Abstract
Daytime sleepiness is common in adolescents. The daytime sleepiness scales developed for western adolescents may not be applicable to Chinese adolescents. This study assesses the psychometric properties of the Chinese adolescent daytime sleepiness scale (CADSS) in a large sample of Chinese adolescents. The CADSS consists of 7 items assessing adolescents’ general feeling of drowsiness and dozing off at different situations during daytime within the past month. Each item is rated on a 5-point scale. A sample of 11,452 adolescents in China completed the CADSS and a structured questionnaire to assess sleep duration, sleep problems, hypnotic use, and behavioral/emotional problems. A subsample of 242 adolescents completed retest questionnaire 2 weeks later. Exploratory factor analysis (EFA), confirmatory factor analysis (CFA), and a receiver operating characteristic (ROC) curve analysis were performed. The CADSS score ranged from 7 to 35 (M = 16.3, SD = 7.4). Internal consistency reliability coefficient was 0.89 and 2-week test–retest reliability coefficient was 0.77. Both EFA and CFA yielded one dominant general factor defined as daytime sleepiness, indicating that the CADSS was essentially unidimensional. The CADSS score was significantly correlated with short nocturnal sleep duration, insomnia symptoms, poor sleep quality, sleep disordered breathing problems, and hypnotic use. ROC analysis indicated that a score of 17 was an acceptable cutoff in distinguishing adolescents with poor daytime functioning. The CADSS is a simple, reliable, and valid scale for assessing daytime sleepiness in Chinese adolescents. Further research is warranted to assess its psychometric properties with clinical samples and non-Chinese adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insufficient sleep, irregular sleep patterns, and daytime sleepiness are common in adolescents due to the misalignment of endogenous circadian rhythms, puberty-related phase delay, and psychosocial developmental needs (such as early school starting) [1, 2]. Epidemiological studies of general adolescent populations demonstrate that most adolescents sleep less than 8 h per night on weekdays [1], 10–20% have difficulty initiating sleep [3,4,5,6], and 20–40% report excessive daytime sleepiness [6, 7]. A growing body of the literature shows that insufficient sleep, sleep disturbances, and excessive daytime sleepiness have negative effects on adolescents’ ability to think and concentrate in school, school performance, behavior and mood during daytime, increased risk for mental health problems, injuries, accidents, and drugs and alcohol use [1, 8,9,10,11]. Several cross-sectional studies have suggested that daytime sleepiness is more strongly than night-time sleep duration associated with poor daytime functioning or that the association between night-time sleep duration and poor daytime function is mediated by daytime sleepiness [12,13,14]. Daytime sleepiness may be more clinically meaningful than sleep duration alone for assessing the adequacy of adolescents’ sleep [14].
Daytime sleepiness is often defined as the subject’s tendency to doze off or to fall asleep, also known as sleep propensity during the day. Although the objective assessments inherent in laboratory test, such as the multiple sleep latency test (MSLT) [15], are available, they cannot capture perceived experience of sleepiness and are not practical and feasible for screening daytime sleepiness in the routine clinical practice and in large-scale epidemiological studies.
To our knowledge, there are 3 subjective daytime sleepiness measures specifically developed for adolescents, including pediatric daytime sleepiness scale (PDSS) [16], the school sleep habits survey (SSHS) [10], and the Cleveland adolescent sleepiness questionnaire (CASQ) [17]. All the scales have shown acceptable internal consistency reliability and construct or concurrent validity. However, all of them were developed based on US adolescents and their reliability and validity may be limited for assessing daytime sleepiness in Chinese adolescents due to social and cultural differences and different school environment and sleep schedules [1, 17,18,19]. For example, the reliability of the PDSS was not consistent between American and Chinese adolescents and between healthy school samples and those with clinically diagnosed sleep disorders [18]. Some questions, such as “Perceived sleepiness while driving a car” in the SSHS and “I feel sleepy when I ride in a bus to a school event like a field trip or sports game” in the CASQ, are not applicable to Chinese adolescents. “I feel sleepy in the evening after school” in the CASQ may be confusing to Chinese adolescents, because Chinese adolescent students usually go to mandatory evening classes and feeling sleepy after the classes is normal. The question “I go through the whole school day without feeling tired” in the CASQ is used to measure fatigue rather than sleepiness [20]. Although the questions ask about sleepiness and wakefulness in a usual week in the CASQ, the response is “never (0 times per month), rarely (<3 times per month), sometimes (1–2 times per week), often (3–4 times per week), and almost every day (≥5 times per week)”. “Never” and “rarely” are confusing to responders. In addition, the PDSS has no specific time frame to assess daytime sleepiness [16]. Furthermore, most measures did not report test–retest reliability and have not been well validated in large samples of general adolescent populations [16,17,18]. Given the above issues of existing measures and Chinese being the largest ethnic group in the world, it is important to develop a simple, reliable, valid, and easily self-administered daytime sleepiness scale for clinical screening and daytime sleepiness research in the general population of Chinese adolescents.
The Chinese adolescent daytime sleepiness scale (CADSS) is a 7-item self-administered questionnaire to assess adolescents’ general feeling of drowsiness and dozing off at different situations during the daytime within the past month. The CADSS was originally developed for Chinese adolescents with consideration of Chinese culture and adolescents’ sleep habits [4, 21] and on the basis of several existing daytime sleepiness measures for western pediatric/adult populations, including PDSS [16], SSHS [10], CASQ [17], the Epworth daytime sleepiness scale (ESS) [22], and the child sleep habits questionnaire (CSHQ) [23], and our series of sleep and health survey in Chinese pediatric populations [4, 19, 24,25,26,27]. The objective of the current study was to assess the psychometric properties of the CADSS in a large sample of Chinese adolescents. Specifically, the first aim was to assess the factor structure of the CADSS by exploratory and confirmatory factor analyses. The second aim was to assess the internal consistency and test–retest reliability of the CADSS. The third aim was to assess its concurrent validity in terms of sleep duration and sleep problems. The fourth aim was to explore the cutoff of the CADSS for predicating poor daytime functioning.
Methods
Participants and procedure
Subjects used for the psychometric assessment of the CADSS were participants of the Shandong adolescent behavior and health cohort (SABHC) in China. Detailed sampling and data collection has been described elsewhere [28]. In brief, participants included 11,836 adolescents from 5 middle and 3 high schools in 3 counties of Shandong Province, China. Shandong, located in the middle and eastern coast of China, is a typical province in terms of population structure and social and cultural life. Shandong has a total population of 95.8 million in 2010 and about half of its population is rural residents. The 3 counties and 8 schools in Shandong were selected for the study, with consideration of their social demographics, the representativeness of adolescent students in the region, prior study collaboration, convenience, and budget to conduct the study. The 8 schools have different morning school start times at 6:20–7:50 a.m. and school end times at 4:20–5:45 p.m.
In November–December 2015, participants were invited to complete a self-administered, structured adolescent health questionnaire (AHQ) to assess sleep, risk behaviors, and mental health. After getting permission from the target schools, trained master-level public health workers administered AHQ to participants in their classrooms during regular school hours. Before filling out the questionnaire, participants were instructed to read the instructions carefully and informed that the survey was anonymous and their participation was voluntary without any penalties for nonparticipation.
The questionnaire was re-administered to 2 classes of middle school students and 2 classes of high school students in the SABHC 2 weeks later to assess the test–retest reliability of the CADSS.
We obtained permission to conduct the study from the principals in the target schools and informed consent from participants before the survey. The study was approved by the research ethics committee of Shandong University School of Public Health and target schools.
Measures
Chinese adolescent daytime sleepiness scale (CADSS)
The CADSS is a self-administered questionnaire. It consists of 7 questions that ask about adolescents’ general feeling of drowsiness and dozing off at different situations during the daytime. The CADSS assesses adolescents’ daytime sleepiness that happened within the past month. Example items are “During the past month, how often would you say you feel sleepy during the day?” “During the past month, how often would you say you have dozed off in the morning classes?” All the 7 items are rated on a 5-point scale from 1 = never, 2 = rarely (<1 time/week), 3 = sometimes (1–2 times/week), 4 = often (3–5 times/week), to 5 = almost every day (6–7 times/week). Summing the scores on the 7 items yields a total CADSS score, ranging from 7 to 35. A higher total score of the CADSS indicates a greater sleep propensity or daytime sleepiness during the past month. The Chinese and English version of the CADSS can be found in the “Appendix”.
Sleep duration and sleep disturbances
Nocturnal sleep duration, insomnia symptoms, sleep disordered breathing, and poor sleep quality during the past month were assessed by the following questions [4, 11, 27]. Sleep duration was asked by “During the past month, on an average school day, how many hours of actual sleep did you get at night?” Insomnia symptoms during the past month were asked about difficulty falling sleep (DIS), difficulty maintaining sleep (DMS), and early morning awakening (EMA) [29]. Sleep disordered breathing was asked about loudly snoring, breath holding or pauses, and snorting/gasping during sleep [23]. Hypnotic use was asked by “How often did you take medicine to help sleep?” The participants answered each question about insomnia, sleep disordered breathing, and hypnotic use with a response from 1 = never, 2 = rarely (<1 time/week), 3 = sometimes (1–2 times/week), 4 = often (3–5 times/week), to 5 = almost every day (6–7 times/week). Insomnia was defined as any of DIS, DMS, and EMA with a response of “often or almost every day (i.e., at least 3 times/week)” [29]. Insomnia severity was the sum of the scores on DIS, DMS, and EMA. Sleep quality was assessed by “During the past month, how would you rate the quality of your sleep overall?” with a 5-point response scale from 1 = excellent, 2 = good, 3 = fair, 4 = poor, to 5 = very poor.
Anxiety/depression
Anxiety and depression were measured by the Youth self-report (YSR) of child behavior checklist [30, 31]. The YSR comprises 103 problem items to which the respondent answers “0” if the problem is not true of him or herself, “1” if the item is somewhat or sometimes true, or “2” if it is very true or often true within the past 6 months. By summing 1s and 2s on all problem items, eight behavioral/emotional syndromes can be assessed. Anxious/depressed subscale was used for the current analysis.
Daytime functioning
Daytime functioning related to sleep was assessed by the question “During the past month, how would you say the negative impact of your sleep problems on your daily activities/functioning?” with a 5-point response scale from 1 = never, 2 = rarely (<1 time/week), 3 = sometimes (1–2 times/week), 4 = often (3–5 times/week), to 5 = almost every day (6–7 times/week). Participants were considered to have poor daytime functioning if their answer was “often or almost every day” (i.e., at least 3 times/week).
Statistical analysis
Means and standard deviations for continuous variables or frequencies for categorical variables were used to summarize data. Correlations among individual items and the correlations between an individual item and total CADSS score of other items were computed. Participants were randomly divided into two subsamples: one for exploratory factor analysis (EFA) and one for confirmatory factor analysis (CFA), to assess construct validity and to compute internal consistency reliability of the CADSS scale. Cronbach’s alpha and coefficient omega were computed to assess internal consistency reliability [32]. Correlation coefficient was computed to measure the 2-week test–retest reliability. Concurrent validity was examined by computing correlations between CADSS score and sleep variables (sleep duration, insomnia, sleep disordered breathing, hypnotic use, and sleep quality). Mean CADSS scores across sleep variables were then compared before and after adjusting for adolescent age, sex, anxiety/depression, and school.
A receiver operating characteristic (ROC) curve analysis was performed to examine the ability of CADSS to predict poor daytime functioning and to identify the optimal cutoffs of excessive daytime sleepiness for predicting poor daytime functioning. The accuracy of prediction was determined by the area under the ROC curve, with an area of 1 representing a perfect test and an area of 0.5 representing a worthless test. The Youden’s index was used to identify the optimal cutoffs. The Youden’s index is computed by sensitivity + specificity −1, ranging between 0 and 1, with the value closer to 1 indicating that the biomarker’s effectiveness is larger [33].
EFA and CFA were conducted in Mplus 7.4 using robust maximum likelihood estimation method. All other statistical analyses were conducted in IBM SPSS Version 22 (Armonk, NY: IBM Corp.).
Results
All sampled students attending school on the day of the survey (n = 11,836) were invited to participate in the SABHC baseline survey. A total of 384 students did not provide a response to any item of the CADSS and were thus excluded, leaving 11,452 participants for the current analysis. Mean age of the sample was 15.0 (SD = 1.5, range 12–18) and 51% were boys. A total of 242 students from 4 classes returned usable retest questionnaires 2 weeks later. Mean age of the test–retest subsample was 14.7 (SD = 1.6) and 53% were girls.
CADSS item analysis
Table 1 describes statistics of each CADSS item and its correlation with total score of other items. More than 30% participants felt sleepy and dozed off easily during the day and more than 20% dozed off in the morning and afternoon classes for ≥3 times per week. Dozing off during watching TV or using internet was less common. The mean score of each item ranged from 1.54 to 3.11. The CADSS items were moderately or highly correlated with each other, with the correlation coefficients ranging from 0.30 to 0.82. Individual items and total score of other items were also moderately or highly and significantly correlated, ranging from 0.45 to 0.83.
Exploratory factor analysis
The first subsample included 5758 participants for EFA. The correlation matrix based on this subsample had two eigenvalues being greater than one (4.221 and 1.041). One-factor model was first run. All 7 items were sufficiently loaded on the general factor with loadings ranged from 0.39 to 0.91. The one-factor model was consistent with our conceptualization that the items were essentially measuring a common factor defined as daytime sleepiness. However, the one-factor model did not fit adequately to the data, χ 2(14) = 1353.09, p < 0.01, RMSEA = 0.129, and CFI = 0.909.
Exploratory bi-factor models were then run with one and two group factors, respectively. The bi-factor model with one group factor showed better fit [χ 2(8) = 613.33, p < 0.01, RMSEA = 0.115, and CFI = 0.959], but the bi-factor EFA model with two group factors fitted the data much better [χ 2(3) = 18.04, p < 0.01, RMSEA = 0.030, and CFI = 0.999]. In the model with two group factors, all items were sufficiently largely loaded on the general factor, daytime sleepiness. The first group factor was dominated by items 5 and 6, and the second group factor was dominated by items 1 and 2. The standardized loadings from one-factor model and two bi-factor models were reported in Table 2.
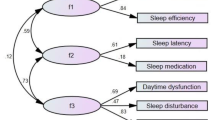
Confirmatory factor analysis
The second subsample contained 5694 for CFA. Because the bi-factor EFA model with 2 group factors fitted the data very well and all items were primarily measuring one common factor, we ran an one-factor CFA model with two correlated residuals: one between item 1 and item 2 and the other between items 5 and 6. This model fitted adequately to the data [χ 2(12) = 453.45, p < 0.01, RMSEA = 0.080, CFI = 0.970]. The standardized loadings ranged from 0.42 to 0.94 and are shown in Fig. 1.
Internal consistency reliability and test–retest reliability
Cronbach’s alpha of the CADSS was 0.89. Based on the CFA model, coefficient omega was 0.88, indicating that 88% of variance among these 7 items was attributable to the common factor. Therefore, the 7 CADSS items scores were summed up to indicate the severity of daytime sleepiness for the following analyses. The test–retest (2-week interval) coefficient of the CADSS was 0.77 (p < 0.0001). The coefficients were very similar between boys (r = 0.77) and girls (r = 0.78).
Concurrent validity
Table 3 reports the correlations between the total CADSS scale score and sleep variables. The CADSS score was significantly correlated with shorter sleep duration, insomnia symptoms, poor sleep quality, hypnotic use, and sleep disordered breathing problems (all p < 0.001). Table 3 also shows the mean CADSS scores across sleep variables before and after adjusting for age, gender, school, and anxiety and depression. Despite the adjustment of demographics and anxiety/depression, mean CADSS scores were significantly higher in adolescents with shorter sleep duration, insomnia, poor sleep quality, hypnotic use, and sleep disordered breathing problems.
Cutoffs for excessive daytime sleepiness of CADSS
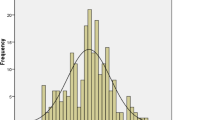
The total CADSS scale score ranged from 7 to 35, with a mean of 16.32 (SD = 7.38) in the sample. Figure 2 displays the distribution of CADSS score and selected percentiles in the sample of adolescents. As shown in Fig. 2, CADSS scores were not normally distributed, with 60% adolescents being scored under 17, 80% under 23 and 95% under 31.
ROC curve analysis was performed to demonstrate sensitivity and false positivity at different cutoffs of CADSS scores for predicting poor daytime functioning related to sleep problems. As shown in Fig. 3, the area under the curve was 0.86 (SE = 0.004, 95% CI = 0.85–0.86, p < 0.0001), indicating that CADSS scale was satisfactory for discriminating those participants with poor daytime functioning related to sleep problems. The cutoff of 16.5 yielded the largest Youden’s index of 0.56, indicating that 16.5 was the best CADSS cutoff score. Using 17 (60th percentile), 23 (80th percentile), and 31 (95th percentile) as cutoffs, the sensitivity and specificity were 77% and 79%, 48% and 92%, and 15% and 99%, respectively.
Based on these percentiles and the results from ROC curve analysis, the possible cutoffs for excessive daytime sleepiness were recommended below.
- Normal:
-
≤16 (≤60th percentile)
- Mild daytime sleepiness:
-
17 (60th percentile)–22
- Moderate daytime sleepiness:
-
23 (80th percentile)–30
- Severe daytime sleepiness:
-
≥31 (95th percentile)
Discussion
Insufficient sleep and daytime sleepiness in adolescents are a world-wide health problem for its adverse impact on daytime functioning [1]. Although several measures have been developed to assess daytime sleepiness in pediatric populations, all of them were originally developed for western adolescents [10, 16,17,18]. Because of differences in social, culture, and school environment or school schedules, the western measures may not be fully applicable to Chinese adolescents [18, 19]. The CADSS is a 7-item self-administered scale for assessing daytime sleepiness within the past month, which was developed based on Chinese culture and school environment and several measures for western pediatric or adult populations [10, 16, 17, 23]. The current study assessed psychometric properties of the CADSS in a large sample of Chinese adolescents (n = 11,452). The psychometric properties of the CADSS are summarized and discussed below.
First, the CADSS demonstrated satisfactory construct validity as assessed by exploratory and confirmatory factor analyses. One general factor could explain 88% of total variance and all the 7 items have a standardized factor loading between 0.42 and 0.94.
Second, the CADSS has satisfactory internal consistency as measured by Cronbach’s alpha (0.89), coefficient omega (0.88), and item-total correlations (0.45–0.83). The internal consistency of the CADSS is comparable or better than that of other existing measures, such as the 8-item PDSS (Cronbach’s alpha = 0.74) [16] and the 16-item CASQ (Cronbach’s alpha = 0.89) [17].
Third, the CADSS has acceptable 2-week test–retest reliability as measured by correlation coefficient (0.77). The existing daytime sleepiness scales have not reported their test–retest reliability [16, 17].
Fourth, the CADSS has good concurrent validities as assessed by significant correlations with short sleep duration, insomnia symptoms, sleep disordered breathing problems, and hypnotic use. Significantly higher CADSS scores were also found in adolescents who slept shorter, had insomnia, SDB, hypnotic use than those who did not before and after adjusting for potential confounding effects of age, gender, school, and anxiety/depression. To our knowledge, CADSS is the only scale that has been validated across multiple sleep problems that may cause daytime sleepiness. CADSS is also the only scale that was validated across multiple sleep variables adjusting for age, gender, school, and anxiety/depression that are all related to daytime sleepiness in adolescents [1, 21].
Fifth, the CADSS demonstrated acceptable discriminating properties to differentiate adolescents with poor daytime functioning as assessed by the area under the curve of 0.86 in the ROC curve analysis. Based on ROC and sensitivity and specificity analyses, scoring 17, 23, and 31 were proposed to be cutoffs of the CADSS for mild, moderate, and severe daytime sleepiness for Chinese adolescents. The existing pediatric daytime sleepiness scales have not recommended cutoffs indicating the severity of daytime sleepiness [16, 17].
Despite the strengths of the study and the sound psychometric properties of the CADSS in a large sample of Chinese adolescents, several limitations need to be considered when interpreting the findings. First, the study did not validate the CADSS with an objective measure of excessive daytime sleepiness such as the MSLT [20]. Second, the study did not include clinical samples of adolescents. Its psychometric properties and proposed cutoffs for clinical use need to be assessed in clinical samples of adolescents with daytime sleepiness complaints/disorders, such as narcolepsy, insomnia, sleep disordered breathing, or circadian rhythm sleep disorders. Third, the measures used to validate the CADSS such as sleep duration, sleep quality, insomnia, SDB, and hypnotic use were all self-reports. Although objective measures for sleep duration and sleep efficiency such as PSG and actigraphy are ideal, it is expensive and not feasible for a large-scale study and research has demonstrated that self-reported sleep duration is correlated with an objective measure such as actigraphy [21, 34]. Furthermore, only adolescents from mainland China were included in the study, it is unknown if the findings could be generalized to other Chinese adolescents outside of mainland China and to non-Chinese adolescents. Further studies are needed to assess its psychometric properties and utility to non-Chinese adolescents and Chinese adolescents outside of mainland China.
In summary, the CADSS consists of only 7 items that measure one general factor, that is, daytime sleepiness. The scale can be easily administered, scored, and interpreted. Despite the limitations of the study, the sound psychometric properties of the CADSS assessed in a large representative sample of adolescents support its suitability for Chinese adolescents for assessing daytime sleepiness. Further assessment with objective sleep measures and with clinical samples would provide new evidence for its clinical and research use in the assessment of adolescent daytime sleepiness.
References
Owens J, Adolescent Sleep Working G, Committee on A. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–32.
Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015;135(3):460–8.
Roberts RE, Roberts CR, Chan W. Persistence and change in symptoms of insomnia among adolescents. Sleep. 2008;31(2):177–84.
Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23(1):27–34.
Hysing M, Pallesen S, Stormark KM, Lundervold AJ, Sivertsen B. Sleep patterns and insomnia among adolescents: a population-based study. J Sleep Res. 2013;22(5):549–56.
Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–8.
Ohida T, Osaki Y, Doi Y. An epidemiologic study of self-reported sleep problems among Japanese adolescents. Sleep. 2004;27(5):978–85.
Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–84.
Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42(3):294–302.
Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69(4):875–87.
Chen H, Bo QG, Jia CX, Liu X. Sleep problems in relation to smoking and alcohol use in Chinese adolescents. J Nerv Ment Dis. 2017;205:353–60.
Perez-Lloret S, Videla AJ, Richaudeau A, et al. A multi-step pathway connecting short sleep duration to daytime somnolence, reduced attention, and poor academic performance: an exploratory cross-sectional study in teenagers. J Clin Sleep Med. 2013;9(5):469–73.
Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline S. Associations of executive function with sleepiness and sleep duration in adolescents. Pediatrics. 2009;123(4):e701–7.
Owens JA, Dearth-Wesley T, Lewin D, Gioia G, Whitaker RC. Self-regulation and sleep duration, sleepiness, and chronotype in adolescents. Pediatrics. 2016;138(6):e20161406.
Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986;9(4):519–24.
Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003;26(4):455–8.
Spilsbury JC, Drotar D, Rosen CL, Redline S. The Cleveland adolescent sleepiness questionnaire: a new measure to assess excessive daytime sleepiness in adolescents. J Clin Sleep Med. 2007;3(6):603–12.
Ji X, Liu J. Subjective sleep measures for adolescents: a systematic review. Child Care Health Dev. 2016;42(6):825–39.
Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among school children in the United States and China. Pediatrics. 2005;115(1 Suppl):241–9.
Moore M, Kirchner HL, Drotar D, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34(10):1175–83.
Liu X, Zhao Z, Jia C, Buysse DJ. Sleep patterns and problems among Chinese adolescents. Pediatrics. 2008;121(6):1165–73.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5.
Owens JA, Spirito A, McGuinn M. The children’s sleep habits questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–51.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27(7):1351–8.
Liu X, Zhou H. Sleep duration, insomnia and behavioral problems among Chinese adolescents. Psychiatry Res. 2002;111(1):75–85.
Liu X, Chen H, Bo QG, Fan F, Jia CX. Poor sleep quality and nightmares are associated with non-suicidal self-injury in adolescents. Eur Child Adolesc Psychiatry. 2017;26(3):271–9.
Liu X, Zhao Z, Jia C. Insomnia symptoms, behavioral/emotional problems, and suicidality among adolescents of insomniac and non-insomniac parents. Psychiatry Res. 2015;228(3):797–802.
Chen H, Wang XT, Bo QG, Zhang DM, Qi ZB, Liu XC, Jia CX. Menarche, menstrual problems and suicidal behavior in Chinese adolescents. J Affect Disord. 2017;209:53–8.
Association AP. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Publishing; 2013.
Achenbach TM. Manual for the youth self-report and 1991 profile. University of Vermont, Burlington, VT, 1991.
Liu XC, Guo CQ, Liu LQ, Sun LM. Reliability and validity of the youth self-report (YSR) of Achenbach’s child behavior checklist (CBCL). Chin Mental Health J. 1997;11(4):200–3 (in Chinese).
Yang Y, Green SB. Coefficient alpha: a reliability coefficient for the 21st century? J Psychoeduc Assess. 2011;29(4):377–92.
Goddard MJ, Hinberg I. Receiver operator characteristic (ROC) curves and non-normal data: an empirical study. Stat Med. 1990;9(3):325–37.
Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–6.
Acknowledgements
The authors would like to thank Lijin County Center for Disease Control and Prevention, Zoucheng City Center for Disease Control and Prevention, and Yanggu County Center for Disease Control and Prevention, Shandong Province, China and all participating school teachers for their help with data collection and all students for their voluntarily participating in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was funded by the Shandong Scientific Technique Development Plan (Grant No. 2014GSF118163) and National Natural Science Foundation of China (Grant No. 81573233).
Conflicts of interest
All authors have no conflict of interest.
Ethical approval
This study was approved by the research ethics committee of Shandong University and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Appendix
Appendix
Chinese adolescent daytime sleepiness scale (CADSS)

During the past month, how often would you say you have had any of these sleep problems? Please circle your answer to the following questions.

Rights and permissions
About this article
Cite this article
Liu, X., Yang, Y., Liu, ZZ. et al. Psychometric assessment of the Chinese adolescent daytime sleepiness scale (CADSS). Sleep Biol. Rhythms 15, 207–216 (2017). https://doi.org/10.1007/s41105-017-0106-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-017-0106-x