Abstract
Purpose of Review
Clinicians struggle to recognize shock in pediatric trauma patients because traditional markers used in adults (tachycardia and hypotension) are late findings in children. Once present, hypotension is indicative of a child in extremis and interventions, such as blood transfusion and hemorrhage control operation, may be too late to provide benefit. In the current review, we describe additional tools that clinicians can use to identify injured children in the early stages of shock, offering the opportunity for early resuscitation, hemorrhage control operation, and lower mortality rates.
Recent Findings
Shock index, pediatric-age adjusted (SIPA) was developed to identify severely injured pediatric trauma patients. An elevated SIPA score is associated with a higher injury severity score, blood transfusion, and ICU admission. Unlike SIPA, the Compensatory Reserve Index (CRI) was developed in adults. CRI is a continuous, noninvasive, individual-specific measure of compensation that provides real-time insight into central volume loss and fluid resuscitation effectiveness. Current work is investigating the utility of CRI in the evaluation and management of pediatric trauma patients.
Summary
Children can compensate for acute blood loss with little change in traditional vital signs, so tachycardia and hypotension in a child may be quickly followed by sudden, unexpected hemodynamic decompensation. Several pediatric specific tools have been developed to help clinicians recognize children at the onset of circulatory compromise versus the onset of decompensation. These include an objective assessment of capillary refill, repeated SIPA calculations, and trending CRI values. Familiarity with these tools can facilitate the early identification of children at risk for decompensation. Incorporating them into everyday practice and decision-making rules can expedite decisions to transfuse blood or perform hemorrhage control procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma remains the leading cause of morbidity and mortality in children, and hemorrhagic shock is the leading cause of preventable death in pediatric trauma patients [1, 2]. Early recognition of injured children in the early stages of shock allows prompt interventions, such as blood transfusion or hemorrhage control procedures, which have been shown to improve patient outcomes, including mortality [2,3,4,5,6,7]. Most severely injured children are stabilized at adult trauma centers (ATCs) before transfer to a pediatric center. As a result, adult clinicians must be able to quickly identify injured children at risk for shock, so that blood transfusion and operative planning can be instituted before the child’s physiology becomes complex and difficult to control. Unfortunately, tools traditionally used to identify adult patients in shock have limited applicability when assessing injured children. Below we describe the limitations of adult-based tools and review several pediatric specific tools that can facilitate identification of injured children in all stages of shock.
Use of Vital Signs to Identify Children in Shock
Clinicians assess central volume status and end-organ perfusion in adults by monitoring traditional vital signs, with heart rate and blood pressure being key markers to identify adult patients in shock. This strategy is limited in children for a variety of reasons. First, normal vital signs vary with patient age. Providers who are unaccustomed to caring for pediatric patients may not know what constitutes a normal heart rate and blood pressure for a given child. Second, age-adjusted hypotension is a very late finding. It indicates a child in extremis and is an independent predictor of mortality in pediatric trauma patients [8••]. Compared to adults, children have a decreased ability to tolerate hypotension and shock [8••]. Third, injured children are able to maintain a relatively normal blood pressure until the point of hemodynamic collapse. This can be understood based on cardiac physiology. Compared to adults, infants and children have limited cardiac reserve, due to a relatively fixed stroke volume. An adult with a resting heart rate of 70 can double their cardiac output by doubling their heart rate. An infant or young child with a resting heart rate of 110 cannot augment their cardiac output in the same way. Children compensate by increasing systemic vascular resistance (SVR) to maintain a normal blood pressure; however, an increase in SVR adversely impacts cardiac output because the heart is now pumping against a higher pressure [9]. Although a child can maintain a normal blood pressure despite significant blood loss (up to 40% of total blood volume), at some point, the heart will no longer be able to efficiently pump against a rising SVR. When that happens, a child experiences hemodynamic collapse, which is marked by a sudden drop in blood pressure and oftentimes cardiac arrest [8••]. This short pre-collapse period in children, before the blood pressure begins to sag, makes early recognition of shock quite difficult. Fortunately, there are several new and emerging pediatric-specific tools to identify injured children at risk for shock.
Despite the limitations described above, age-adjusted hypotension remains an important triage tool to identify children in shock who require blood transfusion or hemorrhage control. Pediatric trauma surgeons have created additional pediatric-specific tools to help physicians identify children in shock. Much of this builds off the adult literature demonstrating the utility of elevated shock index (SI) alone to identify severely injured adult trauma patients. SI, defined as heart rate/systolic blood pressure, of > 0.9 has been used to accurately predict mortality and the need for massive transfusion (MT) in adult trauma patients [10]. Shock index lacks similar utility in children because normal vital signs vary with age. For this reason, shock index, pediatric age-adjusted (SIPA) was developed by dividing the maximum normal heart rate by the minimum normal systolic blood pressure for defined age groups (Table 1). The initial description demonstrated that for children between the ages of 4 and 16, an elevated SIPA was a better discriminator than both unadjusted SI and age-adjusted hypotension at identifying severely injured children who required blood product transfusion, had grade III liver/spleen laceration requiring blood product transfusion, and those who died [11•]. Values for sensitivity, specificity, positive predictive value and negative predictive value for SIPA, age-adjusted hypotension, and SI for outcomes of interest are displayed in Table 2 for comparison. These initial results were subsequently validated in both a multi-center prospective trial and a large national trauma database study, and have been expanded to include children ages 1–4 [12,13,14]. Specifically, SIPA has a higher specificity and positive predictive value than SI > 0.9 for outcomes of blood transfusion within 24 h, Injury Severity Score (ISS) ≥ 25, mortality, ICU admission, and ventilator use among injured children [13]. When looking only at severely injured children (those with ISS ≥ 15), the predictive accuracy of SIPA compared to SI was further improved [13]. The practical application of each of these measures (age-adjusted hypotension, unadjusted SI, and SIPA) is to assist with both trauma team activation and MT activation (discussed below). In terms of trauma team activation (defined by need for emergency operation, endotracheal intubation, and blood product transfusion), all three of these interventions were more likely in pediatric trauma patients with an elevated SIPA than they were in children with age-adjusted hypotension, demonstrating superiority of SIPA to age-adjusted hypotension for trauma team activation [15]. When looking specifically at children with blunt solid organ injury, in one single-center review, 90% of children who went on to require a blood transfusion had an elevated SIPA either prior to hospital arrival or in the emergency department [16]. These data demonstrate that elevated SIPA is quite sensitive at identifying severely injured children and should have suspicion on the part of the evaluating physician that the child is likely severely injured. A national analysis of pediatric trauma patients with blunt liver and/or spleen injury in the TQIP database validated these results, while also demonstrating that a persistently elevated SIPA is predictive of failure of non-operative management (OR 2.3, CI 1.5–3.4, p < 0.001) [17]. These findings support the utility of serial SIPA monitoring to assist in early identification of children with blunt solid organ injury, who may require blood product transfusion and those at risk of failing non-operative management [16, 17]. This highlights that an injured child in the trauma bay with an elevated SIPA is in shock and in need of rapid intervention in the form of blood transfusion or hemorrhage control.
In addition to blood pressure and SIPA, capillary refill time is another traditional measure that can be quite useful when evaluating an injured child. Although data among this specific population are limited, we can learn from the sepsis literature. In the setting of pediatric sepsis, shock is defined by a prolonged capillary refill time of > 2 s or age-adjusted hypotension. If one of these is present at the time of emergency department presentation, the overall mortality rate due to septic shock is 5–7%. If, however, the capillary refill time is prolonged and the patient is hypotensive, the mortality rate rises to 30% [5]. These findings support a brief assessment of capillary refill time during the primary survey and when present, should signal the clinician that the child is in shock and may need intervention such as blood transfusion or hemorrhage control.
Pediatric-Specific Tools to Identify Children in Shock
The data presented above regarding age-adjusted hypotension, SI, and SIPA are based on vital signs at the time of arrival to the emergency department. Vital signs provided by EMS providers at the scene as well as trends in these markers from the scene to emergency department (ED) arrival can also be used to identify severely injured children in shock who require blood transfusion or hemorrhage control.
Use of Pre-Hospital and ED SIPA Values
Nordin et al. expanded on this initial work by using the Pediatric Trauma Quality Improvement Program (TQIP) database to compare SI to pre-hospital and ED SIPA values in pediatric trauma patients ages 1–15 years old, who sustained blunt trauma. In this large study, 34.2% of patients had a persistently elevated SI from the scene to ED arrival, whereas SIPA was persistently elevated for 17.9%. An elevated SIPA at the scene was more predictive of higher ISS, longer hospital length of stay, and need for intubation than elevated SI. An elevated pre-hospital SIPA that remained elevated in the ED was predictive of increased ISS, longer hospital length of stay, ventilator requirement, and mortality [14]. These results support the notion that EMS providers can use pre-hospital SIPA values to triage trauma patients in the field. Pre-hospital SIPA may also be used—with other activation criteria—to inform trauma team activation level. This is stated with the understanding that an elevated pre-hospital SIPA alone leads to significant over triage. If, however, SIPA is elevated in the trauma bay then shock is present, fluid resuscitation should be ongoing and a massive transfusion protocol (MTP) may need to be activated.
Other groups have explored the utility of applying SIPA monitoring following hospitalization to predict the need for intensive care unit (ICU) admission [16, 17, 19]. In a retrospective, single-institution review of 133 traumatically injured children with blunt solid organ injuries (liver, spleen, or renal injuries), 95% of those requiring ICU-level care were found to have either an elevated SIPA or hematocrit < 30% on admission (sensitivity = 95%; negative predictive value = 99%) [16, 17, 19]. These authors recommend using these criteria to help determine which children require ICU level care following blunt solid organ injury.
SIPA Values for Specific Outcomes
SIPA was initially defined as a dichotomous variable, either normal or elevated, and calculated based on the extremes of the normal range. More recent work has investigated the relationship between absolute SIPA values and trauma outcomes. In a recent study, specific pre-hospital and ED SIPA cut-point values were determined to predict the need for massive transfusion and/or mortality in pediatric trauma patients for the following age groups: < 1 year, 1–6 years, 7–12 years, and > 12 years old [20]. Our group sought to determine the degree to which elevated SIPA values could predict outcomes of interest. We also evaluated whether pre-hospital or ED SIPA were better predictors of adverse outcomes and how these values varied with age. We found that for children ages 6–12, an elevated ED SIPA (> 1.76) predicted the need for massive transfusion. In children > 12 years of age, prehospital SIPA > 1.4 was the best predictor of need for massive transfusion. Pre-hospital (> 1.6) and ED SIPA (> 1.24) performed best in the > 12-year-old age group at predicting mortality with an accuracy of 91% and 90%, respectively. This further underscores the physiologic differences of children based on their age, and highlights that age remains an important consideration when evaluating the utility of SIPA to predict specific outcomes in pediatric trauma patients [20]. In terms of practical application, as with all other physiologic measures, the higher the elevation of SIPA (and thus the greater degree of cardiovascular abnormality), the more likely a child is to be in shock and the more likely to require intervention such as blood product transfusion of hemorrhage control.
Limitations of SIPA
While SIPA has been validated for children ages 1–18 years, it has not been validated in neonates and infants < 1 year old. Of all pediatric age groups, neonates and infants possess the most distinct and rapidly changing physiologic characteristics. Their extensive hemodynamic reserve and compensatory abilities pose a challenge for early detection of shock. For these reasons, many of the initial studies evaluating the utility of SIPA in pediatric trauma patients excluded neonates and infants < 1 year old. This is a current limitation of SIPA, and future studies evaluating the utility of this tool for the identification of shock in traumatically injured neonates and infants are needed. Additionally, our group found that when used as a trauma team activation criterion, elevated SIPA in isolation leads to significant over triage. The optimal use of SIPA as part of trauma team activation criteria is likely some combination of elevated SIPA with other physiologic parameters. However, this has not yet been established. The following sections described how various groups have attempted to optimize pediatric trauma team activation criteria. Due to the various uses of SIPA, there is concern regarding the practicality of its use. One simple solution is to post age cut-offs and associated normal SIPA values in the trauma bay so that the values do not need to be memorized by clinicians; this can be posted near where information regarding trauma activations, primary and secondary survey information is displayed. Additionally, a calculator is available on MDCalc for clinicians to utilize in real time.
Scoring Tools That Incorporate Neurologic Status in Shock Recognition
The influence of neurologic injury on trauma outcomes remains an area of active research. Although data in the pediatric population are limited, data from the adult trauma population offer insight. In adult trauma patients with multiple injuries, central nervous system (CNS) injury is the leading cause of death. The combination of CNS injury with hypotension is especially devastating, increasing mortality by two- to threefold [21, 22]. We speculate that that same holds true in children. Recently, our group and others have worked to understand how neurologic status can be incorporated into pediatric trauma triage tools. Adult trauma groups have introduced the concept of inverse or reverse shock index (rSI, which is systolic blood pressure/heart rate) and reported an rSI < 1 is associated with poor outcomes and may be useful to identify trauma patients at high risk of mortality, even in the absence of hypotension [23,24,25,26]. We applied this concept to pediatric cohorts by comparing a new scoring tool rSIG, defined as the reverse shock index (rSI) multiplied by the Glasgow Coma Scale (GCS), to SI, and SIPA in predicting the need for early trauma interventions in pediatric trauma patients utilizing the 2014–2018 TQIP database [27]. Patients with an abnormal rSIG, when compared to those with an abnormal SI or SIPA, were more likely to require blood product transfusion at 4 h, endotracheal intubation, ICP monitoring, and ICU admission. Regardless of age, rSIG more accurately predicted the need for early trauma interventions than SI or SIPA, demonstrating that rSIG may be a useful trauma triage tool at the time of presentation for pediatric patients [27]. Other proposed pediatric-specific scoring tools include a second revision to the Revised Trauma Score (RTS). Filipescu et al. found that the combination GCS, elevated SIPA, peripheral oxygen saturation, and a patient’s temperature better predicted mortality in injured adults and children [28]. Two other manuscripts reported that the combination of elevated SIPA and an abnormal GCS predicted both mortality and need for early blood product transfusion better than elevated SIPA alone [29, 30]. It is clear from the breadth of this work that the optimal pediatric trauma team activation criteria scoring tool has not yet been created. However, this recent work suggests that the combination of an elevated SIPA in a child with an abnormal GCS is an indication that the child is in shock and needs intervention, likely including blood transfusion or hemorrhage control. Ongoing work seeks to optimize these pediatric scoring tools.
The hypothesized reason scoring tools that incorporate neurologic status improve upon the use of tools that incorporate only hemodynamic related vital signs has to do with the effect of severe neurologic injury on a patient’s heart rate and blood pressure. Individuals with profound neurological injury may have normal vital signs due to Cushing’s reflex, resulting in subjective bradycardia and hypertension (which together lead to a lower SIPA) due to increased intracranial pressure. However, due to their neurological injury, their GCS will decrease, and calculation of any of these triage scores can allow for identification of patients in shock in need of intervention.
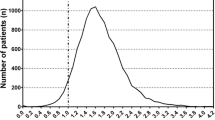
Compensatory Reserve Index
Traditional vital signs (HR, BP, RR, SpO2) are poor surrogates for the body’s compensatory mechanisms. Recent advances in computing power and machine learning algorithms have enabled the development of an algorithm that recognizes individual-specific changes in the photoplethysmogram (PPG) waveforms that represent physiologic mechanisms of hemodynamic compensation [31,32,33]. This technology, called the Compensatory Reserve Index (CRI), estimates an individual’s compensatory reserve in real time and is able to determine how near or far a patient is from hemodynamic decompensation. CRI values range from 1 to 0, and represent the proportion of physiologic reserve remaining, where “1” represents supine normovolemia and “0” is the predicted point of hemodynamic decompensation (Fig. 1). In adult patients, CRI has proven to be more sensitive than a variety of measures, including heart rate, systolic blood pressure, shock index, base deficit, hemoglobin, and hematocrit, in its ability to identify patients who donate as little as one unit of blood, or are actively bleeding [33, 34]. It has been shown to be equivalent to serum lactate in its ability to assess perfusion status related to hemorrhage; the difference being that CRI values are immediate, and lactate values require lab processing times to result [35•]. An increase in a patient’s CRI is associated with the clearance of lactate and mirrors fluid resuscitation effectiveness [35•]. Research on CRI in hemorrhaging children is limited, but CRI has been shown to reflect acute hemodynamic changes in children in several clinical settings, such as burns, sepsis secondary to perforated appendicitis, congenital heart disease, and the need for ECMO in infants with congenital diaphragmatic hernia [36,37,38,39]. It is a completely non-invasive tool with substantial opportunity to accurately identify patients in varying stages of compensated shock, who require volume resuscitation. Efforts are underway to prospectively study CRI in pediatric trauma patients.
Schematic of the compensatory reserve. The compensatory reserve (CR) is indicative of the individual-specific proportion of intravascular volume remaining before the onset of cardiovascular collapse. The sloped line shows a hypothetical decline in CR over time in the setting of volume loss. A CR of “1” represents supine normovolemia, whereas a CR of “0” represents the point at which hemodynamic decompensation develops
Use of Laboratory Values to Identify Children in Shock
Laboratory adjuncts can provide information for identifying children in shock. The two most commonly used measures are base deficit and lactate values. Base deficits have been shown to be important prognostic tools in adults, but extrapolation to children remains a challenge due their physiological differences. Base deficit greater than 8 mmol/L on arterial blood gas has been retrospectively validated to be associated with both need for blood transfusion and increased mortality risk in children [40, 41]. Prospective study of base deficit has shown that a base deficit greater than 5 mEq/L with concomitant admission lactates more than 2.94 mmol/L, to be independently associated with a 2.4 times increased odds of mortality [42]. Lactate has also been studied as a criterion for shock, specifically in the adult population [41]. Both are indications of acidosis and adequacy of resuscitation as lactic acid is produced when oxygen delivery to cells is inadequate. In general, lactate and base deficit are evaluated based are arterial blood samples which can be difficult to obtain in the trauma bay. Among pediatric trauma patients with sepsis, lactate levels have been shown to correlate with venous and arterial samples when the lactate is below 2 mmol/L. If the venous lactate is found to be > 2 mmol/L, the value should be confirmed with an arterial sample [43]. Among well perfused children, the pH of venous and capillary blood gas samples are found to correlate adequately [44]. This may not hold true if the child is in shock. If there is any question of the adequacy of perfusion, an arterial sample should be sent. Use of these laboratory values in tandem can serve to identify children in shock.
Identifying Children in Need of Massive Transfusion
Massive hemorrhage is the leading cause of death among pediatric trauma patients. The goal of an MTP is to restore circulatory volume, replenish hemostatic components, and improve oxygen transport by rapid transfusion of fixed ratios of blood components (fresh frozen plasma (FFP), packed red blood cells (pRBCs), platelets, and cryoprecipitate) [45]. The known benefits of MTPs include decreased variability between providers, ease of use, and improved compliance. Early activation of an MTP is known to improve patient outcomes, including mortality [46,47,48]. Given the positive impact on patient outcomes, most institutions utilize an MTP to facilitate massive transfusion in a bleeding child. The difficulty of developing an MTP for children lies in the accurate identification of children who have experienced significant blood loss and may continue to bleed, based on physiologic parameters, laboratory values, associated injuries, and identified sources of blood loss. At most children’s hospitals, MTP activation criteria are based on physician discretion, because no validated criteria are available for this population. [49, 50].The goal of MTP research is to define criteria that help physicians identify children at risk for or experiencing massive hemorrhage, to allow timely MTP activation. One significant limitation to this work and consensus on this topic is the fact that there is still no standard definition for MTP in the pediatric literature [51]. The number that is commonly used to define massive transfusion is a transfused volume of > 40 ml/kg of pRBC in the first 24 h after injury. Most MTP research looks retrospectively at pediatric trauma patients who received > 40 ml/kg of blood products in the first 24 h after injury to identify clinical criteria that could alert a physician to the need for MTP activation. This work focuses either on the modification of adult-based scoring tools or the development of pediatric-specific scoring tools.
In the adult trauma population, there are a variety of clinical scoring tools that have been developed using a combination of clinical and laboratory values to predict the need for MT. The multitude of scoring tools highlights the fact that no single scoring tool has been adopted or shown to be universally accurate [52,53,54]. Unfortunately, in the pediatric population, adult-based criteria lack the sensitivity and specificity present in the adult population as they often do not account for the physiologic differences and different injury patterns that characterize pediatric trauma [55]. Adult-based scoring tools are unable to predict which children will require MT and which will not [56]. Additionally, most pediatric scoring tools were developed to predict mortality, which does not necessarily signal the need for MT [57]. Fortunately, a few novel scoring tools have been developed and studied with this outcome in mind. Hwu et al. developed two models to predict need for massive transfusion in children, one based on clinical findings (“pre-arrival” model), and another that included laboratory values (ED model) [58]. The “pre-arrival” model gives one point for each of the following: arrival HR ≤ 65 or ≥ 125 bpm, first temperature < 36 °C, arrival GCS ≤ 12, presence of penetrating injury, and active bleeding. The presence of two parameters in the “pre-arrival” model had a sensitivity of 86.5% and specificity of 94.7% in identifying the need for MT in children. The ED model includes the presence of penetrating injury, ED GCS ≤ 13, ED hemoglobin < 11 g/dL, ED temperature < 36 °C, ED PTT > 32 s, and active bleeding, giving one point for each. The presence of two parameters has a specificity of 64.1% and sensitivity of 79.5% in identifying the need for MT in children [58]. The appeal of these two scores is the fact that they were created in pediatric trauma populations with pediatric criteria in mind; however, they have only been evaluated in a single population. Future work will need to validate these scores outside of the initial population from which they were derived.
Unlike Hwu and colleagues who created pediatric-specific scoring tools, our group has approached this problem by modifying adult-based criteria to identify children who require MTP. The ABC (assessment of blood consumption) score, which was developed for use in adults, assigns one point for each of the following: penetrating mechanism, positive focused abdominal sonography for trauma (FAST), SBP < 90, and HR > 120. A score of 2 or greater is used as an MTP activation criterion in adults and yields a sensitivity of 75% and a specificity of 86%. In children, however, the ABC score has only a 29% sensitivity [54]. Replacement of the HR and SBP cutoffs with SIPA (the ABC-S score), to account for age-related changes in physiologic vital signs, displayed only modest improvement in the score’s sensitivity [16]. Phillips et al. adjusted the ABC score by substituting adult vital thresholds for SIPA and added base deficit (< − 8.8) and lactate (> 3.5), to create the ABCD score. A score ≥ 1 was found to have a sensitivity of 97.9% for predicting need for MT [59]. We also developed the BIS score, defined as base deficit (< − 6.9), INR (> 1.4), and elevated SIPA, to account for low rates of penetrating trauma and positive FAST exams among pediatric patients. A BIS score of ≥ 2 was found to have the highest AUC (0.81) with a 98.0% sensitivity, 23.0% specificity, and 77.0% accuracy for predicting MT in children [60]. Most studies using SIPA have largely focused on the ability of SIPA to predict need for blood transfusion in blunt injured pediatric patients. However, as mentioned above, our group aimed to determine what SIPA value would predict the need for MT. Among children > 12 years, a SIPA of > 1.4 in the prehospital setting predicted the need for MT (AUC 0.86). Among children ages 7–12, a SIPA of > 1.16 in the ED predicted the need for MT (AUC 0.87) [20]. These findings further demonstrate the effects of age on physiology and underscore why adult-based criteria perform poorly among children.
One area for further study in the pediatric population is the incorporation of thromboelastography (TEG) into MTP activation criteria. In adults, TEG values have been shown to predict MT needs, with elevated activated clotting times predicting need for pRBC transfusion, maximum amplitude predicting need for platelet transfusion, and alpha angle being more predictive than INR at determining the need for fresh frozen plasma (FFP) transfusion. [50, 61]. TEG parameters, however, have not yet been incorporated into MTP activation criteria in the pediatric population. Thus, our ability to identify injured children who will require massive transfusion remains limited. Current research, which aims to optimize MTP activation criteria for pediatric patients, is still in its early stages. Future work is needed to determine which components of these different scoring systems are most important in identifying children with massive hemorrhage.
Knowledge Gaps and Future Directions
Despite substantial effort and research on shock recognition in pediatric patients, limitations remain. Development of universal definitions and scoring tools in children is complicated by their substantial physiologic variability, which are based on age and size. CRI is able to detect hemodynamic changes earlier than traditional vital signs in adult trauma patients but remains largely unstudied in the pediatric trauma population [33, 34]. The CRI algorithm was developed in adults, and it is unclear if the algorithm translates directly to pediatric patients. A recent study of over 200 pediatric patients, suggests that CRI varies significantly with age. The mean value in children is lower than 0.6, which is considered a lower normal limit for adults [62]. Therefore, a better understanding of normal CRI values in children, how CRI varies with age, and how CRI changes based on volume status in children are needed. Prospective studies to determine what constitutes lower limits of normal in this population are needed, because adult values may not be directly transferable to pediatric patients. This technology has the potential to identify children in shock, but further work to calibrate the algorithm to pediatric patients is needed to improve its accuracy.
Future work to establish scoring tools that are easy to incorporate into clinical practice and applicable to pediatric patients, regardless of age, is also needed. One area of particular need is our current lack of objective criteria to identify children who require trauma team and MTP activation. A variety of new scoring tools are described above; however, none has been validated outside of the population from which they were derived. Furthermore, each of these tools uses a different combination of variables to create a score (Table 3). Future work needs to better define MTP activation criteria in children and clarify how novel tools like SIPA and CRI can be incorporated into MTP and trauma team activation criteria. Recent work by our group aimed to determine if the degree of elevation of SIPA above a certain value can better predict severe injury or need for MT than the dichotomous variable of elevated SIPA that was initially described. These initial findings are interesting and offer a future avenue to optimize these tools [20]. Much of the work described above represents isolated ideas that need to come together in a coherent form to help optimize care of injured children.
Conclusions
Despite many substantial efforts to develop systems and tools to reliability and easily identify injured children in shock who require blood transfusion and hemorrhage control procedures, identifying such children remains a challenge. As described above, there are a variety of pediatric specific tools and scoring systems that can assist in this process, but ultimately, the optimal pediatric trauma team activation criteria and MTP activation criteria remain elusive. However, physicians who care for injured children can use the tools described above to identify children in shock and intervene quickly. SIPA has proven to be a useful tool to signal to the physician that a child is in shock and action should be taken to reverse shock. While we do not advocate for using elevated SIPA alone as a trauma team activation criterion, we do advocate for using SIPA in the trauma bay. For providers who do not calculate SIPA routinely or easily recall the age-based cutoffs, SIPA calculation on MDCalc can be done quickly. Additionally, emergency departments can include abnormal SIPA cutoffs on posters displayed in the trauma bay. If a child presents to the trauma bay following traumatic injury, we recommend calculating the SIPA as part of the primary survey. The presence of an elevated SIPA should heighten the evaluating physician’s suspicion that the child has suffered severe injury, lower the threshold for intervention including blood product transfusion or hemorrhage control, and once stabilized, consideration for transfer to a pediatric trauma center. In terms of MTP activation criteria in pediatric trauma, the optimal scoring tool remains elusive. For this reason, at most centers, surgeon discretion remains a top criterion. In terms of objective criteria, the use of the ABC score, with either adult-based vital sign cutoffs or elevated SIPA can be used to activate the MTP at an institution. More important than specific criteria and scores is that the trauma surgeon evaluating an injured child is able to recognize that normal vital signs vary with age, children are able to maintain normotension despite much larger relative blood loss, and hypotension in a child is a sign of impending hemodynamic collapse. Keeping these physiologic principles in mind when evaluating a child will help physicians recognize children in shock and intervene sooner to control hemorrhage and reverse the effects of shock.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Deaths: leading causes for 2019. National Vital Statistics Report.
Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006;60(6 Suppl):S3-11.
Carcillo J, Han K, Lin J, Orr R. Goal-directed management of pediatric shock in the emergency department. Clin Ped Emerg Med. 2007;8:165–75.
Smith LAA, Carcillo JA, Aneja R. Shock States. In: Zimmerman JJCR, Fuhrman BP, Rotta AT, Kudchadkar SR, Relvas M, Tobias JD, editors. Furhrman and Zimmerman’s Pediatric critical care. 6th ed. Philadelphia: Elsevier; 2022. p. 352- 362.e355.
Carcillo JA, Kuch BA, Han YY, et al. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009;124(2):500–8.
Han YY, Carcillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;112(4):793–9.
Kissoon N, Orr RA, Carcillo JA. Updated American College of Critical Care Medicine–pediatric advanced life support guidelines for management of pediatric and neonatal septic shock: relevance to the emergency care clinician. Pediatr Emerg Care. 2010;26(11):867–9.
•• Leeper CM, McKenna C, Gaines BA. Too little too late: hypotension and blood transfusion in the trauma bay are independent predictors of death in injured children. J Trauma Acute Care Surg. 2018;85(4):674–8. This paper highlights differences in pediatric trauma patients, specifically that hypotension and blood transfusion in the trauma bay in these patients indicate late findings in pediatric shock and are poor prognostic indicators.
Aneja RK, Carcillo JA. Differences between adult and pediatric septic shock. Minerva Anestesiol. 2011;77(10):986–92.
Bruijns SR, Guly HR, Bouamra O, et al. The value of traditional vital signs, shock index, and age-based markers in predicting trauma mortality. J Trauma Acute Care Surg. 2013;74:1432–7.
• Acker SN, Ross JT, Partrick DA, et al. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg. 2015;50:331–4. This data indicates that age-adjusted shock index is more accurate at identifying children who are severely injured, have intraabdominal injury requiring transfusion, and at higher risk of death than shock index unadjusted for age.
Linnaus ME, Notrica DM, Langlais CS, et al. Prospective validation of the shock index pediatric-adjusted (SIPA) in blunt liver and spleen trauma: an ATOMAC+ study. J Pediatr Surg. 2017;52(2):340–4.
Nordin A, Coleman A, Shi J, et al. Validation of the age-adjusted shock index using pediatric trauma quality improvement program data. J Pediatr Surg. 2018;53(1):130–5.
Nordin A, Shi J, Wheeler K, et al. Age-adjusted shock index: from injury to arrival. J Pediatr Surg. 2019;54:984–8.
Acker SN, Bredbeck B, Partrick DA, Kulungowski AM, Barnett CC, Bensard D. Shock index, pediatric age-adjusted (SIPA) is more accurate than age-adjusted hypotension for trauma team activation. Surgery. 2016;161(3):803–7.
Phillips R, Acker S, Shahi N, et al. The shock index, pediatric age-adjusted (SIPA) enhanced: prehospital and emergency department SIPA values forecast transfusion needs for blunt solid organ injured children. Surgery. 2020;168:690–4.
Phillips R, Meier M, Shahi N, et al. Elevated pediatric age-adjusted shock-index (SIPA) in blunt solid organ injuries. J Pediatr Surg. 2021;56:401–4.
American Heart Association. “Pediatric advanced life support.” https://eccguidelines.heart.org/index.php/circulation/cpr-ecc-guidelines-2/part-12-pediatric-advanced-life-support/. Accessed 6 July 2022.
Vandewalle RJ, Peceny JK, Dolejs SC, et al. Trends in pediatric adjusted shock index predict morbidity and mortality in children with severe blunt injuries. J Pediatr Surg. 2018;53(2):362–6.
Stevens J, Reppucci ML, Meier M, Phillips R, Shahi N, Shirek G, et al. Pre-hospital and emergency department shock index pediatric age-adjusted (SIPA) “cut points” to identify pediatric trauma patients at risk for massive transfusion and/or mortality. J Pediatr Surg. 2022;57(2):302–7. https://doi.org/10.1016/j.jpedsurg.2021.09.053.
Manley G, Knudson MM, Morabito D, Damron S, Erickson V, Pitts L. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch Surg. 2001;136(10):1118–23.
Chesnut RM, Marshall SB, Piek J, Blunt BA, Klauber MR, Marshall LF. Early and late systemic hypotension as a frequent and fundamental source of cerebral ischemia following severe brain injury in the Traumatic Coma Data Bank. Acta Neurochir Suppl (Wien). 1993;59:121–5.
Chuang JF, et al. Use of the reverse shock index for identifying high-risk patients in a five-level triage system. Scand J Trauma Resusc Emerg Med. 2016;24:12.
Kuo SCH, et al. The use of the reverse shock index to identify high-risk trauma patients in addition to the criteria for trauma team activation: a cross-sectional study based on a trauma registry system. BMJ Open. 2016;6:e011072.
Lai WH, et al. Using the reverse shock index at the injury scene and in the emergency department to identify high-risk patients: a cross-sectional retrospective study. Int J Environ Res Public Health. 2016;13:357.
Lai WH, et al. Systolic blood pressure lower than heart rate upon arrival at and departure from the emergency department indicates a poor outcome for adult trauma patients. Int J Environ Res Public Health. 2016;13:528.
Reppucci ML, Acker SN, Cooper E, Meier M, Stevens J, Phillips R, Moulton S, Bensard D. Improved identification of severely injured pediatric trauma patients using reverse shock index multiplied by Glasgow Coma Scale (rSIG). J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000003432.
Filipescu R, Powers C, Yu H, Yu J, Rothstein DH, Harmon CM, Clemency B, Guo WA, Bass KD. Improving the performance of the Revised Trauma Score using Shock Index, Peripheral Oxygen Saturation, and Temperature-a National Trauma Database study 2011 to 2015. Surgery. 2020;167(5):821–8. https://doi.org/10.1016/j.surg.2019.12.003.
Reppucci ML, Phillips R, Meier M, Acker SN, Stevens J, Moulton SL, Bensard D. Pediatric age-adjusted shock index as a tool for predicting outcomes in children with or without traumatic brain injury. J Trauma Acute Care Surg. 2021;91(5):856–60. https://doi.org/10.1097/TA.0000000000003208.
Raythatha JH, Aulakh H, Yang S, Mok C, Soundappan SV. Predicting morbidity and mortality in Australian paediatric trauma with the Paediatric Age-Adjusted Shock Index and Glasgow Coma Scale. Injury. 2022;53(4):1438–42. https://doi.org/10.1016/j.injury.2022.01.034.
Convertino VA, Moulton SL, Grudic GZ, Rickards CA, Hinojosa-Laborde C, Gerhardt RT, Blackbourne LH, Ryan KL. Use of advanced machine-learning techniques for noninvasive monitoring of hemorrhage. J Trauma. 2011;71(1 Suppl):S25-32. https://doi.org/10.1097/TA.0b013e3182211601.
Moulton SL, Mulligan J, Grudic GZ, Convertino VA. Running on empty? The compensatory reserve index. J Trauma Acute Care Surg. 2013;75(6):1053–9. https://doi.org/10.1097/TA.0b013e3182aa811a.
Stewart CL, Mulligan J, Grudic GZ, Talley ME, Jurkovich GJ, Moulton SL. The Compensatory Reserve Index Following Injury: results of a prospective clinical trial. Shock. 2016;46(3 Suppl 1):61–7. https://doi.org/10.1097/SHK.0000000000000647.
Nadler R, Convertino VA, Gendler S, Lending G, Lipsky AM, Cardin S, Lowenthal A, Glassberg E. The value of noninvasive measurement of the compensatory reserve index in monitoring and triage of patients experiencing minimal blood loss. Shock. 2014;42(2):93–8. https://doi.org/10.1097/SHK.0000000000000178.
• Johnson MC, Alarhayem A, Convertino V, Carter R 3rd, Chung K, Stewart R, Myers J, Dent D, Liao L, Cestero R, Nicholson S, Muir M, Schwaca M, Wampler D, DeRosa M, Eastridge BJ. Comparison of compensatory reserve and arterial lactate as markers of shock and resuscitation. J Trauma Acute Care Surg. 2017;83(4):603–8. https://doi.org/10.1097/TA.0000000000001595. This is a prospective observational study that highlights the comparative ability of the compensatory reserve index to lacate in identifying initial perfusion status among hemorrhaging patients.
Choi YM, Leopold D, Campbell K, Mulligan J, Grudic GZ, Moulton SL. Noninvasive monitoring of physiologic compromise in acute appendicitis: new insight into an old disease. J Pediatr Surg. 2018;53(2):241–6. https://doi.org/10.1016/j.jpedsurg.2017.11.013.
Ehrmann DE, Leopold DK, Phillips R, Shahi N, Campbell K, Ross M, Zablah JE, Moulton SL, Morgan G, Kim JS. The Compensatory Reserve Index responds to acute hemodynamic changes in patients with congenital heart disease: a proof of concept study. Pediatr Cardiol. 2020;41(6):1190–8. https://doi.org/10.1007/s00246-020-02374-3.
Leopold DK, Phillips RC, Shahi N, Gien J, Marwan AI, Kinsella JP, Mulligan J, Liechty KW, Moulton SL. Low postnatal CRI values are associated with the need for ECMO in newborns with CDH. J Pediatr Surg. 2020;55(1):39–44. https://doi.org/10.1016/j.jpedsurg.2019.09.050.
Stewart CL, Mulligan J, Grudic GZ, Pyle L, Moulton SL. A noninvasive computational method for fluid resuscitation monitoring in pediatric burns: a preliminary report. J Burn Care Res Jan-Feb. 2015;36(1):145–50. https://doi.org/10.1097/BCR.0000000000000178.
Peterson DL, Schinco MA, Kerwin AJ, Griffen MM, Pieper P, Tepas JJ. Evaluation of initial base deficit as a prognosticator of outcome in the pediatric trauma population. Am Surg. 2004;70(4):326–8.
Jung J, Eo E, Ahn K, Noh H, Cheon Y. Initial base deficit as predictors for mortality and transfusion requirement in the severe pediatric trauma except brain injury. Pediatr Emerg Care. 2009;25(9):579–81. https://doi.org/10.1097/PEC.0b013e3181b9b38a.
Hindy-François C, Meyer P, Blanot S, Marqué S, Sabourdin N, Carli P, Orliaguet G. Admission base deficit as a long-term prognostic factor in severe pediatric trauma patients. J Trauma. 2009;67(6):1272–7. https://doi.org/10.1097/TA.0b013e31819db828.
Samaraweera SA, Gibbons B, Gour A, Sedgwick P. Arterial versus venous lactate: a measure of sepsis in children. Eur J Pediatr. 2017;176(8):1055–60. https://doi.org/10.1007/s00431-017-2925-9.
McGillivray D, Ducharme FM, Charron Y, Mattimoe C, Treherne S. Clinical decisionmaking based on venous versus capillary blood gas values in the well-perfused child. Ann Emerg Med. 1999;34(1):58–63. https://doi.org/10.1016/s0196-0644(99)70272-6.
Abuzeid AM, O’Keeffe T. Review of massive transfusion protocols in the injured, bleeding patient. Curr Opin Crit Care. 2019;25(6):661–7.
Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805–13.
Cotton BA, Gunter OL, Isbell J, et al. Damage control hematology: the impact of a trauma exsanguination protocol on survival and blood product utilization. J Trauma. 2008;64(5):1177–82 (discussion 1182-1173).
Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006;60(6 Suppl):S91-96.
Horst J, Leonard JC, Vogel A, Jacobs R, Spinella PC. A survey of US and Canadian hospitals’ paediatric massive transfusion protocol policies. Transfus Med. 2016;26(1):49–56.
Schreiber MA, Perkins J, Kiraly L, Underwood S, Wade C, Holcomb JB. Early predictors of massive transfusion in combat casualties. J Am Coll Surg. 2007;205(4):541–5. https://doi.org/10.1016/j.jamcollsurg.2007.05.007.
Dehmer JJ, Adamson WT. Massive transfusion and blood product use in the pediatric trauma patient. Semin Pediatr Surg. 2010;19(4):286–91. https://doi.org/10.1053/j.sempedsurg.2010.07.002.
Cantle PM, Cotton BA. Prediction of massive transfusion in trauma. Crit Care Clin. 2017;33(1):71–84. https://doi.org/10.1016/j.ccc.2016.08.002.
Yücel N, Lefering R, Maegele M, Vorweg M, Tjardes T, Ruchholtz S, Neugebauer EA, Wappler F, Bouillon B, Rixen D, Polytrauma Study Group of the German Trauma Society. Trauma Associated Severe Hemorrhage (TASH)-Score: probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. Trauma. 2006;60(6):1228–36. https://doi.org/10.1097/01.ta.0000220386.84012.bf (discussion 1236-7).
Nunez TC, Voskresensky IV, Dossett LA, Shinall R, Dutton WD, Cotton BA. Early prediction of massive transfusion in trauma: simple as ABC (assessment of blood consumption)? J Trauma. 2009;66(2):346–52. https://doi.org/10.1097/TA.0b013e3181961c35.
Shih AW, Al Khan S, Wang AY, Dawe P, Young PY, Greene A, Hudoba M, Vu E. Systematic reviews of scores and predictors to trigger activation of massive transfusion protocols. J Trauma Acute Care Surg. 2019;87(3):717–29. https://doi.org/10.1097/TA.0000000000002372.
Acker SN, Hall B, Hill L, et al. Adult-based massive transfusion protocol activation criteria do not work in children. Eur J Pediatr Surg. 2017;27(1):32–5.
Evangelista ME, Gaffley M, Neff LP. Massive transfusion protocols for pediatric patients: current perspectives. J Blood Med. 2020;11:163–72. https://doi.org/10.2147/JBM.S205132.
Hwu TS, Keller MS, Spinella PC, Baker D, Shi J, Leonard JC. Identifying potential predictive indicators of massive transfusion in pediatric trauma. Trauma. 2018;20(2):131–41.
Phillips R, Acker SN, Shahi N, Meier M, Leopold D, Recicar J, Kulungowski A, Partrick D, Moulton S, Bensard D. The ABC-D score improves the sensitivity in predicting need for massive transfusion in pediatric trauma patients. J Pediatr Surg. 2020;55(2):331–4. https://doi.org/10.1016/j.jpedsurg.2019.10.008.
Phillips R, Shahi N, Acker SN, Meier M, Shirek G, Stevens J, Recicar J, Moulton S, Bensard D. Not as simple as ABC: tools to trigger massive transfusion in pediatric trauma. J Trauma Acute Care Surg. 2021. https://doi.org/10.1097/TA.0000000000003412. Online ahead of print.
Cotton BA, Faz G, Hatch QM, Radwan ZA, Podbielski J, Wade C, Kozar RA, Holcomb JB. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. J Trauma. 2011;71(2):407–14. https://doi.org/10.1097/TA.0b013e31821e1bf0 (discussion 414-7).
Rodriguez SA, Morgan GJ, Lara C, Zablah JE. Baseline values of the Compensatory Reserve Index in a healthy pediatric population. Pediatr Cardiol. 2021. https://doi.org/10.1007/s00246-021-02725-8. Online ahead of print.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Moulton co-invented the Compensatory Reserve Index algorithm mentioned in this review. The intellectual property is assigned to the Regents of the University of Colorado. Dr. Moulton co-founded Flashback Technologies, Inc. in 2009 and licensed the technology from the University. He is a consultant at Flashback Technologies, has an equity interest in the company, and receives royalty payments through the University of Colorado. The remaining authors have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Keypoints
1. Adult-based criteria for trauma team activation and other trauma-related protocols lack sensitivity and specificity in the pediatric population.
2. Hypotension is a late finding in children with shock and indicates a child in extremis; new tools should be leveraged to allow early recognition of children at risk for shock.
3. Shock index, pediatric age-adjusted (SIPA) is an age-adjusted tool that is calculated by dividing the heart rate by the systolic blood pressure. An elevated SIPA has been shown to identify severely injured children.
4. The Compensatory Reserve Index (CRI) algorithm uses advanced signal processing methods to assess compensatory features in arterial pulse waveforms and produces a continuous, individual-specific, integrated measure of physiologic compensation, from normovolemia to decompensation.
5. Delayed capillary refill, an elevated SIPA or low CRI indicate shock. These findings warrant aggressive fluid resuscitation and oftentimes an intervention, to prevent an injured child’s physiology from becoming more complex and difficult to control.
6. Incorporating early measures of circulatory compromise such as SIPA or CRI into current practice and existing protocols, may improve pediatric outcomes.
This article is part of the Topical Collection on Pediatric Trauma
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reppucci, M.L., Stevens, J., Moulton, S.L. et al. The Recognition of Shock in Pediatric Trauma Patients. Curr Trauma Rep 8, 202–213 (2022). https://doi.org/10.1007/s40719-022-00239-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40719-022-00239-z