Abstract
Purpose of review
Chronic non-bacterial osteomyelitis (CNO) is an autoinflammatory bone disease most prevalent in children. In this review, we seek to highlight the most recent advances in the understanding of the pathophysiology, treatment, and outcomes of CNO.
Recent findings
Recent observations support a pathophysiologic framework involving imbalanced expression of pro-inflammatory versus anti-inflammatory cytokines, thereby inducing increased differentiation and activation of osteoclasts. Although no medication nor protocol is yet specifically indicated in the treatment of CNO, there exists an expanding body of evidence for agents exerting their effects via interference with these pro-inflammatory pathways (namely non-steroidal anti-inflammatory drugs, disease-modifying anti-rheumatic drugs, bisphosphonates, and biologics), highlighted herein.
Summary
With an incidence rivaling that of bacterial osteomyelitis, childhood CNO represents an important and growing field of study. Once thought to be benign and self-limiting, CNO is now recognized to follow a relapsing and remitting course in the majority of children, and to carry substantial risk of irreversible growth and bone sequelae. Perhaps of greatest importance to the study of CNO treatment is the recent development of the Childhood Arthritis and Rheumatology Research Alliance (CARRA) consensus treatment plans, the implementation of which will allow for prospective comparative effectiveness studies and, ultimately, the development of standardized treatment protocols.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
First described in 1972 by Gideon et al. as “subacute and chronic symmetrical osteomyelitis,” chronic non-bacterial osteomyelitis (CNO) is an autoinflammatory bone disease most prevalent in children [1]. While terminology remains inconsistent across the literature, we apply CNO to describe a spectrum of sterile bone inflammation irrespective of chronicity and lesional distribution, with chronic recurrent multifocal osteomyelitis (CRMO; implying chronicity and/or recurrence and multiple sites of involvement) as its most severe form [2•, 3••].
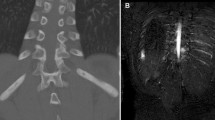
Primarily affecting the metaphyses of long bones, clavicles, mandible, pelvic bones, and (of particular clinical importance) vertebral bodies, CNO generally presents with localized bone pain and imaging findings of osteolysis, sclerosis, and hyperostosis on plain radiographs and bone marrow edema on magnetic resonance imaging (MRI) [2•, 4, 5]. One recent study suggests two predominant radiographic patterns of disease—“tibio-appendicular multifocal” and “claviculo-spinal paucifocal.” In their cohort, only 14% were found to have concomitant involvement of the clavicles and tibiae [6]. Additional extraosseous inflammation, most commonly involving the skin (palmoplantar pustulosis [PPP], acne, psoriasis), joints, and gut, is frequently associated [2•, 3••, 5, 7]. SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome is sometimes considered the adult form of CNO, although this constellation also occurs in adolescence [2•, 3••, 4, 8]. Furthermore, well-described associations with systemic inflammatory illnesses (e.g., inflammatory bowel disease, spondyloarthropathy) likely represent varying phenotypes along the same disease spectrum [4].
Considered an orphan disease with a cited incidence of 0.4 per 100,000 children, recent data suggest that CNO is far more common than previously appreciated: one study of 105 children with osteomyelitis (bacterial and non-infectious) determined near-identical incidences of CNO and bacterial osteomyelitis [9, 10]. This discrepancy likely arises from an increased awareness of inflammatory bone disease and related conditions, as outlined above, and an evolving appreciation of autoinflammation as a whole.
Described complications of CNO include pathologic fracture (most commonly of the vertebral bodies), kyphosis, leg-length discrepancy and other local deformity, and growth impairment secondary to premature epiphyseal fusion. As in many systemic inflammatory illnesses, amplified musculoskeletal pain may be an important comorbidity or complication with significant psychosocial impact [4].
Published in this journal in 2017, Zhao et al. provide a comprehensive overview of treatment options in CNO [4]. In this review, although we present the historical context for and previously reported experience with current therapies, we aim primarily to highlight the most recent advances (subsequent to 2017) in the understanding of the pathophysiology, treatment, and outcomes of CNO.
Making the diagnosis
Much as our ability to detect sterile bone inflammation grows, bolstered chiefly by the widened availability of advanced imaging techniques such as whole-body short tau inversion recovery (STIR) MRI, CNO remains a diagnosis of exclusion. Principal alternative considerations include infectious osteomyelitis, malignancy (e.g., leukemia, lymphoma, primary and metastatic osseous tumors), and Langerhans cell histiocytosis [2•, 11••]. Traditionally, clinicians have been reliant on bone biopsy to confidently exclude these possibilities.
There exist a number of proposed diagnostic criteria for pediatric CNO, two of which we highlight below. None has yet been universally adopted in clinical practice. In 2007, Jansson et al. delineated major (radiologically proven osteolytic/sclerotic bone lesion; multifocal bone lesions; PPP or psoriasis; sterile bone biopsy with signs of inflammation and/or fibrosis, sclerosis) and minor (normal blood count and good general state of health; C-reactive protein [CRP] and erythrocyte sedimentation rate [ESR] mildly-to-moderately elevated; observation time longer than 6 months; hyperostosis; associated with other autoimmune diseases apart from PPP or psoriasis; first or second degree relative with autoimmune or autoinflammatory disease, or with CNO) criteria; the threshold for diagnosis set at two major or one major and three minor criteria [12]. Roderick et al. have since proposed a simplified set of criteria, at times referenced as the “Bristol Criteria”: presence of typical clinical findings (bone pain with or without localized swelling without significant local or systemic features of inflammation or infection) and typical radiographic findings (plain x-ray [showing combination of lytic areas, sclerosis and new bone formation] or preferably STIR MRI [showing bone marrow edema with or without bone expansion, lytic areas, and periosteal reaction]) and either more than one bone (or clavicle alone) without significantly raised CRP (< 30 g/L); or, if unifocal disease (other than clavicle) or CRP > 30 g/L, with bone biopsy showing inflammatory changes (plasma cells, osteoclasts, fibrosis, or sclerosis) without bacterial growth while not on antibiotic therapy) [13].
Perhaps of greatest clinical impact, Jansson et al. later suggested a clinical score for patients with suspected CNO to discriminate those for whom clinical diagnosis is sufficient from those requiring histopathologic evaluation. In their development cohort, CNO was associated with normal blood cell count (13 points); symmetric bone lesions (10 points); lesions with marginal sclerosis (10 points); normal body temperature (9 points); a vertebral, clavicular, or sternal location of lesions (8 points); presence of > 1 radiologically proven lesion (7 points); and CRP > 1 mg/dL (6 points). A score of ≥ 39 yielded a positive predictive value of 97%. Bone biopsy is recommended in patients with unifocal disease and a score of ≤ 28, or in the context of negative bone scintigraphy [14].
Pathophysiology and monogenic CNO
It is now clear that immune dysregulation is central to the development of CNO. In keeping with an autoinflammatory model of disease (idiopathic inflammation with primary involvement of the innate immune system in the absence of high-titer antibodies and autoreactive lymphocytes), disruption in cytokine and chemokine expression is most apparent in monocytes and macrophages [2•]. At present, however, no single causative mechanism has been identified. While in-depth discussion of the immune pathways thus far implicated in CNO is beyond the scope of this review (see Table 1), the following summative framework is supported by recent observations: imbalanced expression of pro-inflammatory (interleukin [IL]-1, IL-6, tumor necrosis factor [TNF]-α, IL-20) versus anti-inflammatory (IL-10 and IL-19) cytokines may induce increased differentiation and activation of osteoclasts via enhanced interaction of receptor activator of nuclear factor-κΒ (RANK) and its soluble ligand RANKL [2•, 15, 16, 17•, 18,19,20].
Compatible with the above model, the familial monogenic disorders Majeed syndrome (involving LPIN2), deficiency of interleukin-1 receptor antagonist (DIRA; involving IL1RN), and pyogenic arthritis, pyoderma gangrenosum, and acne syndrome (PAPA; involving PSTPIP1) all display increased IL-1 signalling and inflammasome activity and result in severe sterile osteomyelitis [2•, 20]. Recently, mutations in the FBLIM1 gene, the expression of which is implicated in the balance between osteoclast bone resorption and osteoblast bone formation, were reported in two families affected by CNO [21•].
Treatment
Diet and lifestyle
The influence of environment on cytokine production and circulating mediators of inflammation represents a rapidly evolving field of study. Interindividual differences in cytokine responses can in part be attributed to interactions between the human immune system, microbial organisms, and their metabolites [22, 23]. Diet and microbiome have long been implicated as putative mediators of the global rise in chronic inflammatory disease. Specifically relevant to inflammatory bone disease, mice deficient of proline-serine-threonine phosphatase-interacting protein 2 (Pstpip2) develops sterile bone inflammation, inflammatory skin disease, and elevations in neutrophil-attracting chemokines and IL-1β, a phenotype strongly resembling CNO [24]. Lukens et al. suggest that dietary modification of the microbiome (namely via diets rich in fat and cholesterol) in Pstpip2-deficient mice may be protective against osseous inflammation via regulation of IL-1β maturation [25]. Moreover, pro-IL-1β production was observed to be decreased in Pstpip2-deficient mice treated with antibiotics, potentially via alteration of the gut microbiome; this may inform the partial, albeit transient, effectiveness of antibiotic therapy in CNO [25,26,27]. Unfortunately, no compelling data exist to support specific dietary intervention in the treatment or prevention of human inflammatory bone disease. This warrants further study.
Pharmacologic treatment
Although our understanding of disease pathogenesis continues to evolve, current pharmacologic treatment strategies for CNO remain empiric, based largely on clinician experience, expert opinion, and non-experimental studies—there remains of definitive lack of clinical trials (Table 2) [2•]. Perhaps of greatest importance to the ongoing and future study of CNO treatment is the recent development of the Childhood Arthritis and Rheumatology Research Alliance (CARRA) consensus treatment plans (CTPs) for CNO refractory to non-steroidal anti-inflammatory drugs (NSAIDs) and/or with spinal lesions, the implementation of which will allow for prospective comparative effectiveness studies [11••]. Therefore, when relevant and available, recommended dosing within this review will refer to that delineated in the CARRA CTPs (Fig. 1). Note that the dosing of disease-modifying anti-rheumatic drugs (DMARD) and biologic therapies is inferred from standard dosing regimens in juvenile idiopathic arthritis (JIA) [11••].
Childhood Arthritis and Rheumatology Research Alliance (CARRA) consensus treatment plans for chronic non-bacterial osteomyelitis refractory to non-steroidal anti-inflammatory drugs and/or with spinal lesions (reference [11]). CNO chronic non-bacterial osteomyelitis, NSAID non-steroidal antiinflammatory drug, DMARD disease-modifying anti-rheumatic drug, MTX methotrexate, SSZ sulfasalazine, TNF tumor necrosis factor, ETN etanercept, IFX infliximab, ADA adalimumab
Paralleling the lack of consensus diagnostic criteria, there exists no established definition of response to therapy in CNO [3••]. No single standardized disease monitoring or assessment tool is yet broadly applied in the clinical setting. Derived from the American College of Rheumatology (ACR) Pediatric Core Set Measures for JIA, itself a derivation of a composite measure of treatment response in rheumatoid arthritis, Beck et al. propose the PedCNO score, calculated from a core set of outcome variables: ESR, number of radiographic lesions, severity of disease estimated by the physician, severity of disease estimated by the patient or parent, and the childhood health assessment questionnaire (CHAQ). Response is defined as follows: PedCNO 30 (50, 70) implies at least 30% (50%, 70%) improvement in at least three core set variable with no more than one of the remaining variables decreased by greater than 30% (50%, 70%) [28]. Zhao et al. propose an MRI-based scoring tool comprising the number unique inflammatory lesions, bone edema severity, total lesion number with periosteal reaction, total lesion number with hyperostosis, bony bar severity, vertebral compression severity, soft tissue inflammation severity, and number of joints with arthritis [29].
The CARRA CTPs define treatment failure at 3 months when a patient fails to improve in ≥ 4/6 of the following criteria or in > 50% of applicable criteria (if not all available): patient pain as measured by visual analog scale (VAS); total number of clinically active lesions (defined as a body part with focal tenderness, and/or swelling, and/or warmth in addition to patient’s report of pain at a known CNO lesion sit); number of radiologic lesions by whole-body MRI or bone scintigraphy; size and degree of bone marrow edema of CNO lesions and/or presence of soft tissue swelling/inflammation related to CNO lesion on imaging; physician VAS; abnormal ESR (≥ 20 mm/h) and/or CRP (≥ 1 mg/dl) level after exclusion of other potential causes [11••]. Of note, the CHAQ, included in the PedCNO core set, is deliberately excluded as it exhibits a floor effect at 3 months [11••, 28]. Treatment success is defined by the CARRA CTPs as resolution of pain, normalization of inflammatory markers, and resolution of bone marrow edema on MRI [5, 11••, 30].
At present, no medication is specifically approved for use in CNO. Despite this, the pharmacologic landscape of CNO treatment is encouraging. Although limited by its retrospective nature and reliance on registry (and therefore at times incomplete) data, the Eurofever international registry database study, published in 2018, is the largest reported case series of CNO to date (486 patients). Within this expansive group, positive response (as elaborated below) was observed with bisphosphonates, NSAIDs, glucocorticoids, and sulfasalazine in 91, 91, 92, and 87%, respectively (3, Class IV).
Non-steroidal anti-inflammatory drugs
NSAIDs remain the most commonly employed first-line agents for patients without active spinal lesions. In a recent survey of CARRA members, 95% of treating physicians reported using NSAIDs as first-line treatment in patients newly diagnosed with CNO [11••]. Although primarily exerting their anti-inflammatory effects via cyclooxygenase (COX) inhibition, NSAIDs have recently been shown to suppress inflammasome activity, and therefore pro-inflammatory cytokine production implicated in CNO’s pathogenesis, independent of COX enzymes [2•, 31].
In the Eurofever study, 74% received NSAIDs, 39% of whom achieved complete remission (denoted as resolution of pain, and normalization of inflammatory markers [ESR and CRP] and imaging abnormalities [allowing for 1–2 foci of asymptomatic bone marrow edema on MRI]). Fifty-two percent achieved partial response, and 9% were classified as non-responders [3••].
Wipff et al. previously described 178 patients with CNO, 97% of whom received NSAIDs as first-line therapy. Improvement in symptoms was noted by the treating physician in 71% (30, Class IV). The effectiveness of NSAIDs in alleviating symptoms is well documented, with most studies reporting pain relief within 1 month of treatment (response rate ranging from 51 to 100%) [4]. It is important to note, however, that symptomatic relief does not necessarily imply resolution of subclinical inflammatory disease and the prevention of resultant osseous damage. Carr et al. described the radiographic pattern of healing in 22 pediatric patients with CNO treated with NSAID (in addition to antibiotic) therapy and found variable residual bone sclerosis, expansion, and vertebral body collapse (with one patient developing progressive kyphosis) [32]. Moreover, Beck et al. reported a case series in which 2/7 patients with vertebral disease treated with naproxen developed pathologic fractures [28].
Overall, NSAID monotherapy has been less successful in inducing complete remission as defined above (range 13 to 77%) [4, 33]. Via the lone published prospective treatment study of CNO, in which 37 patients were treated with naproxen continuously for 6 months (following which sulfasalazine and short-term corticosteroids were added to continued naproxen for an additional 6 months if progressive disease or no further improvement were noted), Beck et al. found that naproxen at doses of 15 mg/kg/day induced symptom-free status in 43% at 6 months. However, only 14% were found to be in radiologic remission (absence of lesions on MRI) at the same time point (28, Class IV). The authors appropriately conclude that most children show a favorable clinical course in the first year of treatment with NSAIDs, although 30–40% may require additional therapies.
Regarding the specific choice of NSAID, there exists a dearth of comparative studies between commonly employed agents. Naproxen is most frequently used, although no data exists to support this preference. As noted by Zhao et al., small cohort studies suggest similar efficacy between indomethacin and diclofenac [4, 34, 35].
Of note, per the CARRA consensus treatment plan, a patient is defined to be refractory to NSAID therapy if he or she remains symptomatic following a minimum of 4 weeks of therapy, at which point second-line treatment, the options for which are outlined below, is considered [11••].
Glucocorticoids
As with NSAIDs, corticosteroids suppress prostaglandin production (via phospholipase A1 inhibition). Additionally, corticosteroids diminish nuclear factor-κΒ (NFκB)–mediated pro-inflammatory cytokine (namely IL-1, IL-6, TNF-α) production [2•, 18]. While effective in rapidly abating inflammatory disease activity, their use is generally limited to short oral bursts (e.g., 2 mg/kg/day prednisone equivalent for 5–10 days) for acute disease flare or to low-dose prednisone equivalent (e.g., 0.1–0.2 mg/kg/day) as bridging therapy until alternate steroid-sparing agents are successfully employed [2•]. Note that the CARRA CTPs limit such “bursts” to a maximum of 6 weeks with or without tapering [11••]. In considering the myriad of potential adverse effects of prolonged corticosteroid exposure (namely decreased bone mineral density, avascular necrosis), particular caution is warranted when treating patients with CNO, wherein osteoclast overactivity is central to pathogenesis.
Regarding their efficacy, complete response to corticosteroids was found in 37% and partial response in 54% of patients within the Eurofever study; no response was noted in 8% [3••]. Borzutzky and colleagues also describe a clinical remission rate of 37%, although detailed follow-up information for this cohort is lacking (5, Class IV).
Disease-modifying anti-rheumatic drugs
As noted in the CARRA CTPs, use of DMARD therapies is reported with variable success and is limited to level IV evidence [11••]. Generally, these treatments are reserved for those with inadequate response to NSAIDs. Overall, remission rate is relatively poor (below 40%), and intolerance to methotrexate (largely due to gastrointestinal adverse effects) is broadly reported [4]. The CARRA CTPs will be critical to the development of standardized studies evaluating the efficacy of DMARDs in CNO.
Methotrexate (MTX)
Complete remission using MTX was achieved in approximately 40% of patients with CNO in a recent study, notably higher than previously reported (20% by Borzutzky et al., 22% in the Eurofever study); however, the authors note that this may be explained by a high prevalence (67.3%) of concomitant systemic rheumatologic disease, namely arthritis, in their cohort [3••, 5, 36].
Importantly, in comparing the relative effectiveness of available therapies in inducing disease remission, Girschick et al. found statistically significant differences between glucocorticoids and MTX, as well as between bisphosphonates and MTX, suggesting perhaps a lesser relative therapeutic effect of MTX. Further supporting this, the rate of non-response was lower with glucocorticoids and bisphosphonates as compared with MTX [3••].
Sulfasalazine (SSZ)
Sulfasalazine (SSZ), although included in the CARRA CTPs, is less frequently employed relative to other DMARD or bisphosphonate therapies—in 9.6% of patients in the Eurofever registry, 31.4% in the Borzutzky cohort, and most recently 13.5% observed by Kostik et al.—and is most commonly chosen in the context of comorbid inflammatory bowel disease or enthesitis-related arthritis, influenced perhaps by a presumed common pathophysiology [3••,5, 33]. In Kostik’s 52 patients, 57.1% achieved complete remission (as previously defined) with SSZ, as compared with 52.6% with NSAID, 44.4% with methotrexate, 88.8% with pamidronate, and 73.3% with TNF-α inhibitors [36]. This is significantly greater than the remission rate (38%) achieved with SSZ in the Eurofever study [3••]. Once more, the high prevalence of associated arthritis (including enthesitis-related arthritis, inflammatory bowel disease, and psoriatic arthritis) among Kostik’s cohort must be considered.
Bisphosphonates
Pamidronate binds to bone and is internalized by osteoclasts, reducing their activity via induction of apoptosis and interference with regulatory protein signalling [37]. Pamidronate has also been demonstrated, in vitro, to inhibit macrophage function and pro-inflammatory cytokine secretion (particularly IL-lβ, IL-6, and TNF-α), thereby exerting anti-inflammatory effects [38]. Interestingly, despite these in vitro findings, no significant clinical effect on CNO-associated arthritis/synovitis has been observed [39•].
Despite its preferential application in patients with more severe disease (particularly that affecting the spine), pamidronate has been noted in some studies to be the most effective of available treatments (88.8% complete remission demonstrated by Kostik et al., 83% by Schnabel et al.) [33, 40]. This is in slight contrast to the Eurofever study, in which 51% of patients treated with bisphosphonates achieved complete response, 46% partial response, and 3% no response [3••].
There is also some suggestion that early and sustained use of pamidronate may improve clinical and radiologic disease activity in multifocal and NSAID-resistant CNO. In their 2019 study, Andreasen et al. studied treatment with a standardized regimen of intravenous pamidronate 1 mg/kg/day (maximum 60 mg/day) for 3 consecutive days every 3 months (first dose in the first series 0.5 mg/kg/day) continued for 2 years in all patients with extended CNO, defined as symmetric multifocal or spinal bone inflammation on MRI and poor clinical response to NSAID therapy. Of note, use of additional immunomodulatory therapies was permitted. Thirty-eight percent achieved clinically inactive disease (asymptomatic, normal ESR) at 1 year; however, 42% experienced clinical relapse at year 2 following medication discontinuation, and 67% experienced flare during the follow-up period. Thirty-two percent attained radiologic remission at 2 years (39, Class IV). More recently, Sułko et al. report a series of 41 NSAID-resistant patients with CNO treated with pamidronate (1 mg/kg/day for 3 days every 3 months). Thirty-two (78%) achieved remission (resolution of symptoms and radiologic lesions) following a mean of 7 infusion cycles (range 1–17) over 20 months. No adverse effects are described (41, Class IV).
Concerning alternative bisphosphonate agents, Zhao et al. found that a single dose of zoledronic acid (ZOL; approximately one hundredfold more potent than pamidronate) as an adjunct to combination infliximab (IFX) and MTX in patients with spinal involvement resulted in clinical and radiographic improvement. Importantly, the study was not designed to address the individual efficacy of ZOL (29, Class IV). There remains insufficient evidence, limited to case reports, to support the use of alendronate in CNO, despite the pragmatic allure of oral bisphosphonate formulations [42].
Reported adverse effects include bone pain, headache, fever, and electrolyte abnormalities (particularly hypocalcemia; patients should be calcium replete prior to therapy). Due to the rare complication of osteonecrosis of the jaw, which has not been reported in the pediatric population, it is advised that all patients be assessed by a dentist prior to treatment, and that no dental extractions be performed within 4 months of receiving bisphosphonates [41].
Biologics
Although the use of biologics in CNO has become increasingly common, there remains a paucity of published data to support their use. Once more, the Eurofever study provides perhaps the most robust information.
Anti-TNF-α
TNF-α blocking agents, most often initiated following inadequate response to NSAIDs and possibly bisphosphonates and/or DMARDs, are the most common biologic medications used in CNO. Their prevalence of use reported by CARRA physician members was 26% for both adalimumab (ADA) and IFX and 17% for etanercept (ETN)—all three are included in the CARRA CTPs [11••]. Of Eurofever registry patients, 3.5% received ETN, followed by IFX (1.8%) and ADA (1.6%) [3••].
Borzutzky et al. included 11 children treated with TNF-α inhibition (7 ETN, 2 ADA, 5 IFX) in their cohort. Collectively, 46% achieved clinical remission, an efficacy greater than that of NSAIDs (13%), glucocorticoids (37%), MTX (20%), and SSZ (18%). Perhaps more notable, 10/11 demonstrated partial or complete response [4, 5].
Within the Eurofever study, 41% of patients treated with ETN (total 17 patients) demonstrated complete response, 29% partial response, and 29% no response. With IFX (total 9 patients), 33% achieved complete response, 44% partial response, and 22% no response. Lastly, with ADA (total 8 patients), 50% attained complete, 50% partial, and zero no response [3••].
Overall, TNF-α blockade has been quite successful in the treatment of NSAID-resistant CNO, most notably in patients with concomitant extraosseous inflammation (e.g., arthritis, inflammatory bowel disease, psoriasis) for which anti-TNF-α medications are otherwise indicated [36].
Anti-IL-1
Data regarding the use of anti-IL-1 therapy in non-familial CNO are generally limited to case reports with mixed response. Pardeo et al. report a cohort of 9 patients with refractory CNO (unsatisfactory response to NSAIDs and bisphosphonates) treated with anakinra, 5 of whom were deemed to exhibit favorable response (physician global assessment from none to minimal based on fever, number of active bone lesions detected by bone scintigraphy, inflammatory marker elevation, and presence of pain and functional impairment) within the first 6 months of therapy [43]. The Eurofever registry includes four patients (0.8% of the total cohort) treated with anakinra, 2 of whom attained remission, 1 achieved partial response, and 1 demonstrated no response [3••]. It is not clear that early response to anti-IL-1 therapy is sustained—Eleftheriou et al. describe a 6-year-old girl with multifocal disease refractory to NSAIDs and pamidronate treated with anakinra, initially with resolution of symptoms and normalization of inflammatory markers at 6 weeks, who subsequently re-developed active disease at 12 months [44].
In contrast to the above, the central role of IL-1 blockade in the treatment of monogenic CNO directly involving dysregulated IL-1 production (Majeed syndrome, DIRA) is well established [4, 45, 46].
Anti-IL-6
There does not yet exist substantive evidence to support the use of anti-IL-6 agents in CNO. Sato et al. report improvement in symptoms, inflammatory markers, and imaging abnormalities using tocilizumab in 2 adult patients with CNO, polyarthritis, and lower extremity myositis [47].
Antibiotics
The role of antibiotic therapy in the treatment of CNO has waned consequent to the recognition of its non-infectious nature. An early case series of 13 patients with CNO treated with azithromycin documented rapid clinical and radiographic improvement; however, symptoms recurred following discontinuation. The beneficial effect was postulated to be secondary to the drug’s anti-inflammatory and immunomodulatory (rather than antimicrobial) effects [27]. Subsequent studies have failed to demonstrate sustained benefit of long-term antibiotics [4, 26].
Interventional procedures and surgery
Beyond the diagnostic utility of bone biopsy, there is currently no routine role for interventional nor surgical procedures in the treatment of CNO. Surgical debridement and even mandibular reconstruction following non-response to medical therapy is described in the adult literature [48].
Other treatments
Both α- and γ-interferon have been used with success in limited case reports [49, 50]. There is insufficient evidence to support their use.
Emerging therapies
Denosumab
Given the apparent central role of RANK and its ligand RANKL in the prevailing pathophysiologic framework of CNO, denosumab (a fully human, high-specificity, and high-affinity monoclonal antibody against RANKL) represents a promising therapeutic option. Few case reports in adults with mandibular CNO (referenced as “diffuse sclerosing osteomyelitis of the jaw”) demonstrate positive results [51, 52]. Thus far, there exist no studies of its use in childhood CNO.
Outcomes
CNO is generally characterized by a polycyclic course with fluctuating periods of inflammatory disease activity. Early literature suggested that the natural history of CNO was one of eventual spontaneous resolution [2•]. The disease is, in fact, self-limiting in some—in limited CNO (single site of involvement), Andreasen et al. observed that 53% of children had clinically inactive disease (asymptomatic, normal ESR) on medication at 1 year from diagnosis, while 63% maintained clinically inactive disease off medication at 2 years [39•]. However, Wipff et al. suggest that the vast majority of children (upward of 90%) with CNO develop multifocal disease within 4 years [30].
Furthermore, a substantial number of patients display ongoing clinical or subclinical disease at long-term follow-up. In 2002, Huber et al. described a cohort of 23 patients with CNO, of whom more than 25% had persistent disease activity (typical signs of bony lesions on clinical examination or clear history of typical symptoms in the 6 months preceding evaluation) at a median of 12.4 years from diagnosis [55]. The broadest data of clinical outcomes stem from the Eurofever study, wherein 52% of patients continued to display active inflammatory disease (clinical manifestations or abnormalities on laboratory or imaging studies) after follow-up of 22–68 months [3••].
As noted above, the absence of clinical symptoms does not preclude ongoing osseous inflammation. Voit et al. performed a long-term imaging follow-up study (greater than 10 years) and found that, despite being asymptomatic, 24% had persistent radiologic abnormalities on MRI [56].
Therefore, cognizant of CNO’s potential irreversible sequelae of fracture, bony deformity, and growth impairment, long-term follow-up is required. Per the CARRA CTPs, patients should be assessed at a minimum every 3 months for the first year. In addition, STIR or T2-weighted fat saturation MRI (preferably whole body, although regional is acceptable in unifocal disease or if whole-body MRI is unavailable) is strongly recommended at 6 and 12 months following any adjustment in therapy, and should otherwise be obtained on an annual basis [11••].
Conclusion
CNO, an autoinflammatory bone disease with an incidence rivaling that of bacterial osteomyelitis, represents an important and growing field of study. Once thought to be benign and self-limiting, CNO is now recognized to follow a relapsing and remitting course in the majority of children, and to carry substantial risk of irreversible growth and bone sequelae. As our understanding of the pathophysiologic mechanisms implicated in CNO evolves, so too does our ability to effectively treat this important condition.
Change history
05 August 2020
The original version of this article unfortunately contained a mistake in Tables 1 and 2 entries.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gideon A, Holthusen W, Masel LF, Vischer D Subacute and chronic “symmetrical” osteomyelitis. Ann Radiol [Internet]. 1972 [cited 2020 Feb 9];15:329–42. Available from: http://ci.nii.ac.jp/naid/10029267638/en/
• Hashkes PJ, Laxer RM. Chronic non-bacterial osteomyelitis. In: Textbook of autoinflammation; 2019. p. 563–85. First complete textbook on the novel field of autoinflammation; describes clinical presentation, pathogenesis, genetics, and latest management strategies for autoinflammatory disorders.
•• Girschick H, Finetti M, Orlando F, Schalm S, Insalaco A, Ganser G, et al. The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Eurofever international registry. Rheumatol (United Kingdom). 2018;57(7):1203–11. Largest reported case series of CNO patients to date; provides valuable data on demographic and clinical features, response to therapy, and outcomes.
Zhao Y, Laxer RM, Ferguson PJ. Treatment advances in chronic non-bacterial osteomyelitis and other autoinflammatory bone conditions. Curr Treat Options Rheumatol. 2017;3(1):17–32.
Borzutzky A, Stern S, Reiff A, Zurakowski D, Steinberg EA, Dedeoglu F, Sundel RP. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012 Nov 1;130(5):e1190–7.
Andronikou S, da Costa TM, Hussien M, Ramanan AV. Radiological diagnosis of chronic recurrent multifocal osteomyelitis using whole-body MRI-based lesion distribution patterns. Cliin Res. 2019 Sep 1;74(9):737–e3.
Gustavson K. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. 1978;93(2):227–31.
Hayem G, Bouchaud-Chabot A, Benali K, Roux S, Palazzo E, Silbermann-Hoffman O, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum. 1999;29(3):159–71.
Jansson AF, Grote V. Nonbacterial osteitis in children: data of a German Incidence Surveillance Study. Acta Paediatr Int J Paediatr. 2011;100(8):1150–7.
Schnabel A, Range U, Hahn G, Siepmann T, Berner R, Hedrich CM. Unexpectedly high incidences of chronic non-bacterial as compared to bacterial osteomyelitis in children. Rheumatol Int. 2016;36(12):1737–45.
•• Zhao Y, Wu EY, Oliver MS, Cooper AM, Basiaga ML, Vora SS, et al. Consensus treatment plans for chronic nonbacterial osteomyelitis refractory to nonsteroidal antiinflammatory drugs and/or with active spinal lesions. Arthritis Care Res. 2018;70(8):1228–37. Outlines first CTPs for CNO refractory to NSAIDs and/or with spinal lesions, the implementation of which will allow for prospective comparative effectiveness studies and, ultimately, the development of standardized treatment protocols.
Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A, et al. Classification of non-bacterial osteitis: retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology. 2007;46(1):154–60.
Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV. Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis. Pediatr Rheumatol [Internet]. 2016;14(1):1–5. https://doi.org/10.1186/s12969-016-0109-1.
Jansson AF, Müller TH, Gliera L, Ankerst DP, Wintergerst U, Belohradsky BH, et al. Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum. 2009;60(4):1152–9.
Cox AJ, Zhao Y, Ferguson PJ. Chronic recurrent multifocal osteomyelitis and related diseases—update on pathogenesis. Curr Rheumatol Rev. 2017 Apr 1;19(4):18.
Taddio A, Zennaro F, Pastore S, Cimaz R. An update on the pathogenesis and treatment of chronic recurrent multifocal osteomyelitis in children. Pediatr Drugs. 2017;19(3):165–72.
Hofmann SR, Kapplusch F, Mäbert K, Hedrich CM. The molecular pathophysiology of chronic non-bacterial osteomyelitis (CNO)—a systematic review. Molecular and Cellular Pediatrics. 2017 Dec;4(1):7. Summarizes the most important recent advances in the understanding of the pathophysiology of CNO and links these advances to treatment strategy.
Hofmann SR, Schnabel A, Rösen-Wolff A, Morbach H, Girschick HJ, Hedrich CM. Chronic nonbacterial osteomyelitis: pathophysiological concepts and current treatment strategies. J Rheumatol. 2016;43(11):1956–64.
Hofmann SR, Kubasch A, Rösen-Wolff A, Girschick H, Morbach H, Hedrich C. Altered expression of IL-10 family cytokines in CRMO result in enhanced inflammasome activation. Pediatr Rheumatol. 2015;13(1):1–2.
Hofmann SR, Kapplusch F, Girschick HJ, Morbach H, Pablik J, Ferguson PJ, et al. Chronic recurrent multifocal osteomyelitis (CRMO): presentation, pathogenesis, and treatment. Curr Osteoporos Rep. 2017;15(6):542–54.
• Cox AJ, Darbro BW, Laxer RM, Velez G, Bing X, Finer AL, et al. Recessive coding and regulatory mutations in FBLIM1 underlie the pathogenesis of chronic recurrent multifocal osteomyelitis (CRMO). PLoS One. 2017;3:e0169687. https://doi.org/10.1371/journal.pone.0169687. First to describe recessive mutations in FBLIM1 contributing to the pathogenesis of sterile bone inflammation; findings suggest CNO is a disorder of chronic inflammation and imbalanced bone remodeling.
ter Horst R, Jaeger M, Smeekens SP, Oosting M, Swertz MA, Li Y, et al. Host and environmental factors influencing individual human cytokine responses. Cell [Internet]. 2016;167(4):1111–1124.e13. https://doi.org/10.1016/j.cell.2016.10.018.
Schirmer M, Smeekens SP, Vlamakis H, Jaeger M, Oosting M, Franzosa EA, et al. Linking the human gut microbiome to inflammatory cytokine production capacity. Cell. 2016;167(4):1125–1136.e8.
Liao HJ, Chyuan IT, Wu CS, Lin SW, Chen KH, Tsai HF, et al. Increased neutrophil infiltration, IL-1 production and a SAPHO syndrome-like phenotype in PSTPIP2-deficient mice. Rheumatol (United Kingdom). 2015;54(7):1317–26.
Lukens JR, Gurung P, Vogel P, Johnson GR, Carter RA, McGoldrick DJ, et al. Dietary modulation of the microbiome affects autoinflammatory disease. Nature. 2014;516:246–9.
Assmann G, Kueck O, Kirchhoff T, Rosenthal H, Voswinkel J, Pfreundschuh M, et al. Efficacy of antibiotic therapy for SAPHO syndrome is lost after its discontinuation: an interventional study. Arthritis Res Ther. 2009;11(5):1–8.
Schilling F, Wagner AD. Azithromycin: Eine anti-inflammatorische Wirksamkeit im Einsatz bei der chronischen rekurrierenden multifokalen osteomyelitis? Eine vorlaufige mitteilung. Z Rheumatol. 2000;59(5):352–3.
Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlöhner S, et al. Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther. 2010;12(2).
Zhao Y, Chauvin NA, Jaramillo D, Burnham JM. Aggressive therapy reduces disease activity without skeletal damage progression in chronic nonbacterial osteomyelitis. J Rheumatol. 2015;42(7):1245–51.
Wipff J, Costantino F, Lemelle I, Pajot C, Duquesne A, Lorrot M, et al. A large national cohort of French patients with chronic recurrent multifocal osteitis. Arthritis Rheumatol. 2015;67(4):1128–37.
Daniels MJD, Rivers-Auty J, Schilling T, Spencer NG, Watremez W, Fasolino V, et al. Fenamate NSAIDs inhibit the NLRP3 inflammasome and protect against Alzheimer’s disease in rodent models. Nat Commun. 2016;7:24–30.
Carr AJ, Cole WG, Roberton DM, Chow CW. Chronic multifocal osteomyelitis. J Bone Jt Surg Ser B. 1993;75(4):582–91.
Kostik MM, Kopchak OL, Maletin AS, Mushkin AY. The peculiarities and treatment outcomes of the spinal form of chronic non-bacterial osteomyelitis in children: a retrospective cohort study. Rheumatol Int [Internet]. 2020;40(1):97–105. https://doi.org/10.1007/s00296-019-04479-2.
Abril JC, Ramirez A. Successful treatment of chronic recurrent multifocal osteomyelitis with indomethacin: a preliminary report of five cases. J Pediatr Orthop. 2007;27(5):587–91.
Job-Deslandre C, Krebs S, Kahan A. Chronic recurrent multifocal osteomylitis: five-year outcomes in 14 pediatric cases. Rev du Rhum (Edition Fr.). 2001;68(5):425–32.
Kostik MM, Kopchak OL, Chikova IA, Isupova EA, Mushkin AY. Comparison of different treatment approaches of pediatric chronic non-bacterial osteomyelitis. Rheumatol Int [Internet]. 2019;39(1):89–96. https://doi.org/10.1007/s00296-018-4151-9.
de Vries E, van der Weij JP, van der Veen CJP, van Paassen HC, Jager MJ, Sleeboom HP, et al. In vitro effect of (3-amino-1-hydroxypropylidene)-1,1-bisphosphonic acid (APD) on the function of mononuclear phagocytes in lymphocyte proliferation. Immunology. 1982;47(1):157–63.
Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlöhner S, Hofmann U, Raab P, Girschick HJ. Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther. 2010 Apr;12(2):R74. http://resolver.scholarsportal.info/resolve/07248741/v12i0006/916_eolafbfr2civ. Accessed 15 Mar 2020.
• Andreasen CM, Jurik AG, Glerup MB, Høst C, Mahler BT, Hauge EM, et al. Response to early-onset pamidronate treatment in chronic nonbacterial osteomyelitis: a retrospective single-center study. J Rheumatol. 2019;46(11):1515–23. Data suggest that early and sustained use of pamidronate may improve clinical and radiologic disease activity in multifocal and NSAID-resistant CNO.
Schnabel A, Range U, Hahn G, Berner R, Hedrich CM. Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44(7):1058–65.
Sułko J, Ebisz M, Bień S, Błażkiewicz M, Jurczyk M, Namyślak M. Treatment of chronic recurrent multifocal osteomyelitis with bisphosphonates in children. Joint Bone Spine. 2019;86(6):783–8.
Hirano D, Chiba K, Yamada S, Ida H. Oral alendronate in pediatric chronic recurrent multifocal osteomyelitis. Pediatr Int [Internet]. 2017;59(4):506–8. https://doi.org/10.1111/ped.13236.
Pardeo M, Marafon DP, Messia V, Garganese MC, De Benedetti F, Insalaco A. Anakinra in a cohort of children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017;44(8):1231–8.
Eleftheriou D, Gerschman T, Sebire N, Woo P, Pilkington CA, Brogan PA. Biologic therapy in refractory chronic non-bacterial osteomyelitis of childhood. Rheumatology (Oxford). 2010;49(8):1505–12.
Herlin T, Fiirgaard B, Bjerre M, Kerndrup G, Hasle H, Bing X, et al. Efficacy of anti-IL-1 treatment in Majeed syndrome. Ann Rheum Dis. 2013;72(3):410–3.
Aksentijevich I, Masters SL, Ferguson PJ, Dancey P, Frenkel J, van Royen-Kerkhoff A, et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med. 2009;360(23):2426–37.
Sato H, Wada Y, Hasegawa E, Nozawa Y, Nakatsue T, Ito T, et al. Adult-onset chronic recurrent multifocal osteomyelitis with high intensity of muscles detected by magnetic resonance imaging, successfully controlled with tocilizumab. Intern Med. 2017;56(17):2353–60.
Rustemeyer J, Siegmund BJ, Okcu Y, Busch A. Total mandibular reconstruction following diffuse sclerosing osteomyelitis. Oral Maxillofac Surg. 2019;23(1):95–9.
Gallagher KT, Roberts RL, MacFarlane JA, Stiehm ER. Treatment of chronic recurrent multifocal osteomyelitis with interferon gamma. J Pediatr. 1997;131(3):470–2.
Andersson R. Effective treatment with interferon-alpha in chronic recurrent multifocal osteomyelitis. J Interferon Cytokine Res. 1995;15(10):837–8.
Hallmer F, Korduner M, Moystad A, Bjornland T. Treatment of diffuse sclerosing osteomyelitis of the jaw with denosumab shows remarkable results-a report of two cases. Clin Case Rep England. 2018;6:2434–7.
Otto S, Burian E, Troeltzsch M, Kaeppler G, Ehrenfeld M. Denosumab as a potential treatment alternative for patients suffering from diffuse sclerosing osteomyelitis of the mandible-a rapid communication. J Craniomaxillofac Surg. 2018 Apr;46(4):534–7.
Truven Health Analytics IWH. Micromedex®RED BOOK®. 2019.
Ilowite NT. Chapter 13 – pharmacology: biologics. In: Textbook of pediatric rheumatology; 2016. p. 161–175.e6.
Huber AM, Lam PY, Duffy CM, Yeung RSM, Ditchfield M, Laxer D, et al. Chronic recurrent multifocal osteomyelitis: clinical outcomes after more than five years of follow-up. J Pediatr. 2002;141(2):198–203.
Voit AM, Arnoldi AP, Douis H, Bleisteiner F, Jansson MK, Reiser MF, et al. Whole-body magnetic resonance imaging in chronic recurrent multifocal osteomyelitis: clinical longterm assessment may underestimate activity. J Rheumatol. 2015;42(8):1455–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Laxer has provided consultation services to the Novartis Pharmaceuticals Corporation, which manufactures canakinumab. Raphaël Kraus declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Rheumatology
Rights and permissions
About this article
Cite this article
Kraus, R., Laxer, R.M. Characteristics, Treatment Options, and Outcomes of Chronic Non-bacterial Osteomyelitis in Children. Curr Treat Options in Rheum 6, 205–222 (2020). https://doi.org/10.1007/s40674-020-00149-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-020-00149-8