Abstract
In this paper, we investigated the relationship between different levels of sleep and the risk of suicide among depressive patients. The sample consisted of 301 adults with depression who were recruited from a hospital in Ningxia, China. The Pittsburgh Sleep Quality Index (PSQI) and the Self-Rating Depression Scale (SDS) were applied to evaluate the quality of sleep and the degree of depression. The Suicidal Risk Factor Assessment Form evaluated suicide risk. A Latent Class Analysis (LCA) has been performed with MPLUS 7.0 to investigate the most probable category of the PSQI sub-scales. Multivariate Logistic Regression was applied to analyse the relation between Sleep Quality and Suicide Hazard in Adult Depressive Patients. Classes identified were “Global sleep impairment”, “Poor sleep quality”, “Short sleep duration” and “Good sleep quality.” Patients with poor overall sleep quality and clear daytime dysfunction had a higher risk of suicide than those with good sleep quality. The results are helpful in understanding the relationship between the variability of sleep patterns and the risk of suicide among depressed people, and it is suggested that some sleep variables may have a higher predictive value than others. The results will provide guidance on how to improve and implement therapy for depressive disorders in adults, and to lower suicidal rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicide is a widespread public health issue, which causes over 700,000 deaths annually, and for every death due to suicide, there can be 20 times as many suicide attempts [1]. In China, suicide is responsible for over 74,000 deaths every year, and there is expected to be 102,500 suicides by 2050 [2]. There is strong evidence that people with depression are at significantly increased risk of suicide [3, 4]. Furthermore, the U.S. Preventive Task Force recommended that a suicide risk evaluation be carried out in conjunction with depression screening [5]. In fact, up to 60% of depressed people will commit suicide and up to 20% will attempt suicide in their lifetime. About 3.4% of depression sufferers die by suicide [6]. Further, such rates have been found to increase with the level of depression [7]. In view of the relatively high risk of suicide in depressed people, Institute of Medicine (IOM) has identified suicide prevention as a matter of urgency and calls for action to identify evidence-based risk factors for suicide prevention [8]. Thus, the determination of the major risk factors for the development of depressed persons is critical to the identification of the highest-risk groups and appropriate intervention, since there is strong evidence that surveillance and proactive management of high-risk patients can lead to a reduction in suicide [9].
One associated feature of depression that may increase suicide risk is sleep disturbances [10]. More than 90% of patients with depression disorder experience sleep problems [11]. It has been reported that, compared to individuals without depression, those with depression have impaired sleep efficiency, sleep maintenance difficulties, reductions in slow wave sleep (SWS), disinhibition of rapid eye movement (REM) sleep, and circadian rhythm alterations [12]. Studies have suggested that sleep disturbances may be a separate risk factor for suicidal behavior in depressive patients [13]. A large number of research suggests that fewer hours of sleep, bad dreams, the use of sleeping drugs, and feeling too cold while sleeping are independent factors for depressed people to commit suicide [14,15,16,17].
Some research has been done on sleep in hospitalized patients with depression, often using a variable-centered approach to evaluate sleep quality. One study, for instance, found that depression was associated with higher rates of sleep deprivation, bad sleep and sleeplessness. [18]. However, this method ignores the objective nature of sleep problem heterogeneity. Large sample epidemiology research has shown that there can be a number of possible combinations of sleep problems [19]. Alternatively, person-centred studies can provide insight into relevant sleep subtypes. Latent Classification Analysis (LCA) is useful in identifying hidden subsets of individuals with clear patterns of abuse subtypes that are not readily observable [20]. Furthermore, no published trial has investigated the relationship between the diversity of sleep disorders in depressive patients and suicidal risk by means of a person-centred questionnaire. It is important not to underestimate the importance of identifying the heterogeneous nature of sleep problems among depressed people, since the definition of more specific sub-types may facilitate the development of more efficient and more focused strategies for preventing suicide among high-risk individuals, instead of using a generic method.
Therefore, based on a series of detailed variables such as type, frequency, and duration of sleep-related indicators or symptoms, the LCA method was used in this study to classify the best latent sleep categories of patients with depression and to analyze the relationship between sleep structure and suicidal risk in patients with depression. The results may help inform the design of specific suicide prevention intervention strategies for patients with depression who exhibit a homogeneous sleep structure, to maximize the intervention effect, and to provide a more reasonable basis for improving sleep disturbances among patients with depression, thereby decreasing the risk of suicide.
Participants and methods
The participants of the current study were aged 18–60 years and were recruited from a general hospital in Ningxia. Hospital institutional review board approval was obtained, and all participants gave oral informed consent before completing study assessments. Trained researchers administered the test measures and a demographic questionnaire to the participants. The analytic sample in this study consisted of 301 adults with a diagnosis of depression, which excluded individuals who had missing key information on sleep status or risk of suicide. Finally, the data of all participants entered the LCA analyses.
Measurements
Pittsburgh sleep quality index (PSQI)
We used the Pittsburgh Sleep Quality Index (PSQI) to measure the sleep status of the participants in the past month. This index consists of 19 items that encompass seven domains of sleep quality: subjective sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The global score was obtained by summing the component scores, and higher PSQI scores indicated poorer sleep quality. For the studied dimensions, scores ≥ 2 indicated the existence of a problem [21] (Cronbach’s alpha = 0.676).
Self-rating depression scale (SDS)
The Self-Rating Depression Scale (SDS) comprises 20 items that evaluate symptoms of depression [21]. The instrument has been validated in a Chinese population [22]. Participants were asked about the frequency of a certain symptom according to how they felt during the preceding seven days. Responses to each item were ranked from one (none or little of the time) to four (most or all of the time), with higher scores corresponding to more frequent symptoms. The sum of the scores of all items was the raw score, and the final index score was converted by multiplying the raw score by 1.25 and then rounding the decimal places (Cronbach’s alpha = 0.844).
Suicidal risk factor assessment form
The Suicidal Risk Factor Assessment Form items assessed three suicide risk domains: Class I risk factors (including suicidal ideation, suicide attempts, self-evaluation, suicidal behavior, hopelessness, helplessness, and alcohol/drug abuse), Class II risk factors (including age, sex, marital status, occupational status, and health status), and Class III risk factors (including interpersonal relationships, family support, interpersonal relationships, self-knowledge, personality traits, career achievements, and stress events). The form yielded a maximum possible score of 43. A total score of 11 or higher was indicative of suicide risk (Cronbach’s alpha = 0.840). However, it is impossible to clearly distinguish between patients with recovering major depression and patients with major depressive episodes.
Socio-demographic characteristics
Participants’ demographic characteristics included age, sex, marital status, educational level, and residence status. Measures of sociodemographic characteristics are provided in the Supplementary Materials.
Statistical analysis
Statistical analyses were performed using SPSS version 25.0 and Mplus 7.0. Firstly, we investigated the best latent classes of potential sleep quality categories by fitting models to a range of potential categories. Potential categories for inclusion included sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. These are all continuous variables. The optimal number of classes was determined based on model fit statistics (Akaike Information Criterion [AIC], Bayesian Information Criterion [BIC], adjusted Bayesian Information Criterion [aBIC], Lo-Mendell-Rubin value [LMR], and entropy), and interpretability of the latent classes. Second, differences in sleep quality in relation to partial demographic characteristics and SDS scores were compared using one-way ANOVA and chi-square tests. Post hoc tests were conducted using Bonferroni correction for multiple comparisons. Finally, associations between latent classes and the risk of suicide were examined using logistic regression analysis.
Results
Participants’ characteristics
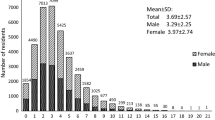
The mean age of the 301 participants (93 males, 208 females) was 32.93 years (SD = 10.148); 217 participants with a suicide risk score of 11 or greater; most were married (N = 177, 58.8%) and more than a third were single (N = 104, 34.6%), while the rest were divorced/widowed (N = 15), and five participants did not disclose their current marital status. Most participants (N = 175) had a university degree or above, while 46 participants did not disclose their education level. Most participants (N = 282, 93.7%) resided in urban areas, with the remainder living in rural areas (N = 15, 5.0%); four participants did not disclose their residence type. Further details are provided in Table 1.
Latent class models of sleep quality
The results of the model fit are shown in Table 2. Four categories were chosen to be the best-fit model on the basis of model fit statistics (lowest AIC and aBIC values), acceptable entropy, and highly interpretable classification. Figure 1 illustrates the likelihood of a latent-class item. Class 1 (global sleep impairment class; 51.8%) included adults who reported poor subjective sleep quality, longer sleep latency, short sleep duration, suboptimal sleep efficiency, palpable sleep disturbances, and more frequent use of sleep medicines. While sleep quality and sleep latency scores were lower than Class 1, daytime dysfunction problems were slightly more severe than it, thus Class 2 (poor sleep quality class; 28.6%) consisted of participants with the highest probability of daytime dysfunction. Class 3 (short sleep duration class: 7.6%) included adults who had a significantly shorter sleep time. Class 4 (good sleep quality class; 12.0%) consisted of adults who had the lowest probability of most sleep problems. They also had the highest sleep mass.
Between-group analyses
Descriptive and between-group statistics are shown in Table 3. One-way ANOVA and Chi-squared tests indicated that there were significant differences in the distribution of age, SDS scores, and PSQI scores (including seven major sleep problems) across the identified classes. Pairwise comparisons were subsequently subjected to Bonferroni correction. These tests showed that only Class 2 (poor sleep quality class) differed from the other three groups. Class 1 and 2 had the highest percentages of depression status and poor sleep affecting daily life (P < 0.05), Class 1 (global sleep impairment class) had the highest percentages of sleep quality, sleep latency habitual sleep efficiency, and PSQI total scores (P < 0.001), while Class 3 (short sleep duration class) had the lowest rates of poor sleep duration (P < 0.001). Classes 1 and 2 also performed worse than Classes 3 and 4 for sleep disturbances (P < 0.001). Finally, for the use of sleep medication, Class 1 differed from Class 2, 3, and 4, whereas use was not significantly different among the final three classes (P < 0.001). Hence, age and SDS scores were included as covariates in the subsequent analyses.
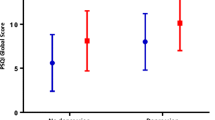
Logistic regression analyses
Table 4 shows that Class 1 and Class 2 had higher odds of risk of suicide than Class 4 (Good sleep quality class; Class 1 OR = 2.369, 95% CI = 1.135, 4.945; Class 2 OR = 2.727, 95% CI = 1.222, 6.087), while the odds for Class 3 approximated those of Class 4. In addition, after adjusting for covariates (age, gender, and depression level), compared to Class 4, the risk of suicide was 2.642 times higher for Class 1 and 2.427 times higher for Class 2 (Class 1 OR = 2.642, 95% CI = 1.211, 5.766; Class 2 OR = 2.427, 95% CI = 1.052, 5.599).
Discussion
The main focus of our study was to explore latent sleep patterns using LCA, which are defined as latent homogeneous subsets in a population of depressed patients based on their individual responses to the 7 PSQI components. More importantly, we examined the relationship between the underlying relationship of sleep disturbances and the risk of suicide among depressed people. Our evidence showed that patients with Class-1 (Global sleep impairment class) and Class-2 (Poor sleep quality class) sleep disorders had a higher risk of suicide than those without sleep disorders, even when adjusting for sex, age, and depression severity.
Several studies have provided convincing evidence that sleep is heterogeneous in the population [23, 24]. Our results indicate that there is heterogeneity in sleep problems among patients with depression. Similar to previous studies, a high percentage of the sample (Class-1, Global sleep impairment class; 51.8%) reported poorer sleep quality. The proportion of participants reporting poor sleep quality in the study was higher than that reported by Zhou et al. [25]; this may be due to the heterogeneity of the sample since our study focused on adults with depression and their research participants were college students. People with mental disorders typically experience more sleep problems than people without such disorders [26]. Thus, clinicians should be alert to the possibility of poor sleep quality in patients with depression, particularly in those who present with multiple sleep problems. Next, we identified Class-2 (Poor sleep quality class) and Class-3 (Poor sleep duration class). Class-2, which included more than a quarter of our sample, was characterized by daytime dysfunction, good sleep duration, and habitual sleep efficiency. Members of Class-3 reported unsatisfactory sleep duration and sleep efficiency, as well as less clear sleep disturbances and less frequent use of hypnotic drugs. In addition to these three groups, the current report also identified Class-4 (Good sleep quality class). Despite not having consistent sleep problem characteristics, it should be noted that Class-2 and Class-3 had similar total scores. The results suggest that the application of overall scores may result in ignoring data associated with the heterogeneous nature of sleep. Thus, future work is needed to examine the different sleep problem characteristics in patients with depression, to optimize targeted intervention measures.
As patients with depressive disorder are very diverse, the demography and the state of depressive disorder have demonstrated a certain level of specificity in predicting the subtypes. Our results showed that participants with daytime dysfunction were younger than those in the other groups. One possible explanation is that young people sleep less at night, which may increase daytime sleepiness and fatigue, leading to daytime dysfunction [27]. This is counter to Julia’s research, which found that daytime dysfunction showed no difference by age [28]. The current findings indicate a potential age difference in daytime dysfunction among adults with depression. Moreover, our results showed that people who experienced more serious symptoms of depression also experienced more sleep problems; this result is consistent with those of other studies [29, 30]. This association could be attributed to poor mental health as a cause of sleep problems [31].
Our findings suggest that, in terms of suicide risk, Class-1 and Class-2 showed significantly higher levels than Class-4 (reference class). In fact, it might be possible for depressed individuals to substitute themselves for a short period of time from everyday issues, while a bad night’s sleep might make it impossible for them to get out of it unless they commit suicide. The Integrated Motivational Will Intervention (IMV) model suggests that a defeat/humiliation experience with no way out is a major factor in suicide attempts [32]. When individuals cannot use effective means, that is, good sleep or escape from unbearable life events, suicide is an alternative approach. Our findings also suggest that certain sleep variables may be weighted more heavily than others in predicting suicide. In this study, although the total scores were close, Class-2 exhibited a higher probability of daytime dysfunction than Class-3, which may contribute to the relatively high risk of suicide in the former. Previous studies have demonstrated that daytime dysfunction, such as daytime sleepiness or difficulty staying awake during the day, is associated with depression [33], life stress [34], life dissatisfaction [35], and hopelessness [36], all of which can increase an individual’s risk of suicidal behavior. A potential explanation is that daytime dysfunction may lead to disrupted sleep–wake cycles and circadian misalignment, resulting in adverse cognitive and emotional consequences [37]. As the mechanism linking daytime sleep disturbance and suicidal ideation is still unclear, future studies need to investigate its relationship with mental and psychological health.
An interesting and thought-provoking finding was that although Class-3 reported significantly poor overall sleep quality (higher than the cut-off PSQI score), when compared with Class 4 (reference class), there was no difference in suicide risk. This finding further demonstrates that the use of total scores is inaccurate for approximating which kind of patient is more likely to commit suicide. This is consistent with the perspective that the use of total scores could lead to disregarding information related to the heterogeneity of sleep problems in patients with depression [38]. A shared characteristic between Class 2 and Class 3 is their similar scores on the PSQI total; however, Class 2 reports worse sleep quality and greater daytime dysfunction than Class 3. On the other hand, Class 3 shows higher scores for sleep duration, indicating shorter sleep times. These observations are consistent with studies demonstrating a strong relationship between sleep quality and quality of life (QOL), whereas the association with sleep duration is less robust [39, 40]. It would be relevant to explore the idea that the connection with overall sleep quality may be more significant than with sleep duration, particularly in relation to the central theme of the study on suicidal risk.
However, the current study has some limitations. First, we used a subjective sleep quality evaluation instead of an objective instrument (for example, polysomnography). As a result, there were no objective data on a number of sleep parameters. However, the PSQI has been reviewed to be more interpretable than other self-reported sleep measures and has been widely used in many studies. Second, due to the cross-sectional nature of the data, the relationships between heterogeneity of sleep problems and suicide risk were associations rather than causal links. In addition, the current study did not consider in depth the heterogeneity of the population with different levels of depression, and future studies need to conduct sensitivity analyses with different participants. Finally, the sample size of this study is relatively small and does not fulfil the EPV (Event Per Variable) requirement. Therefore the results may not be robust enough. However, considering that the number of study participants who possessed suicide risk was more than 70% and the results are somewhat interpretable, they are still presented. In future research, more comprehensive sleep assessments and longitudinal studies of depressed patients are needed, and it should be clearly recognised that suicide is a complex issue that requires more comprehensive consideration of biases caused by psychiatric disorders, life stressors, previous suicidal experiences and social factors to better understand the relationship between changes in various aspects of sleep and suicide.
References
Suicide prevention. https://www.who.int/health-topics/suicide#tab=tab_1.
China health statistics yearbooks. http://www.nhc.gov.cn/mohwsbwstjxxzx/tjzxtjcbw/tjsj_list.shtml.
Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185–99.
Wang X, Cheng S, Xu H. Systematic review and meta-analysis of the relationship between sleep disorders and suicidal behaviour in patients with depression. BMC Psychiatry. 2019;19(1):303.
Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018;212(5):279–86.
Canuso CM, Ionescu DF, Li X, Qiu X, Lane R, Turkoz I, Nash AI, Lopena TJ, Fu DJ. Esketamine nasal spray for the rapid reduction of depressive symptoms in major depressive disorder with acute suicidal ideation or behavior. J Clin Psychopharmacol. 2021;41(5):516–24.
Holma KM, Melartin TK, Haukka J, Holma IA, Sokero TP, Isometsä ET. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: a five-year prospective study. Am J Psychiatry. 2010;167(7):801–8.
Office of the Surgeon, G.; National Action Alliance for Suicide, P., Publications and Reports of the Surgeon General. 2012 national strategy for suicide prevention: goals and objectives for action: a report of the U.S. surgeon general and of the national action alliance for suicide prevention. Washington DC: US Department of Health & Human Services (US); 2012.
Roberts LW, Berk MS, Lane-McKinley K. Ethical considerations in research on suicide prediction: necessity as the mother of invention. JAMA Psychiat. 2019;76(9):883–4.
Chellappa SL, Araújo JF. Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res. 2007;153(2):131–6.
Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, Brown GM, Narashimhan M. Clarifying the role of sleep in depression: a narrative review. Psychiatry Res. 2020;291:113239.
Russell K, Allan S, Beattie L, Bohan J, MacMahon K, Rasmussen S. Sleep problem, suicide and self-harm in university students: a systematic review. Sleep Med Rev. 2019;44:58–69.
Tae H, Jeong BR, Chae JH. Sleep problems as a risk factor for suicide: are certain specific sleep domains associated with increased suicide risk? J Affect Disord. 2019;252:182–9.
Fang X, Zhang C, Wu Z, Peng D, Xia W, Xu J, Wang C, Cui L, Huang J, Fang Y. The association between somatic symptoms and suicidal ideation in Chinese first-episode major depressive disorder. J Affect Disord. 2019;245:17–21.
Geoffroy PA, Borand R, Ambar Akkaoui M, Yung S, Atoui Y, Fontenoy E, Maruani J, Lejoyeux M. Bad dreams and nightmares preceding suicidal behaviors. J Clin Psychiatry. 2022. https://doi.org/10.4088/JCP.22m14448.
McCall WV, Benca RM, Rosenquist PB, Riley MA, McCloud L, Newman JC, Case D, Rumble M, Krystal AD. Hypnotic medications and suicide: risk, mechanisms, mitigation, and the FDA. Am J Psychiatry. 2017;174(1):18–25.
Becker SP, Dvorsky MR, Holdaway AS, Luebbe AM. Sleep problems and suicidal behaviors in college students. J Psychiatr Res. 2018;99:122–8.
Difrancesco S, Lamers F, Riese H, Merikangas KR, Beekman ATF, van Hemert AM, Schoevers RA, Penninx B. Sleep, circadian rhythm, and physical activity patterns in depressive and anxiety disorders: a 2-week ambulatory assessment study. Depress Anxiety. 2019;36(10):975–86.
Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry. 2006;60(12):1364–71.
Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49(1):e63–79.
Yu J, Mahendran R, Abdullah FNM, Kua EH, Feng L. Self-reported sleep problems among the elderly: a latent class analysis. Psychiatry Res. 2017;258:415–20.
Liu X, Tang M, Chen K, Hu L, Wang A. Comparison of the SDS and CES-D in rating depressive symptoms in college students. Chin J Ment Health. 1995;01:19–20.
Chen Y, Zhang B. Latent classes of sleep quality and related predictors in older adults: a person-centered approach. Arch Gerontol Geriatr. 2022;102:104736.
Yue L, Cui N, Liu Z, Jia C, Liu X. Patterns of sleep problems and internalizing and externalizing problems among Chinese adolescents: a latent class analysis. Sleep Med. 2022;95:47–54.
Zhou J, Jin LR, Tao MJ, Peng H, Ding SS, Yuan H. The underlying characteristics of sleep behavior and its relationship to sleep-related cognitions: a latent class analysis of college students in Wuhu city, China. Psychol Health Med. 2020;25(7):887–97.
Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1–22.
Hartley S, Royant-Parola S, Zayoud A, Gremy I, Matulonga B. Do both timing and duration of screen use affect sleep patterns in adolescents? PLoS ONE. 2022;17(10):e0276226.
Boyle JT, Rosenfield B, Di Tomasso RA, Moye J, Bamonti PM, Grandner M, Vargas I, Perlis M. Sleep continuity, sleep related daytime dysfunction, and problem endorsement: do these vary concordantly by age? Behav Sleep Med. 2022;21:436.
Xi S, Gu Y, Guo H, Jin B, Guo F, Miao W, Zhang L. Sleep quality status, anxiety, and depression status of nurses in infectious disease department. Front Psychol. 2022;13:947948.
Plante DT. The evolving nexus of sleep and depression. Am J Psychiatry. 2021;178(10):896–902.
Wang J, Qin W, Pang M, Zhao B, Xu J, Li S, Kong F. The effect of chronic disease and mental health on sleep quality among migrant elderly following children in Weifang city, China. Int J Environ Res Public Health. 2022;19(19):12734.
O’Connor RC, Portzky G. The relationship between entrapment and suicidal behavior through the lens of the integrated motivational-volitional model of suicidal behavior. Curr Opin Psychol. 2018;22:12–7.
Crouse JJ, Carpenter JS, Song YJC, Hockey SJ, Naismith SL, Grunstein RR, Scott EM, Merikangas KR, Scott J, Hickie IB. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention. Lancet Psychiatry. 2021;8(9):813–23.
Nelson KL, Davis JE, Corbett CF. Sleep quality: an evolutionary concept analysis. Nurs Forum. 2022;57(1):144–51.
Weaver TE, Mathias SD, Crosby RD, Bron M, Bujanover S, Menno D, Villa KF, Drake C. Relationship between sleep efficacy endpoints and measures of functional status and health-related quality of life in participants with narcolepsy or obstructive sleep apnea treated for excessive daytime sleepiness. J Sleep Res. 2021;30(3):e13210.
Saguem BN, Nakhli J, Romdhane I, Nasr SB. Predictors of sleep quality in medical students during COVID-19 confinement. L’Encephale. 2022;48(1):3–12.
Liu X, Liu ZZ, Wang ZY, Yang Y, Liu BP, Jia CX. Daytime sleepiness predicts future suicidal behavior: a longitudinal study of adolescents. Sleep. 2019. https://doi.org/10.1093/sleep/zsy225.
Zhang X, Cao D, Sun J, Shao D, Sun Y, Cao F. Sleep heterogeneity in the third trimester of pregnancy: correlations with depression, memory impairment, and fatigue. Psychiatry Res. 2021;303:114075.
Matsui K, Yoshiike T, Nagao K, Utsumi T, Tsuru A, Otsuki R, Ayabe N, Hazumi M, Suzuki M, Saitoh K, Aritake-Okada S, Inoue Y, Kuriyama K. Association of subjective quality and quantity of sleep with quality of life among a general population. Int J Environ Res Public Health. 2021;18(23):12835.
Kudrnáčová M, Kudrnáč A. Better sleep, better life? Testing the role of sleep on quality of life. PLoS ONE. 2023;18(3):e0282085.
Acknowledgements
We thank all the participants who generously shared their time and personal information.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This study was funded by Natural Science Foundation of Ningxia; Grant number: 2020AAC03405.
Author information
Authors and Affiliations
Contributions
HLS: writing original draft, writing review and editing, data curation and software; JS: case diagnosis, inclusion, data curation, software, data curation, writing review and editing; YRW: funding acquisition, project administration, supervision. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest for this study.
Ethical approval
The protocol for this study was approved by the Ethics Committee of General Hospital of Ningxia Medical University. Participants gave oral informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, H., Sun, J. & Wang, Y. Heterogeneity in sleep problems and suicide risk among adults with depression: a cross-sectional study. Sleep Biol. Rhythms (2024). https://doi.org/10.1007/s41105-024-00550-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41105-024-00550-z