Abstract
Implementation of mobile health (mHealth) interventions remains limited among those with schizophrenia. This study examined several logistical barriers to the implementation of mHealth interventions, particularly text message interventions, for people with schizophrenia. This study examined the feasibility of leveraging personal mobile phones to deliver mHealth interventions by using data from a pilot randomized controlled trial (RCT) of a text message intervention delivered on personal mobile phones to 56 people with schizophrenia with motivation reductions. Among those screened for the RCT (n = 100), 91% had a mobile phone. For randomized participants (n = 56), 82.1% had a smartphone, with almost all (93.5%) having an Android processing system. Most randomized participants had unlimited text messages (96.4%) or voice calls (76.8%) with their mobile service plan, with 32.1% having unlimited data each month. At baseline, most used text messages (85.2%) and the internet (59.3%), while fewer participants used mobile applications (35.2%) at least once a week. Finally, there were no significant associations between engagement in the text message intervention and participant demographics, symptoms (positive, mood, negative), neurocognition, or mobile phone or plan characteristics, or phone changes made during the 8-week intervention. Even those with schizophrenia with perceived symptom barriers to mHealth engagement (i.e., motivation reductions) may have access to mobile phones and plans and familiarity with mobile features to engage meaningfully with a text message intervention. These results help to support future implementations of text message interventions, which may enhance the provision of care for those with schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mobile health (mHealth) involves using mobile and wireless technologies (e.g., smartphones, activity tracking devices) to improve health services and client outcomes (Kay et al. 2011). In recent years, mHealth has become an increasingly promising approach in mental health care settings, including among those with schizophrenia (Marcolino et al. 2018; Steinhubl et al. 2013). Indeed, mHealth interventions can improve access to evidence-based treatment among those in areas with limited mental health services (Depp et al. 2010) as well as reduce mental health service needs and costs (Ben-Zeev et al. 2019). Further, among those with schizophrenia, mHealth interventions including short message service (SMS) or text message-based interventions appear to be a feasible, acceptable, and clinically promising method to improve a range of outcomes such as symptom improvement and monitoring, medication adherence, and wellness (Ben-Zeev et al. 2014; Granholm et al. 2011; Naslund et al. 2015; Van Der Krieke et al. 2014). Indeed, the early promise of mHealth interventions has led to policy changes, with the Health Information Technology for Economic and Clinical Health (HITECH) Act signed into law in 2009 to support greater use of health information technology in order to improve healthcare.
In spite of these promising research findings and policy changes, real-world implementation of mHealth interventions for schizophrenia remains rare (Lattie et al. 2019). Few studies have taken a solution-focused approach to understanding and addressing the practical barriers to mHealth implementation (Mohr et al. 2018), including understanding the availability of digital technologies and services and addressing clinician attitudes. At the forefront, one key consideration is the availability of personal mobile devices and service plans that are compatible with mHealth interventions for this population. Among people with severe mental illness (SMI), studies have shown that between 66.4 and 81.4% own a mobile phone (Ben-Zeev et al. 2013; Firth et al. 2015), and upwards of 54% have a smartphone (Gay et al. 2016). However, beyond studies on mobile phone ownership, limited work has examined the types of personal mobile service plans people with SMI have and the feasibility of leveraging these plans to deliver mHealth interventions. In many existing mHealth studies, participants are provided with mobile phones to use during the study period. This reduces the ecological validity and generalizability of findings to clinical settings, as providing mobile phones to clients is not scalable or sustainable for most Community Mental Health Centers (CMHC). People with schizophrenia have also expressed interest in using their existing personal mobile phones to support their recovery, indicating interest in receiving services such as check-ins with providers, text message appointment and medication reminders, and symptom tracking and monitoring (Ben-Zeev et al. 2013; Miller et al. 2015). Using participants’ own phones might also more closely reflect real-world implementation and thus support a quicker transition from mHealth efficacy trials to real-world implementation.
An additional mHealth implementation barrier may be clinician attitudes or concerns regarding the type of symptoms that may interfere with engagement in mHealth interventions (Clough et al. 2019; Donovan et al. 2015). Studies have shown that clinicians are more likely to endorse the use of digital health technologies among those with less severe diagnoses rather than SMIs (Sinclair et al. 2013; Vigerland et al. 2014). This may be because among those with schizophrenia, for example, psychotic symptoms may be perceived as a barrier to mHealth engagement, as individuals with elevated persecutory ideation may express reluctance to engage with digital devices given the possible threats to privacy. Furthermore, it is possible that neurocognitive impairments and negative symptoms that are common among schizophrenia may make it challenging to maintain engagement in an mHealth intervention that is delivered multiple times daily. These or similar concerns may explain clinician reluctance to recommend mHealth interventions for their clients with schizophrenia; however, few studies have examined whether such symptoms do interfere with mHealth intervention engagement.
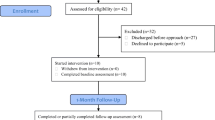
The current study examined the feasibility and potential logistical barriers to using personal mobile phones to deliver mHealth interventions among people with schizophrenia-spectrum disorders. We examined this among those potentially having more symptom barriers to mHealth engagement (i.e., motivation reductions or reduced interest, initiation, and maintenance of occupational, social, and/or recreational activities) by using data from a recent pilot randomized controlled trial (RCT) of a SMS-based intervention that showed greater improvements in motivation, anticipatory pleasure, and recovery-oriented goal attainment compared to a goal-setting condition among those with a schizophrenia-spectrum disorder with at least moderate motivation reductions (Luther et al., in press). Specifically, we detailed the RCT recruitment process and examined whether mobile phone ownership, characteristics, and service plans as well as mobile phone usage patterns could be logistical barriers for the implementation of mHealth interventions that leverage personal mobile phones. We also examined the potential impact of symptoms (positive, mood, negative symptoms), neurocognition, and mobile phone or service plan characteristics in mHealth intervention engagement.
Methods
Participants and Recruitment
Participants were recruited from a large urban CMHC primarily serving outpatients with SMI. All procedures were approved by the university institutional review board. At the beginning of recruitment, a member of the study team met with a supervisor from the CMHC, attended a staff meeting to provide an overview of the study, and posted flyers in the CMHC that remained throughout the 8-month recruitment period. The CMHC supervisor also sent a brief overview of the study to staff via email. Flyers contained a picture of a mobile phone (non-smartphone) and indicated that we were looking for adults with schizophrenia or schizoaffective disorder who had a text message–enabled mobile phone and were willing to participate in an 8-week study. Interested participants were instructed to call a study number posted on the flyers and were then given a brief study overview and a phone screen asking whether they (1) were ≥ 18 years of age, (2) had been diagnosed with a schizophrenia-spectrum disorder, (3) had a mobile phone that could send and receive text messages, and (4) would allow the study team to send text messages to their mobile phone.
Participants who passed the phone screen were invited to complete the baseline interview where we conducted additional eligibility screening and informed consent. Additional eligibility criteria included a confirmed schizophrenia-spectrum diagnosis (using the Structured Clinical Interview for DSM-5; SCID-5; First et al. 2015), ≥ a fourth grade reading level on the Graded Word List (La Pray and Ross 1969), a post-acute illness phase as indexed by no past month inpatient hospitalizations or medication changes, ≥ moderate motivation deficits according to the Clinical Assessment Interview for Negative Symptoms (CAINS; Kring et al. 2013) in at least one domain: family, close friends and romantic relationships, work and school, and/or recreational activities. All eligible participants engaged in a single goal-setting session where they set recovery-oriented goals for an 8-week period. Participants were then randomized (see Luther et al. in press for randomization procedures) to receive either (1) interactive text messages each weekday for 8 weeks to support goal attainment or (2) no additional study intervention (i.e., control condition). All participants completed an 8-week follow-up assessment. Participants completed both baseline and follow-up assessments with raters blinded to randomized condition.
All participants were compensated for completing study assessments, and following a prior study (Ben-Zeev et al. 2014), we reimbursed participants for text message costs ($30/month). To ensure this additional monetary reimbursement was not influencing outcomes, both groups received this compensation. Following prior work (Ben-Zeev et al. 2014; Granholm et al. 2011), the text message group also received text message training with the study interventionist. First, the limits of text message confidentiality and ways to improve privacy (e.g., adding an access password) were reviewed. Next, participants reviewed how to modify relevant settings (e.g., text message notification volume) on their phone and practiced sending and receiving text messages with the study interventionist. This training lasted approximately 15 min.
Text Messages
Participants randomized to the text messages received three sets of text messages each weekday over the 8-week intervention period. The content of the text messages was based on a pre-set script that was individualized for each participant (see Luther et al. in press for additional text message details) and focused on improving goal completion and motivation. Each set of text messages contained one or two questions (e.g., Able to complete [your goal] today?).
Measures
At baseline, in addition to the below measures, participants completed demographic information and answered questions about their mobile phone, payment plan, use preferences, and most common uses. They also completed a measure to assess the frequency with which participants completed a range of activities on their mobile phones over the last month. Twenty activities (e.g., making and receiving a call, checking email) were rated on a 9-point scale ((0) = never, (1) = about once a month, (2) = 2–3 times a month, (3) = once a week, (4) = twice a week, (5) = 3–4 days a week, (6) = 5–6 days a week, (7) = everyday, (8) = multiple times a day).
At the 8-week follow-up, participants were also asked whether they had made any changes to their phone or phone service plan since the baseline interview.
Neurocognitive performance was assessed using the brief neurocognitive assessment (BNA; Fervaha et al. 2014). Based on a study identifying working memory and processing speed as explaining the largest amount of variance in global neurocognition (Fervaha et al. 2014), the updated BNA (Fervaha et al. 2015) assesses working memory with the letter-number sequencing test (Gold et al. 1997) and processing speed with the symbol coding subtest from the Brief Assessment of Cognition in Schizophrenia (BACS; Keefe et al. 2004). A composite standardized z-score was created from guidelines by Fervaha et al. (2015); this score has demonstrated reliability and validity in schizophrenia samples (Fervaha et al. 2015).
Mood and positive symptoms were assessed by the factor analytically derived subscales (Bell et al. 1994) of the interviewer-rated Positive and Negative Syndrome Scale (PANSS; Kay et al. 1987). Mood (depression, anxiety, guilt feelings, and active social avoidance) and positive (delusions, hallucinations, unusual thought content, somatic concern, suspiciousness/persecution, and grandiosity) symptom items are rated on a 7-point scale from 1 (absent) to 7 (severe). PANSS scores have demonstrated satisfactory inter-rater reliability and construct validity in schizophrenia-spectrum samples (Jang et al. 2016; Kay et al. 1987).
Negative symptoms were assessed with the interviewer-rated Clinical Assessment Interview for Negative Symptoms (CAINS; Kring et al. 2013), which assesses expressive symptoms and motivation, anticipatory pleasure, and past week pleasure for such domains as familial relationships and school/work activities. All 13-items are rated on a 0 (no impairment) to 4 (severe deficit) scale. The CAINS has demonstrated good convergent validity and inter-rater reliability in schizophrenia-spectrum samples (Kring et al. 2013).
Analyses
To explore the feasibility of using personal phones to deliver mHealth interventions, descriptive statistics were used to examine potential participants’ reasons for eligibility or ineligibility. Next, given the importance of mobile phone operating systems and reliable data connection for some mHealth interventions, we used descriptive statistics to examine the enrolled participants’ phone characteristics (i.e., phone type and model) and phone payment plan (i.e., cost, services included) and how these changed over the 8-week study period. To characterize participants’ skill and familiarity using mobile phone features that could be leveraged in mHealth, we examined mobile phone use preferences and the frequency of using different mobile phone components (i.e., calendar, mobile applications, etc.). For mobile feature preferences and frequency of use, we focused on baseline data (i.e., pre-intervention) since these features were influenced by randomized condition. For those in the text message condition, we also examined factors that might influence engagement by examining whether their text message response rate ((number of questions sent via text message participants responded to divided by total number of text message questions sent) × 100) during the intervention was correlated with demographics, symptoms (positive, mood, negative symptoms), neurocognition, and mobile phone, or plan characteristics.
Results
Recruitment Feasibility
During the 8-month recruitment period, 100 participants called the study number and completed the phone screen. Nine of these participants did not have a mobile phone. An additional seven were excluded for not having a schizophrenia-spectrum diagnosis (n = 5) or motivation deficits (n = 2). Nine participants lost interest in the study after hearing the study description, while an additional 19 were excluded after expressing interest but then did not attend their in-person interview (n = 12) or did not return phone calls about scheduling their in-person interview (n = 7). Therefore, 56 participants were ultimately randomized, with 27 randomized to the text message condition and 29 randomized to the control condition. Randomized participants had a schizophrenia (n = 23, 41.1%) or schizoaffective disorder (n = 33, 58.9%) diagnosis, a mean age of 46.14 years (SD = 8.76), an average of 11.84 years (SD = 2.37) of education, a mean monthly income of $657.16 (SD = 374.71), and a mean illness duration of 23.66 years (SD = 11.20). Most received Supplemental Security Income (SSI)/Social Security Disability Income (SSDI) (n = 41, 73.2%) and were African-American (n = 39, 69.6%) or Caucasian (n = 14, 25%), male (n = 29, 51.8%), and not currently employed (n = 46, 82.1%). Additional participant characteristics are in Table 1.
Phone Characteristics
As seen in Table 1, 82.1% (n = 46) of those randomized had a smartphone at baseline, with almost all of these operating on an Android processing system (n = 43, 93.5%). Among all participants, the most popular phone brand was LG (n = 22, 39.3%), followed by Samsung (n = 12, 21.4%) and Alcatel (n = 6, 10.7%).
At follow-up (completed by 53 (94.6%) participants), 39 participants (73.6%); (n = 20 (37.7%) text message condition, n = 19 (35.8%) control) had the same physical phone that they had at baseline. Of the remaining participants, 11 (n = 4 text message, n = 7 controls) reported getting a new phone (n = 5 purchased the same phone brand and version after loss or damage to old phone, n = 4 purchased a new phone brand, and n = 2 purchased the same brand, but different phone model). The remaining three participants (n = 1 text message, n = 2 controls), lost (n = 2) or discarded their phone (n = 1) and had not obtained a new phone yet (one was getting a new phone the following day).
Phone Payment and Service Information
All participants had some amount of talking and texting on their mobile service plan. Specifically, 96.4% (n = 54) had unlimited texting, 76.8% (n = 43) had unlimited talking, and 32.1% (n = 18) had unlimited data services each month. For the two participants without unlimited text messages, they had 100 or 500 monthly text messages; for the 13 participants without unlimited talking, they had 100 to 500 min a month. In terms of data (i.e., data transmission needed for internet connectivity), in the full sample (n = 56), the majority (69.6%, n = 39) of participants had some sort of data with their plan. Among those with a smartphone (n = 46), 84.8% (n = 39) had data plans; of these, 46.1% (n = 18) had unlimited data, and the remainder (53.8%, n = 21) had between 1 gigabyte (GB) and 12 GB of data per month.
In terms of participants’ service payment plan, 33 (58.9%) were on month-to month plans, while six (10.7%) were on service contracts. The remaining had Lifeline government subsidized plans which require yearly recertification (n = 13, 23.2%) or used prepaid phone cards (n = 4, 7.1%). For all participants, the average monthly plan cost was $34.18 (SD = 24.75) (ranging from $0 (Lifeline participants with basic services) to $116.00), and participants spent an average of 17.0% (SD = 32.5) of their monthly income on their mobile phone plan. Participants with data plans (n = 39, 69.6%) paid an average of $42.97 per month. In terms of the top 5 service providers, 40% had Metro PCS, 12.7% had Safelink, 9.1% had AT&T, 7.3% had Boost Mobile, and 7.3% had Verizon. At follow-up, 10 (of 53, 18.9%; 5 in each group) participants reported changing their service plan, with 5 participants changing their providers, 4 staying with the same provider but increasing/decreasing services, and one participant canceling their services.
Preferences and Frequency of Use
At baseline, most participants preferred calling (39.3%; n = 22) over texting (25%, n = 14), and the remaining 35.7% (n = 20) did not prefer one communication method over the other. The majority of participants (91.1%, n = 51) reported using their mobile phone multiple times a day, while all reported using their phone each week. The most common features used were text-messaging, calling, and checking the time. Thirty-two (59.3%) and 31 (57.4%) participants reported sending or receiving text messages each day, respectively (See Table 2 for frequency of use results). The majority of participants also made (33, 61.1%) or received (32, 59.3%) a call each day. At least once a week, most participants reported using their phone to also check the time (98.1%, n = 53), listen to music (75.9%, n = 41), check the weather (75.9%, n = 41), check the calendar (74.1%, n = 40), watch videos or TV (63.0%, n = 34), search the internet (59.3%, n = 32), or set an alarm (57.4%, n = 31). Fewer participants reported using their phone at least once a week for additional activities such as using email (48.1%, n = 26), social media (44.4%, n = 24), or mobile applications (apps; 35.2%, n = 19).
Intervention Engagement
The average text message response rate over the 8 weeks was 86.1% (SD = 16.7%) (see Luther et al. in press for more details). As seen in Table 3, engagement (i.e., text message response rate) was not significantly associated with participant demographics or baseline symptoms or neurocognition, including negative symptoms as well as positive symptoms (positive subscale score and individual items (e.g., suspiciousness/persecution): r’s < .19, p’s > .36). Furthermore, engagement was not associated with baseline mobile phone or service plan characteristics or changes in mobile phones or service plans during the study. However, there were two moderate-sized correlations that were trending towards significance; being female was associated with lower engagement (r = − .35; p = .089), and greater baseline anticipatory pleasure reductions were associated with greater engagement (r = .36; p = .075).
Discussion
mHealth interventions are a promising approach to improve mental health access and care for those with SMI. To support greater use of health information technology, the HITECH Act was signed into law in 2009. However, since the law’s passage, large-scale adoption and uptake of mobile interventions in community-based care have been limited (Lattie et al. 2019).
To identify potential logistical barriers to mHealth implementation, including whether personal phones can be leveraged to deliver mHealth interventions, this study examined (1) mobile phone ownership, characteristics, and service plans; (2) mobile phone usage patterns; and (3) the potential interference of demographics, symptoms, and mobile phone and plan characteristics in mHealth engagement. Overall, our findings suggest that a number of those with schizophrenia with perceived potential symptom barriers (i.e., moderate motivation reductions) have access to the mobile devices and plans needed for an mHealth intervention delivered by SMS as well as the familiarity with mobile device features that support meaningful SMS intervention engagement. Furthermore, engagement in an SMS intervention did not appear to be negatively impacted by symptoms (positive, negative, or mood symptoms) or neurocognition.
Consistent with prior work showing that 72 to 81% of people with schizophrenia own a mobile phone (Ben-Zeev et al. 2013; Firth et al. 2015), only 9 out of 100 potential participants who were screened did not have a text message–enabled mobile phone. Of those randomized to our study and thus had at least moderate motivation reductions, 82.1% had a smartphone. This rate is in line with the general US adult population smartphone ownership rate (81%; Pew Research Center b) and is much higher than a prior meta-analysis finding that 35.4% of those with psychosis own a smartphone (Firth et al. 2015) but more in line with later work showing that 54% of those with psychosis own a smartphone (Gay et al. 2016). Our findings suggest that greater negative symptomatology or having an average monthly income below $1000 in those with schizophrenia may not impact phone ownership. The increase in smartphone ownership in schizophrenia aligns with the general population (Taylor and Silver 2019) and may be due to lower entry prices for smartphones (particularly android devices), federal assistance programs for people with lower incomes such as the Federal Lifeline Program in the US that subsidize the cost of mobile phones, including smartphones, and the central role that smartphones play in internet access among those with lower incomes (Pew Research Center 2019a). This smartphone ownership increase also supports the potential viability of using personal mobile phones to deliver smartphone-based mHealth apps (Ben-Zeev et al. 2018; Schlosser et al. 2018) among those with schizophrenia. One important finding was that the majority of participants (93.5%) with smartphones had an Android processing system, an important consideration when developing or studying apps that are compatible only with specific operating systems.
Extending prior work examining phone characteristics in people with schizophrenia, we examined enrolled participants’ service plans, including costs and features to see if these were compatible with the needs of mHealth interventions. Our results show that the average service plan costs $34.18 and service plans with data services cost $42.97. With their service plan, almost all participants had unlimited texting (96.4%) and talking (76.8%) as part of their phone service plans, supporting the viability of using personal phones and mobile services for SMS-based or mobile call–based mHealth interventions or treatment-related reminders. Importantly, the majority (69.6%) of participants had a mobile data plan, and almost a third had unlimited data each month. Notably, the majority of participants also reported regularly using many of these features, with most using SMS (85.2%) and the internet (59.3%), and fewer using mobile applications (35.2%) at least once a week at baseline. While preliminary, these results suggest that many with schizophrenia already have the experience and familiarity with a range of mobile phone features that are commonly used to deliver mHealth interventions. Furthermore, these results, in conjunction with some prior work (Schlosser et al. 2018), suggest it may be feasible among a smaller proportion of people with schizophrenia to use their existing data service plans to deliver app-based mHealth interventions, especially for less data-intensive or native mobile apps or for remote symptom monitoring or sensing. However, given that the success of many mHealth apps requires reliable and continuous connections to mobile data or the internet, more work is needed to identify methods of expanding mobile data access to those with SMI.
Lastly, our study examined whether participant demographics, clinical, or neurocognitive profiles as well as mobile phone or service plan characteristics or changes may interfere with mHealth intervention engagement. Our results suggest that neither demographics nor neurocognition and negative symptoms nor positive symptoms (including delusions and suspiciousness/persecution) were significantly associated with reduced SMS intervention engagement. However, at a trend level, greater baseline reductions in anticipatory pleasure were associated with more engagement, possibly suggesting that those expecting less future enjoyment in their activities might engage and benefit more from mHealth interventions, specifically ones that support engagement in rewarding activities. Together, these findings may potentially alleviate some clinician concerns about more severe symptoms or diagnoses interfering with engagement in mHealth interventions (Sinclair et al. 2013; Vigerland et al. 2014). However, following others (Ben-Zeev et al. 2014; Granholm et al. 2011), we made modifications to reduce engagement barriers, including using text message procedure training and text messages that required a low reading level. Although limited work has examined whether symptoms interfere with mHealth engagement in those SMI, our findings contrast Granholm et al. (2011) who found that the subset of participants that did not engage in a text message intervention (i.e., stopped responding/sending text messages within 2 weeks) had higher negative symptoms and lower functioning and premorbid IQ than those who had greater intervention engagement. These differences in findings may be because Granholm et al. (2011) provided study participants with “older” mobile phones. Learning how to operate these phones may have been a greater barrier to engagement for people with lower functioning and higher negative symptoms. Relatedly, we did not find any significant associations between intervention engagement and mobile phone or plan characteristics, including prior text message experience, monthly service costs, type of text message plan (i.e., unlimited), or type of mobile phone (i.e., smartphone). In addition, although we observed that 18.1% of participants changed their mobile service plan and 30.1% changed their physical phone between baseline and the 8-week follow-up, these changes did not appear to interfere with intervention engagement. Indeed, we did not find a significant association between service plan or mobile phone changes and the intervention response rate. Taken together, symptoms and neurocognition as well as changes to service plans and mobile phones may have limited impact on the use of SMS-delivered interventions, and SMS-based interventions could be successfully used and implemented with people with a range of different phones and service message plans.
Several limitations should be considered when interpreting these results. First, study participants were recruited from one geographical region and CMHC. Second, although the rates of phone ownership we observed were similar to prior SMI studies (c.f., Firth et al. 2015), it is possible that our recruitment strategies for the parent RCT influenced the mobile phone ownership rate we observed in the current study; larger-scale studies are needed to confirm these results. Second, all participants received reimbursement for text-messaging costs over the 8-week study (i.e., to ensure the payment was not differentially influencing outcomes), which may have influenced whether participants changed their mobile service plan during the study. An additional limitation is our sample size, as we may have been underpowered to detect some effects. Indeed, although we were interested in the mobile phone characteristics and service plans of our participants in the RCT, our primary study was not designed to be a population-based survey; thus, these results may not be representative of all people with schizophrenia. For example, participants may have self-selected to enroll in the study because they had higher technology literacy and access. Furthermore, although our results suggest that using participants’ mobile technology is feasible even among those with at least moderate motivation reductions, those with different symptom profiles or more prominent negative symptoms could possibly have greater difficulty engaging in mHealth interventions or have different mobile phone ownership rates or services. Given that mobile technology is constantly evolving and changing, more work is also needed to identify the critical clinician training needed to support the successful implementation of mHealth interventions. Finally, given increased interest in mobile app interventions, future work is needed to examine the feasibility of using personal phones for these and other types of eHealth interventions (e.g., online intervention).
In conclusion, our results suggest that it is increasingly feasible to leverage personal mobile phones and service plans to deliver mHealth interventions among those with schizophrenia, including among those with more significant motivation reductions. Specifically, our results suggest that many people with schizophrenia own a mobile phone and importantly have mobile service plans that are compatible with mHealth interventions, particularly SMS or mobile phone call–based interventions. Furthermore, many with schizophrenia already have the familiarity and experience with mobile devices and features that are used to deliver mHealth interventions, including SMS, the internet, and for some, mobile apps. However, our results also suggest that using personal mobile phones to deliver interventions or assessments relying on continuous and reliable data services may currently only be feasible among a smaller portion of those with schizophrenia. Additionally, neither neurocognition nor positive, negative, or mood symptoms were significantly associated with engagement in the text message intervention. These results suggest that mobile phone ownership and services, prior experience with text messages, and some symptoms may not be barriers to engagement and implementation of text message interventions for those with schizophrenia in community-based settings. Together, these results support the feasibility of using personal mobile devices and plans to deliver mHealth services in community-based settings, which may enhance and expand the provision of care for those with schizophrenia and others with a SMI.
References
Bell, M. D., Lysaker, P. H., Beam-Goulet, J. L., Milstein, R. M., & Lindenmayer, J.-P. (1994). Five-component model of schizophrenia: Assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Research, 52(3), 295–303.
Ben-Zeev, D., Davis, K. E., Kaiser, S., Krzsos, I., & Drake, R. E. (2013). Mobile technologies among people with serious mental illness: Opportunities for future services. Administration and Policy in Mental Health and Mental Health Services Research, 40(4), 340–343.
Ben-Zeev, D., Kaiser, S. M., & Krzos, I. (2014). Remote “hovering” with individuals with psychotic disorders and substance use: Feasibility, engagement, and therapeutic alliance with a text-messaging mobile interventionist. Journal of Dual Diagnosis, 10(4), 197–203.
Ben-Zeev, D., Brian, R. M., Jonathan, G., Razzano, L., Pashka, N., Carpenter-Song, E., Drake, R. E., & Scherer, E. A. (2018). Mobile health (mHealth) versus clinic-based group intervention for people with serious mental illness: A randomized controlled trial. Psychiatric Services, 69(9), 978–985.
Ben-Zeev, D., Buck, B., Hallgren, K., & Drake, R. E. (2019). Effect of mobile health on in-person service use among people with serious mental illness. Psychiatric Services, 70(6), 507–510.
Clough, B. A., Rowland, D. P., & Casey, L. M. (2019). Development of the eTAP-T: A measure of mental health professionals’ attitudes and process towards e-interventions. Internet Interventions, 18, 100288.
Depp, C. A., Mausbach, B., Granholm, E., Cardenas, V., Ben-Zeev, D., Patterson, T. L., Lebowitz, B. D., & Jeste, D. V. (2010). Mobile interventions for severe mental illness: Design and preliminary data from three approaches. The Journal of Nervous and Mental Disease, 198(10), 715–721.
Donovan, C. L., Poole, C., Boyes, N., Redgate, J., & March, S. (2015). Australian mental health worker attitudes towards cCBT: What is the role of knowledge? Are there differences? Can we change them? Internet Interventions, 2(4), 372–381.
Fervaha, G., Agid, O., Foussias, G., & Remington, G. (2014). Toward a more parsimonious assessment of neurocognition in schizophrenia: A 10-minute assessment tool. Journal of Psychiatric Research, 52, 50–56.
Fervaha, G., Hill, C., Agid, O., Takeuchi, H., Foussias, G., Siddiqui, I., Kern, R. S., & Remington, G. (2015). Examination of the validity of the brief neurocognitive assessment (BNA) for schizophrenia. Schizophrenia Research, 166(1–3), 304–309.
First, M. B., Williams, J., Karg, R. S., & Spitzer, R. L. (2015). User’s guide to structured clinical interview for DSM-5 disorders (SCID-5-CV) clinical version: Arlington. VA: American Psychiatric Publishing.
Firth, J., Cotter, J., Torous, J., Bucci, S., Firth, J. A., & Yung, A. R. (2015). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: A meta-analysis of cross-sectional studies. Schizophrenia Bulletin, 42(2), 448–455.
Gay, K., Torous, J., Joseph, A., Pandya, A., & Duckworth, K. (2016). Digital technology use among individuals with schizophrenia: Results of an online survey. JMIR Mental Health, 3(2), e15.
Granholm, E., Ben-Zeev, D., Link, P. C., Bradshaw, K. R., & Holden, J. L. (2011). Mobile Assessment and Treatment for Schizophrenia (MATS): A pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophrenia Bulletin, 38(3), 414–425.
Gold, J. M., Carpenter, C., Randolph, C., Goldberg, T. E., & Weinberger, D. R. (1997). Auditory Working Memory and Wisconsin Card Sorting Test Performance in Schizophrenia. Archives of General Psychiatry, 54(2), 159–165.
Jang, S.-K., Choi, H.-I., Park, S., Jaekal, E., Lee, G.-Y., Cho, Y. I., & Choi, K.-H. (2016). A two-factor model better explains heterogeneity in negative symptoms: Evidence from the Positive and Negative Syndrome Scale. Frontiers in Psychology, 7, 707.
Kay, S. R., Fiszbein, A., & Opfer, L. A. (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261–276. https://doi.org/10.1093/schbul/13.2.261.
Kay, M., Santos, J., & Takane, M. (2011). mHealth: New horizons for health through mobile technologies. World Health Organization, 64(7), 66–71.
Keefe, R. S. E., Goldberg, T. E., Harvey, P. D., Gold, J. M., Poe, M. P., Coughenour, L. (2004). The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophrenia Research, 68, 283–297.
Kring, A. M., Gur, R. E., Blanchard, J. J., Horan, W. P., & Reise, S. P. (2013). The clinical assessment interview for negative symptoms (CAINS): Final development and validation. American Journal of Psychiatry, 170(2), 165–172.
La Pray, M., & Ross, R. (1969). The graded word list: Quick gauge of reading ability. Journal of Reading, 12(4), 305–307.
Lattie, E. G., Nicholas, J., Knapp, A. A., Skerl, J. J., Kaiser, S. M., & Mohr, D. C. (2019). Opportunities for and tensions surrounding the use of technology-enabled mental health services in community mental health care. Administration and Policy in Mental Health and Mental Health Services Research, 1–12.
Luther, L., Fischer, M. W., Johnson-Kwochka, A. V., Minor, K. S., Holden, R., Lapish, C. L., McCormick, B., & Salyers, M. P. (in press). Mobile enhancement of motivation in schizophrenia: A pilot randomized controlled trial of a personalized text message intervention for motivation deficits. Journal of Consulting and Clinical Psychology.
Marcolino, M. S., Oliveira, J. A. Q., D’Agostino, M., Ribeiro, A. L., Alkmim, M. B. M., & Novillo-Ortiz, D. (2018). The impact of mHealth interventions: Systematic review of systematic reviews. JMIR mHealth and uHealth, 6(1), e23.
Miller, B. J., Stewart, A., Schrimsher, J., Peeples, D., & Buckley, P. F. (2015). How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Research, 225(3), 458–463.
Mohr, D. C., Riper, H., & Schueller, S. M. (2018). A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry, 75(2), 113–114.
Naslund, J. A., Marsch, L. A., McHugo, G. J., & Bartels, S. J. (2015). Emerging mHealth and eHealth interventions for serious mental illness: A review of the literature. Journal of Mental Health, 24(5), 321–332.
Pew Research Center (2019a). Internet/broadband fact sheet. Retrieved from https://www.pewresearch.org/internet/fact-sheet/internet-broadband/
Pew Research Center (2019b). Mobile fact sheet. Retrieved from https://www.pewresearch.org/internet/fact-sheet/mobile/
Schlosser, D. A., Campellone, T. R., Truong, B., Etter, K., Vergani, S., Komaiko, K., & Vinogradov, S. (2018). Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophrenia Bulletin, 44(5), 1010–1020.
Sinclair, C., Holloway, K., Riley, G., & Auret, K. (2013). Online mental health resources in rural Australia: Clinician perceptions of acceptability. Journal of Medical Internet Research, 15(9), e193.
Steinhubl, S. R., Muse, E. D., & Topol, E. J. (2013). Can mobile health technologies transform health care? JAMA, 310(22), 2395–2396.
Taylor, K., & Silver, L. (2019). Smartphone ownership is growing rapidly around the world, but not always equally. Retrieved from https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/
Van Der Krieke, L., Wunderink, L., Emerencia, A. C., De Jonge, P., & Sytema, S. (2014). E–mental health self-management for psychotic disorders: State of the art and future perspectives. Psychiatric Services, 65(1), 33–49.
Vigerland, S., Ljótsson, B., Gustafsson, F. B., Hagert, S., Thulin, U., Andersson, G., & Serlachius, E. (2014). Attitudes towards the use of computerized cognitive behavior therapy (cCBT) with children and adolescents: A survey among Swedish mental health professionals. Internet Interventions, 1(3), 111–117.
Funding
This work was supported by the William and Dorothy Bevan Scholarship from the American Psychological Foundation, the Indiana Clinical and Translational Sciences Institute (ICTSI), the ICTSI Clinical Research Center (UL1TR001108), the Indiana University-Purdue University Indianapolis Undergraduate Research Opportunities Program, and the National Institutes of Mental Health (T32MH016259). In addition, Dr. Buck is supported by a NARSAD Young Investigator Award from the Brain and Behavior Foundation and a Mentored Patient-Oriented Research Career Development Award from the National Institutes of Mental Health (K23MH122504).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Considerations
The study procedures were approved by the Indiana University-Purdue University Indianapolis Institutional Review Board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luther, L., Buck, B.E., Fischer, M.A. et al. Examining Potential Barriers to mHealth Implementation and Engagement in Schizophrenia: Phone Ownership and Symptom Severity. J. technol. behav. sci. 7, 13–22 (2022). https://doi.org/10.1007/s41347-020-00162-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41347-020-00162-7