Abstract
Maintaining arch length and integrity by preserving the pulpally involved tooth, as a natural space maintainer is the main aim of primary tooth pulp therapy. Pulpotomy and pulpectomy, the two major procedures used to perform pulp therapy in primary teeth, have evolved over the years. This paper will discuss contemporary pediatric endodontic concepts and definitive indications and contraindications for primary tooth pulp therapy. It will include a step-by-step description of both the mineral trioxide aggregate pulpotomy and a single-visit pulpectomy using rotary files in primary posterior teeth. The high-resolution clinical pictures and the clinical tips will help the reader achieve predictable prognosis when carrying out these valuable procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Quick reference/description
The main aim of performing pulp therapy in primary teeth is the preservation of the pulpally involved teeth until exfoliation to maintain arch integrity and length by acting as natural space maintainers. Appropriate case selection is essential to ensure normal eruption of a healthy permanent successor. A successful outcome of pulp therapy depends on the careful execution of each step of the treatment protocol.
Overview
Treatment modality | Indications | Contraindications |
|---|---|---|
Mineral trioxide aggregate (MTA) pulpotomy Note: The selective removal of carious tissue to soft dentine in deep carious lesions reduces the need for a pulpotomy procedure | Primary tooth with reversible pulpitis in the following scenarios: Unreliable pain history complicated by age of the child and the presence of several teeth with deep caries in the same side of the oral cavity Absence of a layer of mineralized dentin between the carious lesion and the pulp on the radiograph Unintentional pulp exposure during caries excavation | Primary tooth with irreversible pulpitis |
Single-visit pulpectomy | Primary tooth with irreversible pulpitis that is restorable with a full-coverage restoration following pulpectomy Inadequate control of bleeding from root canal orifices during pulpotomy suggestive of inflamed pulp tissue in the root canals | Patients with systemic diseases like congenital heart disease, nephrotic syndrome, etc. Presence of cellulitis associated with suspected tooth In case of the radiographic appearance of infected tooth showing: Advanced internal resorption Excessive external resorption involving more than 1/3rd of the root Interradicular lesion involving the crypt of the successor Severe bone loss causing tooth mobility Perforation in the furcation area |
Materials/instruments
-
Sterile round bur
-
Saline
-
Cotton pellets
-
1% sodium hypochlorite
-
Mineral trioxide aggregate (MTA)
-
Resin-modified glass ionomer cement (RMGIC)
-
Preformed metal or Stainless Steel crown
-
Rubber dam
-
Endodontic hand file
-
Electronic apex locator
-
Flexible nickel titanium (Ni–Ti) rotary files
-
Paper points
-
Calcium hydroxide-iodoform paste (Vitapex, J Morita Corporation, Japan)
-
Disposable syringe for irrigation
Procedure
Premature loss of primary teeth may result in reduced masticatory efficiency, loss of arch length, and esthetic and functional impairment. Therefore, in primary teeth, pulp therapy is performed with different objectives as compared to pulp therapy in permanent teeth. The purpose of pulp therapy in primary teeth is the preservation of the pulpally involved teeth until exfoliation, to maintain the length and integrity of the dental arch by allowing the treated teeth to act as natural space maintainers. Appropriate case selection for pulp therapy ensures proper eruption of a healthy permanent successor. Careful execution of the standard treatment protocol results in the successful outcome of pulp therapy in primary teeth.
MTA pulpotomy
Pulpotomy is the removal of the coronal part of the pulp and insertion of a pharmacotherapeutic medicament for the preservation of the remaining vital pulp within the root canals. Pulpotomy was initially considered a definitive treatment protocol for the management of primary teeth with reversible pulpitis. The requirement of pulpotomy in primary teeth has considerably reduced over time with the introduction of the technique of selective removal of carious tissue.
Despite the introduction of the selective removal of carious tissue technique for the management of deep carious lesions, pulpotomy is required in specific cases of reversible pulpitis. To perform pulpotomy, the infection or inflammation in the affected tooth should be restricted to the coronal pulp only. Hence, the operator should be careful during case selection. While considering a primary tooth for pulpotomy, it is essential to confirm the diagnosis of reversible pulpitis and differentiate it from irreversible pulpitis.
Rationale for MTA pulpotomy
Pulpotomy is usually performed in primary teeth with reversible pulpitis, where the inflammation is confined to the coronal portion of the pulp. This procedure helps to preserve the vitality of the radicular pulp. Consequently, performing a pulpotomy also preserves the pulpally involved tooth in the arch till its exfoliation, which in turn maintains arch length and integrity since the tooth acts as a natural space maintainer.
Traditionally, 1/5th dilution formocresol was used as a pharmacotherapeutic medicament in primary tooth pulpotomy but it does not maintain the vitality of radicular pulp as it devitalizes the pulp tissue in toto. Pulpotomy can also be performed using 15% ferric sulfate, silicate-based cements, carbon dioxide laser or electrocautery. Ferric sulfate can mask a diagnosis of irreversible pulpitis as it can stop bleeding from the hyperemic pulp in the root canals. It also does not seal the pulpal floor leaving accessory communication channels between the pulp chamber and surrounding tissue open.
Using MTA as an agent for pulpotomy helps to maintain the health and vascularity of the radicular pulp after sealing the canal orifices. It also seals the accessory canals in the floor of the pulp and resists bacterial microleakage. Biodentine can be used as an alternative to MTA.
Clinical procedure of MTA pulpotomy
Initial preoperative clinical and radiographic examination of the tooth involved is performed (Fig. 1a, b). The tooth is assessed for signs and symptoms of irreversible pulpitis like spontaneous and unprovoked pain that lingers (except from food lodgment), tenderness to percussion, mobility and presence of an abscess or draining sinus. Such teeth are contraindicated for the procedure. Radiographically, a deep carious lesion is noted with an absence of a layer of mineralized dentin between the carious lesion and the pulp. No signs of internal resorption, interradicular bone loss or pulp calcifications are seen. The decision to perform MTA pulpotomy is made after confirming the diagnosis of reversible pulpitis. The procedure of MTA pulpotomy is performed as follows (Fig. 1):
MTA pulpotomy in a primary lower molar. a Clinical examination showing temporary restoration in tooth 75. b Radiograph showing deep carious lesion approximating the distal pulp horn without a visible layer of dentine separating the carious lesion and the pulp. No pulpal calcifications, interradicular bone loss or internal resorption was noted. c A deep carious lesion with soft carious tissue debris seen after removal of temporary restorative cement. d Complete excavation of carious tissue followed by complete unroofing of the pulp performed using a new sterile bur. e Coronal pulp amputation performed with a sterile slow speed round bur. f Hemorrhage controlled with the application of cotton pellets soaked in saline and blot dried, under moderate pressure. g Hemostasis achieved in all canal orifices. h Pulp chamber swept with a cotton pellet soaked in 1% sodium hypochlorite. i MTA placed on the root canal orifices and pulpal floor. MTA condensed with moist dry cotton pellets. j RMGIC placed over the MTA. k Cementation of a preformed metal crown. l Immediate postoperative radiograph. m Healing after 1 week of placement of crown. n, o Clinical and radiographic view after 4 years showing excellent healing, healthy periradicular tissues and the normal eruption of the permanent first molar
-
Adequate local anesthesia is achieved prior to the initiation of the pulpotomy procedure. The tooth is then isolated, under a rubber dam (Fig. 1c).
-
Complete removal of carious tissue is essential before pulp exposure to prevent iatrogenic infection of the pulp tissue (Fig. 1d).
-
An access cavity is prepared using a sterile bur for complete unroofing of the pulp chamber (Fig. 1d). It should be done without leaving any undercuts to allow easy removal of the entire coronal pulp and prevent persistent bleeding.
-
A sterile slow speed round bur is used for amputation of the coronal pulp (Fig. 1e). It is important to eliminate all filaments of pulp.
-
Thorough debridement of the pulp chamber is performed using saline.
-
Hemorrhage from the pulp chamber is controlled by applying moderate pressure with saline soaked and blot dried cotton pellets over the root canal orifices (Fig. 1f). Dry cotton pellets should not be used as they may engage the blood clot and induce hemorrhage.
-
Hemostasis should be achieved within 5 min (Fig. 1g). Administration of intrapulpal anesthesia or a hemostatic agent should be avoided. These may mask persistent bleeding which indicates inflammation of the radicular pulp. A pulpectomy should be performed if bleeding persists. However, all parameters of case selection should be considered while deciding to proceed with a pulpectomy.
-
A cotton pellet soaked in 1% sodium hypochlorite is used to sweep the pulp chamber once for achieving an antibacterial effect (Fig. 1h).
-
An adherent mix of MTA is placed on the pulpal floor and over the root canal orifices (Fig. 1i). It is condensed to a uniform thickness under gentle pressure with moistened, blot dried cotton pellets. MTA is condensed on the floor, to plug all accessory canals.
-
RMGIC is placed over the MTA to form a hermetic seal (Fig. 1j). As MTA has a prolonged setting time, it is permitted to set below the RMGIC. A temporary restoration can also be used as an alternative to RMGIC. However, use of a temporary restoration necessitates a second appointment for placement of a final restoration thereby increasing the risk of compromising the coronal seal.
-
A preformed metal crown is cemented over the RMGIC restoration to achieve a good coronal seal (Fig. 1k). The crown should be placed in the same appointment or as soon as practically possible. If the coronal tooth structure is adequate thereby ensuring a stable restoration and coronal seal, the use of a preformed metal crown may be omitted.
-
A postoperative radiograph is obtained for future reference and to evaluate treatment outcome (Fig. 1l). On follow-ups, the success of the treatment is evident from stable restorations, healthy periapical tissue, physiologic root resorption and eruption of the permanent tooth (Fig. 1m–o).
Single-visit pulpectomy
Pulpectomy in the primary teeth involves complete extirpation of the pulp tissue followed by obturation of the root canals with an appropriate resorbable material. The popularity and clinical acceptance of the pulpectomy procedure have increased considerably due to its long-term success. Pulpectomy can be a complex procedure due to the torturous nature of root canals, resorbing primary tooth roots, and young children requiring behavior guidance.
Pulpectomy is indicated in teeth with a diagnosis of irreversible pulpitis without accompanying signs of internal or excessive root resorption, interradicular lesion affecting the permanent successor, severe bone loss, mobility or perforation in the furcal area. Managing a pulpally involved primary tooth with pulpectomy preserves the treated tooth until exfoliation.
Rationale for single-visit pulpectomy
Pulpectomy of a primary tooth preserves the affected tooth to maintain the length and integrity of the dental arch until exfoliation by acting as a natural space maintainer. Traditionally, pulpectomy of primary teeth was considered a complex procedure requiring multiple dental visits. The reasons for the evolution of pulpectomy into a single-visit procedure are:
-
Availability of long-term success data
-
Development of standard anxiety management protocols such as inhalation sedation
-
Availability of easy-to-use obturating materials
-
Clinical introduction of apex locators in primary teeth
-
Rotary endodontics in primary teeth
It is best to avoid a multiple-visit pulpectomy as it results in several stressful appointments causing treatment fatigue and loss of cooperation. A viable treatment alternative to a multiple-visit pulpectomy is extraction followed by space maintenance.
Clinical procedure of single-visit pulpectomy
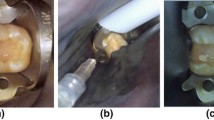
Preoperative clinical and radiographic examinations of the involved tooth are performed (Fig. 2a, b). The tooth is assessed for signs and symptoms of irreversible pulpitis. The restorability of the tooth is also considered. Radiographic examination shows a deep carious lesion in continuation with the coronal pulp and adequate root length. No signs of internal resorption, interradicular bone loss or pulp calcifications are seen. The decision to perform single-visit pulpectomy is made after confirming the diagnosis of irreversible pulpitis with no associated mobility. The procedure of single-visit pulpectomy is performed as follows (Fig. 2):
Single-visit pulpectomy in a primary lower molar. a Clinical examination showing a deep carious lesion in tooth 85. b Preoperative radiograph showing a deep carious lesion in continuation with the pulp chamber with no evidence of floor perforation, bone loss or internal resorption. c Isolation of tooth 85 with rubber dam followed by access opening to expose the coronal pulp tissue. d Measurement of working length using endodontic hand file and electronic apex locator. e Preparation of canals with rotary files. f Gentle irrigation of canals with 1% sodium hypochlorite. g Enlarged and clean root canal orifices following completion of biomechanical preparation. h Drying of canals with paper points. i Obturation of the canals by inserting a syringe tip containing calcium hydroxide-iodoform paste into the canal. j Complete obturation of all four canals. k Core build-up using RMGIC. l Cementation of Hall crown after removal of the rubber dam clamp. m Immediate postoperative radiograph showing adequate obturation and well-fitting crown. n Radiographic view at a 3-year follow-up showing stable restoration, healthy periradicular tissues and the normal eruption of the permanent first molar. o Clinical examination at a 5-year follow-up showing stable restoration, healthy soft tissue and normally erupted permanent first molar. p Radiographic view at a 5-year follow-up showing almost complete resorption of the roots of tooth 85 and normal eruption of tooth 45
-
Adequate local anesthesia is achieved prior to the initiation of the pulpectomy procedure. The tooth is then isolated, under rubber dam (Fig. 2c).
-
Complete removal of carious tissue is essential before pulp exposure (Fig. 2c).
-
An access cavity is prepared using a sterile bur for complete unroofing of the pulp chamber (Fig. 2c). It should be done leaving no undercuts thus gaining straight-line access to all root canals.
-
The canal orifices are identified, and the working length of each canal is determined. Traditionally, the working length was calculated from a radiograph with an endodontic hand file placed in the canal. The working length was considered about 2 mm short of the measured value to avoid over-extension.
-
Use of electronic apex locators provides an accurate value of working length while simultaneously reducing the exposure to ionizing radiation in pediatric patients. The working length is determined by attaching the file clip of the electronic apex locator to the endodontic hand file and insertion of the file into each of the root canals (Fig. 2d).
-
All the canals are then prepared with rotary endodontic files up to the estimated working length (Fig. 2e). Flexible hand or rotary instruments made of nickel-titanium (Ni–Ti) metal alloy are required to negotiate the thin root canals of primary teeth. Use of rotary instruments distinctly reduces the treatment time. Use of a passive rotary system is recommended during rotary preparation in primary teeth.
-
Mechanical preparation of the root canals is followed by gentle irrigation of the canals with 1% sodium hypochlorite (Fig. 2f). A combination of mechanical and chemical debridement is essential during pulpectomy as primary teeth generally contain multiple microscopic accessory canals extending between the pulpal floor and the furcation area along with several ramifications in the root canals.
-
Clean and enlarged root canal orifices and a convex pulpal floor are observed following biomechanical preparation (Fig. 2g). Adequate access to the apical third of the root canal requires proper enlargement of the root canal orifices. This ensures sufficient cleaning and shaping of the canals. Each rotary file system has specific files for management of the coronal third of the root canals.
-
Following adequate cleaning and shaping of the root canals, paper points are used to dry the canals (Fig. 2h). For improved moisture absorption, the paper points should be left in each root canal for a few seconds before removing them.
-
Obturation is performed only after the canals are completely dry and free of exudate.
-
The canals are commonly obturated using a calcium hydroxide-iodoform paste that is injected into the canals via a syringe tip (Fig. 2i). The tip of the syringe containing the calcium hydroxide-iodoform paste (Vitapex, J Morita Corporation, Japan) is placed into the dry root canal just short of the working length. The canals are obturated in a backfill manner by withdrawing the syringe while injecting the material into the canal. Alternatively, Zinc Oxide Eugenol paste or Endoflas can be used as obturating materials.
-
After obturation of each canal, the paste is compressed in the canal orifice using a moist cotton pellet (Fig. 2j). The calcium hydroxide-iodoform paste dispensed in a syringe fulfills all the criteria of an ideal obturating material for use in primary teeth.
-
Following obturation, RMGIC is used for core build-up of the tooth (Fig. 2k). Direct placement of RMGIC on the pulpal floor provides a good coronal seal and is important for a long-term successful outcome of the pulpectomy procedure.
-
A preformed metal crown is cemented on to the tooth, after removal of the rubber dam clamp, to achieve a good coronal seal (Fig. 2l). The crown should be placed in the same appointment or as soon as practically possible. In case of adequate coronal tooth structure, a stable restoration without a preformed crown can be sufficient. However, in case of an extensive, multisurface carious lesion, placement of a Stainless Steel Crown crown is advised for the long-term success of the pulpectomy procedure.
-
A postoperative radiograph is obtained for future reference and to evaluate treatment outcome (Fig. 2m). On follow-ups, the success of the treatment is evident with stable restorations, healthy periapical tissue, physiologic root resorption along with resorption of the obturating material and eruption of the permanent tooth (Fig. 2n–p).
Pitfalls and complications
-
Failure in accurate diagnosis and case selection can lead to failed treatment outcomes.
-
Presence of undercuts following unroofing of the pulp chamber in pulpotomy impairs complete removal of pulp tissue causing persistent pulpal bleeding.
-
Placement of a temporary restoration over MTA requires a second appointment for placement of the final restoration and increases the risk of compromising the coronal seal.
-
Pulpectomy can be a complex procedure in case of torturous root canals and resorbing primary tooth roots, and in young children.
-
Instrument separation in a primary tooth can be an unforeseen complication.
-
The resorption rate of the calcium hydroxide-iodoform paste is faster than that of the tooth root.
-
Over instrumentation during pulpectomy procedure in a primary tooth can damage the underlying permanent tooth.
Further Reading
Kher MS, Rao A (2019) Pulp therapy in primary teeth. In: Contemporary treatment techniques in pediatric dentistry. Springer, Cham
Fuks AB, Kupietzki A, Guelmann M (2013) Pulp therapy for the primary dentition. In: Casamassimo P, Fields H, Mctigue D, Nowak A (eds) Pediatric dentistry: infancy through adolescence. Elsevier, St. Louis, pp 340–344
American Academy of Pediatric Dentistry (2016) Guideline on pulp therapy for primary and young permanent teeth. Pediatr Dent 38(6):280–288
Dhar V, Marghalani AA, Crystal YO et al (2017) Use of vital pulp therapies in primary teeth with deep caries lesions. Pediatr Dent 39(5):E146–E159
Coll JA, Seale NS, Vargas K, Marghalani AA, Al Shamali S, Graham L (2017) Primary tooth vital pulp therapy: a systematic review and meta-analysis. Pediatr Dent 39(1):16–123
Vargas KG, Fuks AB, Peretz B (2016) Pulpotomy techniques: cervical (traditional) and partial. In: Fuks AB, Peretz B (eds) Pediatric endodontics: current concepts in pulp therapy for primary and young permanent teeth. Springer, New York, pp 52–70
Mutluay M, Arikan V, Sari S, Kisa U (2018) Does achievement of hemostasis after pulp exposure provide an accurate assessment of pulp inflammation? Pediatr Dent 40(1):37–42
Smaïl-Faugeron V, Glenny AM, Courson F, Durieux P, Muller-Bolla M, Fron Chabouis H (2018) Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev 5:CD003220. https://doi.org/10.1002/14651858.CD003220
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kher, M.S., Rao, A. Pulp therapy in primary teeth. Clin Dent Rev 4, 16 (2020). https://doi.org/10.1007/s41894-020-00081-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41894-020-00081-z