Abstract
It is well-established that humans have a bias towards immediate, compared to delayed, rewards. Although this bias has been primarily studied using monetary or other consumable commodities, it has also been demonstrated with outcomes of caregiver-mediated behavioral interventions targeting challenging behavior, which is a prevalent concern among children with autism spectrum disorder. In particular, caregivers may discount improvements in their child’s challenging behavior following behavioral interventions when the onset of improvement is delayed (Call et al. Journal of Autism & Developmental Disorders, 45, 1013–1025, 2015). The present study includes a sample of college students reading hypothetical vignettes about children with challenging behavior to evaluate the impact of child characteristics and caregiver role (parent vs. teacher) on discounting and the relationship between discounting of treatment and monetary commodities. Results suggest a discounting pattern across all groups, with no significant differences in discounting based on characteristics of the child/caregiver and steeper discounting for monetary compared to treatment outcomes. The results have implications for future research on caregiver-mediated interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Challenging behaviors are common referral concerns for individuals with autism spectrum disorder (ASD; Mazurek, Kanne, & Wodka, 2013) and are one of the most significant stressors for individuals charged with the care of these individuals (Lecavalier, Leone, & Wiltz, 2006). These behaviors often interfere with academic progress and can be difficult to manage in a classroom setting. Fortunately, there are several examples in the literature of successful treatments for these challenging behaviors using function-based behavioral treatments (Hurl, Whitman, Haynes, & Virues-Ortega, 2016). These treatments typically include components such as extinction and reinforcement (Brosnan & Healy, 2011), which may not have an immediate effect on behavior. Instead, these treatments may require consistent implementation over time before the child’s behavior improves. For some treatment components (e.g., extinction) problem behavior may even initially worsen before an improvement is observed (Lerman & Iwata, 1995).
Using extinction as an example, when implementing treatment, caregivers must make a choice each time the child engages in problem behavior. For instance, a caregiver may calm a child engaging in problem behavior maintained by escape from demands by removing the demand. However, this choice is also likely to reinforce the child’s problem behavior, making it more likely to occur during demands in the future. The other choice is to implement extinction by following through with the demand despite problem behavior. Although doing so is likely to result in continuation, and potentially temporary worsening, of problem behavior, problem behavior is less likely to occur in the future when similar demands are presented.
Despite the better long-term outcome associated with implementing behavioral interventions, it is easy to see how such a choice may be difficult for caregivers with multiple demands for their time and energy. It is perhaps unsurprising that many may choose not to adhere to treatment procedures to produce a short-term reduction in problem behavior (Allen & Warzak, 2000). This choice may be related to a systematic bias consistently displayed by humans towards more immediate gains and against delayed outcomes. This bias is referred to within the literature as “delay discounting” (Rachlin, Raineri, & Cross, 1991) and has been studied systematically within experimental arrangements. In the most commonly used approach, individuals choose between hypothetical monetary rewards that are either available immediately or after a delay, demonstrating that monetary rewards are devalued when delivery is delayed. A bias against delayed rewards has also been found with a variety of other commodities, including drugs, food, and health outcomes (Estle, Green, Myerson, & Holt, 2007; Odum et al., 2002; Odum & Baumann, 2007; Odum & Rainaud, 2003; Yi, Mitchell, & Bickel, 2010).
Building upon this work, Call, Reavis, McCracken, Gillespie, & Scheithauer (2015) conducted a study with parents of children with ASD or other developmental disabilities who were undergoing behavioral treatment for problem behavior. The experimenters presented these participants with choices similar to those in a study by Odum et al. (2002) about health outcomes, with the exception that the treatment consisted of interventions targeting a child’s problem behavior. That is, participants chose between a treatment that would produce an immediate cessation of their child’s problem behavior for a period of time that varied across trials (ranging from .01 to 10 years) or one that produced 10 years without problem behavior following a specific delay (ranging from 1 week to 10 years). For example, one trial consisted of a choice between a treatment that would work immediately and eliminate problem behavior for 6 months versus a treatment that would eliminate problem behavior for 10 years, after a 6-month delay. The majority of participants exhibited a pattern of discounting for treatment outcomes that adhered to the models that have been found to explain delay discounting of other commodities. In addition, the degree to which participants discounted treatment effects did not differ significantly from how they discounted monetary rewards.
The study by Call et al. (2015) was a first step in studying caregiver discounting of delayed outcomes from treatments for their child’s problem behavior. However, there are several potential extensions. First, the study exclusively sampled parents, so it is unclear whether a similar discounting pattern may be found among educators.
In addition, comparisons between discounting of monetary and treatment outcomes are difficult to interpret due to the small sample sizes in prior studies (n = 17; Call et al., 2015). Prior research has often identified that discounting of monetary rewards may be predictive of how an individual discounts other commodities, suggesting that sensitivity to delays is a trait variable (i.e., Charlton & Fantino, 2008; Johnson et al., 2010). However, there are a few examples in the literature of studies that found no correlation between the way that an individual discounts money and other commodities (e.g., health outcomes and money; Chapman, 1996), suggesting that sensitivity to delays may be a state variable. It might be helpful to know whether monetary discounting is related to discounting of treatment outcomes within each individual because monetary discounting could then be used as a proxy to help predict the likelihood that an individual would discount treatment outcomes. A larger sample size is needed to fully compare these two variables.
The small sample size from the study by Call et al. (2015) also prevents analysis of other variables that may influence the extent to which caregivers discount delayed treatment outcomes, such as the severity of the child’s problem behavior that is being treated or the context in which problem behavior occurs. Finally, because that study focused on extending the findings from a past study, which evaluated health outcomes (Odum et al., 2002), to caregivers of children with ASD receiving treatment for problem behavior, it replicated most of the methods from that prior study, including depicting treatment outcomes in terms of intervals of differing durations without symptoms or problem behavior. Although this may be a reasonable manner of quantifying the magnitude of a treatment outcome for a medical treatment, results from caregiver-mediated behavioral treatments may not include immediate and complete elimination of problem behavior.
The purpose of the current study is to add to the literature on discounting of treatment outcomes for problem behavior based on delays using a translational model with college students. In particular, the use of college students as participants allowed for a larger sample size to evaluate the intrasubject relationship between the way an individual discounts money and treatment outcomes. We also aimed to analyze between subject variables to determine the impact of the caregiver role and the severity of the child’s problem behavior on treatment outcome discounting. Finally, the manner of depicting outcomes of treatments as the percentage of improvement more closely resembles the way treatments for problem behavior differ from other discounted commodities, which allowed for a more clinically relevant extension of Call et al. (2015).
Method
Participants
In total, 148 undergraduate students at a southeastern university served as participants. Undergraduate students enrolled in courses in educational psychology selected the opportunity to participate from a list of available research studies to receive course credit. An alternative option to participating in research was made available by course instructors.
Participants completed two discounting assessments (monetary and treatment outcomes). Some participants were excluded due to either missing data or inconsistent patterns of responding following the criteria described by Johnson and Bickel (2008; see below for details). Thus, 81 participants completed the study with valid data-sets for both commodities.
The mean age of these 81 participants was 19.52 years (range 18–28 years) and the majority were female (81.48%). Reported races included Caucasian (75.31%), Asian (8.64%), African American (6.17%), Hispanic/Latinx (6.17%), Middle Eastern (1.23%), biracial (1.23%), and 1.23% did not report their race. About a third of participants (29.63%) reported experience with behavioral treatments, with education the most commonly reported major.
Procedures
The survey was housed in the online survey domain Qualtrics®. A paper copy of the survey was available upon request; no participants contacted the researchers to obtain a paper copy. Participants read an online consent statement prior to accessing the survey. At the end of the survey, participants received a link to provide their name in order to be granted course credit such that names were not directly linked to survey responses. An administrator assigned one research credit to those who provided their name at the completion of the study. Each participant completed a demographic questionnaire, including questions pertaining to their experience with behavioral interventions. Participants next completed a monetary discounting assessment, followed by a delay discounting assessment using vignettes of children who engaged in problem behavior, described below.
For the delay discounting monetary assessment, the survey presented instructions that read:
The following questions will ask you to make some choices about money. You will not get the money that you choose, but I want you to make your choices as though you were really going to get the money. The option on your left shows money that you can have today. The option on your right shows money that you can get after you have waited for some period of time. For example, first you will be asked to choose between $1,000 delivered today versus $1,000 that you would get 1 week from today. For each option select the one you would rather have.
The survey then presented the first choice between a monetary reward available immediately or after a delay. The participant made a selection by clicking a radio button next to the option on the screen. See Fig. 1 for examples of choices in the monetary assessment.
The left column (column A) decreased in the following progression $1,000, $990, $960, $920, $850, $800, $750, $700, $650, $600, $550, $500, $450, $400, $350, $300, $250, $200, $150, $100, $80, $60, $40, $20, $10, $5, and $1. Column A progressed in the same manner for each of the seven delays. The right column (column B) started at a 1-week delay. After all presentations of the monetary values in column A were presented, the delay increased. Delays included: 1 week, 2 weeks, 1 month, 6 months, 1 year, 3 years, and 10 years. These monetary amounts and delays are identical to those used in prior studies on delay discounting (e.g., Bickel, Odum, & Madden, 1999; Rachlin et al., 1991).
Following the monetary assessment, the participant started the treatment discounting assessment. At the commencement of this assessment, the survey presented brief instructions followed by one of four potential vignettes (randomly selected for each participant). The instructions read:
Next, we are going to ask you to make some choices about treatments options for a child with problem behavior. For the purpose of this assessment, we would like you to imagine that you are a [parent or teacher, dependent on the vignette] responsible for implementing a behavioral intervention for the following child who is [your student or child, dependent on the vignette].
Vignettes differed in terms of the severity of the hypothetical child’s problem behavior (severe or mild) and the caregiver role to be assumed by the respondent (teacher or parent). These combinations created four separate vignettes (i.e., severe-parent, severe-teacher, mild-parent, and mild-teacher). Prior to the start of the study, three professionals with extensive experience working with children with ASD and problem behavior in both homes and schools reviewed and provided feedback on the vignettes. To generate a representation of mild and severe problem behavior, the panel was asked to consider the typical child referred and treated in a day-treatment (severe) and outpatient (mild) program targeting problem behavior. The vignettes were then modified until all professionals agreed that they accurately represented commonly presented clinical concerns for parents and teachers of children with ASD and accurately reflected severe or mild problem behavior, based on the specific vignette.
Each vignette included a description of the same hypothetical child: John, a 10-year-old male with ASD who engaged in problem behavior consisting of aggressive and disruptive behavior. Vignettes for the severe and mild problem behavior differed in (1) topographies of problem behavior; (2) frequency of problem behavior; and (3) social impact of problem behavior. At the end of the vignette, the survey explained that a behavior specialist was presenting two options for behavior plans to treat the problem behavior described in the vignette, and that the participant was to select one of these plans acting as if they were the caregiver described in the vignette.
An example of the vignette in the severe-teacher context is presented below.
John is a 10-year-old male diagnosed with autism spectrum disorder. In John’s class there are six students, you as the primary teacher, and two aides. John exhibits aggressive behavior (e.g., hitting, kicking, scratching, pushing, biting) and disruptive behavior (e.g., throwing tables and chairs, breaking toys, kicking holes in walls). He engages in these problematic behaviors approximately 15–20 times a day and it is causing significant disturbance to the classroom as a whole. His aggressive behavior has caused significant injuries to staff members and other students in the classroom including concussions, significant bruising, and lacerations from biting and scratching. Two student aides have quit after injuries acquired from John and students in the class avoid interacting with John. He has made little to no academic progress over the past 3 months due to the intensity of his problem behavior. In addition, it is difficult to implement educational programs for John’s classmate because his problematic behaviors require so much attention from the teacher. The behavioral specialist at the school has presented you with two behavior plans. One results in short-term improvement of John’s problem behavior and the other results in more long-term improvements in John’s problem behavior, but will not result in immediate improvements.
An example of the vignette in the mild-parent context is presented below.
You are the parent and primary caregiver of John, a 10-year-old male diagnosed with Autism Spectrum Disorder. John exhibits aggressive behavior (e.g., pushing, pulling) and disruptive behavior (e.g., throwing paper and pencils, hitting his desk). He engages in these problematic behaviors approximately 5–10 times a day and it is causing some disturbance in your family’s life. His aggressive and disruptive behaviors make it difficult for John to achieve some of his academic goals at school and decrease his engagement in family activities. In addition, it is difficult for John to make friends due to his problematic behavior. You have recently sought out services from a behavior specialist. The therapist has presented you with two behavior plans. One results in short-term improvement of John’s problem behavior and the other results in more long-term improvements in John’s problem behavior, but will not result in immediate improvements.
After the vignette, the survey presented choices between treatments in an identical manner to the monetary discounting assessment with the exception that percentage improvement produced by each treatment was substituted for monetary values, with the delayed value always set at 100% improvement in problem behavior. Immediate treatment outcomes varied across choice trials over the following values representing percentage improvement: 100%, 99%, 96%, 92%, 85%, 80%, 75%, 70%, 65%, 60%, 55%, 50%, 45%, 40%, 35%, 30%, 25%, 20%, 15%, 10%, 8%, 6%, 4%, 2%, 1%, 0.5%, and 0.1%. The seven outcome delays were identical to the monetary assessment. The vignette appeared at the top of the screen for the participant to reference. See Fig. 1 for examples of choices in the treatment assessment.
Data Analysis
At the completion of the study, we extracted participant responses from the online survey domain. Indifference points were calculated for each participant for monetary and treatment outcomes separately by taking the average of the last immediate outcome that was selected (column A in Fig. 1) and the first delayed outcome that was selected (column B in Fig. 1) at each of the seven delay values. Indifference points represent the proportion of the value of the delayed outcome that is retained after the given delay. For example, for the monetary assessment, an indifference point of $725 identified at 6 months indicates that $1,000 (the delayed reward) retains 72.5% of its reinforcing value when it is delayed by 6 months.
Several authors have provided criteria for determining whether a participant’s pattern of responding is indicative of delay discounting (Dixon, Marley, & Jacobs, 2003; Johnson & Bickel, 2008). When indifference points are plotted for each of the delays from the delay discounting assessment, the expected pattern of responses is a monotonic and decelerating curve, with results differing drastically from this pattern considered invalid. Therefore, based on criteria articulated by Johnson and Bickel (2008), we excluded participants with patterns of responding that departed significantly from this expected outcome for either the monetary and/or the treatment outcome discounting tasks.
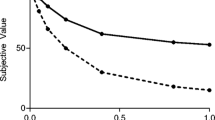
For participants remaining in the analysis, we evaluated the degree to which participants discounted delayed monetary rewards and treatment outcomes. The delay discounting literature typically measures the magnitude of discounting in two ways. First, researchers can calculate the area under the curve (AUC) generated by plotting indifference points at each delay as described above (Myerson, Green, & Warusawitharana, 2001). Using this methodology, a larger AUC is considered to indicate less discounting. Second, one can measure the magnitude of discounting using a mathematical model. Given the relative superiority of two-parameter, hyperboloid models of discounting (Myerson & Green, 1995), we fit a model using free k and s parameters [V = A/(1+kD)s]. Within this equation, V is the subjective (i.e., discounted) value of the reward, A equals the undiscounted value, k describes the discounting rate, D represents the delay, and s accounts for the nonlinear perception of time and magnitude of the outcome (Green & Myerson, 2004). Last, an R2 value was calculated to determine how well the participant’s data matched the expected values given the above equation. We evaluated median AUC, k, and R2 values across discounting assessments and between the four vignette groups.
First, we used a Kruskal-Wallis test to compare discounting of treatment (both AUC and k) and degree of fit to the discounting model (R2) across the different vignette groups to determine if there were significant differences. Next, we conducted a Wilcoxon signed-rank test to determine whether there were significant differences in the model fit and degree of discounting between the monetary and treatment discounting assessments. Last, we conducted Spearman correlations to determine if the degree to which participants discounted money was related to the degree of discounting for treatment outcomes.
Results
As described previously, 67 out of 148 participants were excluded due to inconsistent patterns of responding to one or both of the discounting assessments, leaving our sample of 81 participants. We excluded a similar number of participants for inconsistent responding in the monetary (n = 38) and treatment (n = 46) assessments. Several participants (n = 17) exhibited inconsistent responding for both assessments.
For the included participants, there were no significant differences between the vignette groups on the degree of discounting based on the AUC (p = 0.09) or k value (p =0.83 see Table 1). No significant differences were identified on any variables between groups for the monetary discounting assessment (p = 0.86 for AUC; p = 0.89 for k).
Given that we did not identify differences between groups, all data were considered together for the remaining analyses, comparing discounting of monetary rewards to discounting of treatment outcomes (see Table 2 and Fig. 2). We identified a significant difference in the degree of discounting between the two commodities, with participants discounting monetary rewards (Mdn AUC = 0.44, Mdn k = 0.09) more steeply than treatment outcomes (Mdn AUC = 0.65, Mdn k = 0.80; p < .01 for k and AUC). The median R2 value for the monetary discounting assessment was significantly higher (0.96) for the monetary assessment than for the treatment assessment (0.91; p = .003).
Last, we evaluated the association between the degree of discounting on the monetary and treatment assessments (k and AUC) using a Spearman correlation. We identified a weak relationship between discounting of monetary rewards and treatment outcomes across participants, rs = 0.28, 95% CI [0.07, 0.47], suggesting little association between the degree to which participants discounted the two commodities.
Discussion
Our results suggest that college students completing hypothetical vignettes from the perspective of a caregiver discount the value of outcomes for behavioral treatments for problem behavior exhibited by children with ASD in a predictable manner. This finding supports prior research (Call et al., 2015) and suggests that the outcome of treatments for problem behavior may follow the same principles as other commodities when outcomes are delayed. It also expands the results from Call et al. to situations where the participants were asked to act as teachers managing problem behavior in a school setting. This is an important finding, because it suggests that delay discounting assessments may be used as a tool for gauging how sensitive an individual is to delays in treatment effects, which can subsequently affect parent and teacher training.
We did not identify any systematic differences in discounting based on the different vignettes (i.e., severity of problem behavior or the role of the caregiver between a parent or teacher). However, given that these were hypothetical vignettes, we cannot be sure whether this result generalizes to actual caregivers of children with problem behavior. Future research should replicate this analysis with caregivers of children who actually vary on these dimensions.
It is interesting that participants discounted monetary rewards significantly more steeply than treatment outcomes. This result is counter to the majority of past research, which suggests that monetary rewards are generally discounted less steeply than other commodities (Odum, 2011), and differs from Call et al. (2015) who found no significant difference between treatment and monetary commodities. In addition, despite the finding that results from the treatment discounting assessment matched the discounting model fairly well (R2 = 0.91), it was a poorer fit than the results for the monetary assessment (R2 = 0.96).
There are a few potential explanations for this divergence from past research. First, selecting treatment outcome is partially a choice made for the participant (i.e., problem behavior they are managing) but is also a choice that affects others (e.g., the child, other caregivers, peers, siblings). Thus, the impact of choices regarding the treatment outcome would primarily affect the hypothetical child in the vignette, and the impact on the caregiver may be secondary. In addition, the treatment discounting task differed in that while waiting for treatment to work, the caregiver would be required to do something active, that is, implementing the treatment. In the monetary task, the participant would likely passively wait until the delayed reward becomes available. Because of this, it might be more appropriate to use a monetary discounting task that controls for these variables, by having somebody actively work during the wait period and/or have the money provided to somebody other than the participant. Another potential explanation relates to the consumable nature of most previously studied commodities. Money is considered a generalized reinforcer because it can be used to purchase many other types of reinforcers. In most past research that compared money to other commodities, those other commodities could be purchased by money. However, money cannot immediately purchase desirable treatment outcomes for problem behavior. Last, in most past research the participants commonly experienced the commodities studied in everyday life. In this study, it is likely that the participants had limited exposure to the reward of an improvement in problem behavior. In other words, participants might not have the same history of exposure to differing magnitudes of treatment outcomes (e.g., 40% compared to a 50% improvement in problem behavior) as they do to differing magnitudes of monetary outcomes or other more familiar commodities (e.g., $400 compared to $500). This differing history between the commodities may have affected responding. Additional research should be conducted analyzing commodities that affect others and cannot be purchased by a generalized reinforcer to better understand this relationship.
As previously mentioned, there is mixed research on whether discounting is a trait or state variable (Chapman, 1996; Charlton & Fantino, 2008; Johnson et al., 2010). These results suggest that there is only a weak relationship between the degree to which the same participant discounted money compared to treatment outcomes. Additional research is necessary to more definitively identify whether the degree of discounting of treatment outcomes is related to discounting of other more commonly studied commodities.
Future research should continue to focus on discounting of treatment outcomes, because this line of inquiry may have significant clinical utility. Maintenance of outcomes from behavioral interventions for problem behavior often requires continued implementation by agents-of-change other than the primary behavioral clinician. After a behavioral therapist develops an intervention, they generally train the child’s caregivers (e.g., parents and teachers) to implement the treatment. Unfortunately, these interventions may not result in immediate improvement, and instead the caregiver might have to implement the procedure consistently for some time before they observe changes in the child’s behavior. Additional research may find that a pattern of discounting of delayed treatment outcomes could be predictive of poor treatment fidelity by caregivers. If this is the case, sensitivity to delays, as measured by this or another delay-discounting paradigm, could be used as a clinical screener to identify caregivers that are at high-risk of integrity errors, and guide clinicians to incorporate preventative measures. For example, high-risk caregivers may require additional psychoeducation, in-home support, and follow-up to encourage maintenance.
This study has a few limitations that are worth consideration. First, compared to past research, which has usually excluded less than 20% of the sample (e.g., 18.87% in Cox & Dallery, 2016; 8.07% in Johnson & Bickel, 2008), we excluded a larger percentage of our sample using the Johnson and Bickel criteria. However, because similar numbers of participants were excluded from the monetary and treatment assessments, it is unlikely that this result is specific to the novel outcome of treatment effects evaluated in this study (i.e., percentage improvement in a child’s problem behavior). The increased percentage of excluded participants could potentially be attributed to a combination of factors. First, our sample of college students may have participated primarily to receive course credit and may not have been particularly invested in accurate responding. In addition, the assessment was completed entirely online and the lack of experimenter contact may have also decreased participants’ attention to or investment in the assessment. It is also possible that the computer system or instructions were not sufficiently clear and may have been misinterpreted (e.g., short-term vs. long-term improvements may not be clear to all participants) and the lack of experimenter contact prevented participants from asking questions, the answers to which may have promoted more consistent responding. Future research may consider replicating this study while addressing some of these factors.
Another limitation is the sample used in this study. We chose a sample of college students considering hypothetical vignettes about problem behavior to allow for a larger sample size to make comparisons across groups and between assessments. Given that our results are similar to those found with a smaller sample of actual caregivers of children with ASD (Call et al., 2015), it is possible that results would be similar with actual caregivers. However, additional research is necessary to know for certain how well these results generalize to actual clinical populations.
The wording of questions may also be a limitation in the study. For the treatment discounting task, we elected to use a percentage decrease in problem behavior because this is a common metric used to define treatment success in behavioral treatments for problem behavior and it appeared more representative of applied clinical work compared to the unit of measurement used in Call et al. (2015). However, it may have introduced new variability into the data as it is a more subjective measurement. In particular, we cannot be sure that different participants viewed a specific reduction in problem behavior in the same manner. For instance, one individual may have viewed a 30% improvement to mean a 30% decrease in frequency, whereas another could view this as a 30% decrease in the severity of each instance, and another might interpret it was a decrease in both behavioral dimensions. Future research may compare methods of quantifying reductions in problem behavior in treatment discounting tasks to determine the impact of this variable.
Finally, analyzing the data cumulatively across the different vignettes may have introduced variability in the data and be a potential limitation. We elected to do this because of the nonsignificant differences found between the vignettes and because aggregating the data allowed for a larger sample and more parsimonious analysis. However, it is possible that differences between groups would be observed with a larger sample size, and with this larger sample, analyzing the results between groups separately may be meaningful.
In sum, this study is an important step in determining the degree to which caregivers of children with ASD who engage in problem behavior might discount treatment outcomes. It sets the groundwork for future translational and applied research to continue focusing on exactly how caregivers discount these outcomes and how this may relate to clinically significant variables, such as treatment integrity.
References
Allen, K. D., & Warzak, W. J. (2000). The problem of parental nonadherence in clinical behavior analysis: Effective treatment is not enough. Journal of Applied Behavior Analysis, 33(3), 373–391. https://doi.org/10.1901/jaba.2000.33-373.
Bickel, W. K., Odum, A. L., & Madden, G. J. (1999). Impulsivity and cigarette smoking: Delay discounting in current, never, and ex-smokers. Psychopharmacology, 146, 447–454. https://doi.org/10.1007/PL00005490.
Brosnan, J., & Healy, O. (2011). A review of behavioral interventions for the treatment of aggression in individuals with developmental disabilities. Research in Developmental Disabilities, 32, 437–446. https://doi.org/10.1016/j.ridd.2010.12.023.
Call, N. A., Reavis, A. R., McCracken, C. E., Gillespie, S. E., & Scheithauer, M. C. (2015). The impact of delays on parents’ perceptions of treatments for problem behavior. Journal of Autism & Developmental Disorders, 45, 1013–1025. https://doi.org/10.1007/s10803-014-2257-9.
Chapman, G. B. (1996). Temporal discounting and utility for health and money. Journal of Experimental Psychology. Learning, Memory, & Cognition, 22, 771–791. https://doi.org/10.1037/0278-7393.22.3.77.
Charlton, S. R., & Fantino, E. (2008). Commodity specific rates of temporal discounting: Does metabolic function underlie differences in rates of discounting? Behavioral Processes, 77(3), 334–342. https://doi.org/10.1016/j.beproc.2007.08.002.
Cox, D. J., & Dallery, J. (2016). Effects of delay and probability combinations on discounting in humans. Behavioural processes, 131, 15–23. https://doi.org/10.1016/j.beproc.2016.08.002
Dixon, M. R., Marley, J., & Jacobs, E. A. (2003). Delay discounting by pathological gamblers. Journal of Applied Behavior Analysis, 36(4), 449–458. https://doi.org/10.1901/jaba.2003.36-449.
Estle, S. J., Green, L., Myerson, J., & Holt, D. D. (2007). Discounting of monetary and directly consumable rewards. Psychological Science, 18, 58–63. https://doi.org/10.1111/j.1467-9280.2007.01849.x.
Green, L., & Myerson, J. (2004). A discounting framework for choice with delayed and probabilistic rewards. Psychological Bulletin, 130, 769–792. https://doi.org/10.1037/0033-2909.130.5.769.
Hurl, K., Wightman, J., Haynes, S. N., & Virues-Ortega, J. (2016). Does a pre-intervention functional assessment increase intervention effectiveness? A meta-analysis of within-subject interrupted time-series studies. Clinical Psychology Review, 477, 1–84. https://doi.org/10.1016/j.cpr.2016.05.003.
Johnson, M. W., & Bickel, W. K. (2008). An algorithm for identifying nonsystematic delay-discounting data. Experimental Clinical Psychopharmacology, 16(3), 264–274. https://doi.org/10.1037/1064-1297.16.3.264.
Johnson, M. W., Bickel, W. K., Baker, F., Moore, B. A., Badger, G. J., & Budney, A. J. (2010). Delay discounting in current and former marijuana-dependent individuals. Experimental & Clinical Psychopharmacology, 18, 99–107. https://doi.org/10.1037/a0018333.
Lecavalier, L., Leone, S., & Wiltz, J. (2006). The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research, 50(3), 172–183. https://doi.org/10.1111/j.1365-2788.2005.00732.x.
Lerman, D. C., & Iwata, B. A. (1995). Prevalence of the extinction burst and its attenuation during treatment. Journal of Applied Behavior Analysis, 28(1), 93–94. https://doi.org/10.1901/jaba.1995.28-93.
Mazurek, M. O., Kanne, S. M., & Wodka, E. L. (2013). Physical aggression in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 7, 455–465. https://doi.org/10.1016/j.rasd.2012.11.004.
Myerson, J., & Green, L. (1995). Discounting of delayed rewards: Models of individual choice. Journal of the Experimental Analysis of Behavior, 64, 263–276. https://doi.org/10.1901/jeab.1995.64-263.
Myerson, J., Green, L., & Warusawitharana, M. (2001). Area under the curve as a measure of discounting. Journal of the Experimental Analysis of Behavior, 76(2), 235–243. https://doi.org/10.1901/jeab.2001.76-235.
Odum, A. L. (2011). Delay discounting: Trait variable? Behavioural Processes, 87, 1–9. https://doi.org/10.1016/j.beproc.2011.02.007.
Odum, A. L., & Baumann, A. A. L. (2007). Cigarette smokers show steeper discounting of both food and cigarettes than money. Drug & Alcohol Dependence, 91, 293–296. https://doi.org/10.1016/j.drugalcdep.2007.07.004.
Odum, A. L., Madden, G. J., & Bickel, W. K. (2002). Discounting of delayed health gains and losses by current, never-and ex-smokers of cigarettes. Nicotine & Tobacco Research, 4(3), 295-303. https://doi.org/10.1080/14622200210141257.
Odum, A. L., & Rainaud, C. P. (2003). Discounting of delayed hypothetical money, alcohol, and food. Behavioural Processes, 64, 305–313. https://doi.org/10.1016/S0376-6357(03)00145-1.
Rachlin, H., Raineri, A., & Cross, D. (1991). Subjective probability and delay. Journal of the Experimental Analysis of Behavior, 55, 233–244. https://doi.org/10.1901/jeab.1991.55-233.
Yi, R., Mitchell, S. H., & Bickel, W. K. (2010). Delay discounting and substance abuse-dependence. In G. J. Madden & W. K. Bickel (Eds.), Impulsivity: The behavioral and neurological science of discounting (pp. 191–211). Washington, DC: American Psychological Association.
Availability of Data and Materials
The datasets generated are available from the corresponding author on reasonable request.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of the authors’ affiliated institution and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This also adheres to the APA ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scheithauer, M.C., Call, N.A., Simmons, C.A. et al. Delay Discounting by College Undergraduates of Hypothetical Intervention Effects for Challenging Behavior. Psychol Rec 70, 65–73 (2020). https://doi.org/10.1007/s40732-019-00367-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40732-019-00367-0