Abstract
Purpose of review
Macrophage activation syndrome (MAS) is a life-threatening inflammatory condition, belonging to the spectrum of hemophagocytic lymphohistiocytosis (HLH), which may severely complicate the course of rheumatologic diseases, mainly systemic juvenile idiopathic arthritis. Although the pathophysiology of MAS is still not completely understood, it is characterized by an abnormal proliferation of T lymphocytes and macrophages, responsible for cytokine overproduction and hemophagocytosis. Because MAS may be rapidly fatal, its prompt recognition is imperative in order to immediately start adequate treatment. This review will overview the main features of MAS occurring in the context of childhood inflammatory conditions, discussing the recent updates in diagnosis, pathophysiology, and management.
Recent findings
Recently, several diagnostic tools have been developed to recognize MAS in the context of pediatric inflammatory disorders. These are largely based on routinely available clinical and laboratory features and may aid physician in clinical practice. Progress in understanding the pathophysiology of MAS led to a significant improvement in identifying novel therapies targeting pro-inflammatory cytokines, a less toxic approach for children with MAS.
Summary
In the future, tailored therapy based on the recognition of genetic predisposition, underlying disorder, triggers, and biomarkers will likely improve the outcome of pediatric patients with MAS/sHLH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Macrophage activation syndrome (MAS) refers to a severe and potentially fatal condition, due to an excessive and uncontrolled hyperinflammatory reaction, which might complicate rheumatologic diseases, mainly systemic juvenile idiopathic arthritis (sJIA) and its adult counterpart adult-onset Still’s disease (AOSD). MAS belongs to the spectrum of hemophagocytic lymphohistiocytosis (HLH) and is currently classified among its secondary forms, as a sHLH occurring in the context of a rheumatic disorder [1•, 2•] (Table 1). MAS was firstly reported by Hadchouel and colleagues who in 1985 described an acute-onset encephalopathy with coagulopathy and hepatitis in seven patients with sJIA [3]. The term MAS was then proposed in 1993, due to the observation of an activated monocyte-macrophage system in patients with this syndrome [4].
The overall incidence of MAS in rheumatologic conditions is still unknown. It is estimated that 10% of patients with sJIA develop overt MAS [5], but several pieces of evidence support that this complication might occur subclinically in up to 30–40% of cases [6, 7]. In a recent multinational study on 362 patients with sJIA-associated MAS, the syndrome was diagnosed at sJIA onset in 22% of the patients, and no significant differences in demographic, clinical, and histopathologic features were observed in different countries [8•, 9]. In the cohort of children with systemic lupus erythematosus (SLE) described by Borgia et al. in 2018, MAS occurred in 10% of cases, mainly at SLE onset [10•]. Albeit more rarely, MAS can complicate the course of other rheumatic diseases, such as the Kawasaki disease and juvenile dermatomyositis, and has been reported in sporadic cases of recurrent fever syndromes [11,12,13].
Although most instances of MAS lack an identifiable trigger, the syndrome has been reported more frequently in the context of a flare of the inflammatory underlying disease and after infections, especially Epstein-Barr virus [8•].
Clinically, MAS is characterized by unremitting high fever, cytopenia, hyperferritinemia, hepatosplenomegaly, liver dysfunction, and coagulopathy with hemorrhagic manifestations. Despite increasing awareness, MAS occurrence is still worrisome with a reported 8% mortality rate in sJIA patients [8•].
This article reviews the main features of MAS occurring in the context of childhood inflammatory conditions and discusses the recent updates in diagnosis, pathophysiology, and management.
Clinical manifestations
The clinical presentation of MAS is typically acute and may occasionally be rapidly life-threatening with development of multiorgan failure.
Clinical features at the onset of MAS are generally not specific. Unremitting fever is the main clinical manifestation of MAS together with hepatosplenomegaly and generalized lymphadenopathy. CNS involvement might occur in almost one-third of patients and includes a wide spectrum of severity ranging from headache, lethargy, and irritability to disorientation, seizures, or coma. Hemorrhagic manifestations, from easy bruising and purpura to severe mucosal bleeding, are reported in approximately 20% of cases [8•].
Laboratory abnormalities are crucial in early diagnosis of MAS because their change generally anticipates clinical symptoms. Typical laboratory features include severe cytopenia, liver dysfunction with high levels of serum transaminases, coagulopathy with hypofibrinogenemia, and consequent decrease in the erythrocyte sedimentation rate (ESR). Additional laboratory alterations are increased levels of triglycerides, lactate dehydrogenase (LDH), and d-dimer, and especially a marked hyperferritinemia which is probably the most important laboratory marker of MAS.
MAS clinical features resemble those observed in primary HLH. However, MAS occurs in the context of an underlying highly inflammatory condition. For that reason, a considerable percentage of patients at MAS onset paradoxically present laboratory parameters still within normal range values [8•]. Indeed, in the suspicion of MAS, change over time of laboratory features, especially of white blood cell (WBC) count, neutrophils, platelet count, fibrinogen, and ferritin, is more relevant than their decrease below or increase above a certain threshold. In an experts’ consensus, platelet count, ferritin, and aspartate aminotransferase (AST) resulted in the variables whose change over time was considered more important for a timely diagnosis of MAS in patients with systemic JIA [14•]. An acute CNS worsening or new-onset kidney failure, with an abrupt increase in LDH and AST and decrease in platelet count and fibrinogen out of proportion of other laboratory abnormalities, should raise the suspicion of coexisting thrombotic microangiopathy [15].
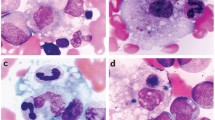
Bone marrow examination might reveal a pathognomonic feature of MAS with well-differentiated macrophages showing hemophagocytic activity. However, hemophagocytosis may be undetectable in approximately one-third of sJIA-associated MAS and in almost 70% of MAS in the context of SLE [8•, 10•]. Absence of hemophagocytosis should not exclude the diagnosis of MAS.
Genetics and pathophysiology
Although MAS pathophysiology is still not completely understood, recent pieces of evidence effectively improved our knowledge on the pathways mainly involved in its development.
As mentioned above, MAS is considered part of the spectrum of HLH and it is thus conceivable that some of the pathogenetic pathways of primary HLH could be involved also in MAS.
In primary HLH, the uncontrolled proliferation of T lymphocytes and macrophages, which is responsible for cytokine overproduction and hemophagocytosis, has been attributed to reduced natural killer (NK) cell and cytotoxic T cell function [16, 17], secondary to homozygous defects in genes involved in perforin-mediated cytolytic pathway [18,18,19,20] (Table 1). Defects in killing prolong the interaction between cytotoxic T lymphocytes or NK cells and the infected target cell, resulting in a pro-inflammatory cytokine storm [21].
Several authors described impaired NK cytotoxic function in patients with sJIA-associated MAS [22]. In recent studies, almost one-third of patients with a history of MAS presented persistent functional abnormalities in NK cell granule release [23], and a reduced functional response to IL-18 in NK cells from SJIA patients has been described [24]. In agreement with these observations, heterozygous mutations in primary HLH genes have been detected in patients with MAS. Vastert et al. demonstrated a higher prevalence of the perforin gene A91V variant in patients with sJIA and MAS than in sJIA patients without MAS or healthy controls [25]. A whole-exome sequencing approach revealed heterozygous mutations in primary HLH genes in up to 40% of patients with MAS [26•, 27]. Interestingly, primary HLH genetic variants have been described also in a group of patients with severe H1N1 influenza and sHLH features [28•].
However, most MAS patients do not have identified mutations in genes involved in cytolytic dysfunction. Indeed, in a recent study conducted on an IL-6 transgenic animal model, in which IL-6 hyperproduction triggers a MAS-like clinical picture, NK cells showed impaired perforin and granzyme expression despite normal degranulation, suggesting a key role of IL-6 in NK cell cytotoxicity inhibition [29, 30].
Despite this strong evidence, MAS patients without cytotoxic defect have been described and IL-6 inhibition does not prevent MAS occurrence in all sJIA patients, suggesting that other pathways are involved in its pathogenesis. Most likely, in sHLH, multiple pathways can combine to determine and amplify the uncontrolled active inflammatory status that progressively lead to the cytokine storm characterized by the overproduction of pro-inflammatory cytokines such as IL-1, IL-6, IL-18, and especially INFγ [5]. Robust pieces of evidence support the role of IFNγ as the key effector in primary HLH [31]. Similarly, high levels of INFγ and INFγ-induced chemokines (CXCL9) have been found to characterize patients with MAS and correlate with typical clinical and laboratory features [32••]. A crucial INFγ promoter, IL-18, has been demonstrated to be persistently elevated in patients with recurrent MAS episodes [33, 34••], suggesting its potential role as a biomarker for patients at risk for MAS. Moreover, in patients with NLRC4-related autoinflammatory disorder, characterized by recurrent HLH episodes, IL-18 levels are chronically elevated [35•].
In accordance with these pieces of evidence, the cytokine storm which characterizes primary HLH, secondary HLH, and MAS can be considered as a final common pathway that results from impaired cytotoxicity, cytokine overproduction, or a combination of both of these factors [2•, 36••, 37] (Fig. 1). Some authors suggested a threshold or multilayer model for MAS pathogenesis: Genetic predisposition, disease activity, or other triggers such as infections, medication toxicity, or cancer contribute in different proportions to the typical MAS/HLH cytokine storm. Once the threshold level has been reached, the final effectors of a common way, typically driven by INFγ, lead to full-blown MAS, regardless of the interplay between the pathogenic factors [2•, 38•].
Pathogenesis of hemophagocytic lymphohistiocytosis (HLH) spectrum diseases. The cytokine storm in primary HLH, secondary HLH, and MAS can be considered as a final common pathway that results from two major mechanisms, often combined: impaired cytotoxicity and cytokine overproduction. pHLH, primary HLH; sHLH, secondary HLH; MAS, macrophage activation syndrome.
Diagnosis
MAS is a severe condition, which may have a rapidly fatal course. Timely recognition and prompt therapeutic intervention are, therefore, imperative. However, because MAS lacks a single pathognomonic feature and is clinically heterogeneous, early diagnosis is often challenging. Furthermore, hemophagocytosis may be absent in the initial phase [39] and lacks specificity for hemophagocytic syndromes [40]. The diagnostic difficulties are compounded by the fact that MAS may mimic other conditions that present with overlapping features, such as a flare of the underlying disease or an infectious complication. Finally, no set of universal criteria validated for the diagnosis of MAS in all different pediatric rheumatologic conditions are available so far.
MAS in sJIA
The clinical similarities between MAS and HLH led some clinicians to recommend the use of the HLH-2004 criteria [41•] (Table 2). However, it is important to remember that sJIA-associated MAS and primary HLH develop in different settings: MAS in the context of an underlying highly inflammatory condition, while primary HLH is a primitive disorder with genetic basis. Although HLH-2004 criteria have been considered potentially suitable for detecting MAS in sJIA, they are affected by several potential shortcomings [42].
Due to the prominent inflammatory nature of sJIA, in a MAS patient, the absolute cut-offs for WBC count, platelet level, and fibrinogen level are usually reached only in a later stage in which treatment might be late. In addition, the identification of low or absent NK cell activity and higher levels of soluble cluster of differentiation 25 (sCD25) have limited use in MAS, due to their scarce availability in the majority of centers and lack of timeliness. Furthermore, as overmentioned, hemophagocytosis has been reported only in 60% of MAS patient at onset [8•].
In 2016, a multinational collaborative effort led to the publication of a set of validated classification criteria for MAS complicating sJIA [43••, 44] (Table 2). These criteria are routinely readily available and timely and are based on a combination of expert consensus, available evidence from the medical literature, and analysis of real patient data. In the validation cohort, final MAS classification criteria for children with sJIA proved to have a sensitivity of 0.73 and specificity of 0.99. However, the 2016 criteria have been primarily proposed as classification criteria for use in clinical trials and for research purposes and not as a diagnostic tool. Indeed, recent pieces of evidence suggested that they could not capture all instances of MAS with subtle onset or incomplete clinical expression, while confirming their strong diagnostic power in identifying full-blown pictures of the syndrome [45]. Furthermore, recent studies showed a limited sensitivity of the 2016 classification criteria in detecting MAS in sJIA patients under biologic treatment, especially with IL-6 inhibitors [46, 47].
Against this background, a diagnostic score for MAS in sJIA, named MS score (Table 2), has been recently developed [48••]. By means of a Bayesian model averaging approach, 7 clinical and laboratory variables (CNS involvement, hemorrhagic manifestations, active arthritis, platelet count, LDH, fibrinogen, and ferritin) with the highest probability of being part of the models with the best performances in MAS diagnosis were selected in the final set of criteria. In this diagnostic tool, laboratory variables are included as continuous variables, potentially increasing the ability of the score to capture different instances of MAS. The MS score is the result of a weighted equation ranging from − 8.4 to 41.8 with a cut-off value of ≥ − 2.1, yielding a sensitivity of 0.85 and specificity of 0.95 in discriminating MAS from an active sJIA flare. While the MS score could be potentially applicable to AOSD, it is not intended to be used in other pediatric rheumatic diseases.
MAS in SLE
MAS has been reported with increasing frequency in childhood-onset SLE (cSLE) and its prevalence in this disease is probably underrecognized [49]. MAS diagnosis in SLE is further complicated by overlapping features, such as fever, cytopenia, splenomegaly, and CNS involvement, between the two conditions. In 2009, Parodi et al. reported the demographic, clinical, and histopathologic features of 38 patients with cSLE-associated MAS, collected in the context of a multinational survey or obtained from a systematic literature review [50•]. The clinical and laboratory features of the 38 cSLE patients with MAS were compared with those of a control group composed of 416 patients with active cSLE without MAS. In this cohort, both HLH-2004 diagnostic guidelines [41•] and 2005 preliminary diagnostic guidelines for MAS complicating systemic JIA [51] were tested but were found to be inadequate for detecting MAS in the context of cSLE. Based on the results of statistical analyses, a set of preliminary diagnostic guidelines for MAS in cSLE was devised (Table 2), yielding a sensitivity of 0.92 and a specificity of 0.90. Owing to the strong discriminatory ability shown by this definition, the presence of hemophagocytosis in the bone marrow aspirate was considered necessary for diagnostic confirmation only in uncertain cases. The practical recommendation that came out from the study findings was that in a patient with cSLE, the occurrence of unexplained fever and cytopenia, especially thrombocytopenia, when associated with hyperferritinemia, should raise the suspicion of MAS. Notably, in the large size cohort of SLE-associated MAS recently described by Borgia et al., all patients with MAS satisfied the Parodi criteria [10•].
Generic criteria for MAS
The lack of universal criteria for MAS makes its recognition in a rheumatologic context other than already-diagnosed sJIA and cSLE further complicated. In 2014, Fardet et al. developed and validated a weighted diagnostic score for the broader category of reactive hemophagocytic syndrome (HS), called the HScore [52••], which includes 9 features: a history of immunosuppression, fever, organomegaly, cytopenia, ferritin, triglycerides, fibrinogen, AST, and presence of hemophagocytosis on bone marrow aspirate (Table 2). In both developmental and validation data sets, the HScore revealed an excellent diagnostic performance and discriminative ability. However, several reasons limit its use in the pediatric population. Because the patient sample included in the study of Fardet et al. was only composed of adults with HS, no conclusion can be reliably drawn regarding the applicability of the HScore to children with reactive HS, especially those with sJIA-associated MAS. In addition, the term “underlying immunosuppression” involves the use of some medications that are rarely prescribed in children with sJIA, such as cyclosporine and azathioprine, and does not include the cytokine inhibitors, which are a cornerstone of the treatment of this disease. Furthermore, as already discussed for HLH-2004 criteria, the threshold level for platelets is too low for detecting MAS in hyperinflammatory conditions, typically characterized by thrombocytosis. Finally, the HScore incorporates the demonstration of hemophagocytosis on bone marrow aspirate, which is often absent in children with reactive HS.
Hyperferritinemia is known to markedly rise in MAS, while the erythrocyte sedimentation rate (ESR) falls due to typical fibrinogen consumption. Recently, the ferritin/ESR ratio was developed by Eloiseily et al. and revealed to be a useful screening test for discriminating MAS from sJIA flare and for distinguishing hemophagocytic syndromes from other febrile conditions [53•].
Distinguishing MAS from primary HLH
Both primary HLH and MAS are potentially fatal conditions and require timely recognition to promptly start an appropriate treatment. However, due to their close similarities, their differentiation at onset may be challenging. Distinction may be particularly difficult when MAS is the first clinical presentation of sJIA, when arthritis may not be present yet, or when primary HLH occurs in later ages. Detection of biallelic pathogenic mutations in a disease-associated gene is the gold standard diagnostic test for primary HLH. However, these studies take weeks to complete and may not be available worldwide. Furthermore, some cases still elude molecular diagnosis [54] and some genetic overlap between MAS and pHLH has been described [25, 26•]. Timely distinction between primary HLH and MAS is, nevertheless, crucial because primary HLH is often more severe than MAS and the management of the two conditions differs.
An international collaborative effort led to the development and validation of a score that may assist in distinguishing primary HLH from systemic JIA-associated MAS [55••]. Based on clinical, laboratory, and histopathologic features of 362 patients with MAS and 258 patients with primary HLH, the score, named MH score, includes 6 routinely available variables: age at onset, neutrophil count, fibrinogen, splenomegaly, platelet count, and hemoglobin. The MH score may aid physicians in early differentiating between primary HLH and sJIA-associated MAS, facilitating the decision-making process regarding initial therapy and identifying those patients who are at higher risk of an inherited form of HLH and require further functional and genetic evaluation.
Treatment
Due to the lack of available controlled studies on MAS therapy, the management of this condition is still largely empiric.
The cornerstone of MAS treatment is traditionally constituted by high doses of glucocorticoids parenterally administered. Intravenous methylprednisolone (2–6 mg/kg/day in 2–4 refracted doses, or 30 mg/kg/day pulses) is the most frequently used glucocorticoid, but dexamethasone might be preferred in case of CNS involvement because of its better passage across the blood-brain barrier. The use of cyclosporine A was advocated in MAS since the 1990s, due to its demonstrated benefit in primary HLH. The ulterior observation of its high efficacy in some severe cases of MAS refractory to glucocorticoids [56, 57] has supported its current inclusion in first-line treatment of MAS.
Etoposide is included in the protocol developed for treating primary HLH [41•] and it is used, especially by pediatric hemato-oncologists, in severe cases of refractory MAS. However, the HLH-2004 protocol carries a significant risk of toxicity and mortality and a reduced etoposide regimen (50–100 mg/m2 once weekly) has been proposed for patients with severe secondary HLH [1•]. Whether or not a less aggressive use of etoposide as second-line therapy for severe refractory MAS will be beneficial remains unclear.
In addition to first-line immunosuppressive medications, such as glucocorticoids and cyclosporine, cytokine-specific inhibitors are increasingly used in MAS and may prove to be more targeted in controlling the cytokine storm. Although efficacy data are limited so far to the retrospective cohort, several pieces of evidence support the efficacy of anakinra, a recombinant IL-1 receptor antagonist, in patients with severe refractory MAS, especially in the context of sJIA [58,59,60,60,61, 62•, 63,64,65]. Although MAS development in sJIA patients on anakinra has been reported, the cause-effect relationship is difficult to establish. In a retrospective cohort of sJIA patients treated with anakinra, MAS occurred in 5 patients; however, an escalation in the dose of anakinra up to 6–10 mg/kg/day resolved MAS in most cases [65]. A randomized, double-blind, placebo-controlled trial in sHLH/MAS in children and adults will give further relevant insights into anakinra use in MAS (ClinicalTrials.gov: NCT02780583).
The pivotal role of INFγ in both primary and secondary HLH is well known [31, 32••, 34••, 66]. In addition, INFγ neutralization in an IL-6 transgenic animal model led to a great improvement in survival and a decrease in ferritin levels [67]. According to these pieces of evidence, a recent open-label phase II/III trial in patients with primary HLH demonstrated the high efficacy of the INFγ inhibitor emapalumab, and led to its approval by FDA for the treatment of primary HLH [68]. In addition, a report described the beneficial use of emapalumab in EBV-associated sHLH [69]. Furthermore, two patients with NLRC4-related disease and in one child with neonatal-onset cytopenia with dyshematopoiesis, autoinflammation, rash, and hemophagocytosis (NOCARH syndrome) have been successfully treated with emapalumab [70, 71]. An open-label phase II trial exploring efficacy and safety of emapalumab in sJIA-associated MAS is ongoing (ClinicalTrials.gov NCT03311854), with promising results.
Various other therapeutic agents for sHLH and MAS spectrum diseases are currently under evaluation. There is too little evidence to support the use of other IL-1 inhibitors, such as canakinumab or rilonacept in MAS, and the reason may be related to different mechanisms of action, under-dosing, or absence of enough clinical data. However, a successful use of canakinumab in two patients with impending MAS refractory to conventional treatment including anakinra has been recently reported [72]. Anti-IL-6 treatment has proven to be beneficial in cytokine release syndrome secondary to CAR T cell therapy or blinatumomab [73, 74], but there are limited data for its use outside of these settings. Due to its emerging role in promoting hyperferritinemic syndromes, IL-18 blocking is a potential target in MAS/sHLH. Indeed, recombinant human IL-18 binding protein effectively treated MAS in a patient with NLRC4 mutation [75]. Finally, inhibition of cytokine signaling via JAK-STAT inhibitors may potentially have a future role in treating sHLH/MAS. Ruxolitinib is a JAK1/2 inhibitor that blocks INFγ and IL-6 among other cytokines. In animal models of HLH, ruxolitinib has been demonstrated to improve the disease [76], and a successful use of ruxolitinib in refractory infection-related sHLH has been reported [77]. However, more data are needed to support a wider use of JAK inhibitors in sHLH/MAS.
Conclusion
MAS is a life-threatening inflammatory condition, belonging to the spectrum of hemophagocytic disorders, which, if inadequately treated, may lead to multiorgan failure and fatal outcome. Its timely recognition is often challenging, but recently developed diagnostic tools might aid physicians in clinical practice. The development of a universal set of criteria and the identification of biomarkers that may be applied to all different rheumatologic disorders will further optimize MAS diagnostic work-up. Progress in understanding the genetics and pathophysiology of MAS led to a significant improvement in the management of this condition. In the future, tailored therapy based on the underlying disorder, triggers, genetic predisposition, and biomarkers will likely ameliorate the outcome of MAS patients.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ravelli A, Davì S, Minoia F, Martini A, Cron RQ. Macrophage activation syndrome. Hematol Oncol Clin North Am. 2015;29:927–41 A exhaustive review of the diagnosis, genetics, pathophysiology, and treatment of MAS complicating sJIA.
Grom AA, Horne A, De Benedetti F. Macrophage activation syndrome in the era of biologic therapy. Nat Rev Rheumatol. 2016;12:259–68 An interesting update on MAS in the context of hemophagocytic syndromes, with a focus on pathophysiology and potential treatment targets.
Hadchouel M, Prieur AM, Griscelli C. Acute hemorrhagic, hepatic, and neurologic manifestations in juvenile rheumatoid arthritis: possible relationship to drugs or infection. J Pediatr. 1985;106:561–6.
Stéphan JL, Zeller J, Hubert P, Herbelin C, Dayer JM, Prieur AM. Macrophage activation syndrome and rheumatic disease in childhood: a report of four new cases. Clin Exp Rheumatol. 1993;11:451–6.
Ravelli A, Grom AA, Behrens EM, Cron RQ. Macrophage activation syndrome as part of systemic juvenile idiopathic arthritis: diagnosis, genetics, pathophysiology and treatment. Genes Immun. 2012;13:289–98.
Behrens EM, Beukelman T, Paessler M, Cron RQ. Occult macrophage activation syndrome in patients with systemic juvenile idiopathic arthritis. J Rheumatol. 2007;34:1133–8.
Bleesing J, Prada A, Siegel DM, Villanueva J, Olson J, Ilowite NT, et al. The diagnostic significance of soluble CD163 and soluble interleukin-2 receptor alpha-chain in macrophage activation syndrome and untreated new-onset systemic juvenile idiopathic arthritis. Arthritis Rheum. 2007;56(3):965–71.
Minoia F, Davì S, Horne A, Demirkaya E, Bovis F, Li C, et al. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a multinational, multicenter study of 362 patients. Arthritis Rheumatol. 2014;66:3160–9 The largest cohort of patients with sJIA-associated MAS described so far, with a particular focus on clinical manifestations at onset, laboratory change over time, treatment approaches and outcome.
Minoia F, Davì S, Horne A, Bovis F, Demirkaya E, Akikusa J, et al. Dissecting the heterogeneity of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Rheumatol. 2015;42:994–1001.
Borgia RE, Gerstein M, Levy DM, Silverman ED, Hiraki LT. Features, treatment, and outcomes of macrophage activation syndrome in childhood-onset systemic lupus erythematosus. Arthritis Rheumatol. 2018;70:616–24 The largest cohort of SLE-associated MAS described so far, including clinical features, treatment and outcome.
Latino GA, Manlhiot C, Yeung RSM, Chahal N, McCrindle BW. Macrophage activation syndrome in the acute phase of Kawasaki disease. J Pediatr Hematol Oncol. 2010;32:527–31.
Rossi-Semerano L, Hermeziu B, Fabre M, Koné-Paut I. Macrophage activation syndrome revealing familial Mediterranean fever. Arthritis Care Res (Hoboken). 2011;63:780–3.
Rigante D, Capoluongo E, Bertoni B, Ansuini V, Chiaretti A, Piastra M, et al. First report of macrophage activation syndrome in hyperimmunoglobulinemia D with periodic fever syndrome. Arthritis Rheum. 2007;56:658–61.
Ravelli A, Minoia F, Davì S, Horne AC, Bovis F, Pistorio A et al. Expert consensus on dynamics of laboratory tests for diagnosis of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. RMD Open. 2016;19(2):e000161 Results of an experts’ consensus on the role of dynamics laboratory change over time in sJIA-associated MAS.
Minoia F, Tibaldi J, Muratore V, Gallizzi R, Bracaglia C, Arduini A, et al. FRI0565 a multinational study of thrombotic microangiopathy in macrophage activation syndrome: a dreadful condition condition which is likely under-recognized. Ann Rheum Dis. 2019. https://doi.org/10.1136/annrheumdis-2019-eular.6199.
Sullivan KE, Delaat CA, Douglas SD, Filipovich AH. Defective natural killer cell function in patients with hemophagocytic lymphohistiocytosis and in first degree relatives. Pediatr Res. 1998;44:465–8.
Stepp SE, Dufourcq-Lagelouse R, Le Deist F, Bhawan S, Certain S, Mathew PA, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science. 1999;286:1957–9.
Feldmann J, Callebaut I, Raposo G, Certain S, Bacq D, Dumont C, et al. Munc13-4 is essential for cytolytic granules fusion and is mutated in a form of familial hemophagocytic lymphohistiocytosis (FHL3). Cell. 2003;115:461–73.
zur Stadt U, Rohr J, Seifert W, Koch F, Grieve S, Pagel J, et al. Familial hemophagocytic lymphohistiocytosis type 5 (FHL-5) is caused by mutations in Munc18-2 and impaired binding to Syntaxin 11. Am J Hum Genet. 2005;85:482–92.
zur Stadt U, Schmidt S, Kasper B, Beutel K, Diler AS, Henter J, et al. Linkage of familial hemophagocytic lymphohistiocytosis (FHL) type-4 to chromosome 6q24 and identification of mutations in syntaxin 11. Hum Mol Genet. 2005;14:827–34.
Jenkins MR, Rudd-Schmidt JA, Lopez JA, Ramsbottom KM, Mannering SI, Andrews DM, et al. Failed CTL/NK cell killing and cytokine hypersecretion are directly linked through prolonged synapse time. J Exp Med. 2015;212:307–17.
Grom AA, Villanueva J, Lee S, Goldmuntz EA, Passo MH, Filipovich A. Natural killer cell dysfunction in patients with systemic-onset juvenile rheumatoid arthritis and macrophage activation syndrome. J Pediatr. 2003;142:292–6.
Cruikshank M, Anoop P, Nikolajeva O, Rao A, Rao K, Gilmour K, et al. Screening assays for primary haemophagocytic lymphohistiocytosis in children presenting with suspected macrophage activation syndrome. Pediatr Rheumatol. 2005;13:48.
Put K, Vandenhaute J, Avau A, van Nieuwenhuijze A, Brisse E, Dierckx T, et al. Inflammatory gene expression profile and defective interferon-γ and granzyme K in natural killer cells from systemic juvenile idiopathic arthritis patients. Arthritis Rheumatol. 2017;69:213–24.
Vastert SJ, van Wijk R, D’Urbano LE, de Vooght KMK, de Jager W, Ravelli A, et al. Mutations in the perforin gene can be linked to macrophage activation syndrome in patients with systemic onset juvenile idiopathic arthritis. Rheumatology (Oxford). 2010;49:441–9.
Kaufman KM, Linghu B, Szustakowski JD, Husami A, Yang F, Zhang K, et al. Whole-exome sequencing reveals overlap between macrophage activation syndrome in systemic juvenile idiopathic arthritis and familial hemophagocytic lymphohistiocytosis. Arthritis Rheumatol. 2014;66:3486–95 A significant portion of sJIA patients with MAS were found to be heterozygous for HLH-related genes by WES analysis, supporting the hypothesis that mutations in HLH genes may contribute to MAS.
Zhang M, Behrens EM, Atkinson TP, Shakoory B, Grom AA, Cron RQ. Genetic defects in cytolysis in macrophage activation syndrome. Curr Rheumatol Rep. 2014;16:439.
Schulert GS, Zhang M, Fall N, Husami A, Kissell D, Hanosh A, et al. Whole-exome sequencing reveals mutations in genes linked to hemophagocytic lymphohistiocytosis and macrophage activation syndrome in fatal cases of H1N1 influenza. J Infect Dis. 2016;213:1180–8 Mutations in HLH-related genes were revealed in severe H1N1 patients with MAS features, promoting the hypothesis of a role of genetic predisposition also in secondary HLH.
Strippoli R, Carvello F, Scianaro R, De Pasquale L, Vivarelli M, Petrini S, et al. Amplification of the response to toll-like receptor ligands by prolonged exposure to interleukin-6 in mice: implication for the pathogenesis of macrophage activation syndrome. Arthritis Rheum. 2012;64:1680–8.
Cifaldi L, Prencipe G, Caiello I, Bracaglia C, Locatelli F, De Benedetti F, et al. Inhibition of natural killer cell cytotoxicity by interleukin-6: implications for the pathogenesis of macrophage activation syndrome. Arthritis Rheumatol. 2015;67:3037–46.
Jordan MB, Hildeman D, Kappler J, Marrack P. An animal model of hemophagocytic lymphohistiocytosis (HLH): CD8 T cells and interferon gamma are essential for the disorder. Blood. 2004;104:735–43.
Bracaglia C, De Graaf K, Marafon DP, Guilhot F, Ferlin W, Prencipe G, et al. Elevated circulating levels of interferon-γ and interferon-γ-induced chemokines characterize patients with macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. Ann Rheum Dis. 2017;76:166–72 The results of this study demonstrated the pivotal role of INFγ also in the pathogenesis of MAS and the potential importance of INFγ-induced chemokines as biomarkers for MAS diagnosis.
Shimizu M, Nakagishi Y, Inoue N, Mizuta M, Ko G, Saikawa Y, et al. Interleukin-18 for predicting the development of macrophage activation syndrome in systemic juvenile idiopathic arthritis. Clin Immunol. 2015;160:277–81.
Weiss ES, Girard-Guyonvarc’h C, Holzinger D, De Jesus AA, Tariq Z, Picarsic J, et al. Interleukin-18 diagnostically distinguishes and pathogenically promotes human and murine macrophage activation syndrome. Blood. 2018;131:1442–55 An in depth evaluation and demonstration of the different role of IL-18 in the pathogenesis of hyperferritinemic syndromes, and particularly as a promoter of MAS.
Canna SW, Almeida de Jesus A, Gouni S, Brooks SR, Marrero B, Liu Y, et al. An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat Genet. 2014;46:1140–6 Description of the first case of NLRC4-related autoinflammatory diseases, suggesting a cross-link between NLRC4 inflammasome activation and MAS pathogenesis.
Schulert GS, Canna SW. Convergent pathways of the hyperferritinemic syndromes. Int Immunol. 2018;30:195–203 An updated and in depth review of the pathophysiology of hyperferritinemic syndromes, suggesting the hypothesis of a convergence of impaired cytotoxic function and cytokine overproduction in the development of MAS and sHLH.
Henderson LA, Cron RQ. Macrophage activation syndrome and secondary Hemophagocytic Lymphohistiocytosis in childhood inflammatory disorders: diagnosis and management. Pediatr Drugs. 2020;22:29–44.
Strippoli R, Caiello I, De Benedetti F. Reaching the threshold: a multilayer pathogenesis of macrophage activation syndrome. J Rheumatol. 2013;40:761–7 This study advanced the key hypothesis of a multilayer or threshold mechanism in the pathogenesis of MAS, in which different pathways might contribute to the development of the syndrome, converging on a final common way.
Aricò M, Janka G, Fischer A, Henter JI, Blanche S, Elinder G, et al. Hemophagocytic lymphohistiocytosis. Report of 122 children from the international registry. FHL Study Group of the Histiocyte Society Leukemia. 1996;10:197–203.
Ho C, Yao X, Tian L, Li F-Y, Podoltsev N, Xu ML. Marrow assessment for hemophagocytic lymphohistiocytosis demonstrates poor correlation with disease probability. Am J Clin Pathol. 2014;141:62–71.
Henter JI, Horne AC, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31 The 2004 protocol for the diagnosis and treatment of HLH, developed by the Histiocyte Society.
Davì S, Minoia F, Pistorio A, Horne AC, Consolaro A, Rosina S, et al. Performance of current guidelines for diagnosis of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2014;66:2871–80.
Ravelli A, Minoia F, Davì S, Horne AC, Bovis F, Pistorio A, et al. 2016 Classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European league against rheumatism/American college of rheumatology/Paediatric rheumatology international trials organisation collaborat. Ann Rheum Dis. 2016;75:481–9 The study that led to the development and validation ACR/EULAR/PRINTO classification criteria for defining MAS in the context of sJIA.
Ravelli A, Minoia F, Davì S, Horne AC, Bovis F, Pistorio A, et al. 2016 Classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a european league against rheumatism/American college of rheumatology/Paediatric rheumatology international trials organisation collaborative initiative. Arthritis Rheumatol. 2016;68:566–76.
Shimizu M, Mizuta M, Yasumi T, Iwata N, Okura Y, Kinjo N, et al. Validation of classification criteria of macrophage activation syndrome in japanese patients with systemic juvenile idiopathic arthritis. Arthritis Care Res. 2018;70:1412–5.
Schulert GS, Minoia F, Bohnsack J, Cron RQ, Hashad S, Konè-Paut I, et al. Effect of biologic therapy on clinical and laboratory features of macrophage activation syndrome associated with systemic juvenile idiopathic arthritis. Arthritis Care Res. 2018;70:409–19.
Shimizu M, Mizuta M, Okamoto N, Yasumi T, Iwata N, Umebayashi I, et al. Tocilizumab modifies clinical and laboratory features of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2020;18:2.
Minoia F, Bovis F, Davì S, Horne AC, Fischbach M, Frosch M et al. Development and initial validation of the MS score for diagnosis of macrophage activation syndrome in systemic juvenile idiopathic arthritis. Ann Rheum Dis 2019;78:1357–1362 This study led to the development and validation of a diagnostic score (MS score) to timely detect MAS in sJIA patients.
Pringe A, Trail L, Ruperto N, Buoncompagni A, Loy A, Breda L, et al. Macrophage activation syndrome in juvenile systemic lupus erythematosus: an under-recognized complication? Lupus. 2007;16:587–92.
Parodi A, Davì S, Pringe AB, Pistorio A, Ruperto N, Magni-Manzoni S, et al. Macrophage activation syndrome in juvenile systemic lupus erythematosus: a multinational multicenter study of thirty-eight patients. Arthritis Rheum, This study proposed the preliminary diagnostic criteria for detecting MAS in the context of SLE. 2009;60:3388–99.
Ravelli A, Magni-Manzoni S, Pistorio A, Besana C, Foti T, Ruperto N, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005;146:598–604.
Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, et al. Development and validation of the Hscore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613–20 The study that led to the development and validation of the Hscore, a diagnostic score for the recognition of reactive hemophagocytic syndromes in adults.
Eloseily EMA, Minoia F, Crayne CB, Beukelman T, Ravelli A, Cron RQ. Ferritin to erythrocyte sedimentation rate ratio: simple measure to identify macrophage activation syndrome in systemic juvenile idiopathic arthritis. ACR Open Rheumatol, This study suggests an useful screening measure to recognize MAS in sJIA and distinguish hemophagocytic syndromes from other febrile conditions. 2019;1:345–9.
Degar B. Familial Hemophagocytic Lymphohistiocytosis. Hematol Oncol Clin North Am. 2015;29:903–13.
Minoia F, Bovis F, Davì S, Insalaco A, Lehmberg K, Shenoi S, et al. Development and initial validation of the macrophage activation syndrome/primary hemophagocytic lymphohistiocytosis score, a diagnostic tool that differentiates primary hemophagocytic lymphohistiocytosis from macrophage activation syndrome. J Pediatr. 2017;189:72–78.e3 The MH score is a validated tool to identify, in patients with an hemophagocytic syndrome, those with the higher risk to have a primitive form of HLH.
Ravelli A, De Benedetti F, Viola S, Martini A. Macrophage activation syndrome in systemic juvenile rheumatoid arthritis successfully treated with cyclosporine. J Pediatr. 1996;128:275–8.
Stéphan JL, Koné-Paut I, Galambrun C, Mouy R, Bader-Meunier B, Prieur AM. Reactive haemophagocytic syndrome in children with inflammatory disorders. A retrospective study of 24 patients. Rheumatology. 2001;40:1285–92.
Kelly A, Ramanan AV. A case of macrophage activation syndrome successfully treated with anakinra. Nat Clin Pract Rheumatol. 2008;4:615–20.
Miettunen PM, Narendran A, Jayanthan A, Behrens EM, Cron RQ. Successful treatment of severe paediatric rheumatic disease-associated macrophage activation syndrome with interleukin-1 inhibition following conventional immunosuppressive therapy: case series with 12 patients. Rheumatol. 2010;50:417–9.
Bruck N, Suttorp M, Kabus M, Heubner G, Gahr M, Pessler F. Rapid and sustained remission of systemic juvenile idiopathic arthritis-associated macrophage activation syndrome through treatment with anakinra and corticosteroids. J Clin Rheumatol. 2011;17:23–7.
Kahn PJ, Cron RQ. Higher-dose anakinra is effective in a case of medically refractory macrophage activation syndrome. J Rheumatol. 2013;40:743–4.
Eloseily EM, Weiser P, Crayne CB, Haines H, Mannion ML, Stoll ML, et al. benefit of anakinra in treating pediatric secondary hemophagocytic lymphohistiocytosis. Arthritis Rheumatol. 2020;72:326–34 A large case-series which analyse the effectiveness of anakinra in secondary HLH.
Lurati A, Terruzi B, Salmaso A, Demarco G, Pontikaki I, Gattinara M, et al. Macrophage activation syndrome (MAS) during anti-IL1 receptor therapy (anakinra) in a patient affected by Systemic Onset Idiopathic Juvenile Arthritis (SOJIA): a report and review of the literature. Pediatr Rheumatol Online J. 2015;3:79–85.
Zeft A, Hollister R, Lafleur B, Sampath P, Soep J, McNally B, et al. Anakinra for systemic juvenile arthritis: the rocky mountain experience. J Clin Rheumatol. 2009;15:161–4.
Nigrovic PA, Mannion M, Prince FHM, Zeft A, Rabinovich CE, Van Rossum MAJ, et al. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum. 2011;63:545–55.
Put K, Avau A, Brisse E, Mitera T, Put S, Proost P, et al. Cytokines in systemic juvenile idiopathic arthritis and haemophagocytic lymphohistiocytosis: tipping the balance between interleukin-18 and interferon-γ. Rheumatol. 2015;54:1507–17.
Prencipe G, Caiello I, Pascarella A, Grom AA, Bracaglia C, Chatel L, et al. Neutralization of IFN-γ reverts clinical and laboratory features in a mouse model of macrophage activation syndrome. J Allergy Clin Immunol. 2018;141:1439–49.
Locatelli F, Jordan MB, Allen C, Cesaro S, Rizzari C, et al. Emapalumab in children with primary Hemophagocytic Lymphohistiocytosis. N Engl J Med. 2020 May 7;382(19):1811–22. https://doi.org/10.1056/NEJMoa1911326.
Lounder DT, Bin Q, de Min C, Jordan MB. Treatment of refractory hemophagocytic lymphohistiocytosis with emapalumab despite severe concurrent infections. Blood Adv. 2019;3:47–50.
Bracaglia C, Prencipe G, Insalaco A, Caiello I, Marucci G, Pecoraro R, et al. Emapalumab, an anti-interferon gamma monoclonal antibody in two patients with NLRC4-related disease and severe hemophagocytic lymphohistiocytosis (HLH) [abstract]. Arthritis Rheumatol. 2018;70(suppl 9):1547.
Lam MT, Coppola S, Krumbach OH, Prencipe G, Insalaco A, Cifaldi C, et al. FRI0540 a novel autoinflammatory disease characterized by neonatal-onset cytopenia with autoinflammation, rash, and hemophagocytosis (NOCARH) due to aberrant CDC42 function [abstract]. Ann Rheum Dis. 2019;78(suppl 2):964.
Papa R, Natoli V, Caorsi R, Minoia F, Gattorno M, Ravelli A. Succesfull treatment of refractory hyperferritinemic syndromes with canakinumab: a report of two cases. Pediatr Rheumatol Online. in press.
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371:1507–17.
Teachey DT, Rheingold SR, Maude SL, Zugmaier G, Barrett DM, Seif AE, et al. Cytokine release syndrome after blinatumomab treatment related to abnormal macrophage activation and ameliorated with cytokine-directed therapy. Blood. 2013;121:5154–7.
Canna SW, Girard C, Malle L, de Jesus A, Romberg N, Kelsen J, et al. Life-threatening NLRC4-associated hyperinflammation successfully treated with IL-18 inhibition. J Allergy Clin Immunol. 2017;139:1698–701.
Das R, Guan P, Sprague L, Verbist K, Tedrick P, An QA, et al. Janus kinase inhibition lessens inflammation and ameliorates disease in murine models of hemophagocytic lymphohistiocytosis. Blood. 2016;127:1666–75.
Slostad J, Hoversten P, Haddox CL, Cisak K, Paludo J, Tefferi A. Ruxolitinib as first-line treatment in secondary hemophagocytic lymphohistiocytosis: a single patient experience. Am J Hematol. 2018;93:E47–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roberta Caorsi declares consultancy fees from Novartis, Sobi, and Eli Lilly. Francesca Minoia declares consultancy and speaker fees from Sobi SR L. Francesco Baldo declares that he has no conflict of interest. Gisella Beretta declares that she has no conflict of interest. Jessica Tibaldi declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Baldo, F., Beretta, G., Tibaldi, J. et al. Macrophage Activation Syndrome in Childhood Inflammatory Disorders: Diagnosis, Genetics, Pathophysiology, and Treatment. Curr Treat Options in Rheum 6, 245–259 (2020). https://doi.org/10.1007/s40674-020-00153-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-020-00153-y