Abstract
Purpose of Review
This review describes the current role of diagnostic and interventional radiology in the management of solid organ trauma, particularly the role of non-operative endovascular interventions such as angioembolization (AE). We will also provide a brief highlight of interventions available for thoracic trauma.
Recent Findings
There has been a paradigm shift over the past 2 decades in the management of solid organ injuries from surgical management to non-operative management, especially in cases of minor injuries. Many factors, including the advances in multidetector contrast enhanced CT (MD-CECT) imaging, demands of cost-effective healthcare, and innovation of minimally invasive interventions with lower complication rates than surgical laparotomy have all contributed to this shift. Interventional radiology now plays a crucial role in the management of solid organ trauma, focusing on less invasive endovascular therapies. In addition, the grading and triaging of patients with stable solid organ traumatic injuries has become more reliant on MD-CECT findings.
Summary
This review article highlights the common imaging findings, grading systems, and most current management guidelines for solid organ trauma with a brief highlight of thoracic trauma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trauma is the leading cause of death in the USA for both men and women under the age of 45 and is the fourth most common cause of overall mortality for all ages [1]. Blunt abdominal trauma accounts for a large proportion of these mortalities [1]. The amount of resources needed to care for these patients as well as the economic burden which trauma places on our healthcare system are substantial. In fact, trauma accounts for approximately $80 billion per year in direct medical care costs [1].
The diagnosis and management of trauma is complex, and has evolved over the past century. In particular, the management of hemodynamically stable patients has changed from operative to non-operative management [2]. With the technologic advances in imaging, particularly the advent of rapid acquisition and high spatial resolution MD-CECT, radiology now plays an ever increasing role in both the diagnosis and management of solid organ trauma [3]. The solid organs are very commonly injured during traumatic injuries, and the most commonly injured solid organs in order from most common to least common are the spleen, liver, kidneys, and pancreas [4]. The American Association for the Surgery of Trauma (AAST) grading system is based on MD-CECT findings, and therefore the rapid and accurate interpretation of MD-CECT is essential to patient care [5]. Like many other disease entities, the complex nature of solid organ trauma requires a multidisciplinary approach with rapid and effective communication between all members of the healthcare team. Because of the recent paradigm shift toward non-operative management in stable solid organ trauma, interventional radiology (IR) now plays a major role in the management of these patients. Image-guided vascular and non-vascular interventions are effective minimally invasive treatment options for certain select patients which have lowered failure rates for non-operative management [6••, 7••].
Initial Workup and Imaging Modalities in Solid Organ Trauma
In most large level 1 trauma centers, an algorithm is used to triage patients with solid organ trauma. The most widely accepted algorithms are based upon the hemodynamic status of the patient [6••, 7••]. If the patient is hemodynamically unstable or has diffuse peritonitis, the patient typically undergoes chest X-ray, pelvic X-ray, and focused assessment with sonography for trauma (FAST) prior to surgery [8]. The primary use of the FAST exam is to screen for free intraperitoneal/retroperitoneal free fluid and/or hemoperitoneum [9]. The FAST exam is performed in the supine position using a 3.5–5.0 MHz convex transducer. Four standard views are obtained: transverse subxiphoid, longitudinal view of the right upper quadrant, longitudinal view of the left upper quadrant, as well as transverse and longitudinal views of the suprapubic region [9]. The minimum amount of free fluid which is able to be detected on FAST exam is approximately 200 mL [10].
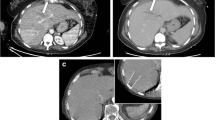
Hemodynamically stable patients will typically undergo MD-CECT of the chest, abdomen, and pelvis (CAP) using intravenous contrast (100–150 mL of low or iso-osmolar contrast). Imaging is typically performed in the portal venous phase of contrast enhancement (65–80 s after the start of contrast administration) [11•]. If active contrast extravasation or pseudoaneurysm is identified on the portal venous phase images, an immediate delayed scan can be obtained to differentiate between contrast extravasation and pseudoaneurysm (Fig. 1). Abnormal enhancement from a pseudoaneurysm will typically remain stable in size whereas active extravasation will increase in density and size on the delayed phase images [12]. If a patient has hematuria or there is high suspicion for injury to the renal collecting system and/or ureters, a 5-min post-contrast delayed imaging should be obtained. In cases of pelvic fractures, hematuria, suspected bladder, or distal ureteral injury, a CT cystogram should be performed. It typically involves administration of 300–500 mL of dilute contrast via a Foley catheter into the bladder. The extravasation of the contrast into the peri-vesicular or peri-urethral tissues help differentiate between intra-peritoneal and extraperitoneal bladder ruptures as well as localize the site of leakage [13, 14].
Splenic injuries. a Axial image of a grade II splenic laceration (black arrow) with contrast extravasation (open arrow) and hemoperitoneum. b Celiac angiogram demonstrates active extravasation from a superior branch of the splenic artery (arrow). c Splenic artery angiogram after distal coil embolization of a superior branch of the splenic artery demonstrates hemostasis without evidence of further contrast extravasation
Hemoperitoneum
Traumatic solid organ injury is commonly associated with hemoperitoneum. CT is more accurate than ultrasound in detecting hemoperitoneum and localizing the source of bleeding. On CT, the attenuation value of free intraperitoneal blood typically ranges between 30 and 45 HU. In contrast, simple free fluid has an attenuation value of 0–10 HU. On ultrasound, acute hemoperitoneum is difficult to distinguish from simple free fluid as the identification of internal echoes is very operator and machine dependent. Non-clotted blood tends to gravitate to dependent sites such as Morrison’s pouch or the pouch of Douglas (recto-vesicle pouch in males) and flows freely between peritoneal recesses. Therefore, the location of the hemoperitoneum alone does not always correlate with the site of injury. Localization of the source of hemorrhage is vital for the management of solid organ trauma.
The source of bleeding is not always conspicuous in cases of solid organ trauma from the history and physical exam alone. CT is particularly helpful to localize the site of bleeding. Blood located adjacent to the site of injury tends to be partially clotted, and is slightly hyperdense (45–70 HU) when compared to non-clotted blood. This phenomenon termed the sentinel clot sign is helpful in localizing the source of bleeding in difficult cases [15]. On-going bleeding can be identified by active contrast extravasation from MD-CECT images. The site and extent of active extravasation play a more important factor in clinical decision making than the actual volume of hemoperitoneum. A large volume of hemoperitoneum does not necessitate the need for emergent laparotomy [16]. One pitfall in evaluating hemoperitoneum comes into play with anemic patient in whom hemoperitoneum may measure less than 20 HU. In such patients, it may not be possible to distinguish hemoperitoneum from simple fluid [17].
Splenic Injuries
The spleen is the most commonly injured solid abdominal organ accounting for approximately half of blunt abdominal injuries [18]. The spleen plays a vital role in immune function, especially in the defense against encapsulated microorganisms. Patients who undergo splenectomy are at risk for severe infection and sepsis [19]. Therefore, non-operative management has become the standard of care in hemodynamically stable patients with splenic injuries. Non-operative management has a success rate ranging from 80 to 90% [20]. The goal is to preserve viable splenic function by avoiding splenectomy. Management of stable patients is heavily dependent on CT findings. The AAST developed a grading system for splenic injuries based on CT findings in 1989 and further revised it in 1994. This grading system describes splenic lacerations and hematomas based on their size and location. A splenic laceration is a well-defined linear or branching hypodensity passing through the normally enhancing tissue. Splenic lacerations are graded based upon their length: grades I–II for lacerations less than or equal to 3 cm, and grade III for lacerations greater than 3 cm (Fig. 1). Hematomas can either be intraparenchymal or subcapsular. A subcapsular hematoma appears as a crescentic low-density collection of blood between the splenic capsule and parenchyma. In comparison, intraparenchymal hematoma is usually a round ill-defined hypodensity within normal vascularized splenic parenchyma (Fig. 2). Hematomas are also graded based upon their size. Grade IV splenic injuries are defined as lacerations extending into and involving segmental or hilar vessels resulting in devascularization of greater than 25% of the spleen (Fig. 3). Grade V injuries are the most severe and encompass shattered or completely devascularized spleen. Grades IV and V injuries are associated with high morbidity and mortality [21•]. A major limitation of the AAST grading system is that active extravasation and contained-vascular injury such as arteriovenous fistula (AVF) and pseudoaneurysm (PSA), are not taken into account. An algorithm based upon contrast extravasation that accounts for these abnormalities has been described by the Canadian Association of Radiologists [22].
Splenic injuries. a Axial CT shows multiple lacerations (black arrows), one that extends into the splenic hilum compatible with grade IV splenic injury. b More superior axial image of the spleen demonstrates hemoperitoneum (star) and active extravasation of contrast (black arrow). c Celiac angiogram fails to demonstrate active extravasation of contrast. d Splenic artery angiogram status post proximal coil embolization of the main splenic artery
Angiographic evaluation and possible embolization is indicated in hemodynamically stable patients with grades IV or V injuries, active contrast extravasation, vascular injury such as AVF or PSA, moderate hemoperitoneum, or evidence of ongoing splenic bleeding [6••]. Successful angioembolization of the bleeding splenic artery is effective in achieving hemostasis in over 90% of cases of hemorrhagic splenic injury [23]. Another indication which has emerged over the last decade is proximal embolization of the splenic arterial trunk in hemodynamically stable patients with high grade injuries and no evidence of hemorrhagic lesion on CT in order to reduce the risk of secondary splenectomy. It has been shown that proximal embolization reduces the vascularization pressure within the spleen allowing traumatic vascular injuries to heal, and decreasing the splenectomy rate by 18% [24, 25]. Additionally, angioembolization can increase the nonoperative salvage rate in patients with splenic trauma [6••].
During angiographic evaluation, celiac and splenic artery angiograms should be performed using a Cobra or Simmons catheter to select the celiac artery. The left gastric artery should be identified as it is often an important collateral feeder vessel to the spleen. The findings on the angiogram determine the most effective technique used for angioembolization. For instance, coil embolization of the proximal splenic artery is desired for injuries with on-going active hemorrhage indicated by active extravasation or intrasplenic contrast blush on the angiogram to rapidly control hemorrhage. Proximal embolization can also be performed in hemodynamically stable patients with clinical evidence of on-going bleeding without contrast extravasation on CT or angiography (Figs. 3 and 4). For proximal embolization, the splenic artery should be embolized distal to the origin of the dorsal pancreatic artery in order to preserve collateral blood supply to the spleen. A more distal selective embolization is warranted (utilizing a coaxial microcatheter system) for PSA or AVF. For distal embolization, care should be taken to place the microcatheter as distal as possible before embolization to preserve native arterial supply to the spleen [26,27,28, 29•]. It is important to embolize both proximal and distal to the PSA or AVF to prevent recurrent hemorrhage. Care should be taken not to deploy coils within an acute traumatic PSA to minimize the risk of expansion and rupture of the PSA. A meta-analysis comparing severe complications requiring splenectomy following angioembolization showed no statistical difference between proximal and distal embolization. However, the rate of splenic infarction not warranting splenectomy was shown to be higher for distal embolization [30]. Proximal embolization is technically less challenging and less time consuming. Therefore, proximal embolization is preferred in cases of active hemorrhage where time is of the essence [29•]. The utility of follow-up CT following angiographic intervention is controversial. A repeat CT may be considered in high-grade injuries to assess for delayed complications such as PSA or AVF.
Splenic injuries. a Axial CT image demonstrates an approximately 5-cm splenic laceration (black arrows) with active extravasation (open arrow) compatible with grade III splenic injury. b Celiac angiogram failed to demonstrate contrast extravasation. c DSA image demonstrates coil embolization of the main splenic artery
Liver Injuries
The liver is the second most commonly injured organ in blunt abdominal trauma with an incidence rate of 15–20% [31]. Although hepatic injuries are less common than splenic injuries, hepatic injuries are the most common cause of death in blunt abdominal [32]. An AAST grading system for hepatic injuries has been described. Lacerations are the most common imaging findings in liver trauma and are graded based upon their depth (less than or equal to 3 cm for grades I–II, and greater than or equal to 3 cm for grades III–V injuries) (Fig. 5). Hepatic lacerations appear as well-defined linear or branching hypodensities within the normally enhancing parenchyma. Hematomas can be subcapsular or intraparenchymal, and are also graded based upon their size. Subcapsular hematomas are well-defined crescenteric collections of hemorrhagic fluid between the liver capsule and parenchyma. Parenchymal hematomas usually appear as ill-defined areas of hypoattenuation within the parenchyma. Grade IV injuries are defined as parenchymal disruption of 25–75% in a single hepatic lobe or parenchymal disruption of 1–3 segments (Fig. 6). Injuries to the retrohepatic IVC or hepatic veins are also categorized as grade IV injuries. Parenchymal disruption of greater than 75% in 1 lobe is categorized as a grade V injury. A complete hepatic avulsion is considered a grade VI injury and has a 91.5% mortality rate [21•, 22]. Just as in splenic trauma, active extravasation and contained vascular injuries are not accounted for in the current AAST grading system [22]. Hepatic injury may also lead to retroperitoneal hemorrhage if the injury extends into the bare area of the liver. The bare area of the liver is located posteriorly, and is devoid of peritoneal lining [33].
Liver injuries. a Axial CT demonstrates approximately 4-cm laceration in the left hepatic lobe (black arrow) with associated hemoperitoneum (black star) and active extravasation of contrast (white arrow) compatible with grade III liver injury. b Celiac angiogram demonstrates active a contrast blush from a tertiary branch of the left hepatic artery. c DSA angiogram status post coil embolization of a secondary/tertiary branch of the left hepatic artery demonstrates stasis without further contrast extravasation
Hepatic injuries. a Axial CT demonstrates a large intraparenchymal hematoma with an area of focal extravasation (arrow) compatible with a grade IV hepatic injury. b Right hepatic artery DSA angiogram shows a small area of active extravasation. c DSA angiogram post coil embolization of the segment 7 branch of the right hepatic artery demonstrates stasis
The majority of liver injuries are managed non-surgically with success rates ranging from 82 to 100% [7••]. Non-operative management has a high success rate in liver trauma as mentioned previously; however, complications are relatively common for high-grade injuries. In fact, the complication rate of grade III injury is 1% but increases to 21% for grade IV trauma, and to 63% for grade V trauma. Major complications include hemobilia, bile peritonitis, bilious ascites, hemoperitoneum, abdominal compartment syndrome, missed injuries, hepatic abscess, and delayed hemorrhage. Bile leaks and bilomas are delayed complications that occur in approximately 3.2% of all hepatic injuries [7••]. On CT scan, they appear as low attenuating fluid collections with a lower density than hematoma, and enlarge over time. Hepatobiliary scintigraphy is an accurate test to detect bilomas and biliary leaks [34]. These can be managed surgically or with image-guided percutaneous drainage.
Typical indications for angioembolization include stable patients with high-grade injury (AAST grade III or greater), unstable patients following laparotomy and surgical packing in order to reduce the risk of delayed hemorrhage, cases of hepatic venous injury, and cases of AVF or PSA. Delayed vascular complications such as AVF and PSA can be seen in up to 20% of liver injuries [35]. AVFs appear as dilated tortuous veins with early filling in the arterial phase. PSAs can be seen as focal contained areas of contrast blush adjacent to arteries on MD-CECT, and do not enlarge on delayed imaging in contrast to active extravasation. Angioembolization has been reported to be up to 83% effective in controlling bleeding after blunt hepatic injury [7••]. When performing angioembolization of the liver, it is important to first perform a celiac angiogram carried out through the portal venous phase to map out the anatomy and ensure normal hepatopetal flow. Once the abnormality is identified, sub-selective catheterization is performed using a coaxial microcatheter system to embolize proximal and distal to the takeoff of the injured artery. Typically coils are used for embolization; however, gelfoam or particles can also be used [36, 37]. All attempts should be made to identify and avoid embolization of the cystic artery as non-target embolization of the gallbladder is a common complication leading to gallbladder necrosis [36]. Contrary to the spleen, infarction of the hepatic parenchyma after angioembolization is a much less common complication as the liver has a dual blood supply. There is no consensus regarding follow-up imaging after embolization; however, it is generally recommended in high grade injuries to identity delayed complications such as AVF, PSA, and biloma. Hepatobiliary scintigraphy and magnetic resonance imaging/cholangiopancreatography (MRI/MRCP) can also be performed to delineate biliary leaks.
Kidney Injuries
The kidney is the third most common organ injured in blunt abdominal trauma occurring in approximately 1–5% of cases. Hematuria is an accurate predictor of urinary tract injury [38,39,40]. An AAST grading system also exists for renal trauma ranging from grades I–V. The AAST classifies renal injury based on the type, size, and location of injury on CT. The types of renal injuries included in the grading system are contusions, hematomas (perirenal and subcapsular), lacerations, major vascular injury, and avulsion of the renal hilum. A renal contusion is a characterized as a focal area of decreased enhancement within the renal parenchyma. Renal hematomas can either be subcapsular or perirenal. A subcapsular hematoma appears as a crescentic hemorrhagic collection between the renal capsule and parenchyma, and depending on the size may exert mass effect upon the renal parenchyma. A perirenal hematoma is a hemorrhagic collection outside of the renal capsule in the perirenal space. A perirenal hematoma is commonly associated with a laceration. Renal lacerations are well-defined linear or branching hypodensities. A grade 1 injury is classified as a contusion or non-expanding subcapsular hematoma. A grade II injury is a non-expanding perirenal hematoma confined to the renal retroperitoneum or a laceration <1 cm. A grade III injury is a laceration >1 cm without injury to the collection system. A grade IV injury is a laceration which extends through the cortex, medulla, and collecting system or injury to the main renal artery or vein with contained hemorrhage. A grade V injury is a completely shattered kidney or avulsion of the renal hilum with devascularization [38,39,40, 41•].
Renal-collecting system injury should be suspected when there is perinephric fluid identified measuring 0–20 HU. Again, when renal injury is suspected, a 5-min delayed scan should be obtained in addition to the portal venous phase scan to evaluate for a renal collecting system and/or ureteral injury. The presence of urinoma is confirmed when there is extravasation of contrast-opacified urine into the perinephric space [38, 39].
Renal vascular trauma typically manifests as laceration or thrombosis of the renal artery or its branches leading to infarction (Fig. 7). An infarct manifests as a peripheral wedge-shaped area of non-enhancement on MD-CECT images. The most severe injury involves laceration or thrombosis of the main renal artery which manifests on CT as non-enhancement of the entire kidney and rapid cutoff of the main renal artery at the level of occlusion. CT findings for injury to the main renal vein include non-enhancement of the renal vein and persistent nephrogram on the affected side [42]. As in splenic and liver injury, the AAST grading scale for kidney injury does not account for active extravasation or PSA (Fig. 8).
Kindney injuries. a Coronal CT demonstrates a renal laceration (arrow) that extends to the renal hilum with non-enhancement (infarction) of the lower pole of the right kidney compatible with a grade IV injury. b DSA selective angiogram of an anterior lower pole branch of the right renal artery demonstrates active extravasation of contrast (arrow). c DSA right renal angiogram post gelfoam embolization of distal lower pole anterior branch of the right renal artery shows no evidence of further contrast extravasation
Kidney injuries. a Axial CT image demonstrates a left renal laceration measuring approximately 1.3 cm (black arrow) with an associated small perirenal hematoma (asterisk) compatible with a grade III renal injury. b Axial CT 10 days later of the same patient demonstrates a contained-enhancing focus (black arrow) in the region of the laceration compatible with a PSA. c DSA renal artery angiogram demonstrates a pseudoaneurysm (arrow) arising from a superior pole distal branch of the renal artery. d DSA renal artery angiogram post coil embolization proximal and distal to the PSA demonstrates no further filling of the PSA
The vast majority (75–80%) of renal trauma are minor injuries (grades I–III) and are managed conservatively. Unstable patients or grade V injuries typically require emergent surgical management. The goal of non-surgical management is to avoid a nephrectomy and to preserve renal function. Rapid diagnosis and treatment of renal trauma is critical as renal ischemia lasting for more than 3 h can result in tubular necrosis and permanent renal dysfunction [43]. Angioembolization is indicated in stable patients with AAST grade III or greater. Distal superselective embolization can be performed in cases of arterial laceration, AVF, and PSA using either coils, gelfoam, or particles [44•]. Because the kidneys are an end organ without collateral supply, care should be taken to embolize as distal as possible in order to preserve renal function. A success rate of as high as 93% has been reported for emergent cases [43]. Another technique implemented by IR in renal trauma is renal stenting. Indications for renal artery stenting are laceration, dissection, or occlusion of the main renal artery. In cases of ureteral injury, percutaneous nephrostomy may be indicated to direct urinary flow away from the site of injury, and thus to promote healing [44•].
Pancreatic Injuries
Blunt pancreatic trauma is relatively uncommon, accounting for less than 2% of all abdominal injuries [45, 46]. Pancreatic injuries occur most commonly from direct impact to the upper abdomen which compresses the pancreas against the vertebral column as in steering wheel and handle bar injuries [47]. Pancreatic injuries occur more commonly in the pediatric population as they have less protective peripancreatic fat. Clinical signs and symptoms of pancreatic injury are often non-specific. The classic triad of leukocytosis, elevated amylase, and upper abdominal pain is rarely encountered [48]. Pancreatic injuries occur rarely in isolation and are commonly associated with injuries to other solid abdominal organs. In fact, 90% of pancreatic injuries involve at least one other organ [45]. The body of the pancreas is the most common site of pancreatic injury. In fact, approximately two-thirds of pancreatic trauma involves the pancreatic body [49].
MD-CECT is used as the initial imaging modality in hemodynamically stable pancreatic injuries. The sensitivity and specificity of CT for pancreatic trauma has been reported to be approximately 80% [50]. CT findings can be subtle, and range from a small contusion to complete transection or comminution of the pancreas. A pancreatic contusion appears as a focal area of hypoattenuation or decreased enhancement within the parenchyma. A laceration is a linear or branching hypodensity. A transection is a full-thickness laceration [50]. The most severe injury is a comminuted or shattered pancreas. Secondary findings include peripancreatic fat stranding, peripancreatic fluid collections, fluid between the splenic vein and pancreas, thickening of the anterior pararenal fascia on the left, and hemorrhage [48]. An AAST grading system has been described for pancreatic injuries. Grade I injuries include minor contusions without duct injury and superficial lacerations without duct injury. Major contusions and lacerations without duct injury constitute grade II injuries. Distal transection or parenchymal injury with duct injury is classified as grade III injury. Grade IV injury is proximal transection or parenchymal injury involving the ampulla or bile duct. Finally, grade V injury is massive disruption of the pancreatic head [51] (Fig. 9).
Pancreatic injuries. a Axial CT image demonstrates subtle hypoattenuation of the pancreatic body (arrow) representing a contusion with a small amount of peripancreatic fluid (asterisk) compatible with a grade I pancreatic injury. b Axial CT image demonstrates a major laceration of the pancreatic body (arrow) without involvement of the main pancreatic duct compatible with a grade II pancreatic injury. There is associated peripancreatic free fluid (asterisk). c Axial CT imaged demonstrates transection of the pancreatic tail (arrow) with associated peripancreatic free fluid (asterisk) compatible with grade III pancreatic injury. d Axial CT demonstrates transection of the pancreatic body and development of a large pancreatic pseudocyst (asterisk) representing a complication of a grade IV pancreatic injury
Early diagnosis and treatment is essential, as mortality associated with pancreatic injuries is approximately 20% [52, 53]. The integrity of the main pancreatic duct is the major deciding factor for operative versus non-operative management [50]. Grades I and II injuries are typically treated with conservative management, whereas grade III and greater injuries (typically associated with injury to the pancreatic duct) are usually treated surgically [54]. In select cases, MRCP may be used to evaluate the involvement and extent of injury to the main pancreatic duct, especially in cases where there are equivocal findings on CT. ERCP and stenting have also been used in select cases [55]. Fistula formation is the most common complication of pancreatic trauma. Other complications are pancreatitis, pseudocyst formation, abscess formation, and duct strictures [49, 56]. The role of interventional radiology in management of pancreatic trauma is limited and mainly involves percutaneous drainage of peripancreatic fluid collections, pseudocysts, and abscesses.
Thoracic Trauma
Thoracic trauma is associated with a high rate of mortality, in fact the overall mortality rate is approximately 10% [57]. The most common mechanism for blunt chest trauma is injury secondary to motor vehicle accident [58]. A wide spectrum of injuries included under the umbrella of blunt chest trauma. We will focus on injuries amenable to treatment by angioembolization which include chest wall injuries with associated pleural and lung parenchymal injuries. Blunt chest trauma is commonly associated with rib fractures which are seen in approximately 50% of patients with blunt chest trauma. Isolated non-displaced rib fractures are treated conservatively and have low morbidity and mortality [59]. Displaced rib fractures, however, are associated with pleural space and lung parenchymal injuries. Pleural-spaced injuries include pneumothorax and hemothorax. Pneumothorax is the collection of air in the pleural space, whereas, hemothorax is the collection of blood in the pleural space. Hemothorax measures higher density than simple fluid, typically between 35 and 70 HU. Hemothorax can originate from a variety of sources. Lung parenchymal injuries include contusions and lacerations. Pulmonary contusion represents alveolar hemorrhage and appears as patchy consolidation with subpleural sparing on CT. Pulmonary laceration is tearing of the pulmonary parenchyma and appears as traumatic pneumatocele or hematocele on CT [60].
Typically in isolated blunt chest trauma, a chest X-ray is the first imaging modality performed in order to rule out life-threatening injuries such as tension pneumothorax in a timely fashion. CT is used for further evaluation in hemodynamically stable patients, especially if chest tube output exceeds 200 mL/h [61]. Hemodynamically unstable are treated with emergent surgical thoracotomy. In stable patients with displaced rib fractures and hemothorax, careful evaluation for contrast extravasation is recommended as these patients may benefit from angioembolization of an intercostal artery (Fig. 10). Angioembolization can also be performed in patients with persistent hemothorax greater than 200 ml/h after chest tube placement [62]. Typically, the femoral artery is accessed, and thoracic aortogram is performed. Selective catheterization of the injured intercostal artery is performed using a Cobra or Sidewinder catheter to look for active extravasation. Then superselective embolization is performed with a coaxial microcatheter system using either particles, coils, gelfoam, or a combination of embolic agents.
Thoracic trauma. a Axial CT image of the chest demonstrates a small blush of contrast extravasation adjacent to the right lateral right fifth rib (arrow) with an associated large hematoma in the posterolateral right chest wall (star) compatible with an intercostal arterial hemorrhage. b DSA selective intercostal artery angiogram demonstrates a small blush of contrast extravasation arising from the lateral fifth intercostal artery (arrow). c DSA intercostal angiogram status post coil embolization of the right lateral fourth and sixth intercostal arteries as the fifth intercostal artery was unable to be selected due to vasospasm or occlusion
Conclusion
Trauma is a major cause of morbidity and mortality in the USA and requires a multidisciplinary approach with established protocols to streamline management of patients with solid organ trauma. The major decision in management of these patients is whether operative management is needed. In hemodynamically stable patients, CT provides essential information needed in order to guide management of these patients. AAST classification helps in evaluating the severity of injury and determining the further course of management. However, the current AAST classification does not account for active extravasation suggesting on-going active bleeding. Non-operative management has become the mainstay of patients with low-grade injuries. Interventional radiology’s role in management of patients with solid organ trauma is ever increasing. Angioembolization is an effective minimally invasive option in select patients with no indication for emergent laparotomy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) http://www.cdc.gov/injury/wisqars. Published 2007. Accessed January 10, 2017.
Raza M, Abbas Y, Devi V, Prasad KV, Rizk KN, Nair PP. Non operative management of abdominal trauma: a 10 years review. World J Emerg Surg. 2013;8:14.
Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. Usefulness of multidetector computed tomography for the initial assessment of blunt abdominal trauma patients. World J Surg. 2006;30(2):176–82.
Cox EF. Blunt abdominal trauma. A 5-year analysis of 870 patients requiring celiotomy. Ann Surg. 1984;199(4):467–74.
Marmery H, Shanmuganathan K, Alexander MT, Mirvis SE. Optimization of selection for nonoperative management of blunt splenic injury: comparison of MDCT grading systems. AJR Am J Roentgenol. 2007;189:1421–7.
•• Stassen NA, Bhullar I, Cheng JD, Crandall ML, Friese RS, Guillamondegui OD, et al. Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S294–300. The above reference outlines and highlights the most current guidelines for management of blunt splenic trauma
•• Stassen NA, Bhullar I, Cheng JD, Crandall M, Friese R, Guillamondegui O, et al. Nonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S288–93. The above reference outlines and highlights the most current guidelines for management of blunt hepatic injury
ACR appropriateness criteria: https://acsearch.acr.org/docs/69409/Narrative/
Korner M, Krotz MM, Degenhart C, Pfeifer K-J, Reiser MF, Lisenmaier U. Current role of emergency US in patients with major trauma. Radiographics. 2008;28:255–44.
Branney SW, Wolfe RE, Moore EE, et al. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J Trauma. 1995;39:375–80.
• Soto JA, Anderson SW. Multidetector CT of blunt abdominal trauma. Radiology. 2012;265:678–93. The above reference describes important MD-CT findings seen in blunt abdominal organ trauma
Anderson SW, Varghese JC, Lucey BC, et al. Bluntsplenictrauma: delayed- phase CT for differentiation of active hemorrhage from contained vascular injury inpatients. Radiology. 2007;243(1):88–95.
Peng MY, Parisky YR, Cornwell EE, Radin R, Bragin S. CT cystography versus conventional cystography in evaluation of bladder injury. AJR Am J Roentgenol. 1999;173(5):1269–72.
Chan DP, Abujudeh HH, Cushing GL, Novelline RA. CT cystography with multiplanar reformation for suspected bladder rupture: experience in 234 cases. AJR Am J Roentgenol. 2006;187(5):1296–302.
Orwig D, Federle MP. Localized clotted blood as evidence of visceral trauma on CT: the sentinel clot sign. AJR Am J Roentgenol. 1989;153(4):747–9.
Federle MP, Jeffrey RB. Hemoperitoneum studied by computed tomography. Radiology. 1983;148(1):187–92.
Levine CD, Patel UJ, Silverman PM, Wachsberg RH. Low attenuation of acute traumatic hemoperitoneum on CT scans. AJR Am J Roentgenol. 1996;166(5):1089–93.
Hassan R, Abd Aziz A, Md Ralib AR, Saat A. Computed tomography of blunt spleen injury: a pictorial review. Malays J Med Sci. 2011;18:60–7.
King H, Shumacker HB. Splenic studies. I. Susceptibility to infection after splenectomy performed in infancy. Ann Surg. 1952;136(2):239–42.
Renzulli P, Gross T, Schnüriger B, et al. Management of blunt injuries to the spleen. Br J Surg. 2010;97(11):1696–703.
• Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38(3):323–4. The above reference includes the most current AAST organ injury scaling for traumatic splenic and liver injuries
Kokabi N, Waqas S, Xing M, Harmouche E, Wilson K, Johnson JO, et al. Intra-abdominal solid organ injuries: an enhanced management algorithm. Can Assoc Radiol J. 2014;65:301–9.
Frandon J, Rodière M, Arvieux C, Michoud M, Vendrell A. BrouxC, et al. blunt splenic injury: outcomes of proximal versus distal and combined splenic artery embolization. Diagn Interv Imaging. 2014;95(9):825–31.
Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperativemanagement of blunt splenic injury: a 5-year experience. JTrauma. 2005;58(3):492–8.
Gaarder C, Dormagen JB, Eken T, Skaga NO, Klow NE, Pillgram-Larsen J, et al. Nonoperative management of splenic injuries: improved results with angioembolization. J Trauma. 2006;61(1):192–8.
Bessoud B, Denys A, Calmes JM, etal. Nonoperative management of traumatic splenic injuries: is there a role for proximal splenic artery embolization? AmJ Roentgenol 2006;186:779–785.
Raikhlin A, Baerlocher MO, Asch MR, et al. Imaging and transcatheter arterial embolization for traumatic spleen icinjuries: review of the literature. Can J Surg. 2008;51:464–72.
Wu SC, Chen RJ, Yang AD, etal. Complications associated with embolization in the treatment of blunt splenic injury. World J Surg 2008; 32:476–482.
• Imbrogno BF, Ray CE. Splenic artery embolization in blunt trauma. Semin Interv Radiol. 2012;29(2):147–9. The above reference describes the most current indications and technique for splenic artery embolization in blunt trauma
Schnüriger B, Inaba K, Konstantinidis A, Lustenberger T, Chan LS, Demetriades D. Outcomes of proximal versus distal splenic artery embolization after trauma: a systematic review and meta-analysis. J Trauma. 2011;70:242–60.
Steichen FM. Hepatic trauma in adults. Surg Clin North Am. 1975;55:387–407.
Yoon W, Jeong YY, Kim JK, et al. CT in blunt liver trauma. Radiographics. 2005;25:87–104.
Patten RM, Spear RP, Vincent LM, Hesla RB, Jurkovich GJ. Traumatic laceration of the liver limited to the bare area: CT findings in 25 patients. AJR Am J Roentgenol. 1993;160(5):1019–22.
Fleming KW, Lucey BC, Soto JA, Oates ME. Posttraumatic bile leaks: role of diagnostic imaging and impact on patient outcome. Emerg Radiol. 2006;12(3):103–7.
Salazar GMM, Walker TG. Evaluation and management of acute vascular trauma. Tech Vasc Interv Radiol. 2009;12:102–16.
Schwartz RA, Teitelbaum GP, Katz MD, Pentecost MJ. Effectiveness of transcatheter embolization in the control of hepatic vascular injuries. J Vasc Interv Radiol. 1993;4(3):359–65.
Kandarpa K, Machan L, editors. Handbook of interventional radiologic procedures. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
Alonso RC, Nacenta SB, Martinez PD, et al. Kidney in danger: CT findings of blunt and penetrating renal trauma. Radiographics. 2009;29(7):2033–53.
Ramchandani P, Buckler PM. Imaging of genitourinary trauma. AJR Am J Roentgenol. 2009;192(6):1514–23.
Santucci RA, McAninch JW, Safir M, Mario LA, Service S, Segal MR. Validation of the American Association for the Surgery of Trauma organ injury severity scale for the kidney. J Trauma. 2001;50(2):195–200.
• Moore EE, Shackford SR, Pachter HL, et al. Organ injury scaling: spleen, liver, kidney. J Trauma. 1989;29(12):1664–6. The above reference outlines and describes the most current AAST organ injury scaling for traumatic renal injuries
Harris AC, Zwirewich CV, Lyburn ID, Marchinkow LO. CT findings in blunt renal trauma. Radiographics. 2001;21:S201–14.
Sauk S, Zuckerman DA. Renal artery embolization. Semin Interv Radiol. 2011;28:396–406.
• Mani N, Kim L. Role of interventional radiology in urologic tract trauma. Semin Interv Radiol. 2011;28:415–23. The above reference outlines the most current indications and technique for IR management of traumatic kidney injuries
Cirillo RL, Koniaris LG. Detecting blunt pancreatic injuries. J Gastrointest Surg. 2002;6:587–98.
Kao LS, Bulger EM, Parks DL, Byrd GF, Jurkovich GJ. Predictors of morbidity after traumatic pancreatic injury. J Trauma. 2003;55:898–905.
Venkatesh SK, Wan JM. CT of blunt pancreatic trauma: a pictorial essay. Eur J Radiol. 2008;67:311–20.
Gupta A, Stuhlfaut JW, Fleming KW, Lucey BC, Soto JA. Blunt trauma of the pancreas and biliary tract: a multimodality imaging approach to diagnosis. Radiographics. 2004;24:1381–95.
Madiba TE, Mokoena TR. Favourable prognosis after surgical drainage of gunshot, stab, or blunt trauma of the pancreas. Br J Surg. 1995;82:1236–9.
Linsenmaier U, Wirth S, Reiser M, Körner M. Diagnosis and classification of pancreatic and duodenal injuries in emergency radiology. Radiographics. 2008;28:1591–601.
Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30(11):1427–9.
Heitsch RC, Knutson CO, Fulton RL, Jones CE. Delineation of critical factors in the treatment of pancreatic trauma. Surgery. 1976;80(4):523–9.
Jones RC. Management of pancreatic trauma. Ann Surg. 1978;187:555–64.
Fisher M, Brasel K. Evolving management of pancreatic injury. Curr Opin Crit Care. 2011;17:613–7.
Canty TG, Weinman D. Treatment of pancreatic duct disruption in children by an endoscopically placed stent. J Pediatr Surg. 2001;36:345–8.
Bradley EL, Young PR, Chang MC, Allen JE, Baker CC, Meredith W, et al. Diagnosis and initial management of blunt pancreatic trauma: guidelines from a multiinstitutional review. Ann Surg. 1998;227:861–9.
The American College of Surgeons Committee on Trauma Leadership. In: Clark DE, Fantus RJ, editors. National Trauma Data Bank (NTDB) annual report. Chicago: Ill: American College of Surgeons; 2007. p. 1–64.
Report on injuries in America: all unintentional injuries, 2005. Available at: http://www.nsc.org/library/report_table_1.htm. Accessed December 9, 2007.
Livingston DH, Haurer CJ. Trauma to the chest wall and lung. In: Moore EE, Feliciano DV, Mattox KL, editors. Trauma. 5th ed. Philadelphia, Pa: McGraw-Hill; 2004. p. 507–37.
Kaewlai R, Avery LL, Asrani A, Novelline RA. Multidetector CT of blunt thoracic trauma. Radiographics. 2008;28:1555–70.
Exadaktylos AK, Sclabas G, Schmid SW, Schaller B, Zimmermann H. Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with “normal” chest radiograph? J Trauma. 2001;51:1173–6.
Hagiwara A, Yanagawa Y, Kaneko N, Takasu A, et al. Indications for transcatheter arterial embolization in persistent hemothorax caused by blunt trauma. J Trauma. 2008;65:589–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Frank Kowalkowski Jr., Gurpreet Sandhu, and Indravadan Patel declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Vascular Interventional Radiology
Rights and permissions
About this article
Cite this article
Kowalkowski, F., Sandhu, G. & Patel, I.J. Role of Interventional Radiology in Solid Organ Trauma. Curr Trauma Rep 3, 212–222 (2017). https://doi.org/10.1007/s40719-017-0091-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40719-017-0091-1