Abstract
Purpose
To describe medical students’ reading habits and resources used during clinical clerkships, and to assess whether these are associated with performance outcomes.
Method
Authors administered a cross-sectional survey to medical students at 3 schools midway through the clerkship year. Closed and open-ended questions focused on resources used to read and learn during the most recent clerkship, time spent and purpose for using these resources, influencers on study habits, and barriers. A multiple regression model was used to predict performance outcomes.
Results
Overall response rate was 53% (158/293). Students spent most of their time studying for clerkship exams and rated question banks and board review books as most useful for exam preparation. Sixty-seven percent used textbooks (including pocket-size). For patient care, online databases and pocket-sized textbooks were rated most useful. The main barrier to reading was time. Eighty percent of students ranked classmates/senior students as most influential regarding recommended resources. Hours spent reading for exams was the only significant predictor of USMLE Step 2 scores related to study habits. The predominant advice offered to future students was to read.
Conclusions
These findings can help inform students and educational leadership about resources students use, how they use them, and links to performance outcomes, in an effort to guide them on maximizing learning on busy clerkships. With peers being most influential, it is important not only to provide time to help students build strong reading and study habits early, but also to guide them towards reliable resources, so they will recommend useful information to others.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
To meet accreditation standards, medical schools must provide opportunities for independent study and unscheduled time to allow medical students to develop the skills of lifelong learning [1]. Nonetheless, a key feature of medical school clinical clerkships is immersion in healthcare settings to facilitate learning in the context of patient care. Frequent generic feedback to medical students in this setting is for them to read more [2, 3]. From an early age, as soon as children acquire literacy skills, they place greater trust in printed material than in information that is only heard or seen [4]. Medical students on clinical clerkships learn in the context of their patient care experiences and other educational sessions, yet the extent to which they read, the resources they use to learn and study, and how these may impact their performance is not well described.
Few studies have examined medical students’ reading habits or how they relate to performance, and most are at one school on one clerkship. A 2006 study of medical students’ reading behaviors while on the internal medicine clerkship indicated that they read for an average of 10.8 h per week, and most students experienced problems reading about patients due to insufficient time [2]. It has been reported that students used electronic resources and question books on the internal medicine clerkship [2, 5] and that any use of the Harrison’s textbook predicted better performance on the medicine National Board of Medical Examiners (NBME) subject matter exam [6]. Some studies, many from earlier eras, describe the reading habits of residents in internal medicine [7, 8] and family medicine residents [9]; one more recently regarding surgery residents’ reading habits showed a positive impact on surgery residents’ reading habits and their in-training exam performance [10]. It is unclear how the findings from these studies relate to current medical students who have access to a wide range of electronic and standard print resources to choose from while caring for patients and while studying for a high-stakes examination throughout the clerkship year. Furthermore, there is a gap in understanding who or what are the main influencers on student's reading and study habits and what advice students receive and give. In order to fill in these gaps in the literature, our study sought to update and build upon prior smaller studies by examining medical students reading and study habits and influences upon their choices, through a multi-institutional, multi-clerkship approach, and examined the potential links between students' reading habits and educational performance outcomes.
Our main research questions were, what are medical students’ reading habits, what resources do they use during clinical clerkships, and are these associated with performance outcomes? In order to empirically examine this, we surveyed medical students from 3 medical schools about their reading habits during the clinical clerkship year, including the resources they used and who influenced them, and assessed whether their self-reported reading habits and resources used were associated with proximal and distal performance outcomes, namely their NBME exam scores and Step 2 performance.
Methods
Study Settings
Three medical schools participated in the study, The George Washington University School of Medicine and Health Sciences (GW), Donald and Barbara Zucker School of Medicine at Hofstra/Northwell (ZSOM), and The University of Illinois College of Medicine at Urbana Champaign (UICOMUC). Each of these schools has a late spring/early summer start to the third-year clerkship and the US Medical Licensing Exam (USMLE) Step 1 is taken at the traditional time, after the pre-clinical curriculum and before the clinical clerkships. Students at each school have both online and physical library access to educational resources and there is typically a weekly student educational “day” or set of sessions that takes place during the clerkships. National Board of Medical Examiners (NBME) subject matter exams are administered after most of the core clinical clerkships and students take the USMLE Step 2 following the core clerkship year.
Survey Instrument and Administration
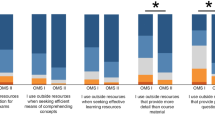
Each school administered the same cross-sectional survey (see Appendix), using Qualtrics (Provo, UT), to its own third-year medical students after their third or fourth clinical clerkship (approximately mid-way through the third year) during the 2017–2018 academic year. The dean’s office at each school sent an email invitation to all third-year medical students, with up to three reminders to students who had not yet completed the survey. The survey for this study was developed by drawing upon question domains used in other smaller studies [2, 8] and all questions were piloted with a senior medical student who helped in the study planning phase. Closed-ended questions asked participants to estimate the number of hours per week they spent using each resource (textbooks, pocket textbooks, primary literature, question banks, board review/test preparation, notes from coursework, online databases, online cases, other online, and other), as well as the percent of time they used each resource for patient care, exam study or to fill knowledge gaps. Usefulness of each resource (for patient care and exam study only) was rated on a 5-point Likert scale (not at all useful = 1, slightly useful = 2, somewhat useful = 3, very useful = 4, and extremely useful = 5). Additional closed-ended questions inquired about barriers to reading (no barriers/challenges, lack of sufficient time to read, didn’t know what to read, hard to find sources appropriate to my training level, other), how often students read for pleasure during clerkships and breaks (5-point Likert scale: 1 = never, 2 = rarely, 3 = weekly, 4 = several times a week, 5 = daily) and whether students who reported reading textbooks accessed these books online or through physical copy. Students were also asked to rank at least three groups who influenced their choice of resources (classmates/senior students, interns/residents/ attending physician on the clerkship, clerkship director/assistant director, faculty advisor/advising or curricular dean, online forum, or other).
In addition, the survey included 3 open-ended questions regarding the factors that determine how material is read, recommendations to future students regarding the optimal way to use learning time during clerkships, and how studying and reading habits have changed during the clinical clerkships compared to the preclinical portion of medical school.
Finally, the survey included demographic questions for students to report their age category, undergraduate major, and specialty of interest.
Scores for the NBME exams and USMLE Step 1 and 2 performance were obtained directly from a representative in the office of medical education or dean's office. The data was then deidentified through the construction of a unique identifier. All further analysis was conducted with the deidentified data.
This study was approved by the Institutional Review Board (IRB) at each participating institution, with GW serving the role as the lead IRB (GW OHR Study Number 121633–28,344).
Statistical Analysis
Data were statistically evaluated using IBM SPSS Statistics (Chicago, IL, USA, Version 25). Comparisons of demographic and clinical variables were performed with an analysis of variance (ANOVA) for continuous variables and chi-square analyses for categorical variables with school as the between subjects’ factor. Bonferroni correction was used to account for multiple post hoc comparisons. Correlations between time spent reading (h) and resource usefulness rating (5-point Likert scale) were performed using the Spearman’s rho (rs) test. A multiple regression model was used to predict Step 2 CK score. The following predictor variables were entered into the model: Step 1 Score, most recent Shelf exam percentile score, number of hours per week reading to study for exams, number of hours per week reading for patient care, number of hours per week reading for knowledge, reading for pleasure during clerkship (never/rarely vs. weekly/several times/daily), and reading for pleasure during breaks (never/rarely vs. weekly/several times/daily).
Analysis of Free Text Responses
For the 3 open-ended survey questions, two authors read all responses (TK and LK) and one author (TK) prepared an initial categorization of the responses which was then discussed with LK for additional input and to determine predominant response categories. Findings were subsequently shared with all authors for any additional input.
Results
Participants
A total of 293 surveys were distributed to students across the three schools, and the overall response rate was 53%. The response rate varied across the three schools: 26% at GW (46/175), 75% at ZSOM (68/91) and 59% at UICOMUC (16/27). Table 1 shows relevant characteristics of each participating school. Demographic data and USMLE exam scores are presented in Table 2. Students from UICOMUC were significantly older than students at ZSOM (χ2(3) = 12.16, p = 0.007), and there was a similar trend comparing students from UICOMUC and GW (χ2 (3) = 7.55, p = 0.056). The three schools had significantly different Step 1 exam scores (F(2,127) = 3.48, p = 0.03); however, post hoc analyses only showed a trend for ZSOM students to have higher Step 1 scores than GW students (p = 0.08) and no significant differences comparing ZSOM to UICOMUC (p = 0.17) and GW to UICOMUC (p = 1.0). There was no difference in Step 2 CK score between the groups (F(2,125) = 0.64, p = 0.53). The three schools had significantly different percentile scores on their most recent clerkship Shelf exam (F(2,122) = 6.6, p = 0.002), with ZSOM students obtaining higher percentile scores than GW (p = 0.004) and a trend towards higher scores compared to UICOMUC students (p = 0.07). School comparisons of specialty choice could not be performed due to small groups sizes in each specialty category.
Time Spent Studying During Clerkships
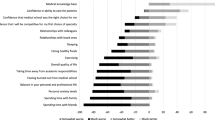
Figure 1 shows the distribution of the average number of hours per week students used each resource and for what reason they used that resource during the most recent clerkship. Students spent most of their time studying for clerkship exams (M = 12.0 h, SD = 9.1). In particular, they used question banks for an average of 6.6 h per week (SD = 5.4) and board review/test prep books for an average of 3.5 h per week (SD = 3.6) in order to prepare for the exam. Students spent an average of 6.6 h (SD = 6.3) reading topics related to patient care. Online databases (e.g., UpToDate, DynaMed, Clinical Key) were primarily used for learning about patient care (M = 3.3 h, SD = 3.9), but students also turned to essentials/pocket-size textbooks (M = 1.6 h, SD = 2.1) and the primary literature (M = 1.5 h, SD = 1.4). There was an even distribution of resources used to fill gaps in knowledge, but on average students spent only 5.6 h per week (SD = 5.9) studying for this reason.
Usefulness of Resources
Table 3 shows how students rated each resource as far as its usefulness for preparing for the clerkship exam and for patient care. Students rated question banks and board review/test prep books as most useful for clerkship exam preparation and online databases and essentials/pocket-sized textbooks as most useful for patient care. This is consistent with the number of hours spent using each resource. Figure 2 shows the relationship between usefulness rating and number of hours for each type of resource specific to whether the reading was for clerkship exams (Fig. 2a, top) or patient care (Fig. 2b, bottom). There was a significant correlation between the number of hours spent using a resource and the perceived usefulness of the resource (for clerkship exam: rs = 0.47, p < 0.001; for patient care: rs = 0.37, p < 0.001).
Students ranked who most influenced their decision regarding what resources to use. Figure 3 shows the distribution of how many students ranked influences as 1st to 3rd most important, 4th to 7th most important, or not at all. Eighty percent of students ranked classmates/senior students as most 1st to 3rd most important. Students also ranked interns/residents (71%) and clerkship directors (48%) as 1st to 3rd most important influences. Faculty advisors were mostly ranked in the bottom (49%) or not ranked at all (30%).
Characterization of How Students Are Reading
Eighty-seven students (67%) reported using textbooks or pocket-size textbooks. Of those 87 students, 42 (48%) reporting using full textbooks only, 15 (17%) reported using essentials or pocket-size textbooks, and 30 (34%) reported using both. Sixty-nine students (79%) who used textbooks reported reading textbooks online. Forty-eight (55%) of students used a physical book that they either borrowed or owned. The strongest barrier to reading on clerkships was insufficient time (75%). Some students did not know what to read (11%) or how to find sources appropriate to their training level (4%). Only a few students reported no barriers to reading (8%). Figure 4 shows the distribution of students reading for pleasure habits during clerkships and on breaks. During clerkships, students never or rarely read for pleasure (70%). However, during breaks between clerkship, most students read several times per week or daily (59%).
Percent of student responses to the question “How often do you read for pleasure or non-career related material?” considering time during clerkships (closed circles) and time during breaks (open circles) separately. Reponses were based on a 5-point Likert scale: never (1), rarely (2), weekly (3), several times (4), and daily (5)
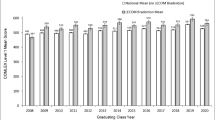
Predictors of Student Performance on Step 2 CK
Table 4 presents the results from the linear regression model predicting Step 2 CK scores. The model was significant (F(7,110) = 18.57, p < 0.001), accounting for 51% of the variance (adjusted R2). Step 1 score, the most recent shelf exam percentile score, and number of hours reading for exam study were significant positive predictors of Step 2 CK scores. For every additional 1 h spent reading “for exam study” per week, there was a 0.30-point increase in Step 2 CK score. Hours spent reading “for patient care” and hours spent reading “for knowledge” were not statistically significantly associated with Step 2 CK scores.
Reading Habits and Recommendations for Future Students: Free-Text Responses
In response to the question, “What are your recommendations for future students regarding the optimal way to use learning time during clerkships?” the predominant advice was to read. This included reading about patients (for clinical care, to solidify knowledge, to fill in gaps, from primary literature, from textbook chapters), suggested reading schedules (daily, throughout, at lunch, before cases, early in the morning), reading review books and about questions answered incorrectly, and balancing reading with doing questions. Next prominently was advice to use downtime (use any little bit of time waiting, to review, study, read, and do questions). Another main recommendation was to complete questions (at home, daily, during the day, early on, for exams, on phone, before exams) and to plan out their study schedule. Other advice included careful selection of resources to use (pick a limited number, stick with them, be deliberate, use thoroughly), to learn about patients by focusing on patient care, to do what works, and to take rest days.
When asked, “What factors determine if you will read textbook material online or in a physical book?” students described two main determinants are access to the book (for about one third of respondents) and cost of the book (for another third of respondents). In terms of access, some noted that availability in the library mattered. In terms of cost, many indicated that they will use whatever is free. More students preferred the physical book than an online version of the book. Reasons for preferring the physical book included gaining background information and for learning and notetaking, the organization of the book including the presence of an index, and other features like if it is small and portable so they could carry it around. Those preferring the online version of textbooks liked the convenience, the ability to read anywhere like in the hospital and on portable devices (phones, tablets), and features like searchability, copy/pasting and online notetaking. Other general factors that played a role included prior students’ recommendations, amount of knowledge sought, length, quality of the online format, and readability.
Finally, students described how their studying and reading habits changed in the clinical clerkships as compared to the preclinical portion of medical school. Their predominant focus during preclinical was on lecture slides, notes, outlines, flashcards, and assigned readings on basic science, with more time available for dedicated study, and some more group study. The predominant features of clinical clerkships were that students felt more efficient, more focused (on patients, on truly understanding, on studying high yield material), they had less time (to read and study new material), and that they used questions banks. Others indicated that they read more (about their patients, using more primary literature and using more textbook). Several students commented that they made no changes from preclinical to clinical. Other comments were that in the clinical learning settings they studied more from what they were seeing and doing, and they studied more on the go, in short bursts, in loud clinical environments, in random allotments, and with less time.
Discussion
In this multi-institutional study of medical students’ reading habits, we report on how third-year medical students spent their study time during clinical clerkships. They predominantly prepared for exams using question banks and board review preparation books and spent over twice as much time reading for exams compared to reading for patient care. Of those clerkship students who did read textbooks, most read physical copies rather than online texts. Students noted they use whatever is available, portable, accessible, and inexpensive. While over 15 years have passed since an initial study of medicine clerkship students' reading habits, notably our study conveys the enduring value of textbooks [2], while still preferring question banks. As declared in a 2005 study, “the age of the textbook is not dead.” [6].
The strongest barrier to reading was time. Nonetheless, many students had a habit of reading for pleasure, time permitting. During clerkships students rarely read for pleasure, but when on breaks between clerkships most students read several times per week or daily. This is an intriguing finding given that there is a vast literature on reading for pleasure in childhood and associations with higher academic attainment, better emotional health, and more empathy [11, 12]. Our findings among medical students also build on a previous survey of health sciences students who listed many benefits of leisure reading. Students reported that leisure reading helped in their development as health professionals, but time, fatigue, and expense were barriers to this kind of reading [13].
In terms of performance outcomes, in addition to Step 1 score predicting Step 2 score as expected, hours spent reading during clerkships for exam study was associated with an increase in Step 2 scores. Although hours spent reading for patient care and reading for knowledge were not independently associated with exam performance after controlling for the effects of other factors, students still found these to be important reasons to read. In free text responses, students reported that their main advice for future students is to read.
The biggest influencer on what resources students used came largely from peer recommendations. This is in keeping with the near peer teaching literature recognizing that it is the social and cognitive congruence among near peer trainees that helps with information sharing and role modeling [14, 15]. Not surprisingly, students in our study reported being influenced most strongly by what their peers just senior to them recommended for success.
In the present study we were able to build on prior studies that looked at medical students on a single clerkship or at a single institution [2, 6], or of residents [8,9,10], or from a much earlier era [2, 7]. Similar to a survey of medical students in Australia, students in our study preferred online question banks for learning [16]. While previous reports indicate that residents' primary motivation for reading was a desire to learn about the problems of one’s patients [8], in our study medical students tended to read for the purpose of preparing for exams, which in turn was found to be significantly associated with Step 2 performance, even once Step 1 and shelf exam performance was taken into account. In addition, previous reports acknowledged that the question of how reading changes throughout medical school was an underexplored area, and found students read less during clerkship years [2]. In our study, students provided open-ended responses describing being more efficient, more focused and reading more during the clerkship years as compared to preclinical years.
Limitations of our study include potential recall bias as with any subjective, self-reported information, though we did ask about student’s most recent clerkship, and we obtained student’s exam performance directly from the schools rather than from the students. Another limitation is that our overall response rate was 53% as not all students opted to complete the survey, and there could be potential differences between respondents and non-respondents in terms of reading habits. Finally, given our focus on reading, we did not include videos as resources, and we did not assess for passive versus active engagement with resources, though the latter comes out in some free text responses; this would be interesting to assess further in future study.
Conclusions
These findings have potential to help inform medical students, clerkship directors, and academic advisors about the resources students use and how they use them, in an effort to provide guidance on how to optimize students’ time while on clinical rotations. With peers or senior students being the most influential, it is important not only to provide time to help students build strong reading and study habits early, but also to guide them towards reliable resources, so they will recommend useful information to their peers.
Availability of Data and Material
Deidentified survey response data available upon request.
Code Availability
Survey administered using Qualtrics.
References
Liaison Committee on Medical Education: functions and structure of a medical school standards for accreditation of medical education programs leading to the MD degree. https://lcme.org/publications/ Accessed October 2020.
Leff B, Harper GM. The reading habits of medicine clerks at one medical school: frequency, usefulness, and difficulties. Acad Med. 2006;81(5):489–94. https://doi.org/10.1097/01.ACM.0000222273.90705.a6.
Watling C, Driessen E, van der Vleuten CP, Vanstone M, Lingard L. Beyond individualism: professional culture and its influence on feedback. Med Educ. 2013;47(6):585–94. https://doi.org/10.1080/09638288.2021.1891304.
Robinson EJ, Einav S, Fox A. Reading to learn: prereaders’ and early readers’ trust in text as a source of knowledge. Dev Psychol. 2013;49(3):505–13. https://doi.org/10.1037/a0029494.
Cooper AL, Elnicki DM. Resource utilization patterns of third-year medical students. Clin Teach. 2011;8(1):43–7. https://doi.org/10.1111/j.1743-498X.2010.00393.x.
DeZee KJ, Durning S, Denton GD. Effect of electronic versus print format and different reading resources on knowledge acquisition in the third-year medicine clerkship. Teaching and Learning in Medicine, An International Journal. 2005;17(4):349–54. https://doi.org/10.1207/s15328015tlm1704_7.
Fafard J, Snell L. Reading habits of house-staff: what, where and why. Med Teach. 1989;11(3–4):279–83. https://doi.org/10.3109/01421598909146413.
Lai CJ, Aagaard E, Brandenburg S, Nadkarni M, Wei HG, Baron R. Brief report: Multiprogram evaluation of reading habits of primary care internal medicine residents on ambulatory rotations. J Gen Intern Med. 2006;21(5):486–9. https://doi.org/10.1111/j.1525-1497.2006.00432.x.
Johnson KH, Dayrit M, Bazargan M. The reading habits of family practice residents. Fam Med. 1997;29(7):488–91.
Kim JJ, Kim DY, Kaji AH, et al. Reading habits of general surgery residents and association with american board of surgery in-training examination performance. JAMA Surg. 2015;150(9):882–9. https://doi.org/10.1001/jamasurg.2015.1698.
Clark C, Rumbold K. Reading for pleasure: a research overview. Natl Lit Trust. 2006;1–35. https://doi.org/10.1037/h0037910
Mak HW, Fancourt D. Longitudinal associations between reading for pleasure and child maladjustment: Results from a propensity score matching analysis. Soc Sci Med. 2020;253:112971. https://doi.org/10.1016/j.socscimed.2020.112971.
Watson EM. The importance of leisure reading to health sciences students: results of a survey. Health Info Libr J. 2016;33(1):33–48. https://doi.org/10.1111/hir.12129.
Bulte C, Betts A, Garner K, Durning S. Student teaching: views of student near-peer teachers and learners. Med Teach. 2007;29(6):583–90. https://doi.org/10.1080/01421590701583824.
Lockspeiser TM, O’Sullivan P, Teherani A, Muller J. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv Health Sci Educ Theory Pract. 2008;13(3):361–72. https://doi.org/10.1007/s10459-006-9049-8.
Wynter L, Burgess A, Kalman E, Heron JE, Bleasel J. Medical students: what educational resources are they using? BMC Med Educ. 2019;19:36. https://doi.org/10.1186/s12909-019-1462-9.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the manuscript warranting authorship as per ICMJE guidelines, i.e., to the study conception/design or acquisition, analysis, or interpretation of the data, drafting/revising, providing final approval, and are ensuring accountability.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved as exempt by the Institutional Review Boards at each participating institution, with The George Washington University Office of Human Research serving as the lead. Consent from participants was obtained electronically.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kind, T., Olvet, D.M., Farina, G. et al. Reading and Study Habits of Medical Students on Clerkships and Performance Outcomes: a Multi-institutional Study. Med.Sci.Educ. 31, 1957–1966 (2021). https://doi.org/10.1007/s40670-021-01409-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-021-01409-5