Abstract
Purpose
The use of extracorporeal life support in the intensive care unit has exponentially increased in the last decade. Initially, its use in the burn population lagged behind the dramatic growth in other patient populations; however, in the last 2–3 years, there has been an increase in the number of publications related to its use in this population. In this article, we review the use of contemporary ECMO in the burn patient population and discuss future trends.
Recent Findings
Level 1 evidence for the use of ECMO in any patient population is scarce, and there is no level 1 evidence for the use of ECMO in burn patients. Recently, there has been an increase in case series and case reports describing the use of contemporary ECMO in burn patients. In addition, there are two large retrospective reviews of large registries utilizing ECMO in burn patients.
Summary
The results from these studies all indicate that outcomes using ECMO in this critically ill patient population has survival rates at least comparable to the survival found in other patient populations. There are still many unanswered questions, and future focus needs to address patient selection, timing of initiation, management, and the duration of ECMO therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The History of ECMO in the Burn Patient
In 1972, the first patient ever treated with ECMO was reported. He was a young trauma patient with severe chest trauma, and aortic injury who subsequently developed “shock lung” or what we now call acute respiratory distress syndrome (ARDS) [3•]. Several years later, the first randomized trial evaluating ECMO versus conventional ventilation was published and demonstrated no mortality benefit, and perhaps even detriment with the use of ECMO in ARDS. However, close evaluation reveals several things which likely led to poor outcomes such as the use of veno-arterial (VA) ECMO for all patients, the use of roller pumps, the use of high dose anticoagulation strategies, and a lack of standardization of devices (four different oxygenators were used). Interestingly, the study had abysmal survival, not only for the ECMO-treated group, but also for the control group which did not receive ECMO. Thus, while we now know this study appears to be an outlier, not only for ARDS patients treated with ECMO but for ARDS patients managed with conventional ventilation strategies, it did dampen the enthusiasm for ECMO in the intensive care unit (ICU).
In the meantime, the industry continued to improve technologically. Percutaneous access techniques were developed, biocoatings were developed to line circuits decreasing the inflammatory response, and centrifugal pumps replaced historic roller pumps leading to less hemolysis and coagulopathy. In 2009, the CESAR trial was published demonstrating the first randomized controlled trial comparing ECMO versus conventional strategies [4]. While criticized for some methodologic design flaws, this was the first Level 1 data demonstrating a survival benefit for ECMO. In the same year, the H1N1 influenza pandemic struck the world, and large retrospective studies revealed excellent outcomes with the use of ECMO in this patient population. This led to an explosion in the use of ECMO, and growth continues to the current date. No longer used only when patients are on the brink of death as a rescue therapy, we are finding that the sooner the pathologic effects of positive pressure ventilation are mitigated on damaged lungs, the better the outcomes. Due to the improved safety profile with new pumps and safer circuits, this treatment modality is finding ever broader indications for use and patient populations previously thought to have been too high risk for ECMO (i.e., trauma) are now able to benefit from this modality [5, 6]. However, a brief perusal of the literature will demonstrate that this modality has been much slower to “catch on” in the Burn ICU literature.
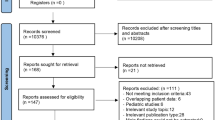
The first reported successful use of ECMO in a burn patient in the United States was in 1998 [7]. Since that time, there are only a handful of case series or case studies that have reached the literature. One of the first series evaluating ECMO in burn patients consisted of a series of three patients in 2001 [8]. In this study, all patients were initially cannulated VV, with one patient requiring conversion to V-VA for hemodynamic instability. Prior to 2009, one of the largest studies evaluating the use of ECMO in 81 adults patients from 1999 to 2008, showed the survival rate for “trauma or burn” patients treated with ECMO was significantly lower (33%) than patients treated with ECMO for other etiologies such as viral pneumonia (78%) or bacterial pneumonia (53%) [9]. In 2013, Asmussen et al., published a systematic review evaluating all literature through March 1, 2012, for burn patients treated with ECMO [10]. At that time, they found eight animal studies, 14 case reports/series, and only six clinical trials meeting criteria for inclusion. Of the six clinical studies (published between 1999 and 2010), only three included adult patients [8, 9, 11] with overall survival rates ranging from 53 to 67%. Two of these studies overlap. The early work at Massachusetts General published by Masiakos et al. 1999 included 31 patients, and the work published by Nehra, et al., a decade later in 2009 included 81 patients. It is important to note that out of these three studies, only 13 of the 84 patients evaluated had “trauma or burn.” Therefore, the review article by Asmussen et al. concluded there was insufficient evidence to draw any type of conclusions about the use of ECMO in patients with burn injury.
The Contemporary Use of ECMO in the Burn Patient
This paucity of literature in the burn population during the advent of ECMO in the USA is striking for two reasons: (1) the use of ECMO for ARDS increased 433% from 2006 to 2011 in non-burn patients [1] and (2) burn is a pathology characterized by high rates of ARDS with significantly increased mortality in those patients developing ARDS [12].
Since the systemic review by Asmussen, et al. in 2013, there has been an increase in the number of studies evaluating the use of ECMO in burn patients utilizing contemporary techniques and devices [10]. Table 1 outlines the studies that include adult patients in which treatment was provided after 2009.
In 2016, one of the first reviews looking at the modern use of ECMO in burn patients reported a shockingly high mortality rate. A retrospective study evaluating 11 patients treated for respiratory failure after burn injury reported a 28-day, 90-day, and in-hospital mortality of 56%, 72%, and 91% [13]. Only one patient lived in this series. The report is written as a letter to the editor and lacks many important details such as burn severity. There is also no indication of disease severity prior to cannulation such as an Apache-II or SOFA score. These results are also not reported with the same metric currently used to track survival outcomes within the ELSO registry, which are (1) successful weaning from ECMO (ECLS survival) and (2) survival to discharge or transfer. Reading through the letter carefully, you can discern the ECLS survival rate was 45% (five patients successfully decannulated) while only two patients made it out of the ICU (survival to transfer 18%) but only one patient made it home (survival to discharge 9%). It is unclear why the mortality was so high after decannulation, though the ECLS runs were comparatively short with an average run of 3.5 days (ranging from 0.5–8.8 days). Other factors perhaps contributing to the high mortality in this series include a high rate of inhalational injury (55%), an older patient population (average age 51 years, ranging from 40 to 72), and the need for VA ECMO in almost a third of the patients. Also, important to note, the author’s make no mention of their ECMO ventilation strategy which can have a profound impact on survival [20].
The next case series published was from a stun grenade explosion in Taiwan [14]. Six patients were brought in with large thermal burns (total body surface area (TBSA) average 89% ranging from 50–99%) as well as evidence of explosion comorbidities (i.e., pneumothorax and open fractures). The average Baux score was quite high at 132, ranging from 99 to 155. Five of the six patients had evidence of inhalational injury and they ranged in age from 29 to 59 years (average 43). Three of the six patients required cardiopulmonary resuscitation and four of the patients were placed immediately on VA ECMO. Only one patient survived to discharge (17%). However, in this series, it is obvious that the expected mortality rate would be very high.
The three additional studies left in our review all reported much better survival to discharge or transfer, ranging from 71 to 100% [15, 16••, 17]. It is important to note in the Eldredge, et al., study that only two of the eight patients included were over the age of 15. The other four are pediatric patients and this may have influenced the survival rate (100%), as pediatric survival with ECMO is quite good.
In 2017, two reviews looking at large registries were also done. Nosanov, et al. evaluated the National Burn Repository and found 30 patients treated with ECMO with a survival to discharge rate of 47% [18••]. The Extracorporeal Life Support Organization Registry was reviewed by Burke, et al. in the same year and found 58 patients with burn injury and a discharge to survival rate of 43% [19••]. While there are limitations with these large registry reviews, they provide valuable insight in the advances being made in the burn patient treated with extracorporeal support.
Discussion
To summarize, ECMO use in the burn patient, despite an initial lag, is slowly growing, now mirroring the growth in other patient populations. Review of contemporary studies is important, and seems to indicate that the survival in patients with burns can match the survival of patients treated for non-burn reasons. The VV ECMO survival to discharge rate for all comers (over 11,000 patients) in the ELSO registry for January 2019 is 59% [21].
Future Trends
There is still much work to be done in understanding the role of ECMO in the severely burned patient. Understanding the underlying disease pathology is crucial, and it is an oversimplification to lump all patients treated with ECMO into the same group. Management is dependent on the underlying pathology. Burn injury represents an immediate, profound inflammatory response especially with inhalational injury, rather than an evolving inflammatory response as in patients with ARDS due to infectious reasons. Therefore, burn patients present with completely different pathology, and deserve special recognition for research and management reasons. These patients often present or develop hypovolemic shock, due to massive volume losses from large wounds. This necessitates aggressive resuscitation, often at the risk of worsening pulmonary edema in injured lungs. ECMO can relieve the burden of gas exchange, allowing for aggressive resuscitation. However, ECMO also requires adequate volume status to function, and thus the shock that occurs from hypovolemia is not relieved by VV or VA ECMO, which may explain some of the increased mortality associated with VA ECMO in burn and perhaps even trauma patients.
We also found many of the studies demonstrate relatively short run times, which may be reflective of the high mortality rate. One early study demonstrated that survival was improved in patients with run times less than 300 h [11]. This may have led to patients being decannulated too early and perhaps led to higher mortality in studies such as the series reported by Soussi, et al. [13]. The average run time for ECMO for ARDS in the large controlled trials is longer, with a median of 9 days (interquartile range of 6 to 16) in the CESAR trial and a mean of 15 days (standard deviation ± 13 days) in EOLIA [4, 22]. The optimum management and weaning strategy for this disease process (burn injury) has yet to be determined. We have been using the EMPROVE protocol (ECMO for PROtective VEntilation) for management and weaning in our trauma and burn population with good results (Fig. 1) [5, 23••].
Current studies are a heterogenous mix of patients with inhalational injury and refractory hypovolemic shock playing important roles. Burn patients requiring VA ECMO portend a poor outcome. There is a similar pattern in the trauma literature [5, 24]. Therefore, just as with other patient populations, patient selection is crucial. Recognition of futility is also an area that warrants further investigation as ECMO is a resource intensive and costly intervention. ECMO will continue to be a rescue therapy, and while mortality is high for tragedies like the Stun Grenade explosion [15], the use of ECMO is appropriate and this study illustrates a heroic and valiant effort to save life.
Conclusion
The ever-expanding role and increasing safety profile of mechanical support for the cardiopulmonary system in the intensive care unit makes evaluating this technology in the burn patient a field ripe for study. There is a need for high-quality randomized controlled trials to determine the appropriate patient selection and management techniques for these patients. We have enough data to support the use of ECMO in the burn patient. The time has come.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sauer CM, Yuh DD, Bonde P. Extracorporeal membrane oxygenation use has increased by 433% in adults in the United States from 2006 to 2011. ASAIO J. 2015;61(1):31–6.
Combes A, Bacchetta M, Brodie D, Muller T, Pellegrino V. Extracorporeal membrane oxygenation for respiratory failure in adults. Curr Opin Crit Care. 2012;18(1):99–104.
• Hill JD, O’Brien TG, Murray JJ, Dontigny L, Bramson ML, Osborn JJ, et al. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson-membrane lung. N Engl J Med. 1972;286:629–34 The first reported use of ECMO in the literature.
Peek GJ, Mugford M, Tiruviopati R, Wilson A, Allen E, Mariamma MT, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicenter randomized controlled trial. Lancet. 2009;374:1351–63.
Grant AA, Hart VA, Lineen EB, Lai C, Ginzburg E, Houghton D, et al. The impact of an advanced ECMO program on traumatically injured patients. Artif Organs. 2018;42(11):1043–51.
Bosarge PL, Raff LA, McGwin G Jr, Carroll SL, Bellot SC, Diaz-Guzman E, et al. Early initiation of extracorporeal membrane oxygenation improves survival in adult trauma patients with severe adult respiratory distress syndrome. J Trauma. 2015;81(2):236–43.
Patton ML, Simone MR, Kraut JD, Anderson HL III, Haith LR Jr. Successful utilization of ECMO to treat an adult burn patient with ARDS. Burns. 1998;24:566–8.
Chou NK, Chen YS, Ko WJ, Huang SC, Chao A, Jan GJ, et al. Application of extracorporeal membrane oxygenation in adult burn patients. Artif Organs. 2001;25(8):622–6.
Nehra D, Goldstein AM, Doody DP, Ryan DP, Chang Y, Masiakos PT. Extracorporeal membrane oxygenation for nonneonatal acute respiratory failure. Arch Surg. 2009;144(5):427–32.
Asmussen S, Maybauer DM, Fraser JF, Jennings K, George S, Keiralla A, et al. Extracorporeal membrane oxygenation in burn and smoke inhalation injury. Burns. 2013;39:429–35.
Masiakos PT, Islam S, Doody DP, Schnitzer JJ, Ryan DP. Extracorporeal membrane oxygenation for nonneonatal acute respiratory failure. Arch Surg. 1999;134(4):375–80.
Ray JJ, Straker RJ, Hart VJ, Meizoso JP, Schulman CI, Loebe M, et al. The use of extracorporeal membrane oxygenation for acute respiratory distress syndrome in severe burns without inhalation injury. J Burn Care Res. 2018;39:640–4.
Soussi S, Gallais P, Kachatryan L, Benyamina M, Ferry A, Cupaciu A, et al. Extracorporeal membrane oxygenation in burn patients with refractory acute respiratory distress syndrome leads to 28% 90-day survival. Intensive Care Med. 2016;42:1826–7.
Hsu PS, Tsai YT, Lin CY, Chen SG, Dai NT, Chen CJ, et al. Benefit of extracorporeal membrane oxygenation in major burns after stun grenade explosion: experience from a single military medical center. Burns. 2017;43:674–80.
Chiu YJ, Ma H, Liao WC, Shih YC, Chen MC, Shih CC, et al. Extracorporeal membrane oxygenation support may be a lifesaving modality in patients with burn and severe acute respiratory distress syndrome: experience of Formosa Water Park dust explosion disaster in Taiwan. Burns. 2018;44:118–23.
•• Ainsworth CR, Dellavolpe J, Chung KK, Cancio LC, Mason P. Revisiting extracorporeal membrane oxygenation for ARDS in burns: a case series and review of the literature. Burns. 2018;44:1433–8 The largest case series describing in detail the use of ECMO in burn patients. The authors provide an excellent overview of the pathophysiology and a review of the current challenges facing implementation in the burn population.
Eldredge RS, Zhai Y, Cochran A. Effectiveness of ECMO for burn-related acute respiratory distress syndrome. Burns. 2019;45:317–21.
•• Nosanov LB, McLawhorn MM, Cruz MV, Chen JH, Shupp JW. A national perspective on ECMO utilization in patients with burn injury. J Burn Care Res. 2018;39:10–4 Retrospective review of the National Burn Repository database evaluating the use of ECMO in burn patients. Results should be interpreted with caution as it does include patients treated before the onset of modern ECMO devices and management practices in 2009.
•• Burke CR, Chan T, McMullan DM. Extracorporeal life support use in adult burn patients. J Burn Care Res. 2017;38:174–8 Retrospective review of the Extracorporeal Life Support Registry evaluating the use of ECMO in burn patients. This is the largest study of patients in the literature (n= 58); however, this study also includes patients treated before modern ECMO devices and practices were adopted (1999–2015).
Grant AA, Badiye A, Mehta C, Wu Z, Koerner M, Vianna R, et al. EMPROVING outcomes: evaluating the effect of an ultra-lung protective strategy for patients with ARDS treated with ECMO. J Heart Lung Transplant. 2019;38(4):S336.
The Extracorporeal Life Support Organization. ECLS Registry Report, International Summary, January 2019. https://www.elso.org/Registry/Statistics.aspx. Accessed 19 April 2019.
Combes A, Hajage D, Capelliar G, Demoule A, Lavoue S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome (EOLIA). N Engl J Med. 2018;378:1965–75.
•• Grant AA, Hart VJ, Lineen EB, Badiye A, Byers PM, Patel A, et al. A weaning protocol for venovenous extracorporeal membrane oxygenation with a review of the literature. Artif Organs. 2018;42(6):605–10. https://doi.org/10.1111/aor.13087Describes a lung protective strategy utilized successfully in patients with traumatic and burn injury.
Ahmad S, Menaker J, Kufera J, O’Connor J, Scalea T, Stein D. Extra-corporeal membrane oxygenation following traumatic injury. J Trauma. 2017;82(3):587–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Grant has nothing to disclose. Dr. Ghodsizad has nothing to disclose. Dr. Ingram has nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection in Burns
Rights and permissions
About this article
Cite this article
Grant, A.A., Ghodsizad, A. & Ingram, W. ECMO in the Burn Patient: the Time Has Come. Curr Trauma Rep 5, 154–159 (2019). https://doi.org/10.1007/s40719-019-00168-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40719-019-00168-4