Abstract
Obstructive sleep apnea (OSA) is correlated with nocturia, erectile dysfunction and depression. The present observational study aims to investigate whether these entities are affected by Continuous Positive Airway Pressure (CPAP) treatment in moderate and severe OSA patients. A cohort consisting of 150 OSA patients were screened for eligibility; treatment with CPAP was recommended in 102 who fulfilled the inclusion criteria. From them, 9 denied therapy, 6 were lost during follow-up, 25 declined from proper CPAP use (control group), and 62 used CPAP properly throughout 12-month follow-up (patients group). All patients were asked to report nocturia episodes/night and complete Epworth Sleepiness Scale (ESS), Functional Outcomes of Sleep Questionnaire (FOSQ), International Index of Erectile Function (IIEF-15) Questionnaire and Zung Self-Rating Depression Scale (Zung SDS) to assess sleepiness, nocturia, erectile function, and depression symptoms at baseline and end of follow-up. Nocturia episodes/night (P < 0.001), ESS (P < 0.001), FOSQ score (P = 0.014), IIEF-15 score (P = 0.027), and Zung SDS score (P = 0.030) were independently improved in patients who properly used CPAP. In detail, “Overall Productivity” (P = 0.012), “Activity Level” (P = 0.006), “Vigilance” (P = 0.001), and “Intimate Relationships and Sexual Activity” (P=0.026) FOSQ subscales as well as “Erectile Function” (P = 0.008) and “Sexual Desire” (P = 0.031) IIEF-15 function domains were independently improved by CPAP. In contrast, no difference was observed in patients who abstained from CPAP therapy. The proper use of CPAP independently improves nocturia, erectile function, and depression symptoms in patients with moderate and severe OSA, implying a direct effect in these entities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is well known to disrupt sleep by causing frequent episodes of upper airway collapse. In case that sleep disruption is so intense as to result in excessive daytime sleepiness and fatigue, the condition is referred as OSA syndrome. OSA is linked with hypertension, stroke, cardiovascular disorders, and abnormal glucose metabolism. Apnea-hypopnea index (AHI) is a measure of severity of OSA.
In general, OSA prevalence ranges from 3 to 7% worldwide. Increased age, male sex, obesity, family history, menopause, craniofacial abnormalities and tobacco or alcohol use are well-established risk factors for OSA [1].
Nocturia, defined by the International Continence Society as “the number of voids recorded during a night’s sleep: each void is preceded and followed by sleep” is not rare even among young adults and is more prevalent in women [2]. There is a strong association between OSA and nocturia; a recent meta-analysis concludes that this association refers only to males [3].
Erectile dysfunction and overall sexual dysfunction were found to be highly prevalent in patients with OSA [4], and a recently published review and meta-analysis concludes that OSA is associated with erectile dysfunction [5].
OSA has also been associated with psychiatric pathology and especially depression affecting quality of life and adherence to CPAP [6, 7].
CPAP is well documented to exert a beneficial effect in both nocturia [8,9,10,11,12] and erectile dysfunction [13,14,15]. A bidirectional link between nocturia [16] and erectile dysfunction [17, 18] with depression has been observed.
Untreated OSA clearly impacts affective disorders and may lead to permanent brain damage. The connection between OSA and psychiatric comorbidities remains obscure, especially in the context of CPAP treatment [19]. Indeed, a relevant meta-analysis demonstrated that CPAP had a moderate clinical effect on symptoms of depression and anxiety in OSA, but it was not superior to placebo (sham CPAP) [7].
Epworth Sleepiness Scale (ESS) is a self-administered questionnaire which constitutes of 8 questions. Respondents are asked to rate, on a 4-point scale (0-3), their usual chances of dozing off or falling asleep while engaged in eight different activities; therefore, the ESS score (the sum of 8 item scores, 0–3) can range from 0 to 24. The higher the ESS score, the higher that person’s average sleep propensity in daily life, or their ‘daytime sleepiness’ (DS). Normal range includes scores between 0 and 10 (0-5: Lower Normal DS, 6-10: Higher normal DS), while scores ≥ 11 represent excessive DS (11-12: Mild, 13-15: Moderate, and 16-24: Severe) [20].
The Functional Outcomes of Sleep Questionnaire (FOSQ) questionnaire consists of 30 questions related to the effects of fatigue on daily activities, and it was designed to evaluate the respondent’s quality of life in relation with DS. Five domains of day-to-day life are examined: activity levels, vigilance, intimacy and sexual relationships, productivity, and social outcomes. For each of the five domains examined, respondents indicate the degree of difficulty they experience when attempting certain activities because they are sleepy or tired. Lower scores designate more acute issues with sleepiness, as 4 corresponds to “no difficulty,” 3 to “a little difficulty,” 2 to “moderate difficulty,” and 1 to “extreme difficulty.” Therefore, the lower the FOSQ score, the greater the functional disability encountered by the respondent [21].
The International Index of Erectile Function (IIEF-15) questionnaire is a validated, multidimensional, self-administered tool for the clinical assessment of erectile dysfunction. A score of 0–5 is awarded to each of the 15 questions that comprise the related function domains, namely, erectile function (6 questions, maximum subscore 30), orgasmic function (2 questions, maximum subscore 10), sexual desire (2 questions, maximum subscore 10), and intercourse satisfaction (3 questions, maximum subscore 15), followed by 2 questions (maximum subscore 10) regarding overall satisfaction. The lower the score, the more severe derangement in erection is considered to emerge [22].
The Zung Self-Rating Depression Scale (Zung SDS) is self-report questionnaire that is widely used to quantify the depressed status of an individual. It consists of 20 questions that rate the four common characteristics of depression (the pervasive effect, the physiological equivalents, other disturbances, and psychomotor activities) that are scored on a Likert scale ranging from 1 to 4 (1: “a little of time, 2: some of the time, 3: good part of the time, 4: most of the time); therefore, the total score may range from 20 to 80. Most people with depression score between 50 and 69, while a score of 70 and above indicates severe depression [23].
The present study aims to investigate the independent effect of CPAP on nocturia, erectile dysfunction and depression in OSA patients with the use of self-reported nocturia episodes/night as well as the response to ESS, FOSQ, IIEF-15, and Zung SDS questionnaires.
Methods
In this observational study, a cohort of consecutive OSA male patients was initially recruited in “Agios Pavlos” Thessaloniki Hospital Sleep Laboratory between December, 2017 and May, 2018 through domiciliary overnight respiratory polygraphy study with the use of SOMNO Screen™ Plus (SOMNO medics GmbH, Germany), and Embletta® and Proxies (Embla, USA) as well as domiciliary overnight pulse oxymetry with the use of Nonin 2500 pulse oxymetry (Nonin, Plymouth, MN, USA). Mean hours of CPAP use/24 h, Apnea-Hypopnea Index (AHI), Respiratory Disturbance Index (RDI), Desaturation Index (DI), mean oxygen saturation (Mean SatO2), and lowest oxygen saturation (Lowest SatO2) were recorded for each patient by an experienced pulmonary and sleep medicine expert.
Inclusion criteria referred to patients that (a) exhibit moderate or severe OSA (AHI ≥ 15/h), (b) are adults aged between 20 and 70 years, (c) have completed ≥ 6 years of education, and (d) have screened for urinary tract infection (UTI). Exclusion criteria included previous exposure to CPAP and severe disorders as (i) severe asthma or chronic obstructive pulmonary disease (COPD); (ii) uncontrolled arterial hypertension (AH) or heart failure (HF); (iii) uncontrolled diabetes mellitus (DM); (iv) severe neurological (e.g., nerve damage causing overactive bladder), urological (e.g., bladder outlet obstruction), or autoimmune disease; (v) psychiatric illness; (vi) recurrent or chronic UTI; (vii) medications like a1-blockers, 5α-reductase inhibitors, muscarinic receptor antagonists, and beta-3-agonists, which could affect nocturia, as well as phosphodiesterase-5 inhibitors, which may intervene in erectile function; (viii) alcohol use disorder, and (ix) illicit drug use.
All patients who fulfilled the inclusion criteria were asked to report nocturia episodes / night and to complete questionnaires concerning sleepiness, nocturia, erectile function, and depression symptoms. In detail, daytime sleepiness was approached by the use of ESS and FOSQ questionnaires, erectile function was assessed using the IIEF-15 questionnaire, and risk for depression was estimated by Zung SDS questionnaire; all results from the above mentioned questionnaires were recorded for each patient by an experienced pulmonary sleep nurse. The nurse who supervised the procedure had been blinded to the clinical characteristics of each patient.
All OSA patients who fulfilled the inclusion criteria and successfully responded to the requested questionnaires were advised to follow treatment with CPAP and entered the study. CPAP treatment was titrated to the best pressure settings from 4 to 20 cm H2O within the first week by trained personnel who remained irrelevant to the study.
Twelve months after the beginning of the study and while treatment continued, all patients repeated domiciliary overnight respiratory polygraphy study as well as domiciliary overnight pulse oxymetry, after which they were again asked to report nocturia episodes/night and to complete ESS, FOSQ, IIEF-15, and Zung SDS questionnaires. Patients that properly used CPAP were referred as “treated patients,” while all that declined from proper CPAP treatment as “untreated patients” and served as a control group. Comparison between “treated” and “untreated” patients was used to detect any potent sources of bias.
Primary outcomes included the self-assessment of nocturia as nocturia episodes/night, subjective sleepiness as measured by ESS and FOSQ questionnaire total scores, subjective erectile function as measured by IIEF-15 questionnaire total score, and subjective assessment of depressive symptoms as approached by Zung SDS questionnaire total score.
Secondary outcomes included the self-assessment sleepiness as measured by FOSQ questionnaire subscales and subjective erectile function as measured by IIEF-15 questionnaire function domains.
The study follows the requirements of the STROBE statement [24] and was approved by the Institutional review board of “Agios Pavlos” Hospital (Decision No G22 / 32 / November 24, 2017), and the principles of the Helsinki Declaration were followed. No financial support was received for the present study. The authors declare that they have no conflict of interest.
The study was designed to detect a minimally clinically important change of at least (i) one nocturia episode/night, (ii) 10% difference in total FOSQ questionnaire score, (iii) 10% difference in total IIEF-15 questionnaire score, and (iv) 10% difference in total Zung SDS score in treated patients between end (t = 12 months) and beginning of the study (t = 0) with at least 90% power at the two-sided 5% level of statistical significance. A 10% was added to the minimum sample computed to tolerate loss-of-follow up cases.
Comparisons of discrete and continuous data between treated and untreated patients were performed with Chi-square test (or, alternatively, Fisher’s exact test if expected values were < 5) and t test, respectively. Data collected before and at the end of follow-up in the group of patients who were properly CPAP users were analyzed using paired comparisons with the aid of paired t test. Estimation of independent correlations of CPAP treatment with episodes of nocturia/night as well as ESS, FOSQ, IIEF-15, Zung SDS scores, FOSQ subscales, and IIEF-15 function domains was performed with the use of general linear models. Maximum tolerated missing data was set to 5%; no imputation was used and therefore missing values were pairwise excluded from further analysis. All means are accompanied by their standard deviations. All numerical values are provided with at least two significant digits. Statistical analysis was performed with the use of SPSS 26.0.0.0 software (IBM Corp.®, 2019). Estimation of desired power was performed using the MedCalc Statistical Software version 19.5.3 (MedCalc ® Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020).
The investigators who performed the data analysis were blinded towards any data that could serve to identify patients, such as names, addresses, telephone numbers, and social insurance ID.
Results
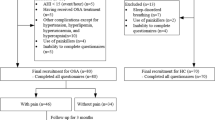
A cohort consisting of 150 consecutive OSA male patients were screened for eligibility; forty-eight of them were considered ineligible for various reasons, while 102 patients, who fulfilled the inclusion criteria and responded to the requested questionnaires, were recommended to follow treatment with CPAP. From them, 9 denied therapeutic intervention, and 6 were lost during the 12-month follow-up period; the rest 87 patients entered the study. During follow-up period, 25 patients declined from CPAP proper use during therapy, while the remaining 62 patients, who properly used CPAP, were sufficient enough to preserve the power of the study as initially designed (Fig. 1). Four out of 25 patients who did not follow CPAP treatment refused or failed to report complete data regarding nocturia episodes/night as well as ESS, FOSQ, IIEF-15, and Zung SDS questionnaires.
The groups of treated and untreated patients presented similar comorbidities and were characterized by comparable values of AHI, RDI, DI, mean SatO2, lowest SatO2, ESS score, nocturia episodes/night, total IIEF-15 score, and Zung SDS score. However, they differed as far as BMI and alcohol habits are referred. Moreover, treated patients exhibited significantly higher “Activity Level” and “Intimate Relationships and Sexual Activity” FOSQ subscales, as well as “Erectile Function and Intercourse Satisfaction” IIEF-15 function domains. A detailed comparison between patient groups is presented in Table 1.
Data and relevant paired comparisons in the group of treated patients are presented in Table 2. CPAP treatment leaded to significant improvement in ESS score, FOSQ score (except from “General Productivity” subscale), nocturia, IIEF-15 score (except from “Orgasmic Function” function domain), and Zung SDS score.
Using general linear model by incorporating differences in nocturia episodes/night, ESS score, FOSQ score, IIEF-15 score, and Zung SDS score as independent variables and use of CPAP in sleep apnea patients as dependent variable, a statistically significant result was obtained for the whole model; P < .001, Wilks’ lambda = 0.573. In detail, nocturia episodes/night (P < 0.001), ESS (P < 0.001), FOSQ score (P = 0.014), IIEF-15 score (P = 0.027), and Zung SDS score (P = 0.030) were independently improved by the use of CPAP.
In detail, regarding FOSQ subscales, “Overall Productivity” (P = 0.012), “Activity Level” (P = 0.006), “Vigilance” (P = 0.001), and “Intimate Relationships and Sexual Activity” (P = 0.026) are independently improved by the use of CPAP; however, “Social Outcome” (P = 0.059) is comparable.
Similarly, regarding IIEF-15 function domains, “Erectile Function” (P = 0.008) and “Sexual Desire” (P = 0.031) are independently improved by the use of CPAP. On the contrary, “Orgasmic Function” (P = 0.581), “Intercourse Satisfaction” (P = 0.079), and “Overall Satisfaction” (P = 0.065) are comparable.
Paired comparisons in the group of untreated patients between characteristics at baseline and at the end of the follow-up period are shown in Table 3. Interestingly, ESS score was found to have been deteriorated (P = 0.039), while no statistically significant difference regarding FOSQ total and subscales scores, IIEF-15 total and function domains scores, nocturia, and Zung SDS score was observed.
A graphical representation of differences in the form of population pyramid concerning differences between the end (t = 12 months) and the beginning of the study (t=0) in treated and untreated patients is provided concerning ESS scores, nocturia episodes/night, Zung SDS scores (Fig. 2), FOSQ total and subscale scores (Fig. 3), and IIEF-15 total and functional domains scores (Fig. 4).
Population pyramid graph depicting differences between end (t = 12 months) and beginning of the study (t = 0) concerning ESS scores (a), nocturia episodes/night (b), and Zung SDS scores (c), total FOSQ score (d) and total IIEF-15 score (e) in treated (1: blue bars at the left side of each chart) and untreated (2: red bars at the right side of each chart) patients
Population pyramid graph depicting differences in FOSQ subscales between end (t = 12 months) and beginning of the study (t = 0) concerning general productivity (a), social outcome (b), and activity level (c), vigilance (d), and intimate relationships and sexual activity (e) in treated (1: blue bars at the left side of each chart) and untreated (2: red bars at the right side of each chart) patients
Population pyramid graph depicting differences in IIEF-15 function domains between end (t = 12 months) and beginning of the study (t = 0) concerning erectile function (a), orgasmic function (b), sexual desire (c), intercourse satisfaction (d), and intimate overall satisfaction (e) in treated (1: blue bars at the left side of each chart) and untreated (2: red bars at the right side of each chart) patients
Discussion
The present study aimed to investigate the effect of CPAP on nocturia, erectile function, and depression symptoms in patients with moderate and severe OSA. Hereby, the proper use of CPAP was documented by the improvement in the EPS and the total FOSQ scores; concerning the latter, the only parameter that remained comparable was the “General Productivity” subscale. Paired comparisons within the treated patients group reveal improvement regarding nocturia, erectile function, and risk for depression while on treatment with CPAP when compared to the beginning of the study (before treatment); moreover, the use of general linear model suggests that CPAP independently exerts its beneficial effect regarding as well as nocturia, erectile function, and risk for depression are referred. Therefore, the present study has demonstrated that the proper use of CPAP independently exerts a beneficial impact on nocturia, erectile function, and depression symptoms in patients with moderate and severe OSA; thus, despite that nocturia, erectile dysfunction and depression are considered to be intertwined [22], improvement in these entities might at least be partly attributed to a direct effect of CPAP treatment. To the best of our knowledge, this is the first time that such a potent direct simultaneous effect of CPAP is demonstrated.
On the contrary, the group of OSA patients that abstained from CPAP treatment were found to have been clinically deteriorated as can be deduced from ESS score, despite that all other parameters regarding nocturia episodes/night as well as FOSQ, IIEF-15, and Zung SDS questionnaires were comparable.
Our results concerning the beneficiary effects of CPAP treatment are in keeping with current knowledge regarding nocturia [9,10,11]. Very recently, a systematic review and meta-analysis of ours concluded that nocturia rates in OSA patients are diminished after CPAP treatment, when compared with nocturia rates before CPAP treatment by 1.13 episodes/night (95% CI: −1.48, −0.78, P < 0.001) and that CPAP beneficial effect is independently correlated with younger age, increased BMI, and less severe cases [25].
Furthermore, as far as erectile dysfunction is concerned, two independent groups of investigators conclude that the use of CPAP in males with moderate [14] and severe [14, 15] OSA might attenuate symptoms of erectile dysfunction based on IIEF-15 questionnaire. Concerning the IIEF-15 function domains, “Orgasmic Function” is the only which has been found to remain comparable in CPAP users in the present study, in contrast with Irer et al. who report improvement even in that domain; however, despite that compliance to CPAP treatment was better in the present study (5.9±1.4 hours/night vs 5.2±1.4 hours/night as reported by Irer et al., P=0.008), this observation might be attributed to the fact that the study hereby included patients up to 70 years of age, while Irer et al. focused on much younger patients (< 50 years old) [14]. Nevertheless, data from literature are scarce concerning this field, and thus the contribution of the present study is considered of added value.
Of interest, the relation between CPAP treatment in OSA patients and mood disorders has not been clarified [26]. A recently performed study demonstrated that the amelioration of depression and anxiety symptoms after CPAP use was only statistically significant when considering anxiety-trait and euthymia, the distinctive component of depression [27]. Furthermore, it was suggested that subjective complaints of daytime impairment including sleepiness, fatigue as well as depression and objective measures of vigilance in patients with OSA should be assessed separately while evaluating the efficacy of CPAP therapy on daytime functioning. [28]. Nevertheless, whether depression has to be separately assessed from nocturia and erectile dysfunction has not been investigated yet.
Lack of randomization might be considered as a limitation of the present study. However, one has to consider that it would be unethical to deprive patients with moderate or severe OSA of treatment with CPAP. Additionally, it could be claimed that the group of OSA patients used as control, namely that comprising of patients who neglected or abstained from CPAP therapy, are shown to be less affected regarding fatigue on daily activities and quality of life in relation with DS as can be deduced from FOSQ questionnaire; however, ESS score is comparable and thus the possibility of introducing a selection bias due to differences in DS cannot be documented.
Another possible limitation that has to be considered is that the two OSA patient groups (these who properly followed CPAP treatment and these who abstained) differ in BMI. BMI is reported to present a significant association with the prevalence of nocturia with dose-dependent manner, regardless of age, sex, hypertension, and diabetes mellitus after taking major confounding factors into account [29]. Moreover, BMI is associated with male hypogonadism and, consequently, with erectile dysfunction [30, 31]; a recent meta-analysis indicated that this relation is also dose-dependent [32]. In addition, Zung SDS score is increased among overweight individuals, thus implying a higher risk for depression [33]. As the control group exhibits significantly lower BMI, one would consider that to be of advantage concerning nocturia, erectile dysfunction and risk for depression. On the contrary, comparable values are observed as far as ESS (P = 0.343), IIEF-15 (P = 0.068) and Zung SDS (P = 0.405) scores are referred, implying that the two groups are in practice comparable. The same can be supported concerning the difference in alcohol intake between CPAP treated patients and controls, as is known that substantial involvement with alcohol negatively affects nocturia [34] and doubles the risk for depression and vice versa [35], while, controversially, moderate alcohol consumption exhibits a beneficial effect on the risk for erectile dysfunction when compared with heavy or regular alcohol use [36].
Findings concerning the primary and secondary outcomes remain unaffected from most biases and confounders as paired comparisons are made within the same group. However, the relatively small sample of the present study, though enough to secure the desired power, hampers generalizability of the results; external validity needs assessment through properly designed prospective studies.
In conclusion, we have demonstrated that the proper use of CPAP in moderate and severe OSA patients might ameliorate nocturia, improve erectile dysfunction, and decrease the risk for depression in an independent manner. Further studies are needed to consolidate these findings and elucidate the possible underlying pathophysiology that these entities might share.
Data Availability
All data are incorporated into the article and its online supplementary material.
References
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–43.
Hunskaar S. Epidemiology of nocturia. BJU Int. 2005;96(Suppl 1):4–7.
Zhou J, Xia S, Li T, Liu R. Association between obstructive sleep apnea syndrome and nocturia: a meta-analysis. Sleep Breath. 2020;24:1293–8. https://doi.org/10.1007/s11325-019-01981-6.
Budweiser S, Enderlein S, Jörres RA, Hitzl AP, Wieland WF, Pfeifer M, et al. Sleep apnea is an independent correlate of erectile and sexual dysfunction. J Sex Med. 2009;6(11):3147–57.
Kellesarian SV, Malignaggi VR, Feng C, Javed F. Association between obstructive sleep apnea and erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res. 2018;30(3):129–40.
Hobzova M, Prasko J, Vanek J, Ociskova M, Genzor S, Holubova M, et al. Depression and obstructive sleep apnea. Neuro Endocrinol Lett. 2017;38(5):343–52.
Gupta MA, Simpson FC, Lyons DC. The effect of treating obstructive sleep apnea with positive airway pressure on depression and other subjective symptoms: A systematic review and meta-analysis. Sleep Med Rev. 2016;28:55–68.
Guilleminault C, Lin CM, Gonçalves MA, Ramos E. A prospective study of nocturia and the quality of life of elderly patients with obstructive sleep apnea or sleep onset insomnia. J Psychosom Res. 2004;56(5):511–5.
Margel D, Shochat T, Getzler O, Livne PM, Pillar G. Continuous positive airway pressure reduces nocturia in patients with obstructive sleep apnea. Urology. 2006;67(5):974–7.
Miyauchi Y, Okazoe H, Okujyo M, Inada F, Kakehi T, Kikuchi H, et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology. 2015;85(2):333–6.
Fernández-Pello S, Gil R, Escaf S, Rodríguez Villamil L, Alzueta A, Rodríguez C, et al. Lower urinary tract symptoms and obstructive sleep apnea syndrome: Urodynamic evolution before and after one year of treatment with continuous positive airway pressure. Actas Urol Esp. 2019;43(7):371–7.
Yu CC, Huang CY, Kuo WK, Chen CY. Continuous positive airway pressure improves nocturnal polyuria in ischemic stroke patients with obstructive sleep apnea. Clin Interv Aging. 2019;14:241–7.
Husnu T, Ersoz A, Bulent E, Tacettin O, Remzi A, Bulent A, et al. Obstructive sleep apnea syndrome and erectile dysfunction: does long term continuous positive airway pressure therapy improve erections? Afr Health Sci. 2015;15(1):171–9.
İrer B, Çelikhisar A, Çelikhisar H, Bozkurt O, Demir Ö. Evaluation of Sexual Dysfunction, Lower Urinary Tract Symptoms and Quality of Life in Men With Obstructive Sleep Apnea Syndrome and the Efficacy of Continuous Positive Airway Pressure Therapy. Urology. 2018;121:86–92.
Coban S, Gunes A, Gul A, Turkoglu AR, Guzelsoy M, Ozturk M, et al. Can continuous positive airway pressure improve lower urinary tract symptoms and erectile dysfunction in male patients with severe obstructive sleep apnea syndrome? Investig Clin Urol. 2020;61:607–12. https://doi.org/10.4111/icu.20200105.
Funada S, Tabara Y, Negoro H, Akamatsu S, Yoshino T, Yoshimura K, et al. Longitudinal Analysis of Bidirectional Relationships between Nocturia and Depressive Symptoms: The Nagahama Study. J Urol. 2020;203(5):984–90.
Liu Q, Zhang Y, Wang J, Li S, Cheng Y, Guo J, et al. Erectile Dysfunction and Depression: A Systematic Review and Meta-Analysis. J Sex Med. 2018;15(8):1073–82.
Yang Y, Song Y, Lu Y, Xu Y, Liu L, Liu X. Associations between erectile dysfunction and psychological disorders (depression and anxiety): A cross-sectional study in a Chinese population. Andrologia. 2019;51(10):e13395.
Vanek J, Prasko J, Genzor S, Ociskova M, Kantor K, Holubova M, et al. Obstructive sleep apnea, depression and cognitive impairment. Sleep Med. 2020;72:50–8.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, et al. An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep. 1997;20(10):835–43.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12:63–70.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Papadopoulos V, Apergis N, Filippou D. Nocturia in CPAP-Treated Obstructive Sleep Apnea Patients: a Systematic Review and Meta-Analysis. SN Compr Clin Med. 2020;2:2799–807. https://doi.org/10.1007/s42399-020-00584-7.
Gupta MA, Simpson FC. Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med. 2015;11(2):165–75.
Carneiro-Barrera A, Amaro-Gahete FJ, Sáez-Roca G, Martín-Carrasco C, Ruiz JR, Buela-Casal G. Anxiety and Depression in Patients with Obstructive Sleep Apnoea before and after Continuous Positive Airway Pressure: The ADIPOSA Study. J Clin Med. 2019;8(12):2099.
Bhat S, Gupta D, Akel O, Polos PG, DeBari VA, Akhtar S, et al. The relationships between improvements in daytime sleepiness, fatigue and depression and psychomotor vigilance task testing with CPAP use in patients with obstructive sleep apnea. Sleep Med. 2018;49:81–9.
Moon S, Chung HS, Yu JM, Ko KJ, Choi DK, Kwon O. wt al. The Association Between Obesity and the Nocturia in the U.S. Population. Int Neurourol J. 2019;23(2):169–76.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153–65.
Barkin J. Erectile dysfunction and hypogonadism (low testosterone). Can J Urol. 2011;18(Suppl):2–7.
Pizzol D, Smith L, Fontana L, Caruso MG, Bertoldo A, Demurtas J, et al. Associations between body mass index, waist circumference and erectile dysfunction: a systematic review and META-analysis. Rev Endocr Metab Disord. 2020;21:657–66. https://doi.org/10.1007/s11154-020-09541-0.
Cui J, Sun X, Li X, Ke M, Sun J, Yasmeen N, et al. Association Between Different Indicators of Obesity and Depression in Adults in Qingdao, China: A Cross-Sectional Study. Front Endocrinol (Lausanne). 2018;9:549.
Noh JW, Yoo KB, Kim KB, Kim JH, Kwon YD. Association between lower urinary tract symptoms and cigarette smoking or alcohol drinking. Transl Androl Urol. 2020;9(2):312–21.
Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106(5):906–14.
Wang XM, Bai YJ, Yang YB, Li JH, Tang Y, Han P. Alcohol intake and risk of erectile dysfunction: a dose-response meta-analysis of observational studies. Int J Impot Res. 2018;30(6):342–51.
Code Availability
Not applicable.
Funding
None received.
Author information
Authors and Affiliations
Contributions
Concerning criteria for authorship, the authors contributed to: i) Research conception and design: NA, AG, VP; ii) Data acquisition: NA, AG; iii) Statistical analysis: VP; iv) Data analysis and interpretation: NA, VP; v) Drafting of the manuscript: NA, AG, DF, VP; vi) Critical revision of the manuscript: NA, AG, DF, VP; vii) Supervision: VP, and viii) Approval of the final manuscript: NA, AG, DF, VP.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
The study was approved by the Institutional review board of “Agios Pavlos” Hospital (Decision No G22 / 32 / November 24, 2017).
Consent to Participate
All individuals (patients and controls) gave their informed consent to participate in the study
Consent for Publication
All authors gave their consent for publication of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 87 kb)
Rights and permissions
About this article
Cite this article
Apergis, N., Gounidis, A., Filippou, D.K. et al. The Use of CPAP Independently Improves Nocturia, Erectile Function, and Depression Symptoms in Obstructive Sleep Apnea Male Patients: an Observational Study. SN Compr. Clin. Med. 3, 1575–1585 (2021). https://doi.org/10.1007/s42399-021-00916-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00916-1