Abstract
Purpose of review
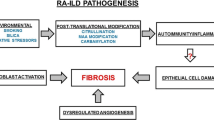
Rheumatoid arthritis–associated interstitial lung disease (RA-ILD) is one of the most serious extraarticular RA manifestations. RA-ILD is associated with worse physical function, lower quality of life, and increased mortality. RA-ILD is comprised of heterogeneous subtypes characterized by inflammation and fibrosis. Diagnosis can be difficult since the presentation of RA-ILD is characterized by non-specific symptoms and imaging findings. Management of RA-ILD is also challenging due to difficulty in precisely measuring pulmonary disease activity and response to treatment in patients who may also have articular inflammation. We provide a current overview of RA-ILD focusing on prevalence, risk factors, and treatment.
Recent findings
Research interest in RA-ILD has increased in recent years. Some studies suggest that RA-ILD prevalence may be increasing; this may be due to underlying biologic drivers or increases in imaging and recognition. Novel RA-ILD risk factors include the MUC5B promoter variant, articular disease activity, autoantibodies, and biomarkers of damaged pulmonary parenchyma. Treatment should focus on controlling RA disease activity, which emerging data suggest may reduce RA-ILD risk. Immunomodulatory and anti-fibrotic drugs may also treat RA-ILD.
Summary
RA-ILD is an underrecognized and serious manifestation of RA, but important progress is being made in identifying risk factors and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with rheumatoid arthritis (RA) have excess respiratory mortality compared with the general population [1•, 2, 3]. RA-associated interstitial lung disease (RA-ILD) is one of the most common and serious extraarticular manifestations of RA. Median survival after RA-ILD diagnosis is only 3–7 years, which is markedly reduced compared with RA patients without ILD and the general population [4, 5••, 6]. Patients with RA-ILD have substantial health care costs and interactions; 72% have an all-cause inpatient admission and 76% have an all-cause emergency department visit [7••]. Patients with RA-ILD also have reduced quality of life and physical function, increased respiratory symptoms, and a more severe RA disease as measured by the Multi-Dimensional Health Assessment Questionnaire (MDHAQ) score and total swollen joint count [8].
RA-ILD is distinguished by subtypes by histologic and/or imaging features [9•, 10]. The most common subtype is usual interstitial pneumonia (UIP), characterized by fibrosis, and typically has a more aggressive clinical course [11•]. Non-specific interstitial pneumonia (NSIP) is also common in patients with RA and is typically characterized by parenchymal inflammation [11•]. Some patients have both inflammatory and fibrotic characteristics that may make it difficult to distinguish between UIP and NSIP, and, perhaps, some patients transition from an inflammatory to a fibrotic form of NSIP [11•]. Other less common RA-ILD subtypes include lymphocytic interstitial pneumonia (LIP), acute interstitial pneumonia (AIP), organizing pneumonia (OP), desquamative interstitial pneumonia (DIP), and respiratory bronchiolitis ILD (RB-ILD) [11•]. Since routine chest computed tomography (CT) imaging is becoming more widely utilized, interstitial lung abnormalities (ILA) are commonly detected and may represent a subclinical RA-ILD form that may progress to clinically significant RA-ILD in some [8, 12•]. Besides RA-ILD, patients with RA may have other pulmonary manifestations including airway disease, pleuritis, nodules, pulmonary vascular disease, bronchiectasis, bronchiolitis, and secondary Sjogren’s syndrome [9•]. Smoking is an established risk factor for RA development and lung diseases such as ILD and emphysema, and this may explain lung abnormalities in some patients [13••]. Finally, patients with RA may be at an increased risk for pneumonia and drug side effects causing pneumonitis [14]. Therefore, lung abnormalities are a relatively common clinical feature of patients with RA with significant morbidity and mortality. This review focuses on RA-ILD given increased research interest in identifying risk factors and treatment for this pulmonary manifestation of RA.
Despite the expanding options of biologic and targeted disease-modifying anti-rheumatic drugs (DMARDs), the prevalence of RA-ILD may be increasing [7••]. Rheumatologists, pulmonologists, and other clinicians are confronted with the management of patients with RA-ILD who may have combinations of articular and pulmonary involvement. In this review, we will provide an update on the prevalence, risk factors, and pharmacologic management of RA-ILD.
Prevalence of RA-ILD
The prevalence of RA-ILD ranges widely in previous research, likely due to varying methodologies in detection [4, 5••, 7••, 12•, 15,16,17, 18•, 19••, 20,21,22,23,24]. Some studies identified RA-ILD through clinical detection (from any means such as symptoms, screening, or incidental findings), with prevalence estimates ranging from 2 to 8%. However, these methods may only identify the most severe forms of RA-ILD and likely underestimate prevalence [4, 17]. Other studies used administrative databases to identify RA-ILD through billing codes or chest imaging/procedures and estimate prevalence from 8 to 20% [5••, 7••, 25,26,27]. However, the evaluation of RA-ILD may incur a billing code even in negative cases, thus resulting in erroneously increased prevalence.
The true prevalence of ILD in RA is not established, and estimates vary widely related to inclusion of subclinical ILD in sensitive methods or exclusion of true, but milder cases, in stringent methods. Research reviews of the images of chest CT scans obtained through clinical care are another method to increase sensitivity of detection, with ILA or RA-ILD prevalence of 10–30% [19••, 21]. In these studies, patients with RA-ILD that did not have chest imaging performed would have gone undetected. Conversely, a proportion of those with ILA may never progress to clinically significant lung disease, or the pulmonary presentations may relate to other causes such as infection, drug toxicity, and smoking. Finally, other studies performed prospective recruitment of patients with RA to obtain chest imaging as part of the research protocol to detect RA-ILD in asymptomatic individuals [12•, 15, 16] or among those with high suspicion of lung disease, with RA-ILD prevalence ranging from 10 to 50% [28]. These difficulties in understanding prevalence of RA-ILD may be overcome by a clear consensus on screening strategy and RA-specific classification criteria for clinical practice.
A recent nationwide US study used pharmacy claims data and found that RA-ILD prevalence was increasing [7••]. Prevalence of RA-ILD increased from 3.2 cases per 100,000 in the general population in 2003 to 6.0 cases per 100,000 in the general population in 2014 (denominator of all RA patients was not reported) [7••]. This is in contrast to improvements in survival of RA patients compared with the general population over the same time period following the introduction of biologic DMARDs [29]. Increasing prevalence of RA-ILD may be due to many factors including as follows: a true increase perhaps due to changes in the underlying epidemiology of RA or its treatment, increased recognition or billing practices from clinicians, increase in detection from advanced chest imaging, or increasing longevity of RA patients. Future investigations should focus on replicating this finding and distinguishing the reasons for possible increased prevalence of RA-ILD. A screening strategy for RA-ILD among those with RA has already been detailed, and investigations concerning screening implementation should be a high research priority [9•].
Risk factors for RA-ILD
Most studies have examined risk factors for RA-ILD as an overall entity, rather than RA-ILD subtypes. As previously discussed, detection of RA-ILD also varies widely by different research methods. These nuances could explain discrepancies in research studies attempting to identify risk factors for RA-ILD. Nevertheless, there is a growing list of identified RA-ILD risk factors (Table 1).
Demographic factors associated with RA-ILD include male sex and older age [6, 30,31,32, 33•]. Since most patients with RA are women, the finding of male sex may be somewhat paradoxical, but is not explained by possible confounding factors including cigarette smoking. Men have over a 2-fold increased risk of RA-ILD compared with women [6]. Future studies should focus on characterizing this sex difference within RA. Older age has also been associated with RA-ILD risk. This finding also deserves dedicated research on how immunosenescence, accelerated aging, or telomere shortening may be associated with RA-ILD risk.
Cigarette smoking has also been implicated as a lifestyle risk factor for RA-ILD [6, 30, 31, 36]. As already mentioned, smoking is a risk factor for RA, and it appears that smoking after RA onset and current smoking also impart risk for RA-ILD. While cigarette smoking has long been associated with poor pulmonary outcomes in many diseases, this finding suggests that at least some RA-ILD risk could be modifiable. Research studies may focus on gene-smoking interactions, which could further delineate some of the mechanisms of RA pathogenesis.
Several clinical RA factors are associated with RA-ILD. Elevations of rheumatoid factor (RF) and anti-citrullinated protein antibodies are risk factors for RA-ILD [6, 30, 31, 36]. Seropositivity for these antibodies portends a more severe articular course and higher risk of extraarticular manifestations including RA-ILD. RA severity factors including prednisone use [31, 45, 46] and rheumatoid nodules [33•] are associated with an increased RA-ILD risk, as have elevated erythrocyte sedimentation rate (ESR) [31, 32, 33•] and longer RA duration [40] are additional RA-ILD risk factors. Articular disease activity was recently associated with incident RA-ILD in a prospective study [19••]. Specifically, moderate to high disease activity was associated with a 2-fold increased risk for RA-ILD compared with low disease activity or remission [19••]. This finding suggests that articular involvement may be a marker of not only systemic inflammation but also ongoing pulmonary inflammation, hence suggesting that disease control through a treat-to-target strategy could delay or even prevent RA-ILD onset. However, other prospective observational and interventional studies are needed to confirm these findings. The potential role of DMARDs in RA-ILD onset is discussed later.
Recently, a large multinational study implicated the MUC5B promoter variant with RA-ILD risk [34••]. MUC5B is a type of mucin that is secreted and glycosylated into pulmonary mucosa as a key contributor to the lubricating and viscoelastic properties of airways and alveoli. This variant of the MUC5B gene (G>T at the rs35705950 single-nucleotide polymorphism) has also been associated with an increased risk for several chronic respiratory diseases, including idiopathic pulmonary fibrosis [51], ILD [52], and chronic obstructive pulmonary disease (COPD) [53]. In individuals with the promoter variant, excess MUC5B secretion impairs mucosal host defense, resulting in overexuberant lung injury from inhaled substances, inflammation, and fibrosis. The MUC5B promoter variant increases the risk for ILD by 3-fold among patients with RA and is specific for the UIP subtype of RA-ILD that is most prone to fibrosis and a severe disease course [34••]. While other genes have also been implicated in RA-ILD, none is as strongly associated as the MUC5B promoter variant [35]. This important finding may set the stage to understand the role of potential perturbations to pulmonary mucosa at airways, such as microbiome and inhalants. Mechanistic studies related to this gene will deepen the understanding of RA-ILD, and clinical studies should also incorporate this into prediction modeling prior to possible clinical application.
Besides RF and anti-citrullinated protein antibodies (ACPAs), other autoantibodies have been investigated for contributions to RA-ILD risk and are currently only available for research purposes. Fine specificity ACPAs including anti-citrullinated alpha-enolase peptide 1 (CEP-1) [37•, 38] and anti-citrullinated heat shock protein 90 (HSP90) [43, 44] have been associated with RA-ILD, supporting the role of ACPAs in RA-ILD pathogenesis [36]. Peptidylarginine deiminase (PAD) isozymes catalyze citrullination, and anti-PAD3/4 have recently been associated with RA-ILD [41•]. Carbamylation is a process similar to citrullination except that it involves the irreversible modification of lysine to homocitrulline without involving enzymes [54]. Anti-carbamylated protein (CarP) antibodies have also been associated with RA-ILD risk [39•]. Malondialdehyde and acetaldehyde are products of oxidative stress that are known to be highly immunogenic, profibrotic, and proinflammatory [55, 56]. Anti-malondialdehyde-acetaldehyde (anti-MAA) antibodies were recently associated with an increased RA-ILD risk [42•]. Anti-IL-1α [47] has also been associated with RA-ILD risk. It is possible that dysregulated post-translational modification of proteins may be important in the development of RA-ILD. Future studies should investigate how citrullination, carbamylation, and MAA may impart RA-ILD risk.
Finally, other non-antibody biomarkers such as LDH [57], CA-125 [58], matrix metalloproteinases [30, 49, 59], plasma surfactant protein D [30], interferon-γ-inducible protein 10 (IP-10)/CXCL10 [49], pulmonary and activation-related chemokine (PARC) [30], fibronectin [48•], and IL-18 [50] were found to be associated with an increased risk of RA-ILD among patients with RA. A model that included demographic, clinical risk factors and biomarkers (MMP7, PARC, surfactant protein D) was able to classify presence of RA-ILD with high accuracy [30], and future studies should consider the utility of incorporating these markers into clinical care for RA-ILD screening.
Treatment of RA-ILD
The treatment of RA can potentially delay or prevent the onset of RA-ILD. We advocate for managing RA articular disease with DMARD therapy, including those with ILD. In patients with progressive ILD despite optimal therapy for RA, one can consider changing the immunosuppressive agent or adding anti-fibrotic therapy.
To date, there are no medications specifically approved by the US Food and Drug Administration (FDA) for treatment of RA-ILD. However, nintedanib is approved for connective tissue disease–associated ILD, which could encompass RA-ILD [60••]. Pirfenidone was recently approved for “unclassifiable ILD,” which may also include RA-ILD [61••]. Most of the current evidence available is drawn from observational studies, case reports, and case series. It may be most beneficial to treat patients with RA-ILD presenting with rapid disease progression and higher extent of lung injury in order to stabilize lung function [62]. Next, we outline the treatment options for RA-ILD as well as best available evidence.
Impact of glucocorticoids and non-biologic and biologic DMARDs on RA-ILD onset
The association of DMARDs with RA-ILD onset is controversial. Some studies identified glucocorticoid use as a risk factor [31, 45, 46], but this could be a marker of RA disease activity, which is also a risk factor for RA-ILD. The possible association of methotrexate with RA-related lung disease is controversial [63]. Pneumonitis is a rare but potentially devastating adverse effect of methotrexate, typically characterized by acute presentation of fever, cough, and chest imaging abnormalities that often resolves with methotrexate discontinuation [64]. A meta-analysis that included six placebo-controlled trials of methotrexate in patients with inflammatory diseases including RA showed no increased risk of pulmonary adverse events, but the sample size was small (504 respiratory adverse events among 1630 participants) and follow-up was short [65]. Another recent observational study (n = 2701) found no evidence that methotrexate was associated with incident ILD in RA, and there was a suggestion that methotrexate may delay the onset of ILD [33•]. A large placebo-controlled trial of methotrexate performed among patients with cardiovascular disease (n = 4786) recently showed a statistically significant increased risk for pulmonary adverse events, but most events were not severe, and patients with RA were excluded [66•].
Clinicians are often confronted with conflicting evidence of the potential impact of DMARDs on RA-ILD risk. For example, clinical trials suggested a potential increase of COPD exacerbations for patients with RA treated with abatacept; follow-up studies found no pulmonary safety concerns and other studies suggested potential benefit of abatacept on RA-ILD [67•]. A recent meta-analysis suggested that leflunomide, tumor necrosis factor inhibitors, rituximab, and tocilizumab may induce pneumonitis or worsen preexisting RA-ILD [68]. However, this finding could be subject to confounding by indication since many patients with RA-ILD are treated with rituximab or could be explained by channeling away from methotrexate in patients suspected to have RA-ILD. Given the high prevalence of chest imaging abnormalities in patients with RA, clinicians must weigh how DMARDs may impact possible progression to clinically severe RA-ILD when choosing medications to treat articular inflammation. Therefore, the pulmonary safety of DMARDs should be a high research priority.
Rheumatologists should readily involve pulmonary colleagues when interpreting possible pulmonary imaging or functional abnormalities to risk stratify patients. A multidisciplinary approach is central in patients with RA that may have several organ systems involved in order to accurately assess disease activity, risks and benefits of medications, and response to treatment. Besides rheumatologists and pulmonologists, this may also include primary care providers, pulmonary rehabilitation, chest radiologists, and pathologists among other specialists. Managing patients with RA-ILD can be particularly challenging since patients may have articular inflammation, pulmonary involvement, or both throughout their disease course.
We now focus on treatment of pulmonary manifestations of RA-ILD.
Immunosuppressive drugs
Glucocorticoids
Glucocorticoids should no longer be considered a first-line therapy in all patients with RA-ILD. However, they may be considered during severe exacerbations or when quick onset of action is desired. Glucocorticoids are no longer used for fibrotic forms of lung disease based on results in IPF showing worsened outcomes [69]. The inflammatory RA-ILD subtypes of RA-ILD, particularly NSIP and OP, may be steroid-responsive [70]. Glucocorticoid therapy is generally started at a prednisone equivalent of 0.5–1 mg/kg/day, or in the case of fulminant disease, pulse dose intravenous methylprednisolone 1–2 g per day. Glucocorticoids should be given with careful monitoring and management of side effects, particularly infection given the propensity for pneumonia or other opportunistic infections. Pneumocystis pneumonia prophylaxis should be considered in patients with RA-ILD who will be on glucocorticoids (thresholds of dose/duration of glucocorticoid for staring prophylaxis are not specifically established in RA-ILD) [71]. Studies have shown that glucocorticoids are associated with a 4-fold increased risk of serious infection in older adults with RA [72]. Glucocorticoid-induced osteoporosis is another important adverse event requiring careful screening and follow-up, particularly given that RA itself is a risk factor for osteoporosis [73]. Glucocorticoid treatment is the most common secondary cause of osteoporosis [74].
Mycophenolate mofetil
Most of the evidence for mycophenolate mofetil (MMF) comes from observational studies in CTD-ILD, particularly systemic sclerosis, in the demonstration of disease stabilization [75, 76]. MMF has also been shown to have a superior safety profile compared with oral cyclophosphamide in scleroderma-ILD [77]. In a small study with CTD-ILD patients (n = 10), MMF was associated with symptom improvement and imaging/pulmonary function test improvement (composite of lung volumes or diffusion capacity) [78]. However, these studies are limited by a small sample size; larger controlled studies will be needed to confirm the findings. MMF has relatively poor efficacy for articular manifestations of RA, and a concomitant DMARD may be needed to control disease activity in joints [79].
Rituximab
Rituximab, a B cell–depleting anti-CD20 antibody, has shown promise in the treatment of CTD-ILD. Small studies demonstrated stable or improved lung function with rituximab therapy in patients with scleroderma-ILD or dermatomyositis-ILD [80, 81]. Rituximab has also been used as rescue therapy for severe and progressive CTD-ILD [82]. In RA patients with ILD, an observational study reporting the experience of using rituximab over 10 years demonstrated that it was relatively safe and did not lead to ILD progression [83•]. A study performed in the British Society for Rheumatology Biologics Register for RA compared outcomes of RA-ILD patients on rituximab (n = 43) with those on a TNFi (n = 309). This study demonstrated lower mortality in patients treated with rituximab vs. those receiving TNFi [84•]. Rituximab has proven efficacy for articular involvement, so it may be considered in patients with simultaneous inflammatory activity in lungs and joints. Rituximab and mycophenolate mofetil may also be considered in combination for some patients.
Cyclophosphamide
Cyclophosphamide has been used to treat many types of ILD, with studies demonstrating lung function stabilization of fibrosis [85]. A recent Cochrane systematic review of cyclophosphamide in the treatment of connective tissue disease–related ILD (CTD-ILD), using four trials (n = 495), demonstrated that cyclophosphamide led to a small improvement in forced vital capacity (FVC) but not DLCO; there was no difference between cyclophosphamide and MMF. Given the toxicity profile of cyclophosphamide, it is reasonable to reserve it for those with the most rapidly progressing or refractory disease. While not typically considered for articular disease activity due to its side effect profile, it may be considered in patients with severe or refractory inflammation in both lungs and joints.
Azathioprine
There are no controlled studies of azathioprine in RA-ILD, but there is generally less enthusiasm for use of azathioprine in any type of ILD after the results of the PANTHER-IPF trial. Based on evidence in IPF, the combination of glucocorticoids and azathioprine was thought to improve survival, but results of the PANTHER-IPF trial in 2012 abruptly altered this management approach [86]. The PANTHER-IPF trial was terminated early due to higher mortality and increased hospitalization rates in the combined prednisone, azathioprine, and N-acetylcysteine arm compared with placebo, with many of the complications attributed to pulmonary infection [87]. However, in a retrospective cohort study of CTD-ILD (n = 54) in 2016, azathioprine was shown to stabilize pulmonary function over time and comparable incidence of adverse outcomes as occurred in the MMF group in the same study [88]. Azathioprine may still be considered in some, such as articular involvement warranting non-biologic DMARDs and contraindication to other drugs.
Other immunomodulatory drugs
Tocilizumab is an interleukin-6 receptor (IL-6R) antibody and is approved for the treatment of RA. A small retrospective study of 28 RA-ILD patients receiving tocilizumab demonstrated potential stabilization of pulmonary disease and an acceptable safety profile [89•]. Conversely, early RCTs and case reports have suggested association between incident ILD with tocilizumab treatment [90]. A recent meta-analysis of observational studies among patients with RA suggested a possible relationship with tocilizumab and worsening of RA-ILD [68]. Further large prospective studies would be necessary to elucidate the efficacy and safety of tocilizumab in RA-ILD.
Abatacept is a soluble chimeric fusion protein of cytotoxic T lymphocyte antigen 4 (CTLA-4)-Ig, blocking the T cell co-stimulation in RA. An open-label study of 63 RA-ILD patients in Spain showed that the majority of patients achieved symptom and PFT stability, with 20–25% of patients experiencing improvement [91•]. A phase 2 open-label clinical trial is currently enrolling patients to study the safety of abatacept among patients with RA-ILD (AbatacePt in Rheumatoid Arthritis-ILD [APRIL]) [92].
There are currently inconclusive data on the pulmonary safety of Janus kinase (JAK) inhibitors. Low rates of ILD have been reported from the RA clinical development programs and post-marketing surveillance studies of tofacitinib and baricitinib [93]. A small open-label trial in 18 patients with amyopathic dermatomyositis–associated ILD demonstrated improvement in pulmonary function and survival in the tofacitinib group compared with historic controls [94]. A randomized, controlled, open-label phase IV clinical trial comparing efficacy of tofacitinib vs. methotrexate in RA-ILD (PULMORA) has not yet started recruitment [95].
Anti-fibrotic drugs
Nintedanib
Nintedanib inhibits multiple tyrosine kinases and is approved by the US FDA for IPF, systemic sclerosis–associated ILD, and chronic fibrosing ILDs with a progressive phenotype, which could include RA-ILD. Nintedanib has been shown to be efficacious in progressive fibrotic ILDs (n = 663) in a randomized, double-blind, placebo-controlled, phase 3 trial (INBUILD trial) with stringent inclusion criteria to demonstrate reduction in disease progression [60••]. This trial included 89 (13%) patients with RA-ILD. Patients in the nintedanib arm had a slower rate of decline in FVC compared with placebo over a 52-week period, with a comparable benefit seen in the treatment of IPF (INPULSIS trial) [96]. Among patients with CTD-ILD, the benefit was more prominent in the UIP subtype vs. other subtypes. Even though there are improvements compared with placebo, the magnitude of clinical benefit is not yet established. Therefore, nintedanib can be considered in patients with RA-ILD. Gastrointestinal side effects may limit its use in some patients.
Pirfenidone
Pirfenidone, an anti-fibrotic agent with anti-inflammatory properties, has demonstrated efficacy in IPF by ameliorating pulmonary function decline and decreasing mortality in randomized controlled trials [97]. It has been approved by the US FDA for the treatment of mild or moderate IPF and “unclassifiable ILD,” which could include IPAF and RA-ILD; it has demonstrated a slower decline in FVC compared with placebo [61••]. Rash and gastrointestinal side effects, such as nausea, are common limiting factors in it use. An open-label, phase 2 study in patients with systemic sclerosis–associated ILD demonstrated tolerability of pirfenidone, even in those taking concurrent MMF [98]. Treatment of RA-ILD using pirfenidone is currently being investigated in an ongoing phase 2 clinical trial (TRAIL1) [99]. Similar to nintedanib, pirfenidone can be considered in patients with RA-ILD, though the magnitude of clinical benefit is unclear, and side effects are common. While not yet directly investigated, it may be reasonable to treat fibrotic subtypes of RA-ILD such as UIP with anti-fibrotic drugs.
Lung transplantation
Lung transplantation can be considered in patients with end-stage RA-ILD who fail to respond to therapy. There are limited data available for outcomes in lung transplant in RA-ILD patients. In a retrospective review of 10 RA-ILD patients compared with 53 IPF patients who underwent lung transplantation, 1-year survival was comparable between the two groups (67% vs. 69%, respectively). The study also found a significant improvement in quality of life related to respiratory symptoms [100]. The candidacy for lung transplant in RA-ILD needs to be carefully evaluated given common RA comorbidities such as osteoporosis and extrapulmonary manifestations such as atherosclerotic cardiovascular disease.
Ongoing trials
The ongoing trials evaluating RA-ILD treatment are outlined in Table 2. These include abatacept, tofacitinib, and pirfenidone.
Conclusions
Pulmonary involvement in RA is relatively common and there has been a growing interest in RA-ILD over the last few years. Many challenges should be acknowledged: lack of a uniform screening strategy that in turn guides the prevalence estimates, unclear natural history in terms of timing of onset and rate of progression, and optimal treatment approaches. Despite these challenges, progress has been made in identifying several novel risk factors. These include the MUC5B promoter variant [34••], moderate to high articular disease activity [19••], autoantibodies such as anti-CarP [39•] and anti-MAA [42•], and biomarkers such as MMP7, PARC, and surfactant protein D [30]. While there are many approved DMARDs and biologic agents used to treat RA, the safety and efficacy of many of these agents in RA-ILD still needs to be evaluated. With some encouraging data in large cohorts on rituximab stabilizing lung disease in RA-ILD, and RCT data with the use of anti-fibrotics, a novel approach of combining selected immunosuppressive and anti-fibrotic therapy will need to be evaluated in a larger clinical trial [61••]. While important gaps in the optimal treatment remain, tremendous progress in distinguishing subtypes of RA-ILD, risk factors for its development, pathogenesis, and management have has been made over the last few years.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Yoshida K, Lin TC, Wei M, Malspeis S, Chu SH, Camargo CA, et al. The roles of post-diagnosis accumulation of morbidities and lifestyle changes on excess total and cause-specific mortality risk in rheumatoid arthritis. Arthritis care res (Hoboken). 2019. https://doi.org/10.1002/acr.24120.A large study with lengthy follow-up demonstrating accumulation of morbidities and excess respiratory mortality for patients with seropositive RA.
Sparks JA, Chang SC, Liao KP, Lu B, Fine AR, Solomon DH, et al. Rheumatoid arthritis and mortality among women during 36 years of prospective follow-up: results from the nurses’ health study. Arthritis Care Res (Hoboken). 2016;68(6):753–62. https://doi.org/10.1002/acr.22752.
England BR, Sayles H, Michaud K, Caplan L, Davis LA, Cannon GW, et al. Cause-specific mortality in male US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68(1):36–45. https://doi.org/10.1002/acr.22642.
Bongartz T, Nannini C, Medina-Velasquez YF, Achenbach SJ, Crowson CS, Ryu JH, et al. Incidence and mortality of interstitial lung disease in rheumatoid arthritis: a population-based study. Arthritis Rheum. 2010;62(6):1583–91. https://doi.org/10.1002/art.27405.
•• Hyldgaard C, Hilberg O, Pedersen AB, Ulrichsen SP, Lokke A, Bendstrup E, et al. A population-based cohort study of rheumatoid arthritis-associated interstitial lung disease: comorbidity and mortality. Ann Rheum Dis. 2017;76(10):1700–6. https://doi.org/10.1136/annrheumdis-2017-211138.A large nationwide study investigating incidence and prevalance of RA-ILD in relation to RA onset.
Kelly CA, Saravanan V, Nisar M, Arthanari S, Woodhead FA, Price-Forbes AN, et al. Rheumatoid arthritis-related interstitial lung disease: associations, prognostic factors and physiological and radiological characteristics--a large multicentre UK study. Rheumatology (Oxford). 2014;53(9):1676–82. https://doi.org/10.1093/rheumatology/keu165.
•• Raimundo K, Solomon JJ, Olson AL, Kong AM, Cole AL, Fischer A, et al. Rheumatoid arthritis-interstitial lung disease in the United States: prevalence, incidence, and healthcare costs and mortality. J Rheumatol. 2019;46(4):360–9. https://doi.org/10.3899/jrheum.171315.A nationwide study showing that RA-ILD has high health care costs and mortality and that prevalence may be increasing over calendar time.
Doyle TJ, Dellaripa PF, Batra K, Frits ML, Iannaccone CK, Hatabu H, et al. Functional impact of a spectrum of interstitial lung abnormalities in rheumatoid arthritis. Chest. 2014;146(1):41–50. https://doi.org/10.1378/chest.13-1394.
• Esposito AJ, Chu SG, Madan R, Doyle TJ, Dellaripa PF. Thoracic manifestations of rheumatoid arthritis. Clin chest Med. 2019;40(3):545–60. https://doi.org/10.1016/j.ccm.2019.05.003.Details a possible screening algorithm to detect RA-ILD.
Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–48. https://doi.org/10.1164/rccm.201308-1483ST.
• Yamakawa H, Sato S, Tsumiyama E, Nishizawa T, Kawabe R, Oba T, et al. Predictive factors of mortality in rheumatoid arthritis-associated interstitial lung disease analysed by modified HRCT classification of idiopathic pulmonary fibrosis according to the 2018 ATS/ERS/JRS/ALAT criteria. J Thorac Dis. 2019;11(12):5247–57. https://doi.org/10.21037/jtd.2019.11.73.Investigated the association of RA-ILD subtypes with mortality.
• Dong H, Julien PJ, Demoruelle MK, Deane KD, Weisman MH. Interstitial lung abnormalities in patients with early rheumatoid arthritis: a pilot study evaluating prevalence and progression. Eur J Rheumatol. 2019;6(4):193–8. https://doi.org/10.5152/eurjrheum.2019.19044 A small prospective longidinal study investigating prevalence and progression of subclinical ILA among patients with RA.
•• Liu X, Tedeschi SK, Barbhaiya M, Leatherwood CL, Speyer CB, Lu B, et al. Impact and timing of smoking cessation on reducing risk of rheumatoid arthritis among women in the nurses’ health studies. Arthritis care res (Hoboken). 2019;71(7):914–24. https://doi.org/10.1002/acr.23837 The large observational study suggests that smoking cessation may reduce risk for seropositive RA.
Wolfe F, Caplan L, Michaud K. Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia: associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy. Arthritis Rheum. 2006;54(2):628–34. https://doi.org/10.1002/art.21568.
Gabbay E, Tarala R, Will R, Carroll G, Adler B, Cameron D, et al. Interstitial lung disease in recent onset rheumatoid arthritis. Am J Respir Crit Care Med. 1997;156(2 Pt 1):528–35. https://doi.org/10.1164/ajrccm.156.2.9609016.
Habib HM, Eisa AA, Arafat WR, Marie MA. Pulmonary involvement in early rheumatoid arthritis patients. Clin Rheumatol. 2011;30(2):217–21. https://doi.org/10.1007/s10067-010-1492-5.
Koduri G, Norton S, Young A, Cox N, Davies P, Devlin J, et al. Interstitial lung disease has a poor prognosis in rheumatoid arthritis: results from an inception cohort. Rheumatology (Oxford). 2010;49(8):1483–9. https://doi.org/10.1093/rheumatology/keq035.
• Duarte AC, Porter JC, Leandro MJ. The lung in a cohort of rheumatoid arthritis patients-an overview of different types of involvement and treatment. Rheumatology (Oxford). 2019;58(11):2031–8. https://doi.org/10.1093/rheumatology/kez177 A comprehensive study of lung involvement among patients with RA.
•• Sparks JA, He X, Huang J, Fletcher EA, Zaccardelli A, Friedlander HM, et al. Rheumatoid arthritis disease activity predicting incident clinically apparent rheumatoid arthritis-associated interstitial lung disease: a prospective cohort study. Arthritis Rheumatol. 2019;71(9):1472–82. https://doi.org/10.1002/art.40904 A prospective cohort study showing that moderate to high disease activity was associated with increased RA-ILD risk compared with low disease activity or remission.
Alamoudi OSB, Attar SM. Pleuropulmonary manifestation in patients with rheumatoid arthritis in Saudi Arabia. Ann Thorac Med. 2017;12(4):266–71. https://doi.org/10.4103/atm.ATM_392_16.
• Salaffi F, Carotti M, Di Carlo M, Tardella M, Giovagnoni A. High-resolution computed tomography of the lung in patients with rheumatoid arthritis: prevalence of interstitial lung disease involvement and determinants of abnormalities. Medicine (Baltimore). 2019;98(38):e17088. https://doi.org/10.1097/MD.0000000000017088 A detailed investigation of the prevalence and risk factors of RA-ILD among patients with high-resolution chest computed tomography performed.
Yilmazer B, Gumustas S, Cosan F, Inan N, Ensaroglu F, Erbag G, et al. High-resolution computed tomography and rheumatoid arthritis: semi-quantitative evaluation of lung damage and its correlation with clinical and functional abnormalities. Radiol Med. 2016;121(3):181–9. https://doi.org/10.1007/s11547-015-0590-5.
McFarlane IM, Zhaz SY, Bhamra MS, Burza A, Kolla S, Alvarez MR, et al. Assessment of interstitial lung disease among black rheumatoid arthritis patients. Clin Rheumatol. 2019;38(12):3413–24. https://doi.org/10.1007/s10067-019-04760-6.
Goggins MR, Conway R, Durcan LJ, Johnston C, Cunnane G. High prevalence of abnormalities on chest radiography in rheumatoid arthritis. Clin Rheumatol. 2019;38(12):3375–80. https://doi.org/10.1007/s10067-019-04717-9.
England BR, Roul P, Mahajan TD, Singh N, Yu F, Sayles H, et al. Performance of administrative algorithms to identify interstitial lung disease in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2019. https://doi.org/10.1002/acr.24043.
Curtis JR, Sarsour K, Napalkov P, Costa LA, Schulman KL. Incidence and complications of interstitial lung disease in users of tocilizumab, rituximab, abatacept and anti-tumor necrosis factor alpha agents, a retrospective cohort study. Arthritis Res Ther. 2015;17:319. https://doi.org/10.1186/s13075-015-0835-7.
Cho SK, Doyle TJ, Lee H, Jin Y, Tong AY, Ortiz AJS, et al. Validation of claims-based algorithms to identify interstitial lung disease in patients with rheumatoid arthritis. Semin Arthritis Rheum. 2020.
Gautam M, Masood MJ, Arooj S, Mahmud ME, Mukhtar MU. Rheumatoid arthritis related interstitial lung disease: patterns of high-resolution computed tomography. Cureus. 2020;12(2):e6875. https://doi.org/10.7759/cureus.6875.
Zhang Y, Lu N, Peloquin C, Dubreuil M, Neogi T, Avina-Zubieta JA, et al. Improved survival in rheumatoid arthritis: a general population-based cohort study. Ann Rheum Dis. 2017;76(2):408–13. https://doi.org/10.1136/annrheumdis-2015-209058.
Doyle TJ, Patel AS, Hatabu H, Nishino M, Wu G, Osorio JC, et al. Detection of rheumatoid arthritis-interstitial lung disease is enhanced by serum biomarkers. Am J Respir Crit Care Med. 2015;191(12):1403–12. https://doi.org/10.1164/rccm.201411-1950OC.
Restrepo JF, del Rincon I, Battafarano DF, Haas RW, Doria M, Escalante A. Clinical and laboratory factors associated with interstitial lung disease in rheumatoid arthritis. Clin Rheumatol. 2015;34(9):1529–36. https://doi.org/10.1007/s10067-015-3025-8.
Saag KG, Kolluri S, Koehnke RK, Georgou TA, Rachow JW, Hunninghake GW, et al. Rheumatoid arthritis lung disease. Determinants of radiographic and physiologic abnormalities. Arthritis Rheum. 1996;39(10):1711–9.
• Kiely P, Busby AD, Nikiphorou E, Sullivan K, Walsh DA, Creamer P, et al. Is incident rheumatoid arthritis interstitial lung disease associated with methotrexate treatment? Results from a multivariate analysis in the ERAS and ERAN inception cohorts. BMJ open. 2019;9(5):e028466. https://doi.org/10.1136/bmjopen-2018-028466 An observational study investigating methotrexate and other RA factors with RA-ILD.
Juge PA, Lee JS, Ebstein E, Furukawa H, Dobrinskikh E, Gazal S, et al. MUC5B promoter variant and rheumatoid arthritis with interstitial lung disease. N Engl J Med. 2018;379(23):2209–19. https://doi.org/10.1056/NEJMoa1801562 A definitive study showing that the MUC5B promoter variant is a strong genetic risk factor for RA-ILD, specifically the UIP subtype.
Wang D, Zhang J, Lau J, Wang S, Taneja V, Matteson EL, et al. Mechanisms of lung disease development in rheumatoid arthritis. Nat Rev Rheumatol. 2019;15(10):581–96. https://doi.org/10.1038/s41584-019-0275-x.
Giles JT, Danoff SK, Sokolove J, Wagner CA, Winchester R, Pappas DA, et al. Association of fine specificity and repertoire expansion of anticitrullinated peptide antibodies with rheumatoid arthritis associated interstitial lung disease. Ann Rheum Dis. 2014;73(8):1487–94. https://doi.org/10.1136/annrheumdis-2012-203160.
• Alunno A, Bistoni O, Pratesi F, La Paglia GMC, Puxeddu I, Migliorini P, et al. Anti-citrullinated alpha enolase antibodies, interstitial lung disease and bone erosion in rheumatoid arthritis. Rheumatology (Oxford). 2018;57(5):850–5. https://doi.org/10.1093/rheumatology/kex520 A study showing the novel association of a specific ACPA with RA-ILD.
Liu Y, Liu C, Li L, Zhang F, Li Y, Zhang S. High levels of antibodies to citrullinated alpha-enolase peptide-1 (CEP-1) identify erosions and interstitial lung disease (ILD) in a Chinese rheumatoid arthritis cohort. Clin Immunol. 2019;200:10–5. https://doi.org/10.1016/j.clim.2019.01.001.
• Castellanos-Moreira R, Rodriguez-Garcia SC, Gomara MJ, Ruiz-Esquide V, Cuervo A, Casafont-Sole I, et al. Anti-carbamylated proteins antibody repertoire in rheumatoid arthritis: evidence of a new autoantibody linked to interstitial lung disease. Ann Rheum Dis. 2020;79(5):587–94. https://doi.org/10.1136/annrheumdis-2019-216709 A study showing the novel association of anti-CarP autoantibodies with RA-ILD.
Yin Y, Liang D, Zhao L, Li Y, Liu W, Ren Y, et al. Anti-cyclic citrullinated peptide antibody is associated with interstitial lung disease in patients with rheumatoid arthritis. PLoS One. 2014;9(4):e92449. https://doi.org/10.1371/journal.pone.0092449.
• Giles JT, Darrah E, Danoff S, Johnson C, Andrade F, Rosen A, et al. Association of cross-reactive antibodies targeting peptidyl-arginine deiminase 3 and 4 with rheumatoid arthritis-associated interstitial lung disease. PLoS One. 2014;9(6):e98794. https://doi.org/10.1371/journal.pone.0098794 A study showing the novel association of anti-PAD3/4 autoantibodies with RA-ILD.
• England BR, Duryee MJ, Roul P, Mahajan TD, Singh N, Poole JA, et al. Malondialdehyde-acetaldehyde adducts and antibody responses in rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheumatol. 2019;71(9):1483–93. https://doi.org/10.1002/art.40900 A study showing the novel association of anti-PAD3/4 autoantibodies with RA-ILD.
Harlow L, Rosas IO, Gochuico BR, Mikuls TR, Dellaripa PF, Oddis CV, et al. Identification of citrullinated hsp90 isoforms as novel autoantigens in rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheum. 2013;65(4):869–79. https://doi.org/10.1002/art.37881.
Chen J, Song S, Liu Y, Liu D, Lin Y, Ge S, et al. Autoreactive T cells to citrullinated HSP90 are associated with interstitial lung disease in rheumatoid arthritis. Int J Rheum Dis. 2018;21(7):1398–405. https://doi.org/10.1111/1756-185x.13316.
Wang JX, Du CG. A retrospective study of clinical characteristics of interstitial lung disease associated with rheumatoid arthritis in Chinese patients. Med Sci Monit. 2015;21:708–15. https://doi.org/10.12659/MSM.890880.
Wolfe F, Caplan L, Michaud K. Rheumatoid arthritis treatment and the risk of severe interstitial lung disease. Scand J Rheumatol. 2007;36(3):172–8. https://doi.org/10.1080/03009740601153774.
Maniwa K, Ogushi F, Tani K, Ohmoto Y, Muraguchi M, Sone S. Increased incidence of autoantibodies to interleukin-1a in rheumatoid arthritis with interstitial lung disease. Respirology. 2000;5(4):315–20.
• Liao KP, Sparks JA, Hejblum BP, Kuo IH, Cui J, Lahey LJ, et al. Phenome-wide association study of autoantibodies to citrullinated and noncitrullinated epitopes in rheumatoid arthritis. Arthritis Rheumatol. 2017;69(4):742–9. https://doi.org/10.1002/art.39974 A study showing the novel association of specific ACPA with RA-ILD.
Chen J, Doyle TJ, Liu Y, Aggarwal R, Wang X, Shi Y, et al. Biomarkers of rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheumatol. 2015;67(1):28–38. https://doi.org/10.1002/art.38904.
Matsuo T, Hashimoto M, Ito I, Kubo T, Uozumi R, Furu M, et al. Interleukin-18 is associated with the presence of interstitial lung disease in rheumatoid arthritis: a cross-sectional study. Scand J Rheumatol. 2019;48(2):87–94. https://doi.org/10.1080/03009742.2018.1477989.
Seibold MA, Wise AL, Speer MC, Steele MP, Brown KK, Loyd JE, et al. A common MUC5B promoter polymorphism and pulmonary fibrosis. N Engl J Med. 2011;364(16):1503–12. https://doi.org/10.1056/NEJMoa1013660.
Hunninghake GM, Hatabu H, Okajima Y, Gao W, Dupuis J, Latourelle JC, et al. MUC5B promoter polymorphism and interstitial lung abnormalities. N Engl J Med. 2013;368(23):2192–200. https://doi.org/10.1056/NEJMoa1216076.
Kesimer M, Ford AA, Ceppe A, Radicioni G, Cao R, Davis CW, et al. Airway mucin concentration as a marker of chronic bronchitis. N Engl J Med. 2017;377(10):911–22. https://doi.org/10.1056/NEJMoa1701632.
Conigliaro P, Chimenti MS, Triggianese P, Sunzini F, Novelli L, Perricone C, et al. Autoantibodies in inflammatory arthritis. Autoimmun Rev. 2016;15(7):673–83. https://doi.org/10.1016/j.autrev.2016.03.003.
Sapkota M, Burnham EL, DeVasure JM, Sweeter JM, Hunter CD, Duryee MJ, et al. Malondialdehyde-acetaldehyde (MAA) protein adducts are found exclusively in the lungs of smokers with alcohol use disorders and are associated with systemic anti-MAA antibodies. Alcohol Clin Exp Res. 2017;41(12):2093–9. https://doi.org/10.1111/acer.13509.
Thiele GM, Tuma DJ, Willis MS, Miller JA, McDonald TL, Sorrell MF, et al. Soluble proteins modified with acetaldehyde and malondialdehyde are immunogenic in the absence of adjuvant. Alcohol Clin Exp Res. 1998;22(8):1731–9.
Zhang Y, Li H, Wu N, Dong X, Zheng Y. Retrospective study of the clinical characteristics and risk factors of rheumatoid arthritis-associated interstitial lung disease. Clin Rheumatol. 2017;36(4):817–23. https://doi.org/10.1007/s10067-017-3561-5.
Wang T, Zheng XJ, Ji YL, Liang ZA, Liang BM. Tumour markers in rheumatoid arthritis-associated interstitial lung disease. Clin Exp Rheumatol. 2016;34(4):587–91.
White ES, Xia M, Murray S, Dyal R, Flaherty CM, Flaherty KR, et al. Plasma surfactant protein-D, matrix metalloproteinase-7, and osteopontin index distinguishes idiopathic pulmonary fibrosis from other idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2016;194(10):1242–51. https://doi.org/10.1164/rccm.201505-0862OC.
•• Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019;381(18):1718–27. https://doi.org/10.1056/NEJMoa1908681 A pivotal clinical trial for efficacy of the anti-fibrotic nintedanib in ILD.
•• Maher TM, Corte TJ, Fischer A, Kreuter M, Lederer DJ, Molina-Molina M, et al. Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med. 2020;8(2):147–57. https://doi.org/10.1016/S2213-2600(19)30341-8 A pivotal clinical trial for efficacy of the anti-fibrotic pirfenodine in ILD.
Antoniou KM, Margaritopoulos G, Economidou F, Siafakas NM. Pivotal clinical dilemmas in collagen vascular diseases associated with interstitial lung involvement. Eur Respir J. 2009;33(4):882–96. https://doi.org/10.1183/09031936.00152607.
Fragoulis GE, Conway R, Nikiphorou E. Methotrexate and interstitial lung disease: controversies and questions. A narrative review of the literature. Rheumatology (Oxford). 2019;58(11):1900–6. https://doi.org/10.1093/rheumatology/kez337.
Kremer JM, Alarcon GS, Weinblatt ME, Kaymakcian MV, Macaluso M, Cannon GW, et al. Clinical, laboratory, radiographic, and histopathologic features of methotrexate-associated lung injury in patients with rheumatoid arthritis: a multicenter study with literature review. Arthritis Rheum. 1997;40(10):1829–37. https://doi.org/10.1002/art.1780401016.
Conway R, Low C, Coughlan RJ, O'Donnell MJ, Carey JJ. Methotrexate use and risk of lung disease in psoriasis, psoriatic arthritis, and inflammatory bowel disease: systematic literature review and meta-analysis of randomised controlled trials. BMJ. 2015;350:h1269. https://doi.org/10.1136/bmj.h1269.
• Solomon DH, Glynn RJ, Karlson EW, Lu F, Corrigan C, Colls J, et al. Adverse effects of low-dose methotrexate: a randomized trial. Ann Intern Med. 2020. https://doi.org/10.7326/M19-3369 A clinical trial showing that methotrexate increased the risk for pulmonary adverse events.
• Kang EH, Jin Y, Desai RJ, Liu J, Sparks JA, Kim SC. Risk of exacerbation of pulmonary comorbidities in patients with rheumatoid arthritis after initiation of abatacept versus TNF inhibitors: a cohort study. Semin Arthritis Rheum. 2019. https://doi.org/10.1016/j.semarthrit.2019.11.010 A propensity score–matched observational study showing that abatacept and TNF inhibitors had similar pulmonary safety in patients with RA and lung diseases, including RA-ILD.
Roubille C, Haraoui B. Interstitial lung diseases induced or exacerbated by DMARDS and biologic agents in rheumatoid arthritis: a systematic literature review. Semin Arthritis Rheum. 2014;43(5):613–26. https://doi.org/10.1016/j.semarthrit.2013.09.005.
Bradley B, Branley HM, Egan JJ, Greaves MS, Hansell DM, Harrison NK, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax. 2008;63(Suppl 5):v1–58. https://doi.org/10.1136/thx.2008.101691.
Kim EJ, Collard HR, King TE Jr. Rheumatoid arthritis-associated interstitial lung disease: the relevance of histopathologic and radiographic pattern. Chest. 2009;136(5):1397–405. https://doi.org/10.1378/chest.09-0444.
Yukawa K, Nagamoto Y, Watanabe H, Funaki M, Iwahashi M, Yamana J, et al. Risk factors for pneumocystis jirovecii pneumonia in patients with rheumatoid arthritis and a prophylactic indication of trimethoprim/sulfamethoxazole. J Clin Rheumatol. 2018;24(7):355–60. https://doi.org/10.1097/RHU.0000000000000731.
Dixon WG, Abrahamowicz M, Beauchamp ME, Ray DW, Bernatsky S, Suissa S, et al. Immediate and delayed impact of oral glucocorticoid therapy on risk of serious infection in older patients with rheumatoid arthritis: a nested case-control analysis. Ann Rheum Dis. 2012;71(7):1128–33. https://doi.org/10.1136/annrheumdis-2011-200702.
Laan RF, Buijs WC, Verbeek AL, Draad MP, Corstens FH, van de Putte LB, et al. Bone mineral density in patients with recent onset rheumatoid arthritis: influence of disease activity and functional capacity. Ann Rheum Dis. 1993;52(1):21–6. https://doi.org/10.1136/ard.52.1.21.
Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int. 2007;18(10):1319–28. https://doi.org/10.1007/s00198-007-0394-0.
Tzouvelekis A, Galanopoulos N, Bouros E, Kolios G, Zacharis G, Ntolios P, et al. Effect and safety of mycophenolate mofetil or sodium in systemic sclerosis-associated interstitial lung disease: a meta-analysis. Pulm Med. 2012;2012:143637–7. https://doi.org/10.1155/2012/143637.
Fischer A, Brown KK, Du Bois RM, Frankel SK, Cosgrove GP, Fernandez-Perez ER, et al. Mycophenolate mofetil improves lung function in connective tissue disease-associated interstitial lung disease. J Rheumatol. 2013;40(5):640–6. https://doi.org/10.3899/jrheum.121043.
Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, et al. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomised controlled, double-blind, parallel group trial. Lancet Respir Med. 2016;4(9):708–19. https://doi.org/10.1016/S2213-2600(16)30152-7.
Saketkoo LA, Espinoza LR. Experience of mycophenolate mofetil in 10 patients with autoimmune-related interstitial lung disease demonstrates promising effects. Am J Med Sci. 2009;337(5):329–35. https://doi.org/10.1097/MAJ.0b013e31818d094b.
Kelly C, Saravanan V. Treatment strategies for a rheumatoid arthritis patient with interstitial lung disease. Expert Opin Pharmacother. 2008;9(18):3221–30. https://doi.org/10.1517/14656560802591430.
Bosello SL, De Luca G, Rucco M, Berardi G, Falcione M, Danza FM, et al. Long-term efficacy of B cell depletion therapy on lung and skin involvement in diffuse systemic sclerosis. Semin Arthritis Rheum. 2015;44(4):428–36. https://doi.org/10.1016/j.semarthrit.2014.09.002.
Doyle TJ, Dhillon N, Madan R, Cabral F, Fletcher EA, Koontz DC, et al. Rituximab in the treatment of interstitial lung disease associated with antisynthetase syndrome: a multicenter retrospective case review. J Rheumatol. 2018;45(6):841–50. https://doi.org/10.3899/jrheum.170541.
Keir GJ, Maher TM, Hansell DM, Denton CP, Ong VH, Singh S, et al. Severe interstitial lung disease in connective tissue disease: rituximab as rescue therapy. Eur Respir J. 2012;40(3):641–8. https://doi.org/10.1183/09031936.00163911.
• Md Yusof MY, Kabia A, Darby M, Lettieri G, Beirne P, Vital EM, et al. Effect of rituximab on the progression of rheumatoid arthritis-related interstitial lung disease: 10 years’ experience at a single centre. Rheumatology (Oxford). 2017;56(8):1348–57. https://doi.org/10.1093/rheumatology/kex072 An observational study suggesting that rituximab may be an acceptable therapeutic choice for RA-ILD.
• Druce KL, Iqbal K, Watson KD, Symmons DPM, Hyrich KL, Kelly C. Mortality in patients with interstitial lung disease treated with rituximab or TNFi as a first biologic. RMD open. 2017;3(1):e000473. https://doi.org/10.1136/rmdopen-2017-000473 An observational study suggesting that rituximab had lower mortality than TNF inhibitors in RA-ILD.
Schupp JC, Kohler T, Muller-Quernheim J. Usefulness of cyclophosphamide pulse therapy in interstitial lung diseases. Respiration. 2016;91(4):296–301. https://doi.org/10.1159/000445031.
Raghu G, Depaso WJ, Cain K, Hammar SP, Wetzel CE, Dreis DF, et al. Azathioprine combined with prednisone in the treatment of idiopathic pulmonary fibrosis: a prospective double-blind, randomized, placebo-controlled clinical trial. Am Rev Respir Dis. 1991;144(2):291–6. https://doi.org/10.1164/ajrccm/144.2.291.
Idiopathic Pulmonary Fibrosis Clinical Research N, Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366(21):1968–77. https://doi.org/10.1056/NEJMoa1113354.
Oldham JM, Lee C, Valenzi E, Witt LJ, Adegunsoye A, Hsu S, et al. Azathioprine response in patients with fibrotic connective tissue disease-associated interstitial lung disease. Respir Med. 2016;121:117–22. https://doi.org/10.1016/j.rmed.2016.11.007.
• Manfredi A, Cassone G, Furini F, Gremese E, Venerito V, Atzeni F, et al. Tocilizumab therapy in rheumatoid arthritis with interstitial lung disease: a multicenter retrospective study. Intern med J. 2019. https://doi.org/10.1111/imj.14670 An observational study suggesting that tocilizumab may be an acceptable therapeutic choice for RA-ILD.
Jani M, Hirani N, Matteson EL, Dixon WG. The safety of biologic therapies in RA-associated interstitial lung disease. Nat Rev Rheumatol. 2014;10(5):284–94. https://doi.org/10.1038/nrrheum.2013.197.
• Fernandez-Diaz C, Loricera J, Castaneda S, Lopez-Mejias R, Ojeda-Garcia C, Olive A, et al. Abatacept in patients with rheumatoid arthritis and interstitial lung disease: a national multicenter study of 63 patients. Semin Arthritis Rheum. 2018;48(1):22–7. https://doi.org/10.1016/j.semarthrit.2017.12.012 An observational study suggesting that abatacept may be an acceptable therapeutic choice for RA-ILD.
APRIL (AbatacePt in Rheumatoid Arthritis-ILD). .
Harigai M. Growing evidence of the safety of JAK inhibitors in patients with rheumatoid arthritis. Rheumatology (Oxford). 2019;58(Suppl 1):i34–42. https://doi.org/10.1093/rheumatology/key287.
Chen Z, Wang X, Ye S. Tofacitinib in amyopathic dermatomyositis-associated interstitial lung disease. N Engl J Med. 2019;381(3):291–3. https://doi.org/10.1056/NEJMc1900045.
Effects of tofacitinib vs methotrexate on rheumatoid arthritis interstitial lung disease. Accessed 31 May 2020.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–82. https://doi.org/10.1056/NEJMoa1402584.
Noble PW, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47(1):243–53. https://doi.org/10.1183/13993003.00026-2015.
Khanna D, Albera C, Fischer A, Khalidi N, Raghu G, Chung L, et al. An open-label, phase II study of the safety and tolerability of pirfenidone in patients with scleroderma-associated interstitial lung disease: the LOTUSS trial. J Rheumatol. 2016;43(9):1672–9. https://doi.org/10.3899/jrheum.151322.
Phase II study of pirfenidone in patients with RAILD (TRAIL1). Accessed.
Yazdani A, Singer LG, Strand V, Gelber AC, Williams L, Mittoo S. Survival and quality of life in rheumatoid arthritis-associated interstitial lung disease after lung transplantation. J Heart Lung Transplant. 2014;33(5):514–20. https://doi.org/10.1016/j.healun.2014.01.858.
Funding
Dr. Khanna was supported by the NIH/NIAMS K24 AR063120-07 and R01AR07047. Dr. Doyle is supported by the National Institutes of Health (K23 HL119558 and R03 HL148484). Dr. Sparks is supported by the Rheumatology Research Foundation K Supplement Award, the National Institutes of Health (grant numbers K23 AR069688, K23 HL119558, R03 AR075886, L30 AR066953, P30 AR070253, and P30 AR072577), and the R. Bruce and Joan M. Mickey Research Scholar Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Dellaripa reports involvement in a clinical trial funded by Genentech and a study funded by Bristol-Myers Squibb. Dr. Bolster reports clinical trial funding from Cumberland and Corbus; is a consultant to Gilead Sciences; and has stock ownership in Johnson and Johnson. Dr. Khanna is a consultant to Acceleron, Actelion, Amgen, Bayer, Boehringer Ingelheim, CSL Behring, Corbus, Galapagos, Genentech/Roche, GSK, Gilead, Horizon Merck, Mitsubishi Tanabe Pharma, Regeneron, Sanofi-Aventis, and United Therapeutics; and holds stocks in Eicos Sciences, Inc. Dr. Doyle reports research funding from Bristol-Myers Squibb and involvement in a clinical trial funded by Genentech and Bristol-Myers Squibb. Dr. Sparks reports research funding from Bristol-Myers Squibb and Amgen and consultancy to Bristol-Myers Squibb, Gilead, Inova, Janssen, and Optum.
Human and Animal Rights and Informed Consent
This article does not contain any primary data of human or animal subjects performed by any of the authors.
Disclaimer
The funders had no role in the decision to publish or preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard University, its affiliated academic health care centers, or the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Rheumatoid Arthritis
Rights and permissions
About this article
Cite this article
Huang, S., Kronzer, V.L., Dellaripa, P.F. et al. Rheumatoid Arthritis–Associated Interstitial Lung Disease: Current Update on Prevalence, Risk Factors, and Pharmacologic Treatment. Curr Treat Options in Rheum 6, 337–353 (2020). https://doi.org/10.1007/s40674-020-00160-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-020-00160-z