Abstract
Purpose of Review
Traveling through deep space raises challenges to biological systems that have not been fully appreciated or addressed. In addition to the lack of gravity, the space environment includes exposure to charged remnants of supernova explosions beyond our solar system that travels with enormous velocities and energies, called HZE (high atomic number Z and energy E) particles and have the potential to disrupt chemical bonds within the human body though ionization. As a process, the collision of charged particles with matter is not new to physicists and biologists on Earth, and we have extensive data on low-linear energy transfer (LET) ionizing radiation from both accidental and deliberate exposures, dating back to the discovery of radioactive isotopes by Madame Curie. One of the primary morbidities associated with radiation exposure is the challenge to the hematopoietic system. The purpose of the current review is to discuss some of the basic tenants of hierarchical tissue systems by elaborating the effects of radiation damage to the hematopoietic stem cell and how terrestrial radiation and space radiation differ.
Recent Findings
The last few decades of research in the field of space radiation, which consists of high-LET ions of 4He, 12C, 16O, 28Si, 48Ti, and 56Fe, and low-LET protons, have shown that there is a significantly more deleterious impact on the hematopoietic system by the high-LET ions compared to protons, X-rays, and γ-rays. Ground-based high-LET radiation experiments have shown not only in vitro and in vivo adverse effects on hematopoietic stem cells, but also that human leukemia can be induced in humanized mouse models.
Summary
High-LET space radiation is more lethal to hematopoietic stem cells compared to low-LET radiation, but further research is required in order to understand the impact of high-LET radiation on hematopoietic malignancies. Most of the ground-based studies, because of technical difficulties and cost issues, have been carried out at high dose rates with only one ion species at a time. What remains to be clearly described, however, is the potential damage to the hematopoietic system from exposure to the more complex types of radiation at low dose rates that will occur during space travel and how space agencies can sufficiently protect our astronauts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the dawn of space exploration, the National Aeronautics and Space Administration (NASA) and other space agencies around the world have wondered how far in deep space humans can go, survive, and still return to earth safely. NASA’s manned missions to the moon landed the first humans on the surface in 1969. However, more than 45 years have passed since those initial triumphs, and we have not yet returned to the moon or sent humans beyond our celestial partner. NASA’s next ambitious manned missions includes sending astronauts to the moon and eventually Mars and back, a journey that will take roughly 2 to 3 years including time on the surface for research purposes, significantly longer than the 10-day journeys of the Apollo missions and beyond the protection afforded by the Earth’s magnetosphere. Long-term space travel requires a deeper understanding of the effects of the space environment on human physiology, which can be affected by factors such as microgravity, environmental constraints, and emotional stress. Only through pushing our primarily earth-based experimental models to the extreme can we begin to gain insight into how we will fare so far from home.
One of the major underappreciated health concerns for the long-term deep-space missions is the exposure to space radiation. While there are highly accurate predictions of the types and doses of radiation in deep space from various Mars-bound vehicles, we currently have a poor understanding of how exposure to it will influence human health directly, and thus, we lack of a predictable health risk model for deep-space endeavors. Space radiation consists of a broad spectrum of low- and high-linear energy transfer (LET) radiations coming from galactic cosmic radiation (GCR), solar energetic particles (SEP) emitted from the sun itself, and trapped energetic particles in the Van Allen radiation belts [1,2,3]. GCR are composed of high-energy protons (85%), helium ions (14%), and nuclei of heavier elements such as 12C, 16O, 20Ne, 28Si, 40Ca, 48Ti, and 56Fe ions, called HZE (high atomic number Z and energy E) particles (1%) [4]. SEPs and trapped energetic particles in the Van Allen radiation belts include low- to medium-energy protons and electrons [4]. Astronauts on the International Space Station (ISS) travel below and through the Van Allen belts and are generally protected from SEPs and most of the GCR by the magnetic field of the earth and to a lesser extent by the extensive shielding materials on the station itself, which can absorb lower energy protons and charged particles. However, astronauts on deep-space missions will be challenged by GCR and SEP radiation, occasional solar weather changes in the form of fairly high dose rate solar particle events (SPEs), and the Van Allen radiation belts as they travel beyond low earth orbit with only the spacecraft hull and contents to shield them [5]. Despite the low frequency of HZE ions, contributing to only 1% of GCR, HZE ions deliver about 1–2 mSv whole-body dose per day and have dense ionization patterns such that they are the main contributor to risk from space radiation [4, 6]. Therefore, the deep-space environment includes radiation exposure to HZE particles that we as a species have not endured, but will need to resolve before a 2–3-year-exposure during a Mars mission.
The most extensive data on the devastating effects of low-LET radiation on human health were derived from individuals exposed to the atomic bomb explosions in Hiroshima and Nagasaki in 1945. Two of the most sensitive organ systems have proven to be the hematopoietic and the gastrointestinal systems, with dose being the most discriminating factor between onset and severity of the two. Analysis of survivors of the immediate bomb blasts have found that the majority of ionizing radiation (IR)-related deaths were associated with hematopoietic failure caused by total body irradiation (TBI), including individuals who received doses between 2.5–5 Gy [7,8,9]. For long-term survivors, increased cancer risk has become a significant cause of death, with leukemia having the highest relative risk of any malignancy [10]. However, studies have shown that high-LET radiations typical of the GCR are more damaging than low-LET radiations such as X-rays or γ-rays, and thus, risk prediction models for astronaut health effects need to be adjusted [11•]. The major space radiation-associated health risks that have been identified in various experimental models here on Earth using ground-based particle accelerator facilities are degenerative damage to various organ systems (including the circulatory system, central nervous system, and bone, muscle, and cartilage microarchitecture), cataract formation, and genetic mutations and cancer, which are all thought to occur in the relatively low-dose environment of space [5]. Various studies have been carried out using mouse models of carcinogenesis to understand the types of cancers that might occur in humans in response to HZE ion exposure, such as mammary tumor, melanoma, hepatocellular carcinoma, intestinal colorectal cancer, and leukemia [12,13,14]. The radiosensitive nature of the hematopoietic system makes it a crucial target for investigating the impact of high-LET irradiation in animal models in order to extrapolate the risk to human in the space radiation environment. A better understanding of the harmful impact of space radiation will also allow us to design appropriately targeted radioprotectors, mitigators, and novel shielding designs and materials to protect astronauts for future deep-space missions. This review includes recent findings of the harmful impact of high-LET IR on hematopoietic stem cells (HSCs), along with an overview of what has been learned over recent decades of investigation into HSC maintenance and the effects of low- and high-LET radiations.
Bone Marrow Niche and HSC Homeostasis
Hematopoietic stem cells generate billions of cells every day throughout the life of an organism via the orchestrated processes of proliferation, self-renewal, and differentiation into functional blood cells [15,16,17,18]. Internal and external stresses continuously threaten HSC integrity, and accumulation of genetic instability could lead to either stem cell failure or hematopoietic malignancies. HSCs remain largely quiescent, effectively minimizing endogenous stress caused by cellular respiration and DNA replication processes [19]. When forced to enter a proliferative state, the health of HSCs depends on factors and cellular players in the bone marrow (BM) niche, including perivascular cells, endothelial cells, osteoblasts, macrophages, and sympathetic nerves [20, 21]. HSC homeostasis is affected by niche signaling, niche location, HSC stress and regeneration after injury, and even aging. Therefore, hematopoiesis is a tightly controlled process occurring in the marrow microenvironment that controls HSC potency and ultimately organismal health [22]. However, HSC homeostasis is governed by many molecular pathways that have been discovered over recent decades and will not be discussed here, as they have been reviewed by others [23, 24].
Over the life of an organism, HSCs are continuously challenged by various stresses such as oxidation, hypoxia, inflammation, and terrestrial radiation, which is composed of ~ 55% of high-LET-charged particles from radon and its decay progeny [25]. Thus, understanding normal hematopoietic homeostasis and responses to these exogenous stressors can inform about how HSC will tolerate space radiation. In the context of cancer therapy, it is well appreciated that therapeutic radiation is used in the treatment of a broad spectrum of cancers including hematopoietic malignancies such as leukemia or lymphoma, and can also lead to bone marrow injury [15]. From a radiobiology perspective, many laboratory studies have shown that the hematopoietic system is the most radiosensitive, and damage caused by IR may lead to hematopoietic dysfunction or malignancies [8]. In addition, damage to the HSCs themselves or damage to the supportive BM niche cells could lead to altered HSC repopulation and bone marrow vascularization, exacerbating the harmful impact of IR [26, 27]. Collectively, many years of clinical experience and laboratory research have shown that IR is one of the major stressors for the hematopoietic system by inducing genomic instability leading to stem cell defects.
Hematopoietic Stem Cell Injuries Caused by Low-LET Ionizing Irradiation
Low-LET IR contains enough energy to remove tightly bound electrons from the orbits of atoms, causing ionization of target materials including biological ones. IR can disrupt the structure and function of DNA, lipids, and proteins and can lead to functional changes that may cause cell cycle arrest, senescence, malignant transformation, or even cell death. Ionization of DNA is particularly worrisome because it can cause DNA single- and double-stranded breaks, DNA-DNA and DNA-protein crosslinks, and oxidized base and sugar damages, which if unrepaired or misrepaired may lead to the accumulation of mutations that will have lasting effects. IR damage occurs through both direct and indirect mechanisms by deposition of energy into DNA itself and by the hydrolysis of nearby water molecules that produces free radicals such as hydroxyl radicals, superoxide anions, hydrogen peroxide, and others, which in turn can chemically alter DNA and chromatin proteins in the near vicinity. IR-induced damage does lead to a hematopoietic malignancy in humans, typically acute and chronic myeloid leukemias [28,29,30]. Apart from HSC malignancies, IR exposure can also increase risk of local and systemic infections, anemias, and potentially even susceptibility to other cancer through compromised immune function [31]. Therefore, elucidating mechanisms of IR-induced HSC injury are important to understand the susceptible nature of hematopoietic system. Several processes have been identified to have a role in IR-induced HSC injury, including [1] reduction in the number of HSCs due to apoptosis, senescence, or differentiation and [2] damage to the niche microenvironment affecting niche signaling [32,33,34]. IR is a potent activator of apoptosis and studies have shown that modulating the expression levels of a key anti-apoptotic protein, BCL-2, can protect the hematopoietic compartment against radiation-induced HSC death [35, 36]. Moreover, recent studies have investigated the role of Puma, pro-apoptotic BH3-only protein, and have shown that it plays a crucial role in IR-induced HSC apoptosis [37, 38].
Radiation also affects differentiation of HSCs, and a recent study has shown that exposure to IR depletes HSCs by boosting their differentiation into the lymphoid lineage [39]. In the early 1960s, it was demonstrated that human diploid fibroblasts have a limited growth efficacy due to finite length of telomeres that function to “cap” the end of chromosomes [40, 41]. The first evidence of senescence in hematopoietic stem cells was observed in Bmi1−/− mice where knockout mice developed progressive BM hypoplasia leading to early death [42, 43]. In fact, the study has shown that IR treatment induces senescence in vitro and in vivo with increased expression of SA-B-gal, p16, and Arf [33, 34]. Radiation-induced senescence is a well-described process that relates to production of reactive oxygen species (ROS) in fibroblasts and is likely also highly relevant in the HSC setting [44,45,46]. In fact, it was found that ataxia-telangiectasia-mutated (ATM−/−) mice exhibited progressive failure of hematopoietic function attributed to premature senescence due to increased production of ROS [46]. Finally, studies have also shown that IR not only affects HSCs directly, but also induces significant BM stroma (including fibroblasts) injury in a time- and dose-dependent manner [47,48,49]. Collectively, these data suggest that HSC would be quite sensitive to IR damage due to exposure to space radiation.
Protecting humans from IR exposure that causes stem cell damage and HSC damage in particular is a significant challenge. To date, many studies have focused on designing biomarkers that can predict long-term radiation injuries and assess the efficacy of chemical radioprotectors (delivered prior to exposure) and mitigators (delivered post-exposure) that could significantly minimize damage. Antioxidants, such as N-acetyl cysteine (NAC), have demonstrated utility in preventing low-LET proton-induced BM failure by reducing ROS levels in a mouse model [50]. Resveratrol has also shown reducing the effects of IR by acting as a strong antioxidant and a potent activator of Sirtuin1 (Sirt1) in mice [51]. Amifostine is a well-studied radioprotector in pre-clinical and clinical settings but has significant side effects making it impractical for human use [52]. In general, antioxidants are a part of an important regimen to reduce the effects of exposure to low-LET ionizing radiation. However, antioxidants are not likely to be a sufficient strategy on their own to protect astronauts from space radiation because of the different nature of high-LET radiation-induced damage.
SPE and GCR Impact on Hematopoietic Stem/Progenitor Cells
On the journey to Mars, every cell in an astronaut’s body will be hit by low- and medium-energy 1H ions (protons) approximately every 3–4 days, 2He nuclei every few weeks, and HZE particles every few months [5]. Radiation exposure from these sources during spaceflight could have profound short- and long-term negative impacts on human physiology including morbidity/mortality in astronauts [1, 53, 54]. Unlike low-LET photon-based radiations such as X- and gamma rays, high-LET radiations such as HZE particles deposit a large amount of energy in a very small distance (the penumbra) from the particle core through energy depositions by the ion itself and large numbers of so-called delta-ray electrons ejected along its path. These highly localized energy depositions can create patterns of complex or clustered DNA damage consisting of multiple base modifications, single-strand breaks, and double-strand breaks within a few helical DNA turns [55, 56]. The complexity of clustered DNA damage increases with increasing Z of HZE particles, rendering DNA repair even more difficult [1]. Unrepaired DNA damage in HSCs is thought capable of inducing either clonogenic death or substantial genomic instability leading to cancer. Therefore, it is crucial to study the effect of HZE particles on HSCs and their functionality in order to better understand the health risks associated with space travel.
NASA has the goal of generating risk models for space travel that limit the risk of mortality by cancer to a 3% overall increase [1]. We have established that the human hematopoietic system is highly sensitive to the development of leukemia and lymphomas from exposure to low-LET sparsely ionizing X- and γ-rays, which are a well-known outcome in the A-bomb survivors. Protons, which are the most frequent IR species in the SEP and GCR fields in space, are charged particles that have similar LET values to γ-rays, making them an important ion species to study the risk associated with space travel under the general hypothesis that information gleaned from terrestrial radiation sources would be applicable. Many studies have been carried out to compare the effects of different energy protons on experimental cell and animal models including effects of TBI proton exposure on the hematopoietic system, using cesium-137 or cobalt-60 gamma rays as reference standard radiations. Simulated SPE protons at a dose of 0.5 or 1 Gy have shown significant increased chromosomal aberration in lymphocytes up to 2 months post-exposure compared to untreated mice [57]. C57BL/6J mice exposed to 1 Gy of 150 MeV 1H irradiation showed substantial BM injury resulting in significant lower frequency of HSCs long term after whole-body exposure [58]. Sequential exposure to protons (1 GeV) and heavy ion such as 56Fe ions (1 GeV/n) showed significant deleterious in vitro impact on HSC colony formation [59••]. These studies imply that despite their similar LET values, protons likely have increased potential for short- and long-term harmful impacts to human hematopoietic system.
Though much lower in frequency than protons, the GCR field is also composed of low-LET 2He nuclei and nuclei of lighter elements such as 12C, 16O, 20Ne, and 28Si with LET values ~ 10-fold higher than protons whose effects are poorly understood regarding impact on the hematopoietic stem cell population. The growing interest and investment in heavy ion (hadron) radiotherapy such as 12C ion therapy for cancer treatment also demands careful determination of HZE ion effects on normal physiology. Heavy ion radiotherapy takes advantage of the Bragg curve of the charged particle, which describes the relationship of energy delivered versus distance, to deliver highly localized doses precisely to a tumor at the particle’s so-called Bragg peak, thereby limiting exposure to the normal tissue beyond the target area. However, the effect of heavy ion exposure on normal circulating HSC or in the marrow within the treatment field could in theory lead to DNA damage and even malignant development. Thus, there is significant justification for understanding the effects of hadrons on the HSC on normal tissues as well.
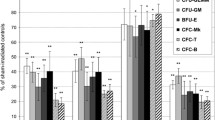
CD34+ stem cells from human placental/umbilical cord blood exposed in vitro to carbon ion (290 MeV/n) at 0.5 or 1.5 Gy dose inflict severe damage to clonal growth of myeloid hematopoietic stem/progenitor cells (HSPCs) compared to low-LET X-rays [60]. The short- and long-term impact of HZE particles on the hematopoietic system was also studied recently in a rodent model. Acute effects of a 1 Gy TBI 16O ion irradiation (600 MeV/n) on C57BL/6J mice showed a significant decrease in peripheral blood cells at 2 weeks that was correlated with substantial reduction in HSPC clonogenic potential in an in vitro assay compared to sham-irradiated controls [61]. Epigenetic changes, such as DNA methylation, are known to align with HSC lineage commitment and can demonstrate changes after significant cellular stress and even correlate with carcinogenesis [13, 62, 63]. Exposure of CBA/CaJ mice to doses less than 0.5 Gy of 28Si ions (300 MeV/n) resulted in an increased chromosomal aberrations and a global inhibition of 5-hydroxymethylcytosine in HSPCs 6 months postirradiation compared to sham controls [64••]. Furthermore, it was also shown that whole-body 28Si ion exposure in CBA/CaJ mice caused significantly higher levels of apoptotic cell death and inflammatory response in BM cells 6 months post-exposure compared to sham-irradiated mice [65]. These findings suggest that medium-LET HZE particle irradiation has short- and long-term effects on HSCs and like high LET HZE ions, which are beginning to demonstrate some unpredicted changes to HSC biology compared to standard X- and gamma-ray radiation.
Studies have also been carried out in animal models to understand the effects of high-LET HZE particles (48Ti and 56Fe ions) on HSCs. Proteomic profiling of murine HSPCs after exposure to 48Ti ions (1 GeV/n) identified networks related to cancer, hematological disorders, and immunological diseases by Ingenuity Pathway Analysis (IPA) 6 months postirradiation [66]. One of the most biologically significant components of health risks from GCR exposures in space are 56Fe ions. Even though their frequency in the GCR field is minor, the overall dose equivalent resulting from exposure to 56Fe ions constitutes almost 25% of the total dose equivalent due to GCR [67]. Mice exposed to 0.4 Gy of 56Fe ions (600 MeV/n) showed persistent and significant changes in epigenetic status, including DNA methylation patterns, in HSPCs compared to terminally differentiated BM cells [68•]. Chromosomal damage in bone marrow cells collected from CBA/CaJ mice showed that 56Fe ion (1000 GeV/n) exposure resulted in higher frequencies of chromosomal exchanges and breaks compared to γ-rays [69]. Studies have also demonstrated that whole-body 56Fe ion irradiation cause leukemia and lymphoma in mice [13, 70]. In addition, studies in humanized mouse models, which have the significant advantage of assessing the effects on human HSCs in an in vivo setting, showed that 20 cGy of 56Fe ions (1 GeV/n) could reproducibly result in the development of human T cell acute lymphoblastic leukemia (T-ALL) 6–9 months post-transplant [59••]. Remarkably, this is the first example of HZE ion-induced human leukemia. Collectively, the findings suggest that high-LET radiation that will confront astronauts during deep-space missions can also significantly lead to hematopoietic dysfunction or malignancies.
Despite continuous improvements in spacecraft-shielding materials and designs, exposure to SEPs and GCR cannot be completely eliminated by adding more spacecraft shielding due to the simple issue of weight limitation. The thickness of the spacecraft required to fully shield against all incident radiation would not be practically possible and becomes complicated by the fact that GCR ions result in fragmentation of the hull materials and can deliver similar cumulative doses inside the spacecraft by multiple secondary fragments typically with high-LET values as well [71, 72]. Traditional antioxidants have shown to be moderately useful in minimizing the harmful effects of low-LET IR on humans and could also be useful as an adjunct therapy to minimize cell damages created by the low-LET delta rays coming off of HZE particles core. However high-LET-charged particles themselves create higher levels of direct damage to DNA (in addition to indirect damage by delta rays) by generating clustered DNA lesions that makes antioxidant strategies less effective. Apart from shielding and antioxidants, one recent study has shown that a single dose of the steroid hormone androstenediol (Δ5 androsten-3β, 17β-diol [AED]) could ameliorate hematopoietic injury caused by 3 Gy of 56Fe (1 GeV/n) ion exposure in a mouse model [73]. Beyond this exciting initial story, with an incompletely defined mechanism, the effects of GCR on the hematopoietic system remain a significant concern for space travel. Cumulatively, these studies have shown that low- and high-LET charged particles in the space radiation environment are more damaging to hematopoietic stem/progenitor cells than low-LET X- and gamma radiations and further investigation is necessary in order to design better strategies to keep astronauts healthy during and well after they return from deep-space missions.
Conclusion
The nature of human curiosity and technology of the twenty-first century has brought us to a place where traveling into deep space is no longer an unreachable dream. Human space exploration has the potential to open up new avenues for discoveries that will eventually benefit all of society. Government space agencies and private companies around the world are working towards a shared goal that includes human-based deep-space missions in the near future, including plans to send astronauts back to the moon and to Mars by 2030, feats which are not only limited by significant technical challenges but also by concerns of human health over the 2–3-year journey and for the remainder of lives of the astronauts back on earth. We as a species have not lived or traveled in deep space to understand the health challenges that we will encounter during the Mars mission. However, the moon missions and ISS missions have given us some insight into health risks associated with traveling into deep space and that IR exposure and its effects are principal among them. So far, many decades of research with IR has shown its harmful effects on almost every organ system in human biology with the hematopoietic system in particular being one of the most vulnerable. While recent research has shown the adverse effects of low- and high-LET-charged particle radiation on HSCs, we have not yet developed a precise, quantitative, risk-assessment model that can be used to determine health risks associated with long-term space travel beyond low earth orbit. One of the reasons for not achieving this goal is the cost and technical difficulties associated in replicating the exact space radiation conditions on earth for experimental purposes. So far, ground-based space radiation experiments have been carried out at high dose rates with either a single ion species, or sequential exposure to limited different ions. However, we know that during space explorations, astronauts will be exposed to a broad spectrum of different ions at different energies at any given time point with a cumulative dose rate in mSv/day. These facts suggest that future studies should focus on understanding the impact of low dose rate and mixed ion irradiation on the hematopoietic system. Therefore, extensive research of the space radiation effects on HSCs will not only assess the dangers of space travel, but also help to design better strategies to protect astronauts during and after deep-space missions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cucinotta FA, Schimmerling W, Wilson JW, Peterson LE, Badhwar GD, Saganti PB, et al. Space radiation cancer risks and uncertainties for Mars missions. Radiat Res. 2001;156:682–8.
Edwards AA. RBE of radiations in space and the implications for space travel. Physica Medica: PM: An International Journal Devoted to the Applications of Physics to Medicine and Biology: Official Journal of the Italian Association of Biomedical. Physics. 2001;17(Suppl 1):147–52.
Schimmerling W, Cucinotta FA, Wilson JW. Radiation risk and human space exploration. Adv Space Res: Off J Committee Space Res. 2003;31:27–34.
Heinrich W, Roesler S, Schraube H. Physics of cosmic radiation fields. Radiat Prot Dosim. 1999;86:253–8.
Chancellor JC, Scott GB, Sutton JP. Space radiation: the number one risk to astronaut health beyond low Earth orbit. Life. 2014;4:491–510.
Saganti PB, Cucinotta FA, Wilson JW, Simonsen LC, Zeitlin C. Radiation climate map for analyzing risks to astronauts on the mars surface from galactic cosmic rays. Space Sci Rev. 2004;110:143–56.
Hall EJ, Giaccia AJ. Radiobiology for the radiologist. 6th edition, 2006; ix:546.
Waselenko JK, MacVittie TJ, Blakely WF, Pesik N, Wiley AL, Dickerson WE, et al. Medical management of the acute radiation syndrome: recommendations of the Strategic National Stockpile Radiation Working Group. Ann Intern Med. 2004;140:1037–51.
Shao L, Luo Y, Zhou D. Hematopoietic stem cell injury induced by ionizing radiation. Antioxid Redox Signal. 2014;20:1447–62.
Shimizu Y, Kato H, Schull WJ. Risk of cancer among atomic bomb survivors. J Radiat Res. 1991;32 Suppl 2:54-63.
• Cacao E, Hada M, Saganti PB, George KA, Cucinotta FA. Relative biological effectiveness of HZE particles for chromosomal exchanges and other surrogate cancer risk endpoints. PLoS One. 2016;11:e0153998. This article provides detailed RBE prediction based on a parametric track structure model to chromosomal exchanges occurring in normal human lymphocyte and fibroblast cells and comparing to published data for malignant transformation
Bielefeldt-Ohmann H, Genik PC, Fallgren CM, Ullrich RL, Weil MM. Animal studies of charged particle-induced carcinogenesis. Health Phys. 2012;103:568–76.
Weil MM, Bedford JS, Bielefeldt-Ohmann H, Ray FA, Genik PC, et al. Incidence of acute myeloid leukemia and hepatocellular carcinoma in mice irradiated with 1 GeV/nucleon (56)Fe ions. Radiat Res. 2009;172:213–9.
Datta K, Suman S, Kallakury BV, Fornace AJ Jr. Exposure to heavy ion radiation induces persistent oxidative stress in mouse intestine. PLoS One. 2012;7:e42224.
Lucas D, Scheiermann C, Chow A, Kunisaki Y, Bruns I, Barrick C, et al. Chemotherapy-induced bone marrow nerve injury impairs hematopoietic regeneration. Nat Med. 2013;19:695–703.
Pietras EM, Lakshminarasimhan R, Techner JM, Fong S, Flach J, Binnewies M, et al. Re-entry into quiescence protects hematopoietic stem cells from the killing effect of chronic exposure to type I interferons. J Exp Med. 2014;211:245–62.
Lymperi S, Ferraro F, Scadden DT. The HSC niche concept has turned 31. Has our knowledge matured? Ann N Y Acad Sci. 2010;1192:12–8.
Wang LD, Wagers AJ. Dynamic niches in the origination and differentiation of haematopoietic stem cells. Nat Rev Mol Cell Biol. 2011;12:643–55.
Orford KW, Scadden DT. Deconstructing stem cell self-renewal: genetic insights into cell-cycle regulation. Nat Rev Genet. 2008;9:115–28.
Friedenstein AJ, Chailakhyan RK, Latsinik NV, Panasyuk AF, Keiliss-Borok IV. Stromal cells responsible for transferring the microenvironment of the hemopoietic tissues. Cloning in vitro and retransplantation in vivo. Transplantation. 1974;17:331–40.
Song J, Kiel MJ, Wang Z, Wang J, Taichman RS, Morrison SJ, et al. An in vivo model to study and manipulate the hematopoietic stem cell niche. Blood. 2010;115:2592–600.
Morrison SJ, Scadden DT. The bone marrow niche for haematopoietic stem cells. Nature. 2014;505:327–34.
Mendelson A, Frenette PS. Hematopoietic stem cell niche maintenance during homeostasis and regeneration. Nat Med. 2014;20:833–46.
Crane GM, Jeffery E, Morrison SJ. Adult haematopoietic stem cell niches. Nat Rev Immunol. 2017;17(9):573-90.
Suda T, Takubo K, Semenza GL. Metabolic regulation of hematopoietic stem cells in the hypoxic niche. Cell Stem Cell. 2011;9:298–310.
Cao X, Wu X, Frassica D, Yu B, Pang L, Xian L, et al. Irradiation induces bone injury by damaging bone marrow microenvironment for stem cells. Proc Natl Acad Sci U S A. 2011;108:1609–14.
Ito K, Hirao A, Arai F, Takubo K, Matsuoka S, Miyamoto K, et al. Reactive oxygen species act through p38 MAPK to limit the lifespan of hematopoietic stem cells. Nat Med. 2006;12:446–51.
Bizzozero OJ Jr, Johnson KG, Ciocco A. Radiation-related leukemia in Hiroshima and Nagasaki, 1946–1964 I. Distribution, incidence and appearance time. N Engl J Med. 1966;274:1095–101.
Yoshinaga S, Mabuchi K, Sigurdson AJ, Doody MM, Ron E. Cancer risks among radiologists and radiologic technologists: review of epidemiologic studies. Radiology. 2004;233:313–21.
Radivoyevitch T, Sachs RK, Gale RP, Molenaar RJ, Brenner DJ, Hill BT, et al. Defining AML and MDS second cancer risk dynamics after diagnoses of first cancers treated or not with radiation. Leukemia. 2016;30:285–94.
Brook I, Elliott TB, Ledney GD, Knudson GB. Management of postirradiation sepsis. Mil Med. 2002;167:105–6.
Dominici M, Rasini V, Bussolari R, Chen X, Hofmann TJ, Spano C, et al. Restoration and reversible expansion of the osteoblastic hematopoietic stem cell niche after marrow radioablation. Blood. 2009;114:2333–43.
Meng A, Wang Y, Brown SA, Van Zant G, Zhou D. Ionizing radiation and busulfan inhibit murine bone marrow cell hematopoietic function via apoptosis-dependent and -independent mechanisms. Exp Hematol. 2003;31:1348–56.
Meng A, Wang Y, Van Zant G, Zhou D. Ionizing radiation and busulfan induce premature senescence in murine bone marrow hematopoietic cells. Cancer Res. 2003;63:5414–9.
Domen J, Gandy KL, Weissman IL. Systemic overexpression of BCL-2 in the hematopoietic system protects transgenic mice from the consequences of lethal irradiation. Blood. 1998;91:2272–82.
Domenech J, Cartron G, Clement N, Estienne MH, Herault O, Truglio D, et al. Persistent decrease in proliferative potential of marrow CD34(+)cells exposed to early-acting growth factors after autologous bone marrow transplantation. Bone Marrow Transplant. 2002;29:557–62.
Shao L, Sun Y, Zhang Z, Feng W, Gao Y, Cai Z, et al. Deletion of proapoptotic Puma selectively protects hematopoietic stem and progenitor cells against high-dose radiation. Blood. 2010;115:4707–14.
Yu H, Shen H, Yuan Y, XuFeng R, Hu X, Garrison SP, et al. Deletion of Puma protects hematopoietic stem cells and confers long-term survival in response to high-dose gamma-irradiation. Blood. 2010;115:3472–80.
Wang J, Sun Q, Morita Y, Jiang H, Gross A, Lechel A, et al. A differentiation checkpoint limits hematopoietic stem cell self-renewal in response to DNA damage. Cell. 2012;148:1001–14.
Hayflick L, Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res. 1961;25:585–621.
Campisi J, Kim SH, Lim CS, Rubio M. Cellular senescence, cancer and aging: the telomere connection. Exp Gerontol. 2001;36:1619–37.
Lessard J, Sauvageau G. Bmi-1 determines the proliferative capacity of normal and leukaemic stem cells. Nature. 2003;423:255–60.
Danet GH, Pan Y, Luongo JL, Bonnet DA, Simon MC. Expansion of human SCID-repopulating cells under hypoxic conditions. J Clin Invest. 2003;112:126–35.
Miyamoto K, Araki KY, Naka K, Arai F, Takubo K, Yamazaki S, et al. Foxo3a is essential for maintenance of the hematopoietic stem cell pool. Cell Stem Cell. 2007;1:101–12.
Park IK, Qian D, Kiel M, Becker MW, Pihalja M, Weissman IL, et al. Bmi-1 is required for maintenance of adult self-renewing haematopoietic stem cells. Nature. 2003;423:302–5.
Ito K, Takubo K, Arai F, Satoh H, Matsuoka S, Ohmura M, et al. Regulation of reactive oxygen species by Atm is essential for proper response to DNA double-strand breaks in lymphocytes. J Immunol. 2007;178:103–10.
Greenberger JS. Toxic effects on the hematopoietic microenvironment. Exp Hematol. 1991;19:1101–9.
Hendry JH. The cellular basis of long-term marrow injury after irradiation. Radiother Oncol: J Eur Soc Ther Radiol Oncol. 1985;3:331–8.
Bierkens JG, Hendry JH, Testa NG. The radiation response and recovery of bone marrow stroma with particular reference to long-term bone marrow cultures. Eur J Haematol. 1989;43:95–107.
Wang Y, Liu L, Pazhanisamy SK, Li H, Meng A, Zhou D. Total body irradiation causes residual bone marrow injury by induction of persistent oxidative stress in murine hematopoietic stem cells. Free Radic Biol Med. 2010;48:348–56.
Zhang H, Zhai Z, Wang Y, Zhang J, Wu H, Wang Y, et al. Resveratrol ameliorates ionizing irradiation-induced long-term hematopoietic stem cell injury in mice. Free Radic Biol Med. 2013;54:40–50.
Boccia R. Improved tolerability of amifostine with rapid infusion and optimal patient preparation. Semin Oncol. 2002;29:9–13.
Townsend LW. Implications of the space radiation environment for human exploration in deep space. Radiat Prot Dosim. 2005;115:44–50.
Durante M, Cucinotta FA. Heavy ion carcinogenesis and human space exploration. Nat Rev Cancer. 2008;8:465–72.
Georgakilas AG, O’Neill P, Stewart RD. Induction and repair of clustered DNA lesions: what do we know so far? Radiat Res. 2013;180:100–9.
Hada M, Georgakilas AG. Formation of clustered DNA damage after high-LET irradiation: a review. J Radiat Res. 2008;49:203–10.
Chang PY, Doppalapudi R, Bakke J, Wang A, Menda S, Davis Z. Biological impact of low dose-rate simulated solar particle event radiation in vivo. Radiat Environ Biophys. 2010;49:379–88.
Chang J, Feng W, Wang Y, Luo Y, Allen AR, Koturbash I, et al. Whole-body proton irradiation causes long-term damage to hematopoietic stem cells in mice. Radiat Res. 2015;183:240–8.
•• Rodman C, Almeida-Porada G, George SK, Moon J, Soker S, Pardee T, et al. In vitro and in vivo assessment of direct effects of simulated solar and galactic cosmic radiation on human hematopoietic stem/progenitor cells. Leukemia. 2017;31:1398–407. This research paper provide the first ever evidence of human leukemia formation in mouse model after 56 Fe ions irradiated human marrow transplanted in mice
Monzen S, Yoshino H, Kasai-Eguchi K, Kashiwakura I. Characteristics of myeloid differentiation and maturation pathway derived from human hematopoietic stem cells exposed to different linear energy transfer radiation types. PLoS One. 2013;8:e59385.
Chang J, Luo Y, Wang Y, Pathak R, Sridharan V, Jones T, et al. Low doses of oxygen ion irradiation cause acute damage to hematopoietic cells in mice. PLoS One. 2016;11:e0158097.
Koturbash I, Pogribny I, Kovalchuk O. Stable loss of global DNA methylation in the radiation-target tissue—a possible mechanism contributing to radiation carcinogenesis? Biochem Biophys Res Commun. 2005;337:526–33.
Loree J, Koturbash I, Kutanzi K, Baker M, Pogribny I, Kovalchuk O. Radiation-induced molecular changes in rat mammary tissue: possible implications for radiation-induced carcinogenesis. Int J Radiat Biol. 2006;82:805–15.
•• Rithidech KN, Honikel LM, Reungpathanaphong P, Tungjai M, Jangiam W, Whorton EB. Late-occurring chromosome aberrations and global DNA methylation in hematopoietic stem/progenitor cells of CBA/CaJ mice exposed to silicon ((28)Si) ions. Mutat Res. 2015;781:22–31. This research paper showed the first time a link between reduction in 5-hmC and genomic instability in myeloid colonies of HSPC 6 months post 28 Si ions irradiation
Tungjai M, Whorton EB, Rithidech KN. Persistence of apoptosis and inflammatory responses in the heart and bone marrow of mice following whole-body exposure to (2)(8)Silicon ((2)(8)Si) ions. Radiat Environ Biophys. 2013;52:339–50.
Rithidech KN, Tungjai M, Jangiam W, Honikel L, Gordon C, Lai X, et al. Proteomic profiling of hematopoietic stem/progenitor cells after a whole body exposure of CBA/CaJ mice to titanium (48Ti) ions. Proteomes. 2015;3:132–59.
Particle HZE. Neutron dosages from cosmic rays on the lunar surface. J Phys Soc Jpn. 2009;78:149–52.
• Miousse IR, Shao L, Chang J, Feng W, Wang Y, Allen AR, et al. Exposure to low-dose (56)Fe-ion radiation induces long-term epigenetic alterations in mouse bone marrow hematopoietic progenitor and stem cells. Radiat Res. 2014;182:92–101. This research paper showed that high-LET 56 Fe ion radiation cause long-term epigenetic alteration and radiation induced genomic instability could lead to hematopoietic malignancies
Rithidech KN, Honikel L, Whorton EB. mFISH analysis of chromosomal damage in bone marrow cells collected from CBA/CaJ mice following whole body exposure to heavy ions (56Fe ions). Radiat Environ Biophys. 2007;46:137–45.
Kennedy AR, Davis JG, Carlton W, Ware JH. Effects of dietary antioxidant supplementation on the development of malignant lymphoma and other neoplastic lesions in mice exposed to proton or iron-ion radiation. Radiat Res. 2008;169:615–25.
Cucinotta FA, Durante M. Cancer risk from exposure to galactic cosmic rays: implications for space exploration by human beings. The Lancet Oncology. 2006;7(5):431.
Townsend LW. Overview of active methods for shielding spacecraft from energetic space radiation. Phys Med: PM :Int J Devoted Appl Phys Med Biol: Off J Italian Assoc Biomed Phys. 2001;17(Suppl 1):84–5.
Loria R, Beckman M, Contaifer D, Tamariz F, Gibb D, Thompson L, et al. Beta androstenediol mitigates the damage of 1 GeV/n Fe ion particle radiation to the hematopoietic system. Cancer Biother Radiopharm. 2011;26:453–9.
Acknowledgments
We thank Thomas F. Peterson for his generosity. SMW is funded by NASA NNJ13ZSA001N.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rutulkumar Patel and Scott M. Welford declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Radiation Biology and Stem Cells
Rights and permissions
About this article
Cite this article
Patel, R., Welford, S.M. How Will the Hematopoietic System Deal with Space Radiation on the Way to Mars?. Curr Stem Cell Rep 3, 312–319 (2017). https://doi.org/10.1007/s40778-017-0104-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40778-017-0104-6