Abstract
Basic sciences are a cornerstone of undergraduate medical education (UME), yet research indicates that students’ basic science knowledge is not well retained. Many UME curricula are increasing the integration between the basic and clinical sciences with the goal of enhancing students’ knowledge levels; however, the impact of clerkship training on students’ basic science knowledge remains inconclusive. Thus, using clerkship directors’ expectations as framework, we aimed to assess third-year medical students’ basic science knowledge during clerkship training and evaluate the influence of clerkship training on their basic science knowledge. Using concepts deemed necessary by clerkship directors, we created a basic science assessment for each clerkship rotation. Assessments were distributed to third-year medical students as a pre- and post-test to assess their basic science knowledge prior to and at the completion of each rotation. On average, students retained ≥ 60% of relevant basic science knowledge from pre-clerkship, and neither clerkship rotation order, nor the basic science discipline being assessed, impacted students’ basic science knowledge levels. Post-test data revealed that students, on average, reinforced fundamental concepts during clerkship. Interestingly, even though lower-performing students demonstrated the greatest post-test improvement, they still left each rotation with knowledge deficits compared with their highest-performing peers, suggesting that the clinical experience of clerkship appears to be particularly beneficial for lower-performing students, in regard to enhancing their basic science knowledge. Overall, results indicate that earlier exposure to clinical learning in UME, along with integration of basic science education into clerkship, could promote students’ basic science knowledge acquisition and retention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The basic sciences are a cornerstone of undergraduate medical education (UME), as they are essential for achieving overall expertise in the field of medicine [1, 2]. Basic science education in UME primarily focuses on the disciplines of anatomy, biochemistry, microbiology, pathology, pharmacology, and physiology, all of which are fundamental for effectively preparing trainees for clinical practice [3,4,5,6,7]. Topics of nutrition and imaging are often integrated with the basic sciences as they are essential for diagnosing and managing certain clinical conditions [8, 9]. There is a common misconception associated with basic science education that it is essentially a collection of facts which students need to memorize and recall, when in actuality, basic science knowledge is fundamental for students when reconstructing characteristics of a disease [3]. Therefore, in order to be proficient in a clinical setting, students must first master the foundations of the basic sciences, following which they can start to conceptualize the relevant clinical concepts and diagnoses [3, 6, 10,11,12].
Basic science knowledge is vital for fostering trainees’ proficiency in a clinical setting, as it is fundamental for the development of students’ clinical reasoning skills, which are essential for the problem-solving process physicians rely on to construct differential diagnoses and reach a clinical decision [2, 13, 14]. When trainees are evaluating patient signs and symptoms, they are relying on their basic science foundation to determine the most probable diagnosis [14]. Further evidence suggests that novices, such as clerks, actively rely on their basic science knowledge more so than experts in the field [14, 15], and the importance of strong basic science knowledge holds true as trainees are transitioning into their post-graduate career, as a lack of basic science knowledge has been directly correlated with failure rates on medical board examinations [16,17,18]. Additionally, a strong basic science foundation has been associated with enhanced diagnostic accuracy in the clinic [4, 6, 14]. For example, when patients present with complex signs and symptoms that are not easily diagnosable, trainees must rely on their basic science foundation in order to navigate and interpret the clinical condition, and ultimately reach a conclusion [6, 11, 19]. However, trainees are not the only cohort who requires a strong basic science foundation in the clinic as research also indicates that for complex clinical cases and diseases, senior physicians more actively rely on basic science concepts during the clinical reasoning process [20]. Overall, this suggests that comprehension and retention of basic science knowledge, which underpins all clinical conditions, are fundamental for the development of clinical science knowledge, clinical reasoning skills, and diagnostic accuracy, all of which are essential for success on board examinations, and achieving overall competence as a physician [2, 14, 21].
Despite the basic sciences providing the language for the field of medicine, many studies demonstrate that medical students’ basic science knowledge is not well retained, and there is a consistent decrement of their basic science knowledge as they progress through their training, which unfortunately can translate to a compromised quality of patient care [4, 22,23,24]. When evaluating basic science content learned in the first year of study, medical students’ knowledge of some concepts can drop to a retention rate as low as 46% after 8–10 months of initial exposure to the material [25], and other research demonstrates that students’ knowledge declined below the minimal level of competency of 65% within 5–11 months [23]. When assessing specific basic science disciplines, medical students’ knowledge dropped to an average of 61.7% and 67.1% after a period of 10–11 months in the topics of immunology and physiology, respectively; however, their knowledge fell to 41.5% in the subject of neuroanatomy, which may suggest that the extent to which students retain their basic science knowledge could be subject specific [26]. These knowledge deficits that many trainees display may be contributing to the lack of proficiency they tend to demonstrate in a clinical setting [23, 27].
With the current reported retention rates of basic science knowledge, many UME curricula are enhancing the integration between the basic and clinical sciences with the goal of promoting students’ knowledge acquisition and retention [28]. According to one learning principle that is rooted in cognitive psychology, students’ learning is most effective when the organization of knowledge is aligned with how the knowledge will be used [29]. In the context of UME, delivering basic science content with a clinical focus, and consistently making connections between the basic and clinical sciences, can enhance students’ understanding and retention of the material [30, 31]. However, there is very little research focusing solely on students’ basic science knowledge reinforcement during their clinical training. Some studies have demonstrated that clinical experiences integrated early on in UME can enhance students’ learning of clinical science knowledge, clinical skill proficiency, and their understanding of student-patient relationships, compared with students without early clinical experiences [32, 33]. Therefore, when clinical learning sessions are effectively integrated with basic science instruction, we may be able to foster students’ learning in the necessary basic sciences knowledge concepts [2, 21, 28, 30, 34].
Based on the evidence provided above, there is a need for an educational model that ensures that students are competent in the basic science fundamentals. Traditionally, many UME curricula present the basic sciences in the first 2 years of study (pre-clerkship), with the subsequent years of training focusing primarily on the clinical sciences [1, 4, 7, 35]. While the importance of basic science rigor at the pre-clerkship level continues to be supported by present-day educators, many UME curricula are increasing the vertical integration within their program to help make students’ learning more relevant, and ultimately better preparing them for clinical practice [28, 34]. With vertical integration, there is enhanced integration between the basic and clinical sciences across the years of UME training [28, 30, 34, 36]. For example, educators will incorporate case studies and clinical examples into their basic science lectures to aid with students’ understanding of the basic science content [28]. Further to this, some medical curricula are introducing earlier clinical experiences for students, such as taking a patient’s medical history, which has been shown to enhance students’ preparedness for their transition to their next stage of training [36, 37]. However, it is not fully known how, or to what extent, the clinical experience of clerkship impacts students’ basic science knowledge.
The majority of basic science knowledge retention studies utilize existing course assessments; however, in the present study, we evaluated students’ basic science knowledge levels according to concepts clerkship directors expect students to know when entering clerkship. Through the evaluation of students’ basic science knowledge retention and reinforcement levels during their clerkship training within the existing UME curriculum, we can provide insights into the effectiveness of basic science education at the pre-clerkship level and determine the influence of clerkship training on students’ basic science knowledge levels, and collected data can be utilized by educators to help inform curricular revisions to enhance the delivery of basic science content at the pre-clerkship level. Thus, the specific aims of this study were to (i) assess current third-year medical students’ knowledge retention of basic science concepts deemed necessary for students to know by clerkship directors and (ii) evaluate the influence of the clinical experience of clerkship on students’ basic science knowledge levels.
Materials and Methods
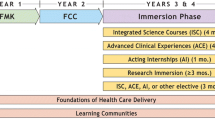
This research was conducted at the Schulich School of Medicine and Dentistry, during the 2017–18 academic year. Schulich has a 4-year UME training program where the basic sciences are integrated with the clinical sciences into systems-based courses. The basic sciences are delivered during pre-clerkship (years one and two) using primarily large group learning (didactic lectures), small group learning (laboratory sessions, small group discussions), and independent learning methods. In year 1, students study the basic sciences in the following courses: Introduction to Medicine, Blood, Infection & Immunity, Skin, Heart & Circulation, Respiration & Airways, and Genitourinary System. In the second year of study, the basic sciences are incorporated into Digestion & Nutrition, Endocrine & Metabolism, Reproduction, Key Topics in Family Medicine, Musculoskeletal System, Emergency Care, Neurosciences, Eye & Ear, and Psychiatry & the Behavioral Sciences (Table 1). Following the first 2 years of study, students begin clerkship year, in which there are six different core rotations: pediatrics, obstetrics and gynecology (OB/GYN), internal medicine, family medicine, psychiatry, and surgery. Students are also required to participate in an emergency medicine and an anesthesia rotation, which are mandatory sub-rotations of internal medicine and surgery, respectively. Following clerkship year, students complete clinical electives, the post-graduate matching process (Canadian Resident Matching Service (CARMs)), and a course that focuses on the transition to their post-graduate training (Integration & Transition).
Creation of Basic Science Assessments
Using basic science concepts deemed necessary by clerkship directors at Schulich UME [38], a basic science assessment was created for each core clerkship rotation: pediatrics, OB/GYN, internal medicine, family medicine, psychiatry, and surgery. For the purpose of this study anatomy, biochemistry, imaging, microbiology, nutrition, pathology, pharmacology, and physiology were classified as the basic sciences. Each assessment was comprised of 45 clinical-vignette style, basic science multiple-choice questions (Fig. 1), which were reflective of the basic science concepts and the frequency of topics that were mentioned in the interviews with clerkship directors [38]. Prior to implementation, each assessment was reviewed by clerkship directors, basic scientists, and a focus group consisting of fourth-year medical students, to ensure the assessments were appropriate. While the assessments were reviewed by the clerkship directors, the majority of clinical instructors and preceptors were not privy to the assessment questions.
Eight groups of students (groups A–H) (Table 2) rotated through the six core clerkship rotations, four of which are 6 weeks in length. Surgery and internal medicine are 12-week rotations with two groups of students rotating through each of them simultaneously, both of which have mandatory sub-rotations of anesthesia and emergency medicine, respectively. It is important to note that each group of students (A–H) would follow a different rotation order depending on their schedule.
Implementation of Basic Science Assessments
Prior to implementation, the students were briefed on the formative nature of the assessments, and how the assessment data was going to be used for research purposes. Informed consent was not required from participants as this research was deemed Quality Improvement/Quality Assessment (QI/QA) by Western Research Ethics. During the 2017–2018 academic year, the basic science assessments were distributed to third-year medical students (n = 172) prior to (pre-test) and at the completion (post-test) of each of the six core clerkship rotations to assess students’ basic science knowledge retention and reinforcement (Table 3). The questions were the same on both the pre- and post-tests, with the post-test questions arranged in a scrambled format so students were less likely to rely on their memory to complete the assessment. Students completed the pre- and post-tests, which had a time limit of 70 min, using the University of Western Ontario’s Learning Management System, OWL (Sakai 11.3-owl3.1). After completing the pre-test, students were provided with general formative feedback on the assessed topics, while following the post-test students received individualized feedback to help promote their personal development during clerkship year. Once all six rotation assessments were completed, an item analysis was conducted on each individual assessment question (n = 270) to evaluate student performance and means and to ensure the questions were of high quality. Assessments were not evaluated for equivalency of difficulty level since the assessment questions were derived from interviews with clerkship directors [38].
Statistical Analysis
Data was analyzed using IBM SPSS Statistics (IBM SPSS Version 21; Armonk, NY, USA). A one-way analysis of variance (ANOVA) with an alpha (α) level of 0.05 was used to determine if clerkship rotation, rotation order, basic science discipline, or student performance quartiles had any significant effect on students’ assessment performance. These analyses were followed by a post hoc analysis for multiple comparisons (Bonferroni correction) with an alpha (α) level of 0.01 to determine which relationships were significantly different, and p values subjected to the Bonferroni correction will be denoted as pbonf for the purposes of this research (i.e., pbonf ≤ 0.01). Students’ pre- and post-test scores were statistically compared using a paired sample, two-tailed t test (p ≤ 0.05). Graphs were created using Prism 8 (GraphPad Software, Version 8.3.1; San Diego, CA, USA).
Results
Students’ Basic Science Knowledge Retention
During the 2017–2018 academic year, Schulich’s UME passing threshold was 60%, and assessment data revealed that third-year medical students achieved an average greater than 60% on the pre-test prior to entering each clerkship rotation (Fig. 2). More specifically, the highest average scores were achieved in internal medicine (72%), and the lowest in surgery (63%). No significant differences were identified among the rotation-specific assessments (ANOVA; p > 0.05). The item analysis of each assessment question (n = 270) revealed that the majority of assessment questions were of high quality with a discrimination index of ≥ 0.2; questions that did not meet the expected level of quality were reviewed by the research team, but no questions were removed from the assessments.
Third-year medical students, on average, achieve > 60% on each basic science pre-test assessment, indicating that they retained relevant basic science knowledge from pre-clerkship. Scatter plots demonstrate the range of individual student scores on the pre-test. No significant differences were identified among the clerkship rotation pre-test assessments (ANOVA, p > 0.05) (n = number of students who completed the assessment)
Clerkship directors predicted that basic science knowledge newly acquired or re-enforced in previous rotations would be carried forward to subsequent rotations and, as a result, indicated that they expected students in their final rotation to have a better working knowledge of the basic sciences compared with students who are entering their first rotation [38]. However, when we examined the pre-test scores with a focus on students’ rotation order, we found that there were no statistically significant differences among the eight groups (ANOVA; p > 0.05) (Fig. 3). For example, for students completing pediatrics as their first rotation (group A), versus students completing pediatrics as their last rotation (group H), there was no significant difference (Fig. 3a). This finding was the same for all six clerkship rotations.
Medical students’ basic science knowledge retention was not influenced by clerkship rotation order. Pre-test scores (± SD) plotted against students’ clerkship rotation order, demonstrating no significant differences among the student groups (A–H) for each clerkship rotation (a–f), suggesting that students’ pre-test performance was not influenced by their clerkship rotation order (ANOVA; p > 0.05) (n = number of students)
Each assessment question (n = 270) was categorized according to which basic science was assessed (anatomy, biochemistry, imaging, microbiology, nutrition, pathology, pharmacology, physiology), and the question scores were analyzed. Data revealed that the average score was at least 60% in each basic science discipline on the pre-test, with the highest mean scores achieved in biochemistry (85%) and the lowest mean scores achieved in anatomy (61%) (Fig. 4). It should be noted that only two assessment questions were mapped to the discipline of biochemistry. Regardless of the average score of each basic science discipline, data also revealed that there were some assessment questions for which, on average, students did not achieve ≥ 60%. There were no statistically significant differences among the average scores in the individual basic sciences disciplines (ANOVA; p > 0.05).
Medical students’ basic science knowledge was not influenced by the basic science discipline being assessed. Average pre-test assessment question scores revealed that students achieved, on average, > 60% in each basic science discipline. No significant differences were identified in assessment question scores among the basic science disciplines (ANOVA; p > 0.05)
Students’ Basic Science Knowledge Reinforcement
Students’ average post-test scores were significantly higher compared with their pre-test scores for all rotations (p ≤ 0.05) (Fig. 5), indicating that they reinforced fundamental basic science knowledge during every rotation. Students achieved the highest average post-test score in the pediatric rotations (78%), and conversely, had the lowest average post-test score in the surgery rotation (68%). The largest increase, from pre- to post-test score, occurred during the pediatric rotation (10%), with the smallest increase taking place in internal medicine (2%).
Third-year medical students, on average, achieve > 60% on each basic science pre-test, and their average scores significantly improve in every rotation on the post-test assessment. Third-year medical students achieved, on average, > 60% on the pre-test assessment in each rotation (column with lines), indicating that they retained relevant basic science knowledge from pre-clerkship. On average, the post-test scores (filled column) were significantly higher in all six clerkship rotations indicating that students, on average, reinforced basic science knowledge during each rotation (paired sample t test; *p ≤ 0.05). Scatter plots demonstrate the range of student scores on both the pre- and post-test assessment (n = number of students who completed both the pre- and post-test assessments)
To determine if the clerkship groups were comparable with one another and if prior clerkship experiences reinforced students’ basic science knowledge at the completion of each rotation, students’ post-test scores were analyzed according to clerkship rotation order. No differences were found among the clerkship groups in all six clerkship rotations (ANOVA; p > 0.05) (Fig. 6).
Medical students’ basic science knowledge reinforcement, following each clerkship rotation, was not enhanced by previous clerkship experiences. Students’ post-test scores (± SD) were plotted against students’ clerkship rotation order. No significant differences among student groups were found (a–f) (ANOVA; p > 0.05) (n = number of students)
Students’ pre-test scores were divided into quartiles to determine if lower-performing (quartiles 1 and 2), higher-performing (quartiles 3 and 4), or all students were improving their basic science knowledge levels between pre- and post-test assessments (Fig. 7). The analysis revealed that lower-performing students’ post-test scores were significantly higher (p ≤ 0.01) compared with their pre-test for all clerkship rotations. Additionally, the post-test scores were also significantly higher for students whose pre-test scores were in the third quartile during the pediatrics (Fig. 7a; p < 0.001) and psychiatry (Fig. 7e; p = 0.005) rotation. For students in the fourth quartile, there were no differences between their pre- and post-test scores, except for psychiatry, where the post-test score was significantly lower than the pre-test score (Fig. 7e; p = 0.001).
Lower-performing students improve their basic science knowledge during clerkship; however, they do not achieve the knowledge levels of higher-performing students. Students’ pre-test scores (square with lines) were used to generate quartiles. Analysis revealed that lower-performing students (quartiles 1 and 2) achieved significantly higher scores on the post-test (filled square) assessment in all clerkship rotations (a–f), and quartile 3 students achieved significantly higher scores on the post-test during pediatrics and psychiatry (t test; *p ≤ 0.01). Additionally, higher-performing (upper quartiles) students’ pre- and post-test scores were significantly higher compared with lower-performing (lower quartiles) students’ post-test scores in five clerkship rotations, with the exception of psychiatry (ANOVA, Bonferroni post hoc test; **pbonf ≤ 0.01), suggesting that lower performing students do not achieve the knowledge levels of higher-performing students. Note: each data point represents an individual students’ score on the basic science assessments
While quartile 1 students achieved significantly higher scores on the post-test compared with the pre-test, their post-test scores were significantly lower (pbonf ≤ 0.01) compared with quartile 4 students’ pre-test scores in all six clerkship rotations (Fig. 7). Additionally, quartile 1 students’ post-test scores remained significantly lower (pbonf ≤ 0.01) compared with students’ post-test scores in quartile 4 in five clerkship rotations, with the exception of psychiatry.
Discussion
Students’ Basic Science Knowledge Retention
To our knowledge, no other study has examined students’ knowledge retention of basic science concepts based on clerkship directors’ expectations. In the present study, we revealed that, on average, students achieved a score greater than 60% on the assessments prior to entering each clerkship rotation (pediatrics 68% (± 12%) (range 20–96%); OB/GYN 67% (± 12%) (range 22–91%); internal medicine 72% (± 12%) (range 38–91%); family medicine 70% (± 11%) (range 13–91%); psychiatry 67% (± 9%) (range 13–91%); surgery 63% (± 12%) (range 9–96%); Fig. 2). This indicates that students do, on average, retain relevant basic science knowledge from their pre-clerkship training prior to entering clerkship, which has previously been shown in the literature [26, 39]. However, the data also revealed that there are students in every rotation whose scores fall below 60% on the pre-test. This trend has been documented in the literature indicating that students’ basic science knowledge levels can drop below 60% within 1 year of initially learning the material [25, 26, 40]. Even though average retention levels appear to be standard across student cohorts and curricula, the required level of basic science knowledge retention for a medical student entering a clinical setting remains inconclusive.
As previously mentioned, clerkship directors expect more basic science knowledge from students who are in their final rotation of clerkship versus students just entering clerkship [38]. Further to this, some literature demonstrates that students who completed their pediatric rotation near the end of clerkship year tended to perform better on relevant clinical assessments and board examinations, compared with students who completed pediatrics at the beginning of their clinical training [42]. Knowing this, we expected that students would further learn fundamental basic science concepts during their clinical training and, therefore, achieve higher assessment scores on pre-tests as they progressed through clerkship. However, we found that rotation order had no effect on students’ performance (Fig. 3), and therefore, their clinical experiences in previous clerkship rotations had no influence on their basic science knowledge retention levels. To our knowledge, there is no literature focusing specifically on the effect of clerkship rotation order on students’ basic science knowledge levels. Interestingly though, when analyzing the clinical sciences, other research has shown that students who complete their surgery, psychiatry, pediatrics, or OB/GYN rotations towards the end of clerkship year tend to perform better on rotation specific assessments [41,42,43,44]. However, contrary to this, Park et al. [45] highlighted that the timing of students’ psychiatry rotation had no effect on student performance with respect to their psychiatry rotation exam and clinical skill assessment scores. The present study focused strictly on the basic science concepts that clerkship directors expect students to know coming into clerkship; thus, overall, these findings may suggest that rotation-specific learning provides students with the opportunity to hone their clinical science knowledge more than their basic science knowledge, simply due to the clinical focus of clerkship.
Others have shown that students’ basic science knowledge retention can vary across the basic science disciplines [26, 39]; however, in the present study, we found that, on average, students achieved > 60% in each basic science discipline, with the highest and lowest average scores achieved in biochemistry (85%) and anatomy (61%), respectively (Fig. 4). However, it should be noted that there were only two assessed concepts associated with biochemistry, and thus, these concepts may be identified as high yield and may not be representative of general biochemistry knowledge retention. In agreement with our findings, other studies have found that, when testing students’ knowledge after 12–21 months of initially learning the material, students, on average, did achieve a passing grade in the disciplines of anatomy [46], physiology [47], and pharmacology [48]. While the average scores did vary across the disciplines, there were no significant differences among the basic science disciplines, suggesting that students’ basic science knowledge retention is not discipline specific.
Overall, these findings indicate that students, on average, retained fundamental basic science knowledge from pre-clerkship. However, despite the average scores, pre-test data highlighted that there were some concepts where the average grade of the students was below the minimal level of competency (60%). One potential solution to help increase students’ basic science knowledge retention could be to implement more well-defined milestones into basic science pre-clerkship curricula [49]. By implementing clear, fixed assessment outcomes, all students can work towards achieving the same educational goals and increase their self-accountability as they do so [50,51,52,53]. With this type of curricular framework, educators and curricula committees can ensure that all students are achieving a level of competency in the basic sciences that is expected of them prior to entering clerkship.
Students’ Basic Science Knowledge Reinforcement
There is limited research analyzing students’ reinforcement of basic science knowledge during clerkship training. In the present study, we revealed that students’ post-test scores were, on average, significantly higher compared with their pre-test scores in each clerkship rotation (Fig. 5), with the largest increase occurring during the pediatric rotation (∆10%). Interestingly, the clerkship directors of the pediatric rotation indicated that there was a higher volume of out-of-clinic learning sessions compared with the other clerkship rotations. Thus, the out-of-clinic learning sessions that students were immersed within during the pediatric rotation may have provided them with the opportunity to further learn fundamental basic science concepts, ultimately leading to enhanced performance on the post-test scores. There is evidence in the literature demonstrating that vertical integration across the basic and clinical sciences can foster students’ understanding of clinically relevant content [28, 30, 36], and the findings from the present study suggest that the out-of-clinic learning sessions may have had a similar effect on students’ basic science knowledge. Therefore, by enhancing the vertical integration within UME curricula through incorporating more basic science learning sessions during clerkship training, students can better integrate their basic and clinical science knowledge [28, 30, 34], which could enhance their understanding and retention of fundamental basic science content.
Consistent with the trend identified with the pre-test scores, the order of clerkship rotations did not influence students’ post-test scores as there were no differences among the student groups (Fig. 6). Similar results have been found pertaining to the clinical sciences during clerkship, as Myhre et al. demonstrated that two groups of third-year medical students were comparable with one another with respect to their clinical science knowledge [54]. Thus, our findings suggest that rotation order had no effect on students’ basic science knowledge reinforcement.
While students’ average post-test scores significantly increased during each clerkship rotation, our data further revealed that lower performing students (quartiles 1 and 2) demonstrated a significant improvement on their post-test, compared with their pre-test, in all six clerkship rotations (Fig. 7). Consistent with the findings from the present study, Koles et al. [55] determined that when second-year undergraduate medical students are learning pathology with a clinical focus via team-based learning and case-based learning, students in the lowest-performing quartile demonstrated the greatest improvement on their end-of-course pathology assessment, compared with their higher-performing peers. Similar results have been found in a clinical setting which revealed that undergraduate medical students who are completing their surgery clerkship rotation and are ranked in the lowest quartile on their entry exams for surgery demonstrated the greatest improvement on their final surgical examination in that same specialty, both of which consisted of multiple-choice questions and a clinical assessment [56]. Taken together, these results suggest that the clinical focus of clerkship that trainees are exposed to may enable lower-performing students to further learn, or reinforce, fundamental basic science concepts that are pertinent to that particular rotation.
Quartile 3 students also showed improvement in their post-test scores in two rotations: pediatrics and psychiatry (Fig. 7a, e). Just as we saw for quartiles 1 and 2, these students are also benefitting from the clinical experience of clerkship, with respect to their basic science knowledge. Alternatively, these findings could also be representative of a ceiling effect. This phenomenon has been identified in a gross anatomy course for medical students [57], and in other educational contexts, such as foreign language and statistics courses [58, 59], and suggests that higher-performing students receive their highest achievable grade, relative to their peers, on their first examination [60]. Thus, perhaps the higher-performing students in this study, with the exception of quartile 3 students in pediatrics and psychiatry, achieved their highest possible score on their initial assessment, the pre-test, and as a result, there was limited room for improvement on the subsequent post-test assessments [60, 61].
Although students in quartile 1 did demonstrate a significant improvement on the post-test, their performance did not rise to the level of the average pre-test assessment scores of quartile 4 students in all six rotations (Fig. 7). Other studies have indicated that prior academic performance is the best predictor of success on future assessments. For example, second-year medical students’ pre-test scores were found to predict their post-test performance on diagnostic classification during a microscopic pathology course [62], and when analyzing the impact of face-to-face and online instruction on student performance, incoming grades were shown to be a significant predictor, for overall course performance in both an undergraduate microscopic anatomy and a systemic human anatomy course [63, 64]. Similarly, we found that lower-performing students’ pre-test scores were a predictor for their basic science knowledge levels at the end of each clerkship rotation. As previously discussed, enhanced integration between the basic and clinical sciences can promote students’ learning and understanding of the content [28], and there is evidence to suggest that earlier exposure to the clinical sciences can have a positive impact on students’ overall learning [336566]. Thus, by increasing the vertical integration between the basic and clinical sciences in UME through the introduction of clinical experiences earlier in pre-clerkship and by promoting basic science education in the latter years, we may be able to enhance students’ knowledge acquisition and retention of the fundamental basic sciences, particularly for lower-performing students, thereby ensuring that all students are proficient in the necessary basic science fundamentals after completing their pre-clerkship training to improve their transition to clerkship [28, 30, 67,68,69].
Limitations
The results from this study are from a single academic year at one institution; therefore, data may not be representative of other student cohorts nor other UME curricula. In regard to the assessment data, a re-test bias could have positively influenced students’ post-test scores as students may have had some recollection of the pre-test questions that they previously completed. Further to this, students received generalized pre-test feedback; as a result, they could have targeted their learning towards concepts included on the pre-test, which could have positively impacted their post-test performance. Additionally, students’ intrinsic motivation, or lack thereof, could have positively or negatively impacted their assessment score(s).
Conclusion
Overall, the results from this study revealed that students, on average, retain at least 60% of their basic science knowledge from pre-clerkship. However, regardless of students’ average scores, our data also highlighted that there are some basic science concepts where the average grade of the students is below the minimal level of competency (60%). One way in which curricula committees and educators can help increase students’ basic science knowledge levels is by incorporating more well-defined assessment outcomes throughout pre-clerkship. Under this curricular framework, all students can work towards achieving the same academic goals, and thus, educators can ensure that all trainees are attaining the minimum level of proficiency in the basic sciences that are necessary for students to successfully transition to clerkship. We also found that students, on average, reinforced fundamental concepts during clerkship, suggesting that the clinical experience of clerkship has a positive influence on students’ basic science knowledge levels. Interestingly, the largest increase from pre- to post-test scores occurred during the pediatric rotation where there was a higher volume of out-of-clinic learning sessions. This result suggests that through the integration of more basic science learning sessions during clerkship year, we may be able to enhance students’ understanding of fundamental basic science concepts. Most notably, our data revealed that even though lower-performing students demonstrated the greatest improvement on the post-test, they still displayed deficits in their basic science knowledge at the end of each rotation, when compared with their higher-performing peers. This finding indicates that the clinical experience of clerkship appears to be most beneficial for lower-performing students’ basic science knowledge. As previously discussed, learning the basic sciences with a clinical focus has been shown to enhance students’ learning of the material. Thus, these results from this study may suggest that earlier exposure to clinical experiences could enhance the relevance of the basic sciences, thereby promoting an increased rate of basic science knowledge retention. Therefore, by enhancing the integration between the basic and clinical sciences via earlier clinical experiences during pre-clerkship and extending basic science education into clerkship year, we may be able to help foster students’ basic science knowledge retention so that all students are well equipped with the basic science knowledge that is necessary for successful clinical practice. Moving forward, future research should explore the impact of earlier clinical experiences on students’ basic science knowledge levels during their pre-clerkship training, to help ensure all students are competent in the fundamental knowledge prior to entering a clinical setting.
Data Availability
Available upon request.
Change history
02 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40670-021-01444-2
References
Flexner A. Medical education in the United States and Canada: a report to the Carnegie Foundation for the advancement of teaching. Carnegie Bulletin. New York: The Carnegie Foundation for the Advancement of Teaching; 1910.
Finnerty EP, Chauvin S, Bonaminio G, Andrews M, Carroll RG, Pangaro LN. Flexner revisited: the role and value of the basic sciences in medical education. Acad Med. 2010;85:349–55.
Woods NN, Brooks LR, Norman GR. The value of basic science in clinical diagnosis: creating coherence among signs and symptoms. Med Educ. 2005;39:107–12.
Spencer AL, Brosenitsch T, Levine AS, Kanter SL. Back to the basic sciences: an innovative approach to teaching senior medical students how best to integrate basic science and clinical medicine. Acad Med. 2008;83:662–9.
Pawlina W. Basic sciences in medical education: why? How? When? Where? Med Teach. 2009;31:787–9.
McColl GJ, Bilszta J, Harrap S. The requirement for bioscience knowledge in medical education. Med J of Aust. 2012;2012(196):409.
Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med. 2013;88:1407–10.
Pascual TN, Chhem R, Wang SC, Vujnovic S. Undergraduate radiology education in the era of dynamism in medical curriculum: an educational perspective. Euro J of Rad. 2011;78:319–25.
Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, Laur C, Lenders CM, Levy MD, Palmer CA, Pratt CA, Rock CL, Saltzman E, Seider DL, Van Horn L. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Amer J of Clin Nutr. 2014;99(5):1153–66.
Boshuizen HP, Schmidt HG. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci. 1992;16(2):153–84.
Custers EJ, ten Cate OT. Very long-term retention of basic science knowledge in doctors after graduation. Med Educ. 2011;45(4):422–30.
Nouns Z, Schauber S, Witt C, Kingreen H, Schüttpelz-Brauns K. Development of knowledge in basic sciences: a comparison of two medical curricula. Med Educ. 2012;46(12):1206–14.
Barrows HS, Feltovich PJ. The clinical reasoning process. Med Educ. 1987;21:86–91.
Woods NN, Brooks LR, Norman GR. The role of biomedical knowledge in diagnosis of difficult clinical cases. Adv in Health Sci Educ. 2007;12:417–26.
Pangaro LN. The role and value of the basic sciences in medical education: the perspective of clinical education–students’ progress from understanding to action. Med Sci Educ. 2010;20:307–13.
Lazić E, Dujmović J, Hren D. Retention of basic sciences knowledge at clinical years of medical curriculum. Croat Med J. 2006;47:882–90.
Malau-Aduli BS, Lee AY, Cooling N, Catchpole M, Jose M, Turner R. Retention of knowledge and perceived relevance of basic sciences in an integrated case-based learning (CBL) curriculum. BMC Med Educ. 2013;13(1):139.
West C, Kurz T, Smith S, Graham L. Are study strategies related to medical licensing exam performance? Intern J of Med Educ. 2014;5:199.
Smith K. The case for basic sciences in the undergraduate curriculum. Clin Teach. 2010;7:211–4.
Norman GR, Trott AD, Brooks LR, Smith EKM. Cognitive differences in clinical reasoning related to postgraduate training. Teach and Learn in Med: An Intern J. 1994;1994(6):114–20.
Norman G. How basic is basic science? Adv Health Sci Educ Theory Pract. 2007;12:401–3.
Ling YU, Swanson DB, Holtzman K, Bucak SD. Retention of basic science information by senior medical students. Acad Med. 2008;83(10):82–5.
Schneid SD, Pashler H, Armour C. How much basic science content do second-year medical students remember from their first year? Med Teach. 2019;41:231–3.
Tokuda Y, Goto E, Otaki J, Jacobs J, Omata F, Obara H, Takahashi O. Undergraduate educational environment, perceived preparedness for postgraduate clinical training, and pass rate on the National Medical Licensure Examination in Japan. BMC Med Educ. 2010;10(1):35.
Weggemans MM, Custers EJ, ten Cate OT. Unprepared retesting of first year knowledge: how much do second year medical students remember? Med Sci Educ. 2017;27(4):597–605.
D’Eon MF. Knowledge loss of medical students on first year basic science courses at the University of Saskatchewan. BMC Med Educ. 2006;6(1):5.
Sanson-Fisher RW, Rolfe IE, Williams N. Competency based teaching: the need for a new approach to teaching clinical skills in the undergraduate medical education course. Med Teach. 2005;27:29–36.
Dahle LO, Brynhildsen J, Fallsberg MB, Rundquist I, Hammar M. Pros and cons of vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum: examples and experiences from Linköping. Sweden Med Teach. 2002;24:280–5.
Ambrose SA, Bridges MW, DiPietro M, Lovett MC, Norman MK. How learning works: seven research-based principles for smart teaching. John Wiley & Sons. 2010.
Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach. 2015;37:312–322.
Cooke M, Irby DM, O’Brien BC. Educating physicians: a call for reform of medical school and residency. John Wiley & Sons. 2010.
Kossoff EH, Hubbard TW, Gowen CW Jr. Early clinical experience enhances third-year pediatrics clerkship performance. Acad Med. 1999;74:1238–41.
Dyrbye LN, Harris I, Rohren CH. Early clinical experiences from students’ perspectives: a qualitative study of narratives. Acad Med. 2007;82:979–88.
Wilkinson TJ, Gower S, Sainsbury R. The earlier, the better: the effect of early community contact on the attitudes of medical students to older people. Med Educ. 2002;36:540–2.
Kulasegaram KM, Martimianakis MA, Mylopoulos M, Whitehead CR, Woods NN. Cognition before curriculum: rethinking the integration of basic science and clinical learning. Acad Med. 2013;88:1578–85.
Wijnen-Meijer M, ten Cate OTJ, van der Schaaf M, Borleffs JC. Vertical integration in medical school: effect on the transition to postgraduate training. Med Educ. 2010;44:272–9.
Cameron A, Millar J, Szmidt N, Hanlon K, Cleland J. Can new doctors be prepared for practice? A review Clin Teach. 2014;11:188–92.
Norris ME, Cachia MA, Johnson MI, Rogers KA, Martin CM. Expectations and perceptions of students’ basic science knowledge: through the lens of clerkship directors. Med Sci Educ. 2020;1–11.
Swanson DB, Case SM, Luecht RM, Dillon GF. Retention of basic science information by fourth-year medical students. Acad Med. 1996;71:80–2.
Custers EJ. Long-term retention of basic science knowledge: a review study. Adv in Health Sci Educ. 2010;15:109–28.
Baciewicz FA Jr, Arent L, Weaver M, Yeastings R, Thomford NR. Influence of clerkship structure and timing on individual student performance. Amer J of Surg. 1990;159:265–8.
Cho JE, Belmont JM, Cho CT. Correcting the bias of clerkship timing on academic performance. Arch of Ped and Adolescent Med. 1998;152:1015–8.
Hampton HL, Collins BJ, Perry JK, Meydrech EF, Wiser WL, Morrison JC. Order of rotation in third-year clerkships. Influence on academic performance. J of Repro Med. 1996;41:337–340.
Manley M, Heiss G. Timing bias in the psychiatry subject examination of the National Board of Medical Examiners. Acad Psych. 2006;30:116–9.
Park RS, Chibnall JT, Morrow A. Relationship of rotation timing to pattern of clerkship performance in psychiatry. Acad Psych. 2005;29:267–73.
Blunt MJ, Blizard PJ. Recall and retrieval of anatomical knowledge. Bri J of Med Educ. 1975;9:252–63.
Weitman M. A study of long-term retention in medical students. J of Experi Educ. 1964;1964(33):87–91.
Rodriguez R, Campos-Sepulveda E, Vidrio H, Contreras E, Valenzuela F. Evaluating knowledge retention of third-year medical students taught with an innovative pharmacology program. Acad Med. 2002;77:574–7.
Chen HC, van den Broek WS, ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Harris P, Snell L, Talbot M, Harden RM, International CBME Collaborators. Competency-based medical education: implications for undergraduate programs. Med Teach. 2010;32:646–650.
O’Brien BC, Irby DM. Enacting the Carnegie Foundation call for reform of medical school and residency. Teach and Learn in Med. 2013;25:S1–8.
Simpson JG, Furnace J, Crosby J, Cumming AD, Evans PA, David MFB, Harden RM, Lloyd D, McKenzie H, McLaghaln JC, McPhate GF, Percy-Robb IW, MacPherson SG. The Scottish doctor-learning outcomes for the medical undergraduate in Scotland: a foundation for competent and reflective practitioners. Med Teach. 2002;24:136–43.
Sonnadara RR, Mui C, McQueen S, Mironova P, Nousiainen M, Safir O, Reznick R. Reflections on competency-based education and training for surgical residents. J of Surg Educ. 2014;71:151–8.
Myhre DL, Woloschuk W, Jackson W, McLaughlin K. Academic performance of longitudinal integrated clerkship versus rotation-based clerkship students: a matched-cohort study. Acad Med. 2014;89:292–5.
Koles P, Nelson S, Stolfi A, Parmelee D, DeStephen D. Active learning in a year 2 pathology curriculum. Med Educ. 2005;39:1045–55.
Healy DG, Fleming FJ, Gilhooley D, Felle P, Wood AE, Gorey T, McDermott EW, Fitzpatrick JM, O’Higgins NJ, Hill AD. Electronic learning can facilitate student performance in undergraduate surgical education: a prospective observational study. BMC Med Educ. 2005;5:23.
Lufler RS, Zumwalt AC, Romney CA, Hoagland TM. Effect of visual–spatial ability on medical students’ performance in a gross anatomy course. Anat Sci Edu. 2012;5:3–9.
Rifkin B. A ceiling effect in traditional classroom foreign language instruction: data from Russian. Modern Language J. 2005;89:3–18.
Keeley J, Zayac R, Correia C. Curvilinear relationships between statistics anxiety and performance among undergraduate students: evidence for optimal anxiety. Stat Educ Res J. 2008;7:4–15.
Albanese M. Problem-based learning: why curricula are likely to show little effect on knowledge and clinical skills. Med Educ. 2000;34:729–38.
Lycke KH, Grøttum P, Strømsø HI. Student learning strategies, mental models and learning outcomes in problem-based and traditional curricula in medicine. Med Teach. 2006;8:717–22.
Helle L, Nivala M, Kronqvist P, Ericsson KA, Lehtinen E. Do prior knowledge, personality and visual perceptual ability predict student performance in microscopic pathology? Med Educ. 2010;44:621–9.
Barbeau ML, Johnson M, Gibson C, Rogers KA. The development and assessment of an online microscopic anatomy laboratory course. Anat Sci Educ. 2013;6:246–56.
Attardi SM, Rogers KA. Design and implementation of an online systemic human anatomy course with laboratory. Anat Sci Educ. 2015;8:53–62.
Tayade D, Dandekar K. The impact of early clinical exposure on first MBBS students. Intern J of Health and Biomed Res. 2014;2:176–81.
Rawekar A, Jagzape A, Srivastava T, Gotarkar S. Skill learning through early clinical exposure: an experience of Indian medical school. J Clin Diagnostic Res. 2016;10:JC01-JC04.
Rajan SJ, Jacob TM, Sathyendra S. Vertical integration of basic science in final year of medical education. Intern J of Applied and Basic Med Res. 2016;6:182–5.
Ryan MS, Feldman M, Bodamer C, Browning J, Brock E, Grossman C. Closing the gap between preclinical and clinical training: impact of a transition-to-clerkship course on medical students’ clerkship performance. Acad Med. 2020;95:221–5.
Hopkins R, Pratt D, Bowen JL, Regehr G. Integrating basic science without integrating basic scientists: reconsidering the place of individual teachers in curriculum reform. Acad Med. 2015;90:149–53.
Acknowledgements
We wish to thank UME clerkship directors and scientists (Drs. Johnson, Crowley, Ceccini, Heinemann) at the Schulich School of Medicine & Dentistry and the fourth-year medical student focus group for reviewing and providing editorial feedback on the basic science assessments prior to implementation.
Funding
This research was funded by the Government of Ontario (Ontario Graduate Scholarship) and the American Association for Anatomy (Education Research Scholarship) and Schulich School of Medicine & Dentistry's Summer Research Training Program (University of Western Ontario).
Author information
Authors and Affiliations
Contributions
All authors made contributions to the study design, and/or data analysis, and/or data interpretation. Additionally, all authors were involved in drafting and/or editing this manuscript and provided final approval.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Norris, M.E., Cachia, M.A., Johnson, M.I. et al. Are Clerks Proficient in the Basic Sciences? Assessment of Third-Year Medical Students’ Basic Science Knowledge Prior to and at the Completion of Core Clerkship Rotations. Med.Sci.Educ. 31, 709–722 (2021). https://doi.org/10.1007/s40670-021-01249-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-021-01249-3