. However, systematic studies thoroughly compiling and describing the pathological findings associated with abortions linked to these agents are scant.
Even though several approaches have been used to diagnose and study reproductive diseases in livestock, the postmortem examination of aborted fetuses remains an important tool for this purpose, allowing the observation of pathological changes and collection of samples for confirmatory ancillary testing. Therefore, the objective of this study is to retrospectively characterize the pathological and etiological findings of cases of bovine abortion due to sporadic/opportunistic bacterial and fungal agents, diagnosed in the State of Rio Grande do Sul, Brazil.
Material and methods
Case selection
A retrospective search was performed at the database of the Veterinary Pathology Laboratory of the Universidade Federal do Rio Grande do Sul (UFRGS), Brazil. Cases of bovine abortion associated with sporadic bacterial and fungal agents diagnosed from 2004 to 2019 were compiled.
Fetuses met the criteria to be included if (i) opportunist bacterial or fungal agents were isolated in pure or nearly pure culture from fetal tissues or the placenta; (ii) fetal tissues or the placenta presented microscopic findings consistent with a bacterial or fungal infection, including suppurative lesions associated or not with intralesional agents; and (iii) no other abortifacient agent could be retrieved from the case at the time of the postmortem examination. Although Listeria monocytogenes is commonly classified as a primary reproductive agent, we included abortion cases due to this agent because infections leading to fetal loss are rarely seen in our diagnostic routine. Exceptions to the first criterion were made in cases of mycotic abortion in which culture was not available, but etiology identification was possible with immunohistochemistry (IHC) against Aspergillus sp.
Fetuses that met the following criteria were excluded from the study: (i) cases of abortion associated with primary reproductive pathogens, such as Brucella abortus, Campylobacter sp., Coxiella burnetii, and Leptospira sp.; (ii) cases presenting histopathological findings indicative of a bacterial etiology, in which no significant growth occurred or culture results were not available; (iii) cases with gross or microscopic lesions consistent with a fungal etiology, in which culture results were not available and IHC against Aspergillus sp. was negative; (iv) severely autolyzed aborted fetuses and calves that died in the neonatal period but were referred as aborted fetuses; (v) and cases lacking sufficient tissue to perform re-evaluations.
Case information and pathological evaluation
Postmortem examination reports and corresponding photographic files were reviewed in the selected cases. Compiled case information included breed, sex, and gestational age estimated through the measurement of crown-rump length [14] or through reproductive records, when available. Compiled information also included the presence of placenta with the referred submission, gross lesions, and complementary diagnostic results documented in the postmortem examination reports. Since only formalin-fixed paraffin-embedded (FFPE) tissue blocks were available in most cases, all investigations were conducted using histopathology, histochemistry, and/or IHC. FFPE tissue blocks were searched in the archives of the Veterinary Pathology Laboratory of UFRGS. Histological c. (3–4 μm thick) were prepared, routinely stained by hematoxylin and eosin (HE), and reassessed.
Microscopic findings were classified according to their distribution in the different organs, and inflammatory lesions were characterized and subjectively graded as mild, moderate, and severe. In addition to that, the presence and morphology of bacterial and fungal agents were recorded. Available sections of the gastrointestinal tract (forestomachs, abomasum, small and large intestine) were searched for evidence of bacterial or fungal colonization. When necessary, Grocott methenamine silver (GMS) and Brown-Hopps stains were employed in tissue sections to evidence fungi and Gram-positive bacteria, respectively.
Microbiology
Bacteriology and mycology results available in the postmortem examination reports were used to determine the etiological agent involved in each case. Standard bacterial culture was routinely conducted in all fetuses with fresh samples of lung, abomasum content, placenta (when available), and any additional organ showing gross changes at postmortem examination. Tissues were inoculated on 5% sheep blood agar plates (Mueller Hinton, Kasvi®, Brazil) and MacConkey agar (Kasvi®, Brazil) and incubated at 37 °C for 72 h. Identification of bacterial isolates was based on culture, morphotinctorial, and biochemical features. When gross and microscopic changes were consistent with mycotic abortion, fresh samples of skin, placenta, abomasum content, and lung were inoculated on Sabouraud dextrose agar and incubated at 25–30 °C [15].
Immunohistochemistry
IHC was conducted using rabbit polyclonal antibodies to characterize pathogen tissue distribution in cases of abortions due to E. coli (1:200 dilution; ViroStat®, Westbrook, Maine, USA) and L. monocytogenes (1:200 dilution; BD®, Franklin Lakes, New Jersey, USA), previously diagnosed by bacterial culture. The occurrence of Aspergillus sp. infection in cases of mycotic abortion was confirmed with IHC against Aspergillus sp. (1:80 dilution; antibody mouse anti-Aspergillus spp., Bio-rad®, Hercules, California, USA) when the infection was inferred by fungal culture or presumed by fungi morphology at histopathology (cases with no fungal culture available). In these cases, IHC positive results were considered diagnostic of Aspergillus sp. infection, even when fungal culture was absent. Additionally, sections from all selected cases were submitted for IHC anti-B. abortus (1:20 dilution; polyclonal antibody, rabbit anti-B. abortus, non-commercial) [16].
For each case, one slide was selected from organs presenting visible bacteria/fungi and associated inflammatory changes on histopathology. Sections of cases of E. coli mastitis, L. monocytogenes meningoencephalitis, Aspergillus fumigatus pneumonia, and B. abortus bronchopneumonia were used as positive control sections. Primary antibodies were replaced by Universal Negative Control Serum (Biocare medical, Concord, California, USA) in the negative control sections. Antigen retrieval was carried out in microwave oven for 5 min. for E. coli, with citrate buffer (pH 6.0) in a heating chamber (40 min./96 °C) with Tris EDTA buffer (pH 9.0) for Aspergillus spp., with proteinase K for 10 min. for B. abortus, and was not performed for Listeria monocytogenes. In all cases, amplification was performed with MACH 4: Universal HRP-Polymer (Biocare medical, Concord, California, USA). The reaction was detected with 3′-diaminobenzidine chromogen (Dako, Glostrup, Denmark) (IHC anti-E. coli, anti-Aspergillus spp., and anti-L. monocytogenes), and with 3-amino-9-ethylcarbazole chromogen (AEC; Sigma, St. Louis, MO, USA) (IHC anti-B. abortus). Slides were counterstained with Harris’ hematoxylin.
Additional tests
Results of additional tests aiming to rule out the involvement of important abortigenic agents were retrieved from the postmortem examination reports. Tissue sections of thymus and brain from all fetuses submitted between 2004 and 2013 were tested for bovine viral diarrhea virus (BVDV) through IHC as previously described [17], and fresh samples of thymus and spleen of fetuses submitted between 2014 and 2019 were tested for BVDV through PCR [18]. Direct fluorescent antibody test (FAT) for Leptospira sp. was performed in imprint preparations of kidney from fetuses submitted between 2004 and 2014 [19], and fresh samples of liver and kidney from fetuses submitted between 2015 and 2019 were tested for Leptospira sp. through PCR [20]. IHC anti-Neospora caninum was performed in tissue sections of fetuses presenting microscopic lesions suggestive of protozoal infection, including non-suppurative encephalitis, myocarditis, and myositis, as previously described [21].
Results
The screening process resulted in a total of 24 cases which met the inclusion criteria, consisting of 19 cases of sporadic/opportunistic bacterial infections (cases 1–19) and 5 cases of fungal infections (cases 20–24). Diagnosed agents were Staphylococcus sp. (8/24), Escherichia coli (5/24), Listeria sp. (3/24), Streptococcus sp. (2/24), Mannheimia haemolytica (1/24), Aspergillus sp. (4/24), and Geotrichum candidum (1/24). Information of individual cases of bacterial abortion and Aspergillus sp. abortion are shown in Tables 1 and 2, respectively. The placenta was referred for examination in 11/24 cases, and placental microscopic lesions were observed in all cases. All included cases were negative for B. abortus (IHC), BVDV (IHC or PCR) and Leptospira sp. (IFA or PCR), and none of the cases showed microscopic lesions that warranted IHC anti-N. caninum.
Bacterial infections
Staphylococcus sp.
Gross lesions were observed in only one case of Staphylococcus infection (fetus 7). These changes were characterized by moderate fibrin deposition covering the visceral pleura in the lung cranioventral region (Fig. 1a), and this case has been published elsewhere [22]. Microscopic lesions were observed primarily in the lungs in all cases of Staphylococcus sp. and Staphylococcus aureus-associated abortions. These changes were multifocal and ranged from mild to severe. Histological patterns were classified as suppurative bronchopneumonia (3/8), necrosuppurative and fibrinous bronchopneumonia (4/8), and alveolar exudation and thrombosis with minimal inflammation (1/8). Other pulmonary changes included fibrinous pleuritis (3/8), thickening of the interlobular septa by fibrin exudation and edema (3/8), and thrombosis (3/8). Coccoid bacterial aggregates were seen amidst lung lesions in seven cases, and these aggregates were abundant (5/8) (Fig. 1b and c) or rare (2/8).
Bovine fetuses, Staphylococcus aureus-associated abortions. a At the opening of the thoracic cavity, moderate amount of fibrin is seen covering the visceral pleura of the cranioventral area of the lung. b Lung, suppurative pneumonia associated with moderate fibrin deposition and numerous coccoid bacterial aggregates, HE, bar, 180 μm. c Lung, numerous Gram-positive cocci aggregates are observed, Brown-Hopps stain, bar, 180 μm. d Placenta, chorionic epithelium showing necrosis, fibrin deposition, and numerous cocci, HE, bar, 90 μm. e Placenta, numerous Gram-positive cocci are observed colonizing the surface of the chorionic epithelium. Brown-Hopps stain, bar, 180 μm. f Abomasum, numerous cocci are seen in the abomasal lumen and adhered to the mucosa, HE, 90 μm
The placenta was available for examination in only two cases, both of which presented multifocal fibrinosuppurative placentitis associated with necrosis and bacterial cocci (Fig. 1d). Brown-Hopps stain revealed that cocci observed in the lungs (Fig. 1c) and placenta (Fig. 1e) were Gram-positive. Sections of the gastrointestinal tract were available for reassessment in 7/8 cases, and bacteria were seen in the lumen or adhered to the mucosa without associated inflammatory changes in four fetuses (Fig. 1f). Microscopic lesions seen in other organs included thrombosis in the thymus, thrombosis in the epicardium, and multifocal necrosuppurative hepatitis (one case each).
Streptococcus sp. and Mannheimia haemolytica
The lung was the primarily affected organ in these cases. Gross changes were observed in only one case of Streptococcus sp. abortion (fetus 10), and lesions consisted of multifocal to coalescing, firm, and white areas (0.2–4 cm in diameter) in the cranioventral region of the lung (Fig. 2a). Microscopically, these foci were represented by large numbers of Gram-positive coccoid bacterial aggregates surrounded by moderate inflammatory infiltrate of neutrophils, fibrin deposition, and necrosis (Fig. 2b–c). Marked fibrin deposition was also observed in the visceral pleura. The second case of Streptococcus sp. associated abortion presented mild, multifocal fibrinosuppurative bronchopneumonia with rare Gram-positive cocci and marked expansion of interlobular septa by edema, fibrin deposition, and congestion.
Bovine fetuses, abortions due to opportunistic bacterial agents. Abortion due to Streptococcus sp. infection (a, b, c). a At the opening of the thoracic cavity, firm, multifocal to coalescing, white areas (0.2–4 cm in diameter) are seen in the cranioventral region of the lung. b Lung, severe necrosuppurative and fibrinous bronchopneumonia associated with numerous coccoid bacterial aggregates, HE, 360 μm, C which are Gram-positive cocci, Brown-Hopps stain, bar, 240 μm. d Abortion due to Mannheimia haemolytica infection. Lung, numerous bacterial rods are observed filling a bronchiole, and some adjacent alveolar spaces, HE, bar 120 μm
The abortion associated with Mannheimia haemolytica was characterized by marked, multifocal suppurative bronchopneumonia associated with large numbers of rod-shaped bacteria inside bronchioles, bronchi, and alveolar spaces (Fig. 2d). The placenta was not available for evaluation in any of these cases. Bacteria were not observed in the lumen or adhered to the mucosa of the gastrointestinal tract in any of the cases.
Escherichia coli
No gross changes were recorded in cases of E. coli-associated abortions. Histologic lesions were observed in two or more organs in 4/5 fetuses. Microscopic findings were characterized by large amounts of free bacterial rods occasionally associated with mild necrosis, mild inflammatory infiltrate of neutrophils, and mild fibrin deposition. Most commonly, numerous bacterial aggregates were seen freely in the interstitial space and inside blood vessels with minimal inflammatory or necrotic changes (Fig. 3a). Affected organs included the lung (3/5), liver (2/5), kidney (2/5), heart (2/5), skeletal muscle (2/5), brain (2/5), eyelid (1/5), spleen (1/5), and thymus (1/5).
Bovine fetuses, abortions due to opportunistic/sporadic bacterial agents. Abortions due to Escherichia coli infection (a–b). a Heart, numerous bacterial rods are observed filling the lumen of a blood vessel HE, bar 120 μm. b Placenta, marked necrosuppurative placentitis, HE, bar 240. Inset: placenta, marked immunolabeling for E. coli adhered to the surface of the remaining chorionic epithelium, IHC, bar, 240 μm. Abortions due to Listeria sp. infection (c, d, e, f). c Placenta, marked necrosis, inflammatory infiltrate of neutrophils, and deposition of debris are observed affecting chorionic villi, HE, bar 360 μm. d Placenta, chorioallantois blood vessel, numerous bacterial rods are seen in the lumen and invading the endothelium and vessel wall, HE, bar 240 μm. Inset: placenta, numerous Gram-positive rods are observed inside blood vessels of the chorioallantois, Brown-Hopps stain, bar, 240 μm. e Lung, mild, diffuse inflammatory infiltrate of neutrophils and multifocal moderate fibrin deposition are observed, HE, bar 240 μm. f Placenta, marked immunolabeling for Listeria monocytogenes adhered to the surface of the remaining chorionic epithelium and inside blood vessels, IHC, bar, 240 μm
Bacterial aggregates were found in the lumen and adhered to the mucosa of the gastrointestinal tract in 2/3 cases (sections unavailable in two cases). The placenta was available for evaluation in 3/5 calves. These three cases showed multifocal, mild to severe necrosuppurative placentitis associated with fibrin deposition, deposition of necrotic debris (Fig. 3b), and rare (2/3) to numerous (1/3) rod-shaped bacterial aggregates. IHC was positive in 5/5 cases. Immunolabeling evidenced numerous E. coli in the interstitial space and inside blood vessels in the lungs and kidney (fetus 15), in the heart (fetus 13), and adhered to the chorionic epithelium and amidst necrotic areas in the placenta (fetus 12, 14, and 16) (Fig. 3b, inset).
Listeria sp.
Gross changes were observed solely in the placenta of one fetus, and these were represented by diffuse, severe thickening of cotyledons and intercotiledonary regions due to marked deposition of friable, dull, and yellow material (fetus 19). The placenta was available for analysis in 2/3 fetuses, both of which showed similar histologic lesions characterized as moderate (fetus 17) to marked (fetus 19), multifocal necrosuppurative placentitis (Fig. 3c) associated with large numbers of small, Gram-positive bacterial rods amidst necrotic areas, adhered to the remaining chorionic epithelium, and inside chorionic blood vessels (Fig. 3d). In one case, lesions were restricted to the placenta (fetus 17). In the second case, additional findings included multifocal, moderate fibrinosuppurative bronchopneumonia (Fig. 3e) associated with numerous small, Gram-positive bacterial rods and few bacteria in the intestinal lumen (fetus 19). The third case, in which placenta was unavailable for examination (fetus 18), presented similar, small Gram-positive bacterial rod aggregates nearly occluding blood vessels in the brain, liver, spleen, thymus, lung, skeletal muscle, eyelid, forestomaches, abomasum, and small and large intestine. Additionally, mild, multifocal suppurative bronchopneumonia associated with numerous bacterial rods filling alveolar spaces, bronchioles, and bronchi were seen. In this case, bacteria were also observed invading the mucosa of the small and large intestine, in association with vasculitis and thrombosis in the submucosa. IHC yielded positive results in the three cases. Immunolabeling confirmed Listeria sp. aggregates inside blood vessels in the brain (fetus 18) and chorionic blood vessels of the placenta (fetuses 17 and 19) (Fig. 3f). In cases 17 and 19, IHC also labeled large numbers of Listeria sp. amidst areas of inflammation and necrosis in the placenta and adhered to the remaining chorionic epithelium (Fig. 3f).
Fungal infections
Four cases of Aspergillus sp. or Aspergillus fumigatus (cases 20–23) and one case of Geotrichum candidum (case 24) infections were assessed. This latter fetus presented dermatitis and pneumonia, and detailed pathological and etiological features of this case have been published elsewhere [23] and will not be addressed here. The etiological diagnosis of Aspergillus sp. associated abortion was made through fungal culture and IHC (cases 20 and 23) or only through positive IHC immunolabeling (cases 21 and 22) (Table 2).
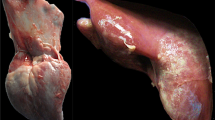
Gross lesions were restricted to the skin and placenta in cases of Aspergillus sp. abortion. The placenta was available for examination in all four cases, and gross changes were observed in all of them. The cotyledons and, often, the intercotiledonary regions were moderately to severely thickened, reddened, and showed deposition of friable, dull, and yellow material. In one case (case 23), small cotyledon-like structures were observed in the intercotiledonary regions in the chorioallantois (adventitial placentation) (Fig. 4a). This particular fetus was reported to be nine months of gestation according to the farmer’s record; however, the fetus seemed smaller, had very sparse haircoat, and crown-rump measurement was consistent with seven months of gestation. Cutaneous lesions (fetuses 20, 22, and 23) were represented by irregular, multifocal to coalescing, raised, round to oval, white to grey areas (1–4 cm) located predominantly in the head, neck, trunk, and fore and hind limbs (Fig. 4b).
Bovine fetuses, abortions due to Aspergillus sp. infection. a Placenta, the cotyledons are markedly thickened and irregular, and show deposition of yellow and dull material. Numerous, small, cotyledon-like structures are observed in the intercotiledonary regions (adventitial placentation). b Multifocal, irregular, raised, round to oval, white to gray areas (1–3 cm in diameter), are observed in the skin of the head and neck. c Placenta, large numbers of basophilic fungal hyphae are observed in the stroma of the chorioallantois, frequently invading the walls of blood vessels, HE, bar, 240 μm. Inset: multifocal immunolabeling for Aspegillus sp. hyphae is observed in the placenta, IHC, bar, 240 μm. D Placenta, blood vessels of the chorioallantois show marked fibrinoid necrosis and thrombosis. Also, severe inflammatory infiltrate of neutrophils is observed in the adjacent placental tissue, HE, bar, 240 μm. e Skin, hair follicles are markedly dilated and filled predominantly with neutrophils and necrotic debris. Also, multifocal intraepidermal pustules and diffuse hyperkeratosis are observed, HE, bar, 360 μm. f Skin, hair follicles are ruptured, and marked inflammatory infiltrate composed predominantly by neutrophils, associated with deposition of fibrin and necrotic debris are seen in the dermis, HE, bar, 240 μm. Inset: numerous fungal hyphae are observed inside hair follicles and in the adjacent dermis, GMS, bar, 240 μm
Microscopic placental changes were observed in all cases of Aspergillus sp. associated abortion (4/4). Changes were characterized by severe, multifocal to coalescing necrosuppurative and fibrinous placentitis, which effaced the superficial chorionic epithelium and frequently extended to the deep layers of the chorioallantois. Fungal hyphae were seen in all cases, sometimes amidst inflammatory changes and frequently presenting angioinvasion (Fig. 4c). Moderate-to-severe fibrinoid necrosis of blood vessel walls and thrombosis (Fig. 4d) were seen in all cases. Additional changes included marked edema in the intercotiledonary regions and multifocal areas of hemorrhage.
In the skin, microscopic lesions in cases of Aspergillus sp. abortion were represented by marked suppurative or necrosuppurative dermatitis, folliculitis, and vasculitis, as well as hyperkeratosis and intraepidermal pustules. Lesion severity and predominant histological pattern varied among cases, and among skin sections of the same fetus. In some cases, histological findings included marked dilatation of hair follicles, which were filled with large numbers of neutrophils, fewer macrophages, lymphocytes, and plasma cells, as well as necrotic debris (Fig. 4e). Sometimes, hair follicles were ruptured, and inflammation extended to the adjacent dermis (Fig. 4f). In other cases, skin lesions were more superficial and characterized by intracorneal pustules, moderate-to-severe hyperkeratosis, and superficial dermatitis and perifolliculitis.
Aspergillus sp. hyphae were seen in all cases amidst lesions. Fungal hyphae presented amphophilic to basophilic staining on HE slides (Fig. 4c), and these structures were strongly positive on GMS (Fig. 4f, inset). Hyphae were 3–6 μm wide, commonly showed dichotomous branching at acute angles (45°) and septation.
In the lung, microscopic changes were observed in 3/4 cases of Aspergillus sp. infection. Lesions consisted of multifocal areas of moderate neutrophilic and histiocytic bronchopneumonia, often forming small nodules. Fungal hyphae were observed in the lungs of two fetuses. Additional findings included moderate, multifocal necrotic hepatitis in one case (fetus 23). Sections of the gastrointestinal tract were available for examination in 2/4 cases, none of which showed microscopic changes. IHC anti-Aspergillus sp. was positive in all cases, showing moderate, multifocal labeling of fungal hyphae in the skin (fetus 23) and placenta (fetuses 20, 21, 22, and 23) (Fig. 4C, inset), amidst areas of inflammation and necrosis.
Discussion
The pregnant uterus and fetal membranes show increased susceptibility to colonization by numerous infectious agents. Several factors are believed to be associated with this susceptibility, including fetus isolation from the maternal immune system, elevated temperatures, and slow local inflammatory response [24]. Hematogenous spread seems to be the most common route of infection of the fetomaternal interface in cattle, while ascending infections are uncommon in this species [24]. The colonization of fetal membranes may occur as a result of an episode of bacteremia or fungal systemic infections, leading to placentitis, impairment of blood and nutrient supply to the fetus, and dissemination to the amniotic fluid [25]. After colonizing the placenta, microorganisms may gain entry to the fetus by two routes [4]. The first occurs after microorganisms spread to the amniotic fluid, where fungal or bacterial agents may be inhaled, ingested, or colonize the skin of the fetus [25]. A second route occurs in specific infections, for instance Listeria monocytogenes and Salmonella spp., in which after colonizing the placenta, microorganisms enter the fetus through the umbilical cord circulation, leading to systemic lesions [4].
Fungi and certain bacteria observed in this study, such as Staphylococcus sp., Streptococcus sp., and Mannheimia haemolytica, may have gained access to the fetus predominantly through the first route [4, 25]. This is corroborated by the fact that bronchopneumonia was a major and a consistent finding in most of these fetuses, especially in cases involving the mentioned bacteria above, and dermatitis was a common finding in cases of mycotic abortion. Nevertheless, some fetuses presented mild changes in other organs, which could indicate that systemic dissemination may occur with disease progression, as previously reported [7]. As previously mentioned, Listeria monocytogenes is believed to enter the fetus through the bloodstream after placental colonization, leading to a systemic and septicemic disease in the fetus [4], as observed in the reported cases. In Brazil, the main clinical presentation of bovine listeriosis is the neurologic form [26], and cases of fetal loss attributed to this disease have rarely been documented [27]. Therefore, this study brings supporting evidence to corroborate the occurrence of L. monocytogenes as a cause of fetal loss in Brazilian cattle.
Cases of E. coli infection herein observed seem to differ from cases of Staphylococcus sp, Streptococcus sp., and Manhemia hemolytica infections. For E. coli infection, even though pneumonia and gastrointestinal tract colonization were present in some cases, the main finding consisted of large numbers of bacteria in several organs, frequently inside blood vessels and without a significant inflammatory response. Even though previous studies have documented the occurrence of cattle abortions due to E. coli infection [5, 9], the role of this bacterium in bovine fetal loss seems controversial [5]. Nevertheless, herein we were able to determine E. coli tissue colonization, vascular dissemination, and sometimes associated inflammatory changes by HE and IHC, which corroborates the participation of E. coli in certain cases of sporadic bovine abortion.
Placental lesions were consistently observed in our cases, reinforcing the importance of submitting and evaluating fetal membranes in order to increase diagnostic accuracy, mainly in cases where a bacterial or fungal etiology is suspected, since abortions may occur in the absence of significant lesions in fetal tissues [28]. Placental lesions were especially severe in cases of mycotic abortion, with marked vascular lesions, which agrees with the literature [13]. One particular case of fungal abortion had adventitial placentation, and the corresponding fetus seemed smaller than the expected according to the gestational age reported by the owner. Adventitial placentation is a compensatory mechanism that occurs in cases of placental insufficiency in cattle [29] that may occur as a result of inadequate number of caruncles (congenital) or more commonly due to placental inflammation [29]. In the case reported, fungal placentitis may have led to placental insufficiency, resulting in inadequate fetal supply and underdevelopment, leading ultimately to adventitial placentation as a compensatory mechanism.
Gross changes were not common in cases of opportunist bacterial infections, highlighting the importance of standard sampling for microbiological culture and histopathology during postmortem examinations in fetuses. In contrast, fungal infections led to typical macroscopic lesions in most cases, predominantly in the placenta and in the skin, which agrees with the scientific literature [13, 24]. Even though microbiological culture is crucial for the diagnosis of bacterial/fungal abortion, the simple identification of opportunistic agents from the placenta or fetal tissues is not considered of diagnostic value, since several of them may represent environmental contamination after fetal expulsion or cervix opening [5]. Therefore, the association of microbiological results with the observation of pathological findings and exclusion of other important abortigenic agents, as conducted in this study, appears to be an appropriate approach when dealing with this type of submission [5].
Another interesting finding of this study was the observation of bacterial agents in the lumen and adhered to or invading the mucosa of the gastrointestinal tract of some examined fetuses. Although this event is known to occur in aborted fetuses [24], these pathological findings seem to be commonly overlooked in the postmortem diagnostic routine. Colonization of the gastrointestinal tract is believed to be associated with ingestion of amniotic fluid containing bacteria or fungi after placental dissemination [24] and explains why abomasum contents are commonly sampled to perform microbiological cultures. Therefore, the search for bacteria in histological sections of the gastrointestinal tract may represent a useful complementary tool in the diagnostic routine of aborted fetuses.
Main limitations of this study include the small number of cases assessed and inherent shortcomings associated with retrospective studies (e.g., variability and change in procedures conducted in different years by different professionals and dependence on the quality of previous postmortem records). Additional limitations include shortcomings that are intrinsic to studies on causes of abortion through postmortem examinations (e.g., autolysis, insufficient or incomplete submissions, multiplicity of possible etiologies, and constant need for complementary tests).
In conclusion, the postmortem examination of bovine fetuses is a fundamental tool in the diagnostic approach of fetal losses. Abortions due to opportunist bacterial and fungal agents commonly show typical gross and/or histological features that, when taken in conjunction with complementary ancillary testing (e.g., bacterial and fungal cultures, and IHC), allow the determination of such agents as causes of abortion. This work highlights the importance of complete submissions, especially the placenta, to increase the likelihood of reaching a final diagnosis. Also, we point out the importance of evaluating the gastrointestinal tract in aborted fetuses, organs that are commonly overlooked in this type of submission and may yield important complementary information to the pathological diagnosis.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Cabell E (2007) Bovine abortion: aetiology and investigations. In Pract 29:455–463. https://doi.org/10.1136/inpract.29.8.455
Lee JI, Kim IH (2007) Pregnancy loss in dairy cows: the contributing factors, the effects on reproductive performance and the economic impact. J Vet Sci 8:283–288. https://doi.org/10.4142/jvs.2007.8.3.283
Reese ST, Franco GA, Poole RK, Hood R, Montero LF, Oliveira Filho RV, Cooke RF, Pohler KG (2020) Pregnancy loss in beef cattle: a meta-analysis. Rev Anim Reprod Sci 212:106251. https://doi.org/10.1016/j.anireprosci.2019.106251
Anderson ML (2012) Disorders of cattle. In: Njaa BL (ed) Kirkbride’s – diagnosis of abortion and neonatal loss in animals, 4th edn. Wiley, New York, pp 13–48
Kirkbride CA (1992) Etiologic agents detected in a 10-year study of bovine abortions and stillbirths. J Vet Diagn Invest 4:175–180. https://doi.org/10.1177/104063879200400210
Antoniassi NAB, Juffo GD, Santos AS, Pescador CA, Corbellini LG, Driemeier D (2013) Causas de aborto bovino diagnosticadas no Setor de Patologia Veterinária da UFRGS de 2003 a 2011 [Causes of bovine abortion diagnosed by the Sector of Veterinary Pathology of the Federal University of Rio Grande do Sul in the years 2003–2011]. Pesq Vet Bras 33:155–160. https://doi.org/10.1590/S0100-736X2013000200004
Clothier K, Anderson M (2016) Evaluation of bovine abortion cases and tissue suitability for identification of infectious agents in California diagnostic laboratory cases from 2007 to 2012. Theriogenology 85:933–938. https://doi.org/10.1016/j.theriogenology.2015.11.001
Macías-Rioseco M, Silveira C, Fraga M, Casaux L, Cabrera A, Francia ME, Robello C, Maya L, Zarantonelli L, Suanes A, Colina R, Buschiazzo A, Giannitti F, Riet-Correa F (2020) Causes of abortion in dairy cows in Uruguay. Pesq Vet Bras 40:325–332. https://doi.org/10.1590/1678-5150-PVB-6550
Wolf-Jäckel GA, Hansen MS, Larsen G, Holm E, Agerholm JS (2020) Jensen TK (2020) Diagnostic studies of abortion in Danish cattle 2015–2017. Acta Vet Scand 62:1–12. https://doi.org/10.1186/s13028-019-0499-4
Kirkbride CA (1993) Bacterial agents detected in a l0-year study of bovine abortions and stillbirths. J Vet Diagn Invest 5:64–68. https://doi.org/10.1177/104063879300500114
Corbellini LG, Pescador CA, Frantz FJ, Cardoso M, Driemeier D (2006) Staphylococcus spp. abortion: skin lesions caused by Staphylococcus aureus infection in an aborted bovine-fetus. Vet Res Commun 30:717–772. https://doi.org/10.1007/s11259-006-3353-x
Costa LS, Snel GGM, Cristo TG, Ribeiro LR, Furlan LV, Camargo GB, Driemeier D, Casagrande RA (2019) Trueperella pyogenes como causa de aborto em uma vaca – relato de caso [Trueperella pyogenes as an abortion cause in a cow – case report]. Arq Bras Med Vet Zootec 71:1950–1954. https://doi.org/10.1590/1678-4162-10755
Corbellini LG, Pescador CA, Frantz FJ, Lima M, Ferreiro L, Driemeier D (2003) Aborto por Aspergillus fumigatus e A. niger em bovinos no sul do Brasil [Abortus by Abortus by Aspergillus fumigatus and A. niger in cattle in southern Brazil]. Pesq Vet Bras 23:82–86. https://doi.org/10.1590/S0100-736X2003000200005
Barr CB, Anderson ML, Blanchard PC, Daft BM, Kinde H, Conrad PA (1990) Bovine fetal encephalitis and myocarditis associated with protozoal infections. Vet Pathol 27:354–361. https://doi.org/10.1177/030098589002700508
Markey B, Leonard F, Archambault M, Cullinane A, Maguire D (2013) Clinical veterinary microbiology, 2nd edn. Mosby Elsevier Health Sciences, London
Antoniassi NAB, Juffo GD, Pescador CA, Corbellini LG, Sonne L, Gomes MJP, Nakazato L, Driemeier D (2016) Occurrence and characterization of bovine abortion caused by Brucella abortus infection in southern Brazil. Arch Med Vet 48:43–49. https://doi.org/10.4067/S0301-732X2016000100006
Bianchi MV, Konradt G, Souza SO, Bassuino DM, Silveira S, Mósena ACS, Canal CW, Pavarini SP, Driemeier D (2017) Natural outbreak of BVDV-1d–induced mucosal disease lacking intestinal lesions. Vet Pathol 54:242–248. https://doi.org/10.1177/0300985816666610
Vilcek S, Herring AJ, Herring JA, Nettleton PF, Lowings JP, Paton DJ (1994) Pestiviruses isolated from pigs, cattle and sheep can be allocated into at least three genogroups using polymerase chain reaction and restriction endonuclease analysis. Arch Virol 136:309–323. https://doi.org/10.1007/bf01321060
Miller DA, Wilson MA, Kirkbride CA (1989) Evaluation of multivalent Leptospira fluorescent antibody conjugates for general diagnostic use. J Vet Diagn Invest 1:146–149. https://doi.org/10.1177/104063878900100210
Merien F, Amouriaux P, Perolat P, Baranton G, Girons IS (1992) Polymerase chain reaction for detection of Leptospira spp. in clinical samples. J Clin Microbiol 30:2219–2224
Pescador CA, Corbellini LG, Oliveira EC, Raymundo DL, Driemeier D (2007) Histopathological and immunohistochemical aspects of Neospora caninum diagnosis in bovine aborted fetuses. Vet Parasitol 150:159–163. https://doi.org/10.1016/j.vetpar.2007.08.028
Henker LC, Lorenzett MP, Riboldi CI, Siqueira FM, Driemeier D, Pavarini SP (2020) Bovine abortion associated with Staphylococcus aureus infection - characterization of S. aureus strain isolated from fetal tissues. Cienc Rural 50:1–5. https://doi.org/10.1590/0103-8478cr20190901
Antoniassi NAB, Juffo GD, Santos AS, Pescador CA, Ferreiro L, Driemeier D (2013) Geotrichum candidum as a possible cause of bovine abortion. J Vet Diagn Invest 25:795–797. https://doi.org/10.1177/1040638713508284
Schlafer DH, Foster RA (2016) Female genital tract: abortion and stillbirth. In: Maxie MG (ed) Jubb, Kennedy & Palmer’s pathology of domestic animals, vol 3, 6th edn. Elsevier, Amsterdam, pp 398–441
Miller RBA (1977) A summary of some of the pathogenetic mechanisms involved in bovine abortion. Can Vet J 18:87–95
Konradt G, Bassuino DM, Prates KS, Bianchi MV, Snel GGM, Sonne L, Driemeier D, Pavarini SP (2017) Suppurative infectious diseases of the central nervous system in domestic ruminants. Pesq Vet Bras 37:820–828. https://doi.org/10.1590/S0100-736X2017000800007
Silva TMA, Oliveira RG, Mol JPS, Xavier MN, Paixão TA, Cortez A, Heinemann MB, Richtzenhain LJ, Lage AP, Santos RL (2009) Etiologic diagnosis of bovine infectious abortion by PCR. Cienc Rural 39:2563–2570. https://doi.org/10.1590/S0103-84782009000900028
Taylor RF, Njaa BL (2012) General approach to fetal and neonatal loss. In: Njaa BL (ed) Kirkbride’s – diagnosis of abortion and neonatal loss in animals, 4th edn. Wiley, New York, pp 1–12
Schlafer DH, Foster RA (2016) Female genital tract: Pathology of the gravid uterus, placenta, and fetus. In: Maxie MG (ed) Jubb, Kennedy & Palmer’s pathology of domestic animals, vol 3, 6th edn. Elsevier, Amsterdam, pp 393–389
Acknowledgements
The authors thank all veterinary practitioners and farmers that submitted fetuses to our Veterinary Pathology Laboratory at UFRGS, as well as everyone in the veterinary pathology team that assisted with postmortem examinations of aborted fetuses or provided diagnostic technical support throughout the years. We thank Dr. Gustavo Geraldo Medina Snel for his fundamental assistance with microbiological cultures of abortion samples for several years. We thank all laboratories that collaborated with our diagnostic routine, and their teams, for the great and continuous technical support provided: Laboratório de VirologiaVeterinária da FaVet (UFRGS), Setor de Medicina Veterinária Preventiva (Preventiva–FaVet–UFRGS), Laboratório de Bacteriologia Veterinária (LaBacVet–FaVet–UFRGS), and Laboratório de Micologia (FaVet–UFRGS). We also thank Vitor Fernandes for his assistance proofreading the manuscript.
Funding
The authors would like to thank “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq) and “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior” (CAPES)–Finance Code 001, for the financial support.
Author information
Authors and Affiliations
Contributions
Luan C. Henker was the main responsible for data collection and interpretation, as well as drafting the manuscript. Luan C. Henker and Marcele B. Bandinelli performed immunohistochemical exams. Bruna C. Lopes assisted with microbiological cultures of samples submitted from 2017 to 2019. Luan C. Henker and Igor R. dos Santos performed the histochemical preparations. Luan C. Henker and Saulo P. Pavarini re-evaluated H&E slides and delineated the study. Luan C. Henker, Marina P. Lorenzett, Daniele M. Bassuino, Gregory D. Juffo, Nadia A. B. Antoniassi, Caroline A. Pescador, Luciana Sonne, David Driemeier, and Saulo P. Pavarini performed the postmortem examinations and pathological examinations throughout the years. All authors critically revised and made intellectual contributions to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
All cases described herein occurred spontaneously, with no experimentation, inoculation, or treatment of live animals. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Responsible Editor: Luis Nero
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Henker, L.C., Lorenzett, M.P., Lopes, B.C. et al. Pathological and etiological characterization of cases of bovine abortion due to sporadic bacterial and mycotic infections. Braz J Microbiol 53, 2251–2262 (2022). https://doi.org/10.1007/s42770-022-00853-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-022-00853-8