Abstract
This study was designed to evaluate the outcome of the implemented post-cesarean section (CS) surgical site infection (SSI) prevention protocol in Ahmadi Hospital, Kuwait. A total of 229 women who delivered by elective repeat cesarean section (ERCS) were included in this comparative study: 112 women who delivered by ERCS after the implemented protocol (study group) compared to 117 controls (who delivered by ERCS before the implemented protocol). The outcome include the incidence of post-CS SSI after and before the implemented protocol and the risk factors which may predispose to post-CS SSI. The incidence of post-CS SSI was significantly high in the controls (who delivered by ERCS before the implemented protocol) compared to the study group (who delivered by ERCS after the implemented protocol) (12.8% (15/117) versus 3.6% (4/112), respectively) (P = 0.01). The relative risk (RR) analysis showed that obesity and pregestational diabetes were significant risks for post-CS SSI (RR 0.35 (95%CI; 0.13–0.99) P = 0.04 and RR 0.24 (95%CI; 0.063–0.93) P = 0.03, respectively). In addition, the prolonged rupture of membranes (ROM) before the ERCS, duration of ERCS (more than 1 h), and surgical difficulties/adhesions during the ERCS were significant risks for post-CS SSI (RR 6.0 (95%CI; 1.003–35.9) P = 0.04, RR 6.0 (95%CI; 1.003–35.9) P = 0.04, and RR 6.0 (95%CI; 1.003–35.9) P = 0.04, respectively). The incidence of post-CS SSI after ERCS significantly reduced following the post-CS SSI prevention protocol. Obesity, pregestational diabetes, prolonged ROM, duration of ERCS (more than 1 h), and surgical difficulties/adhesions during the ERCS were definite risks for post-CS SSI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cesarean section (CS) rate increased in both developed and developing countries [1,2,3]. The incidence of primary CS increased, due to extensive fetal monitoring, maternal preferences, improved safety of anesthesia, and, consequently, the incidence of repeat CSs also increased [4].
Repeat CS is recommended electively for women with previous three or more CSs. Many obstetricians are inclined to do an elective repeat CS (ERCS) after only two previous CSs [4].
Tapia et al. reported a CS rate of 27% in three Peruvian regions between 2000 and 2010, and they observed a yearly increase in the CS rates from 23.5 to 30% [5].
The CS rate in most Middle East countries is less than 15%, and the higher CS rates are reported in Egypt (26%) and Sudan (20%) [1].
Consequently, there is a rise in CS-associated complications [6]. Surgical site infection (SSI) is one of the CS complications which occur following bacterial invasion of the CS incision [7, 8].
The incidence of post-CS SSI is 11% in low- and middle-income countries, 20% in Africa [8], and under 10% in the UK [9].
Post-CS SSI is the main cause of prolonged hospital stays and healthcare system burden after CSs [7]. The World Health Organization (WHO) reported that the SSI contributes to more than 400,000 extra days of hospital stays in the USA at a cost of an additional US$ 10 billion per year [8]. In addition, the post-CS SSI increases the postoperative hospital stays threefold in the UK [9]. Previous studies recommended the use of preoperative prophylactic antibiotics and standard infection control protocols to reduce the post-CS SSI risk [7, 10]. Therefore, this comparative study is designed to evaluate the outcome of the implemented post-CS SSI prevention protocol in Ahmadi Hospital, Kuwait.
Methods
This comparative study was conducted in the Obstetrics and Gynecology Department of Ahmadi Hospital, Kuwait Oil Company (KOC), after approval of the institute ethical committee and informed consents. The trial was registered under the trial number ACTRN12618000483257 [11].
Data of women between 18 and 40 years old, who delivered by ERCS after the implemented post-CS SSI prevention protocol, were collected and included in the study group. The hospital records were reviewed, and data of women who delivered by ERCS before the implemented protocol were collected and included in the control group.
Women who delivered by emergency CSs and refused to participate and/or give consent were excluded from this study.
Collected preoperative data include age, obstetrics history, number of previous CSs, body mass index (BMI), preoperative medical disorders (anemia and/or diabetes), prolonged rupture of membranes (ROM), and/or chorioamnionitis before the ERCS.
Collected intraoperative data include the duration of the ERCS, surgical difficulties/adhesions, and blood transfusion during or after the ERCS.
Postoperative collected data include postoperative anemia, wound condition (especially the post-CS SSI), duration of hospital stay, antibiotic doses, and culture results.
The study group who delivered by ERCS after the post-CS SSI prevention protocol was monitored for signs and symptoms of SSI during their hospital stay after the current ERCS and for 30 days after hospital discharge in the outpatient department (OPD). Wound complications were recorded, notified to the infection control team, and managed according to the hospital protocol.
Post-CS SSI occurs following bacterial invasion of the CS incision [7, 8]. Superficial SSI is defined as a purulent discharge from the skin and subcutaneous tissue of the incision site. Deep SSI is defined as a discharging wound with deep tissue involvement and abscess formation, whereas an organ/space infection is a combination of deep SSI characteristics and extension beyond the fascial/muscle layers [7].
The approved Ahmadi Hospital post-CS SSI prevention protocol includes (1) strict glycemic control in diabetic women before the CS [12], (2) preoperative antiseptic showering with 4% chlorhexidine gluconate the night before the ERCS [12,13,14], (3) administration of prophylactic intravenous antibiotics 60 min before the skin incision [15], (4) higher dose of preoperative antibiotics in obese women (prepregnancy weight of 90–100 kg) [12, 15], (5) the use of clippers for hair removal preoperatively [12], (6) the use of chlorhexidine-alcohol for skin preparation immediately before the ERCS [11,12,13,14], (7) the use of an alcohol-based hand rub as a preoperative antiseptic [13], (8) closure of the skin using subcuticular sutures [12, 16], (9) closure of the subcutaneous tissue (SC) if the SC thickness is more than or equal 2 cm [13], and (10) avoidance of unproven techniques [13].
The primary outcome measure is the incidence of post-CS SSI after and before the implemented post-CS SSI prevention protocol. The secondary outcome measures are the risk factors which may predispose to post-CS SSI as the number of the previous CSs, overweight, obesity, preoperative anemia, pregestational diabetes (pre-existing diabetes before pregnancy), prolonged ROM (ROM more than 24 h prior to labor), chorioamnionitis, duration of current ERCS (more than 1 h), surgical difficulties during the current ERCS, postoperative anemia, and/or blood transfusion.
The American Congress of Obstetricians and Gynecologists (ACOG) recommends the use of a single dose of the first-generation cephalosporin (cefazolin 2 g) or single-dose combination of clindamycin (900 mg) with an aminoglycoside for those with significant penicillin allergy, as preoperative prophylaxis before CS [15].
Chorioamnionitis is diagnosed by uterine tenderness, maternal leucocytosis, positive C-reactive proteins, pro-calcitonin, and leucocyte esterase [17].
Sample Size
The required sample size was calculated using G*Power software version 3.17 for sample size calculation (Heinrich Heine Universität; Düsseldorf; Germany), setting α-error probability at 0.05, power (1-β error probability) at 0.95%, and effective sample size (w) at 0.5. The effective sample of more than or equal to 220 women in two groups (study group and controls) needed to produce a statistically acceptable figure.
Statistical Analysis
Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 20 (IBM Corporation, Chicago, Illinois, USA). Numerical variables are presented as mean and standard deviation (±SD), while categorical variables are presented as number and percentage (%). Student’s t test was used for the analysis of quantitative data and chi-square (x2) test for analysis of qualitative data. The relative risk (RR) of different variables which may predispose to post-CS SSI was also calculated. A P value < 0.05 was considered significant.
Results
A total of 229 women who delivered by ERCS are included in this study: 112 women who delivered by ERCS after the implemented protocol (study group) compared to 117 controls (who delivered by ERCS before the implemented protocol), to evaluate the outcome of the implemented post-CS SSI prevention protocol in Ahmadi Hospital, Kuwait.
The incidence of post-CS SSI was significantly high in the controls (who delivered by ERCS before the protocol) compared to the study group (who delivered by ERCS after the protocol) (12.8% (15/117) versus 3.6% (4/112), respectively) (P = 0.01) (Table 1).
The two studied groups were matched with no difference regarding the number of the previous CSs before the current ERCS and number of overweight (BMI 25–29.9 kg/m2) and obese (BMI more than or equal to 30 kg/m2) women included in each group. The study and control groups were also matched with no difference regarding the number of women with pregestational (pre-existing) diabetes (15/112 (13.4%) versus 21/117 (17.9%), respectively) (P = 0.4), number of women with prolonged ROM and chorioamnionitis (1/112 (0.9%) and 1/112 (0.9%) versus 6/117 (5.13%) and 5/117 (4.27%)), respectively) (P = 0.07 and 0.1, respectively) included in each group (Table 1).
The rates of surgical difficulties/adhesions and duration of the current ERCS more than 1 h were similar with no difference between the two studied groups (0.9% in the study group versus 5.13% in controls; P = 0.07). The rate of preoperative and postoperative moderate anemia was significantly high in the controls (3.42% (4/117) and 7.7% (9/117), respectively) compared to that of the study group (0% (0/112) and 0.9% (1/112), respectively) (P = 0.01 and 0.01, respectively). In addition, the blood transfusion rate was significantly high in the controls compared to that of the study group (7.7% (9/117) versus 0.9% (1/112), respectively) (P = 0.01) (Table 1).
The relative risk (RR) of different variables which may predispose to post-CS SSI was calculated and showed that the obesity and pregestational diabetes were significant risks for post-CS SSI (RR 0.35 (95%CI; 0.13–0.99) P = 0.04 and RR 0.24 (95%CI; 0.063–0.93) P = 0.03, respectively). In addition, the prolonged ROM before the ERCS, duration of ERCS (more than 1 h), and surgical difficulties/adhesions during the ERCS were significant risks for post-CS SSI (RR 6.0 (95%CI; 1.003–35.9) P = 0.04, RR 6.0 (95%CI; 1.003–35.9) P = 0.04, and RR 6.0 (95%CI; 1.003–35.9) P = 0.04, respectively) (Table 2).
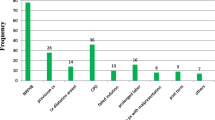
The post-CS SSI cases and risk factors of post-CS SSI in the two studied groups were summarized in Fig. 1.
The mean hospital stay was significantly high in the post-CS SSI cases (19 cases in the two studied groups) compared to (210 cases) noninfected cases (7.3 ± 2.9 days versus 3.2 ± 1.7, respectively) (P = 0.0001). In addition, the mean number of antibiotic doses was significantly high in post-CS SSI cases compared to noninfected cases (22.5 ± 2.4 versus 2.02 ± 1.6, respectively) (P = 0.003). The post-CS SSI was superficial in 89.5% (17/19), while it was deep SSI in 10.5% (2/19). The culture results of the post-CS SSI cases showed Staphylococcus aureus in 78.9% (15/19), Escherichia coli in 15.8% (3/19), and no growth in 5.3% (1/19) (Table 3).
Discussion
Post-CS SSI is the main cause of prolonged hospital stays and healthcare system burden after CSs [7]. The post-CS SSI risk can be significantly reduced after the use of standard infection control protocols [7, 10]. Therefore, 229 women who delivered by ERCS were included in this study to evaluate the outcome of the post-CS SSI prevention protocol in Ahmadi Hospital, Kuwait.
Women who delivered by ERCS after the implemented protocol were included in the study group (112 women), and the data were compared to that of women who delivered by ERCS before the protocol (117 women).
The two studied groups were matched with no difference regarding the number of the previous CSs before the current ERCS, number of overweight (P = 0.4) and obese women (P = 1.0), number of women with pregestational diabetes (P = 0.4), and number of women with prolonged ROM (P = 0.07) and chorioamnionitis (P = 1.0) included in each group. In addition, the rates of surgical difficulties/adhesions and duration of the current ERCS more than 1 h were similar with no difference between the two studied groups (P = 0.07 and 0.7, respectively).
The incidence of post-CS SSI was significantly high in the controls (who delivered by ERCS before the protocol) compared to the study group (who delivered by ERCS after the protocol) (12.8% (15/117) versus 3.6% (4/112), respectively) (P = 0.01).
The implemented post-CS SSI prevention protocol was the main cause behind the reduced rate of post-CS SSI between the two studied groups. Similarly, Alfouzan et al. and Krieger et al. concluded that the post-CS SSI risk can be significantly reduced after the use of preoperative prophylactic antibiotics and standard infection control protocols [7, 10].
Although the incidence of post-CS SSI is under 10% in the UK [9] and 3.1% in Poland [18], the reported incidence of post-CS SSI was as high as 11% in low- and middle-income countries, 20% in Africa [8], 11.0% in Wodajo et al.’s study [19], 12.6% in Shrestha et al.’s study [20], and 11.7% in Wendmagegn et al.’s study [21].
The implemented post-CS SSI prevention protocol includes the administration of prophylactic intravenous antibiotics 60 min before the skin incision and a higher dose of preoperative antibiotics in obese women [12, 15].
Similarly, Liu et al. found that the antibiotic prophylaxis given in the proper time before the CSs reduces the post-CS SSI risk [22]. Scholz et al. reported that the use of routine antibiotic prophylaxis (cefazolin or gentamicin/clindamycin for penicillin-allergic patients) as a prevention bundle was effective to reduce the post-CS SSI [23], while Ben Shoham et al. found that the SSI rates after CS were similar with no difference when the prophylactic antibiotics are given before surgery or after cord clamping [24].
The implemented protocol also includes preoperative antiseptic showering with 4% chlorhexidine gluconate the night before ERCS [12,13,14] and the use of chlorhexidine-alcohol for skin preparation immediately before the ERCS [11,12,13,14].
Although, Corcoran et al. found that the use of 2% ChloraPrep for skin disinfection before incision leads to a significant reduction in post-CS SSI rate [25]. A recent Cochrane review concluded that it is not yet clear what sort of skin preparation may be most effective for preventing post-CS SSI [26].
In addition, the implemented protocol includes the use of clippers for hair removal preoperatively [12], closure of the skin using subcuticular sutures [12, 16], and avoidance of unproven techniques [13].
Cocoran et al. concluded that the use of nonabsorbable sutures for skin closure and clippers instead of razors before incision leads to a significant reduction in SSI rate [25]. Similarly, Shrestha et al. reported the use of interrupted skin sutures as a risk for post-CS SSI [20].
In addition, Liu et al. found that the use of adhesive drapes increases the SSI risk [22], and Mahomed et al. found that the povidone-iodine irrigation before skin closure is of no benefit in post-CS SSI prevention [27].
The RR analysis done in this study showed that the obesity and pregestational diabetes were significant risks for post-CS SSI (RR 0.35 (P = 0.04) and RR 0.24 (P = 0.03), respectively). In addition, the prolonged ROM before the ERCS, duration of ERCS (more than 1 h), and surgical difficulties/ adhesions during the ERCS were significant risks for post-CS SSI (RR 6.0 (P = 0.04), RR 6.0 (P = 0.04), and RR 6.0 (P = 0.04), respectively).
Shrestha et al. reported the emergency CSs, ROM before the CSs, and vertical incisions as possible risks for post-CS SSI [20]. Wendmagegn et al. found the PROM, prolonged labor, rural setting, and chorioamnionitis were independent risks for SSI after CSs [21]. Wodajo et al. found that the prolonged labor, prolonged ROM, and prolonged duration of surgery increased odds of post-CS SSI (6.78, 5.83, and 12.32, respectively) [19]. In addition, Shikha et al. concluded that the emergency CS, obstructed labor, prolonged ROM, and prolong the duration of operation are possible considerable risks for post-CS SSI [28].
However, the RR analysis in this study showed that the moderate anemia (either pre- or postoperative) and blood transfusion (during or after the ERCS) were not risk factors for post-CS SSI (P = 0.7, 0.1, and 0.1, respectively). Wendmagegn et al. reported the blood loss during CSs as an independent risk for post-CS SSI [21]. In addition, Wodajo et al. [19] and Shikha et al [28] reported postoperative anemia as a significant predictor for post-CS SSI. The difference between this study and other studies regarding the postoperative anemia and blood loss during or after CSs as possible risks for post-CS SSI can be explained by (1) our medical team awareness of postoperative anemia, and its consequences on wound complications, and (2) our hospital policy which necessitates correction of the intraoperative blood loss in order to maintain the postoperative hemoglobin after CSs more than or equal 10 g%.
The mean hospital stays and mean antibiotic doses were significantly high in the post-CS SSI cases compared to those of the noninfected cases (P = 0.0001 and 0.003, respectively).
Alfouzan et al. reported the post-CS SSI as the main cause of prolonged hospital stays and healthcare system burden after CSs [7]. In addition, Saeed et al. reported that the post-CS SSI increases the postoperative hospital stays threefold in the UK [9].
The culture results of the post-CS SSI cases showed Staphylococcus aureus in 78.9% (15/19) and Escherichia coli in 15.8% (3/19). Similarly, Shikha et al. found that 85% of the SSI after CS occurred by Staphylococcus aureus and 15% by Escherichia coli [28].
The current study found that the incidence of post-CS SSI after ERCSs significantly reduced from 12.8 to 3.6% following the post-CS SSI prevention protocol. In addition, the current study found that obesity, pregestational diabetes, prolonged ROM, duration of ERCS (more than 1 h), and surgical difficulties/adhesions during the ERCSs were definite risks for post-CS SSI.
The current study was the first registered, comparative study conducted in Kuwait, following a definite SSI prevention protocol to reduce the incidence of post-CS SSI after ERCSs.
Incomplete records of the controls (delivered by ERCSs) before the implemented protocol was the only limitation faced during this study.
We recommend worldwide the use of effective post-CS SSI prevention protocols or guidelines to reduce the post-CS SSI and its consequences of prolonged hospital stays and healthcare system burden.
Conclusion
The incidence of post-CS SSI after ERCS was significantly reduced following the post-CS SSI prevention protocol. Obesity, pregestational diabetes, prolonged ROM, duration of ERCS (more than 1-h), and surgical difficulties/adhesions during the ERCS were the definite risks for post-CS SSI.
Data Availability
The datasets analyzed during the current study are not publicly available due to the concern for patient safety and confidentiality but are available from the corresponding author upon reasonable request.
References
Abdelazim IA, Elbiaa AA, Al-Kadi M, Yehia AH, Sami Nusair BM, Faza MA. Maternal and obstetrical factors associated with a successful trial of vaginal birth after cesarean section. J Turk Ger Gynecol Assoc. 2014;15(4):245–9. https://doi.org/10.5152/jtgga.2014.14104.
Vogel JP, Oladapo OT, Manu A, Gülmezoglu AM, Bahl R. New WHO recommendations to improve the outcomes of preterm birth. Lancet Glob Health. 2015;3(10):e589–90. https://doi.org/10.1016/S2214-109X(15)00183-7.
Molina G, Weiser TG, Lipsitz SR, Esquivel MM, Uribe-Leitz T, Azad T, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2015;314(21):2263–70. https://doi.org/10.1001/jama.2015.15553.
Abdelazim I, Alanwar A, Svetlana S, Sakiyeva K, Farghali M, Mohamed M, et al. Complications associated with higher order compared to lower order cesarean sections. J Matern Fetal Neonatal Med. 2020;33(14):2395–402. https://doi.org/10.1080/14767058.2018.1551352.
Tapia V, Betran AP, Gonzales GF. Cesarean Section in Peru: Analysis of Trends using the Robson classification system. PLoS One. 2016;11(2):e0148138. https://doi.org/10.1371/journal.pone.0148138.
Sakiyeva KZ, Abdelazim IA, Farghali M, Zhumagulova SS, Dossimbetova MB, Sarsenbaev MS, et al. Outcome of the vaginal birth after cesarean section during the second birth order in West Kazakhstan. J Fam Med Prim Care. 2018;7(6):1542–7. https://doi.org/10.4103/jfmpc.jfmpc_293_18.
Alfouzan W, Al Fadhli M, Abdo N, Alali W, Dhar R. Surgical site infection following cesarean section in a general hospital in Kuwait: trends and risk factors. Epidemiol Infect. 2019;147:e287. https://doi.org/10.1017/S0950268819001675.
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276–87. https://doi.org/10.1016/S1473-3099(16)30398-X.
Saeed KBM, Greene RA, Corcoran P, O'Neill SM. Incidence of surgical site infection following caesarean section: a systematic review and meta-analysis protocol. BMJ Open. 2017;7(1):e013037. https://doi.org/10.1136/bmjopen-2016-013037.
Krieger Y, Walfisch A, Sheiner E. Surgical site infection following cesarean deliveries: trends and risk factors. J Matern Fetal Neonatal Med. 2017;30(1):8–12. https://doi.org/10.3109/14767058.2016.1163540.
http://www.ANZCTR.org.au/ACTRN12618000483257.aspx. The outcome of the hospital protocol for prevention of surgical site infection during cesarean deliveries. Last accessed 16/11/2020.
Conroy K, Koenig AF, Yu YH, Courtney A, Lee HJ, Norwitz ER. Infectious morbidity after cesarean delivery: 10 strategies to reduce risk. Rev Obstet Gynecol. 2012;5(2):69–77.
Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2015;28(5):573–7. https://doi.org/10.3109/14767058.2014.926884.
Shen NJ, Pan SC, Sheng WH, Tien KL, Chen ML, Chang SC, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center. J Microbiol Immunol Infect. 2015;48(3):322–8. https://doi.org/10.1016/j.jmii.2013.08.005.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–83. https://doi.org/10.1097/AOG.0b013e3182238c31.
Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis. Am J Obstet Gynecol. 2015;212(5):621.e1–10. https://doi.org/10.1016/j.ajog.2014.12.020.
Cataño Sabogal CP, Fonseca J, García-Perdomo HA. Validation of diagnostic tests for histologic chorioamnionitis: systematic review and meta-analysis. Eur J Obstet Gynecol Reprod. 2018;228:13–26. https://doi.org/10.1016/j.ejogrb.2018.05.043.
Różańska A, Jarynowski A, Kopeć-Godlewska K, Wójkowska-Mach J, Misiewska-Kaczur A, Lech M, et al. Does surgical site infection after caesarean section in Polish hospitals reflect high-quality patient care or poor postdischarge surveillance? Results from a 3-year multicenter study. Am J Infect Control. 2018;46(1):20–5. https://doi.org/10.1016/j.ajic.2017.07.025.
Wodajo S, Belayneh M, Gebremedhin S. Magnitude and factors associated with post-cesarean surgical site infection at Hawassa University Teaching and Referral Hospital, Southern Ethiopia: a cross-sectional study. Ethiop J Health Sci. 2017;27(3):283–90. https://doi.org/10.4314/ejhs.v27i3.10.
Shrestha S, Shrestha R, Shrestha B, Dongol A. Incidence and risk factors of surgical site infection following cesarean section at Dhulikhel Hospital. Kathmandu Univ Med J. 2014;12(46):113–6. https://doi.org/10.3126/kumj.v12i2.13656.
Wendmagegn TA, Abera GB, Tsehaye WT, Gebresslasie KB, Tella BG. Magnitude and determinants of surgical site infecion among women underwent cesarean section in Ayder comprehensive specialized hospital Mekelle City, Tigray region, Northern Ethiopia, 2016. BMC Pregnancy Childbirth. 2018;18(1):489. https://doi.org/10.1186/s12884-018-2075-8.
Liu Z, Dumville JC, Norman G, Westby MJ, Blazeby J, McFarlane E, et al. Intraoperative interventions for preventing surgical site infection: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2018;2(2):CD012653. https://doi.org/10.1002/14651858.CD012653.pub2.
Scholz R, Smith BA, Adams MG, Shah M, Brudner C, Datta A, et al. A Multifaceted surgical site infection prevention bundle for cesarean delivery. Am J Perinatol. 2019. https://doi.org/10.1055/s-0039-3400993.
Ben Shoham A, Bar-Meir M, Ioscovich A, Samueloff A, Wiener-Well Y. Timing of antibiotic prophylaxis in cesarean section: retrospective, difference-in-differences estimation of the effect on surgical-site-infection. J Matern Fetal Neonatal Med. 2019;32(5):804–8. https://doi.org/10.1080/14767058.2017.1391784.
Corcoran S, Jackson V, Coulter-Smith S, Loughrey J, McKenna P, Cafferkey M. Surgical site infection after cesarean section: implementing 3 changes to improve the quality of patient care. Am J Infect Control. 2013;41(12):1258–63. https://doi.org/10.1016/j.ajic.2013.04.020.
Hadiati DR, Hakimi M, Nurdiati DS, da Silva Lopes K, Ota E. Skin preparation for preventing infection following caesarean section. Cochrane Database Syst Rev. 2018;10(10):CD007462. https://doi.org/10.1002/14651858.CD007462.pub4.
Mahomed K, Ibiebele I, Buchanan J. The Betadine trial - antiseptic wound irrigation prior to skin closure at caesarean section to prevent surgical site infection: A randomized controlled trial. Aust N Z J Obstet Gynaecol. 2016;56(3):301–6. https://doi.org/10.1111/ajo.12437.
Shikha SS, Latif T, Moshin M, Hossain MA, Akter H, Shamsi S, et al. Evaluation of surgical site infection among post cesarean patients in Mymensingh Medical College Hospital. Mymensingh Med J. 2018;27(3):480–6.
Acknowledgments
The authors are grateful to the women who agreed and gave consent to participate in this study.
Financial Disclosure
Nil.
Author information
Authors and Affiliations
Contributions
Ibrahim A. Abdelazim (IAA) is responsible for the study concept and design, data collection, registration of the trial, final revision before publication, and submission for publication.
Mohannad Abu-Faza (MAF) is responsible for the study design, data collection, Microsoft editing, and final revision before publication.
Soud Al-Ajmi (SAA) is responsible for the study concept, data collection, and revision, ethical approval, intellectual content, and final revision before publication.
M. Farghali (MF) is responsible for the study concept, data collection, and revision, Microsoft editing, statistical analysis, and final revision before publication.
Svetlana Shikanova (SS) is responsible for the study concept, data collection, and revision, intellectual content, reference update, and final revision before publication.
Corresponding author
Ethics declarations
Ethical Approval
The study was approved by Ahmadi Hospital ethical committee and registered under the trial number ACTRN12618000483257.
Conflict of Interest
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Rights and permissions
About this article
Cite this article
Abdelazim, I.A., Abu-Faza, M., Al-Ajmi, S. et al. The Outcome of the Hospital Protocol for Prevention of Surgical Site Infection After Cesarean Deliveries. SN Compr. Clin. Med. 3, 862–869 (2021). https://doi.org/10.1007/s42399-021-00777-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00777-8