Abstract
Basic sciences are a cornerstone of undergraduate medical education (UME) as they provide a necessary foundation for the clinical sciences to be built upon and help foster trainees’ competency. However, research indicates that students’ basic science knowledge is not well retained, and as a result, students are ill-prepared, with respect to their basic science knowledge, when entering clerkship. One potential reason why students may not be prepared for clerkship is a lack of understanding as to which basic science concepts are critical for medical students to retain from pre-clerkship. We facilitated interviews with all core UME clerkship directors to establish which basic science concepts they expect students to know prior to each clerkship rotation, along with student’s basic science strengths and areas of improvement. Interviews revealed that students are expected to have some knowledge of every basic science prior to clerkship, with pharmacology being a strong focus, as many specialties deal with common drugs and classes of drugs. Additionally, general anatomy and physiology knowledge were deemed student strengths in two rotations. Clerkship directors focused on perceived areas of improvement more than perceived strengths, with the most prevalent areas being pharmacology, microbiology, and detailed anatomy. These results represent views of clerkship directors from one Canadian institution; however, since clerks rotate through institutions across Canada, this data provides the impetus for creating a national discussion to help foster standardization of UME curricula, with the overarching goal of ensuring all graduates are proficient in the necessary fundamentals as they transition into residency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The basic sciences are a fundamental component of undergraduate medical education (UME) curricula, and pioneers of medical education believe that the basic sciences provide a necessary foundation in medical training [1,2,3,4,5]. Basic sciences are a cornerstone of medical education, providing the framework upon which the clinical sciences are built [2, 6,7,8,9]. In order to be proficient in a clinical setting, students must first master normal structure and function of the basic sciences, following which they can start to create mental representations of diseases and conceptualize the relevant clinical concepts [4, 8, 10,11,12]. Not only do the basic sciences create a solid foundation for the understanding of clinical conditions [8, 12], but a strong basic science foundation has also been associated with enhanced diagnostic accuracy in the clinic [4, 13, 14]. For patients that are presenting with complex signs and symptoms that are not easily diagnosable, trainees must rely on their basic science foundation in order to interpret the clinical condition, problem solve, and ultimately reach a conclusion [4, 11, 15]. The importance of a basic science foundation holds true even as trainees are approaching clinical expertise, as basic science knowledge has also been shown to be a vital element for practicing physicians and experts in the field [16,17,18]. With the basic sciences essentially being the language of medicine [19], trainees must be proficient in the necessary fundamentals in order to navigate the exponentially increasing body of both basic and clinical science medical research [4], and ultimately keep up with today’s dynamic health care demands [20, 21].
Abraham Flexner was a pioneer of medical education who believed that basic science education was the cornerstone of UME curricula [1, 2]. Flexner created a UME curricular model in which the first two years comprised basic science education, followed by two years of clinical training [1, 5, 14, 22]. Nowadays, the importance of basic science rigor during pre-clerkship continues to be supported by present-day educators and learners as most Canadian medical schools follow an adapted Flexnerian model of medical education in which the basic and clinical sciences are integrated into the first two years of study (pre-clerkship), with the remaining two years focusing primarily on clinical training [6, 8, 12, 14, 19]. Regardless of this time-tested model [23], one challenge that many curricula committees and educators are faced with is determining which basic science content to include in pre-clerkship. Currently, there is no core basic science curriculum or standardized syllabus outlining which concepts are critical for medical students to retain by the end of their pre-clerkship training, and as a result, the basic science curricula tend to develop and evolve independently at each institution [5]. Based on the literature, we know that pre-clerkship should focus on fundamental basic science and medical knowledge to prepare trainees for their future career [4, 16]; however, the specific basic science concepts that students are expected to know, and the depth in which they are expected to learn them, have yet to be determined [4].
Furthermore, research demonstrates that students’ basic science knowledge from their pre-clerkship training is not well retained [12, 14, 24, 25], and there is a further decline of trainees’ basic science knowledge as they progress through their education [26]. This decrement of basic science knowledge can unfortunately translate to a lack of overall competency as students complete their medical training, and can also result in poor outcomes on medical board examinations [12, 17, 27]. Moreover, although the literature demonstrates that teaching the basic sciences in conjunction with the underlying clinical relevance can actually help foster students’ basic science knowledge retention [28, 29], the integration of clinical sciences into pre-clerkship decreases the time dedicated to the basic sciences [30, 31], which may also negatively influence students’ knowledge retention. Thus, based on the current reported retention rates of students’ basic science knowledge, we need to ensure trainees are retaining the relevant basic science concepts, and are proficient in the necessary fundamentals prior to entering a clinical setting.
As previously discussed, the goal of UME is to provide students with the necessary knowledge and skills that will set them up for clinical success after graduation. However, research indicates that students training under present-day UME curricula often display a lack of confidence and proficiency as they transition into a clinical setting, which is likely multi-factorial, but may be due to a weak basic science foundation [30]. This lack of clinical competence is echoed by research indicating that a number of newly minted medical graduates often feel unprepared for clinical practice, with respect to their basic science knowledge [32]. While there is variability among institutions and graduating cohorts, the literature highlights that the number of students who feel unprepared for practice, with respect to their basic science knowledge, can range from 8% upwards of 81% [32,33,34], which can unfortunately translate to a decreased quality of patient care [32]. The lack of proficiency and basic science knowledge retention we see in current trainees may also be stemming from a disconnect among medical educators within the various stages of medical training, such as pre-clerkship and clerkship. While these medical educators may consider all basic science content to be important in UME, it remains unclear which basic science concepts can lead to enhanced student performance in clerkship. Therefore, by facilitating communication among pre-clerkship, clerkship, and residency educators, we can hopefully improve basic science education in UME, thereby promoting continuity throughout a trainees’ medical education and fostering student success in a clinical setting.
Based on the necessity of basic science knowledge, the current reported knowledge retention rates, and the perceptions of current medical graduates, there is a need for an educational model that ensures students are proficient and competent in the necessary basic science fundamentals prior to clerkship, and ultimately prior to graduation. The literature has been focused on the expectations of students’ clinical skills and competencies, such as professionalism and communication, prior to clerkship [35, 36]; however, the specific basic science concepts that should be delivered in pre-clerkship curricula, and the detail in which they need to be taught, is currently unknown. Thus, the purpose of this study was to determine which basic science concepts UME clerkship directors expect medical students to know prior to entering each clerkship rotation, along with their perceptions of current student strengths and areas requiring improvement, with respect to their basic science knowledge.
Materials and Methods
Schulich UME Curriculum
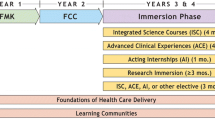
The Schulich School of Medicine & Dentistry has two campuses located in London, Ontario, Canada, and Windsor, Ontario, Canada. Within the current UME curriculum at the Schulich School of Medicine & Dentistry, the basic and clinical sciences are integrated into systems-based courses that span years one and two. In year one, students study the basic and clinical sciences in the following courses: Introduction to Medicine, Blood, Infection & Immunity, Skin, Heart & Circulation, Respiration & Airways, and Genitourinary. In the second year of study, the basic and clinical sciences are incorporated into Digestion & Nutrition, Endocrine & Metabolism, Reproduction, Musculoskeletal System, Neurosciences, Eye & Ear, and Psychiatry & Behavioral Sciences. Following the first two years of study, students begin clerkship year, in which there are six different core rotations: pediatrics, obstetrics and gynecology (OB/GYN), internal medicine, family medicine, psychiatry, and surgery (Table 1). Students are also required to participate in an emergency medicine and an anesthesia rotation, which are mandatory sub-rotations of internal medicine and surgery, respectively.
Clerkship Director Interviews
Schulich’s basic science pre-clerkship UME curriculum course objectives were reviewed by two authors including a UME assistant professor and a doctoral student. The objectives were used as a framework to create an interview questionnaire. Prior to implementation, the interview questionnaire was reviewed by an educational researcher at The University of Western Ontario to ensure the questions were impartial and targeted towards the basic science pre-clerkship curriculum. The questionnaire comprised inquiries that assess clerkship director’s expectations of students’ basic science knowledge, along with clerkship director’s perceptions of current student strengths and weaknesses, and included questions such as “Which basic science concepts are students expected to know coming into this clerkship rotation?”, along with more targeted questions such as, “Which, if any, specific developmental conditions, fetal or embryonic, are students expected to have the fundamental knowledge of, in terms of identifying and explaining the anatomical basis, prior to entering the rotation?”. Depending on the clerkship director’s answers, follow-up questions, such as “Which developmental conditions do you feel students struggle with the most?”, were asked.
Using the questionnaires as a guide, 1-h interviews were conducted with UME clerkship directors from both London and Windsor campuses for the six core clerkship rotations: family medicine, internal medicine, OB/GYN, surgery, pediatrics, and psychiatry. The clerkship directors of the two core sub-rotations, anesthesia and emergency medicine, were also interviewed. Each campus has 1–2 clerkship directors for each rotation; thus, the number of clerkship directors present at each interview varied (Table 2). Interviews were audio-recorded (using QuickTime Player–Audio Version 10.4), following which the interviews were transcribed. A codebook based on the six core basic sciences was created and used as a template (Table 3). During the interview process, certain basic science themes emerged, such as genetics and immunology, and these themes were included in the codebook as subcomponents; however, the subcomponents were not part of the interview questionnaire and so not all clerkship directors were asked about these subcomponents.
The interview transcripts were then coded by two researchers (using ATLAS.ti software Version 1.6.0) according to the template in Table 3, and into the following categories: (i) which basic science concepts clerkship directors deemed to be necessary and (ii) perceived student strengths or (iii) perceived areas requiring improvement with respect to basic science knowledge (Fig. 1). It should be noted that Nutrition and Imaging are not classified as basic sciences; however, these topics were discussed with the clerkship directors as they are an integral part of UME curricula and an essential link between the basic and clinical sciences [37, 38].
Statistical Analysis
Using the coding data output from ATLAS.ti, frequencies of the basic science themes were calculated for each clerkship rotation based on the averages between the two coders. Intraclass correlation coefficients (ICC) were used to assess the inter-rater reliability of codes, and the average measures of the ICC tests were reported. Intraclass correlation coefficient statistical analyses were performed in SPSS using a reliability measures, two-way mixed model (IBM SPSS Version 21; Armonk, NY, USA). The following ICC intervals were used to define the magnitude of reliability [39]: ICC < 0.4 = poor; 0.4 < ICC < 0.59 = fair; 0.60 < ICC < 0.74 = good; ICC > 0.74 = excellent.
Results
The themes depicted in Fig. 2 demonstrate the prevalence of each basic science appearing in the transcribed interviews from all six core clerkship rotations and the two sub-rotations of anesthesia and emergency medicine. Overall, data revealed that students were expected to have some knowledge of every basic science prior to entering clerkship year. More specifically, pharmacology was the most prevalent, and biochemistry was the least prevalent, with respect to which basic science concepts third-year medical students are expected to know prior to entering clerkship. The ICC indicated excellent reliability (≥ 0.89) of the coding data for each clerkship rotation.
Interview transcripts indicated that pharmacology had the highest frequency rate in four clerkship rotations: internal medicine, surgery, family medicine, and psychiatry. The clerkship directors of these rotations identified classes of drugs, drug dosing, and drug interventions as fundamental pharmacological concepts that undergraduate medical students should know prior to entering clerkship year. Contrary to this, biochemistry was only deemed necessary by the OB/GYN clerkship directors, and this was in regard to hormones and hormone structure. Directors of surgery and pediatrics rotations deemed the anatomical sciences of higher importance compared with other basic sciences. Some examples of gross anatomical and embryological concepts highlighted were arterial supply, innervation, anatomical relationships, normal embryological development, and malformation. Histology and neuroanatomy were seldom mentioned by clerkship directors as these topics tend to become more of a focus in upper year selectives. The data also demonstrated that pathology and physiology knowledge is expected in every rotation. The most prevalent pathologies identified by the clerkship directors were pneumonia, chronic obstructive pulmonary disease, diabetes, hypertension, and polycystic ovarian syndrome. These conditions were supported by the physiology concepts deemed necessary by clerkship directors, such as heart and lung physiology, IV fluids, ovulation, and the underlying physiology of cellular dynamics and the coagulation cascade. Furthermore, microbiology concepts of infection, abscesses, and common bacteria were deemed necessary by family medicine, internal medicine, emergency medicine, OB/GYN, surgery, and pediatrics directors. Microbiology was not identified by the psychiatry or anesthesia clerkship directors, as they indicated that they typically do not deal with microorganisms within their respective specialty.
Nutrition and imaging are not classified as core basic sciences; however, these topics were also discussed with clerkship directors as they are an integral part of pre-clerkship and must be integrated with the basic and clinical sciences [35, 36]. With respect to imaging, understanding the benefits and drawbacks of different imaging modalities, along with an approach to a chest x-ray, were the main concepts identified by surgery, family medicine, OB/GYN, psychiatry, and emergency medicine clerkship directors. Nutrition was deemed important for all eight required clerkship rotations, and was focused around basic dietary needs of different patient populations, along with drug interactions with certain foods, vitamins, and minerals (Table 4).
When discussing basic science concepts that current students are proficient in prior to clerkship, directors from two rotations, internal medicine and family medicine, were able to identify perceived student strengths, which were anatomy and physiology. These rotation directors indicated that students coming into their rotations “knew their anatomy”; however, they also noted that students only needed a “general” anatomical knowledge base, with less specifics, for these specialties. Physiology was also identified as a student strength by the internal medicine clerkship directors, as they stated that current students “typically have a solid foundation of physiology” upon which important clinical concepts can be built, but once again were only expected to have a general knowledge of this basic science. The clerkship directors of the remaining rotations (emergency medicine, surgery, anesthesia, OB/GYN, pediatrics, psychiatry) did not indicate any student strengths, despite being asked directly for comments on student basic science strengths (Table 5).
Clerkship directors identified areas where students could improve their level of knowledge in every basic science. However, anatomy (surgery, emergency medicine, OB/GYN, anesthesia), microbiology (family medicine, internal medicine, OB/GYN, pediatrics), and pharmacology (internal medicine, emergency medicine, OB/GYN, anesthesia) were identified as the most prevalent basic sciences requiring improvement. Surgery rotation directors identified arterial supply, important arterial branches, and anatomical relationships as anatomical areas requiring improvement. One example provided by surgery clerkship directors was that students should know the head of the pancreas is resected with the duodenum because of the shared blood between the two structures during a Whipple’s procedure. The clerkship director of emergency medicine identified a lack of knowledge in musculoskeletal (MSK) anatomy, specifically the hand since many individuals present to the emergency department with hand lacerations. Vasculature of the pelvis and respiratory system anatomy were identified as areas requiring improvement by OB/GYN and anesthesia clerkship directors, respectively. When discussing microbiology, OB/GYN clerkship directors identified infectious diseases, wound infection, and abscesses as areas where student knowledge is currently lacking. Collectively, family medicine, internal medicine, and pediatrics rotation directors identified general microbiology and underlying microorganisms as an area needing improvement for current students. In regard to pharmacology, antibiotics and appropriate treatment of infectious diseases were identified as topics requiring improvement by both internal medicine and OB/GYN clerkship directors. The emergency medicine rotation director indicated toxicology and pharmacological resuscitation as areas where students should improve their knowledge prior to clerkship. Many students are presented with patients suffering from hypotension, hypertension, bradycardia, or tachycardia during their clerkship year; thus, the anesthesia rotation director identified that incoming student’s knowledge of pharmacological treatments for these conditions could be improved (Table 5).
Discussion
Basic sciences are a cornerstone of UME, and educators believe that a strong basic science foundation is necessary for medical students to achieve overall competence [1,2,3,4,5, 8, 9]. However, the specific basic science concepts students need to retain from pre-clerkship, and the depth in which they are expected to learn them, have yet to be determined. This poses a challenge when curricula committees and educators are trying to determine which content to incorporate into their UME program. One way to approach this discrepancy is by increasing communication between pre-clerkship and clerkship educators and incorporating the basic science concepts that clerkship directors deem “necessary for students to know” into the pre-clerkship curriculum. In this study, we found that clerkship directors expect students to have some knowledge of every basic science prior to entering clerkship year, with pharmacology being the most prevalent for students to know, and biochemistry the least. When discussing current students’ basic science knowledge, clerkship directors noted more areas where they would like to see improved basic science knowledge than students’ strengths in current knowledge.
Pharmacology was deemed necessary for students to know prior to every rotation as students must know common drugs and classes of drugs for every specialty. Pharmacology is a fundamental aspect of medical education [40, 41], and based on our results, it was the most prevalent basic science identified in family medicine, surgery, internal medicine, and psychiatry, as these specialties heavily rely on pharmacological interventions. Additionally, four clerkship directors (internal medicine, emergency medicine, OB/GYN, anesthesia) identified pharmacology as a basic science where students could improve their knowledge level. Other basic sciences, such as physiology and biochemistry, underpin pharmacology [42], and this complexity may lead to clerkship directors perceiving a lack of knowledge in current trainees [43]. However, medical students are not the only cohort struggling with pharmacology; other studies indicate that junior doctors also lack confidence and proficiency in their ability to safely prescribe medications [43, 44]. By not having a fundamental working knowledge of the underlying basic sciences, such as physiology and biochemistry, students may not achieve a full understanding of pharmacology, which consequently could negatively affect their proficiency in clerkship and lead to this perception clerkship directors have of students.
Anatomy and physiology were also deemed fundamental for students to know by all rotation directors, which is in agreement with Flexner who stated that anatomy and physiology are the pillars of a strong basic science foundation [1], and more recent educator-scholars who suggest that UME curricula must ensure that medical students are receiving a robust education in these two basic sciences [45,46,47]. With anatomy and physiology being complementary basic sciences, structure and function are often taught in tandem with one another, and this integration may symbiotically promote knowledge retention of each subjects’ concepts [9]. The family and internal medicine clerkship directors identified anatomy and physiology as current student strengths. Although students were only expected to have a general knowledge of these subjects, our data suggests that students’ pre-clerkship education is providing them with the anatomical and physiological foundational knowledge necessary for success in these two rotations. In contrast, clerkship directors indicated that students’ knowledge of anatomy and physiology required improvement when entering the remaining rotations (OB/GYN, surgery, pediatrics, psychiatry, anesthesia, emergency medicine), noting that these rotations require students to know more complex and detailed concepts related to each basic science. There are multiple factors that could influence students’ knowledge retention of more complex anatomy and physiology content [48, 49], but based on the necessity of a strong foundation in these two basic sciences for the successful practice of medicine, we must ensure that students are learning and retaining the necessary concepts that are fundamental for every clerkship rotation.
Pathology was deemed necessary by all rotation directors supporting the literature indicating that it is a vital component to the study of medicine [50,51,52]. Clerkship directors did not indicate pathology as a strength or an area requiring improvement suggesting they perceive students to have an adequate level of pathology knowledge when entering clerkship. As previously mentioned, many present-day UME curricula integrate the clinical and basic sciences in pre-clerkship resulting in the underlying pathologies and clinical conditions being taught in conjunction with the “normal” structure and function. This integration may foster students’ knowledge retention of pathology.
Microbiology was deemed necessary for students to know in five of the six core clerkship rotations, with the exception of psychiatry, and was further identified as an area where students could improve by family medicine, internal medicine, OB/GYN, and pediatrics clerkship directors. Literature indicates that there is limited time dedicated to microbiology in UME, which may lead to a lack of microbiology knowledge in current students [53]. Consequently, this deficiency in knowledge may translate to decreased diagnostic accuracy in the clinic [54]. This provides the impetus to review the intricacies of microbiology content within the curriculum, with the overarching goal of enhancing microbiology education in UME.
Biochemistry was only deemed necessary for students to know by OB/GYN directors in regard to reproductive hormones, which initially suggests that most rotation directors do not consider this basic science necessary for students to know prior to entering clerkship. However, as previously mentioned, biochemistry underpins and compliments other basic sciences, such as pharmacology [42]. For clerkship directors and practicing physicians, this biochemical knowledge may now be second nature as they are relying on it daily when prescribing and adjusting pharmacological treatment plans [55, 56], whereas medical students still need to develop their foundational background. Therefore, this basic science is still fundamental for students to learn during pre-clerkship, but the relevance of biochemistry and the way in which it is integrated into UME curricula may need to be revised [55].
Nutrition was deemed fundamental for students to know for each rotation, as it can play an integral role in disease prevention and treatment [57, 58]. However, the literature indicates that nutrition education is inadequate in many UME curricula [57]. As a result, clinicians are not confident in providing nutritional counseling to patients [59, 60], which was echoed in our interviews when clerkship directors perceived students as being uncomfortable with nutritional counseling for patients. Therefore, it is necessary to ensure students are receiving a comprehensive education in nutrition across all specialties and body systems, ultimately providing them with the knowledge and confidence to provide patients with nutritional guidance [59].
Imaging was deemed essential by four clerkship directors (surgery, family medicine, OB/GYN, psychiatry). While students are not required to understand the intricacies and complexities of all imaging modalities prior to clerkship, clerkship directors noted that it is pertinent that they know basic x-ray practices. The use of all imaging techniques is on the rise due to factors such as improved technology and an increased demand from today’s patient population and can lead to earlier diagnoses for certain clinical conditions [61]. However, errors in diagnosis, or misdiagnosis, can result in serious or fatal medical mistakes [62]. Therefore, it is imperative that medical students are learning and retaining the necessary fundamentals of medical imaging during their pre-clerkship training so they can effectively employ various modalities as a supplemental tool to accurately diagnose patients and promote positive patient outcomes.
Graduates are competent medical trainees who perform well on Medical Council of Canada licensing exams; however, clerkship directors still identified many areas where students could be stronger in their basic science knowledge. These findings are consistent with literature indicating that students are lacking basic science knowledge after completing their pre-clerkship training [12, 14, 24, 25], and although the basic science concepts are taught during pre-clerkship, it has been shown that students lose their basic science knowledge as they progress through the remainder of their medical training [26]. Further to this, research indicates that new medical graduates often lack proficiency and feel ill-prepared for clinical practice with respect to their basic science knowledge [30, 32,33,34]. Unfortunately, these shortcomings in basic science knowledge can result in a lack of overall competence in medical training, which ultimately can translate to poorer patient care [32]. Based on these findings, one may question why clerkship directors perceive students are not retaining fundamental basic science content, despite it being taught in the curriculum.
There are likely many elements that are influencing these perceptions. One potential factor is that pre-clerkship courses are delivering too much information, which can lead to superficial learning of the content, making it difficult for students to retain the high-yield, fundamental basic science concepts that are required for clerkship [2, 63]. Another potential factor could be a lack of integration between some basic and clinical science concepts [64]; as a result, basic science concepts are typically out of context which can impede students’ learning and retention of basic science knowledge [22], and negatively affect their abilities in clerkship. Or could the clerkship directors’ perceptions be due to a disconnect between what pre-clerkship educators are teaching and what knowledge clerkship educators are expecting? This study reveals the expectations of the clerkship directors, and the collected information will be fed forward to pre-clerkship educators to promote continuity between pre-clerkship and clerkship education. Moving forward, the data collected from this study can be used as a guide to assess students’ basic knowledge retention and to evaluate the current basic science curriculum with the overarching goal of improving basic science education in UME.
Limitations
The observations identified in this study are from a single institution; therefore, results may vary not only between clerkship directors and preceptors but also across UME curricula; however, this data provides insight into the concepts clerkship directors are expecting students to know and because undergraduate medical trainees participate in elective clerkship rotations across Canada, this is an expectation of all students nationally. When interviewing the clerkship directors, the interviews were guided with the use of questionnaires, while the questionnaires aided in providing consistency across all interviews and helped to guide the discussion in a sequential manner, the structured format of the interviews may have limited the conversation, and as a result, key discussion points may have been missed. One caveat to the interviews is that it was purely based on the clerkship directors’ perceptions of current students’ basic science knowledge; thus, some potential biases could have stemmed from the interviews as the directors could have been biased towards their specialty. Additionally, negative information tends to have a stronger influence during evaluations, compared with positive information [65], which likely influenced the data when discussing current student strengths and weaknesses. To support this likelihood, clerkship directors mentioned in the interviews that they are not surprised when a clerk knows something while on rotation, but what does catch them off guard is when a clerk is lacking fundamental knowledge. Thus, while clerkship directors’ views of students’ basic science knowledge level are informative, their perceptions are just one factor that will be used in conjunction with other metrics to inform curricular decisions.
Conclusion
Clerkship directors expect students to bring knowledge of every basic science to their clerkship rotations. Additionally, they perceive there to be many areas where students could improve their basic science knowledge level, as they are transitioning into clerkship. These perceptions are likely multifactorial; however, some potential factors may be teaching too much detail that it overshadows the fundamental basic science concepts that students must know, a lack of integration between relevant basic and clinical science concepts, or a potential disconnect between pre-clerkship and clerkship curricula. Thus, this study provides the impetus to conduct further research to explore the potential influences on clerkship directors’ perceptions of medical students’ basic science knowledge. Although this research data only represents one intuition’s voice, due to the fact that clerks rotate through institutions across Canada, this discussion should be initiated at the national level to ensure that the expectations of students and the basic science concepts taught in pre-clerkship are standardized. Furthermore, this research methodology can be used as a template by other faculty and educators for evaluating which basic science content should be included in other pre-clerkship curricula, with goals of creating dialog across institutions, and ultimately, fostering consistency among basic science education in UME curricula.
References
Flexner A. Medical education in the United States and Canada: a report to the Carnegie Foundation for the advancement of teaching. Carnegie bulletin. New York: The Carnegie Foundation for the Advancement of Teaching 1910.
Finnerty EP, Chauvin S, Bonaminio G, Andrews M, Carroll RG, Pangaro LN. Flexner revisited: the role and value of the basic sciences in medical education. Acad Med. 2010;85:349–55.
Miles KA. Diagnostic imaging in undergraduate medical education: an expanding role. Clin Rad. 2005;60(7):742–5.
McColl GJ, Bilszta J, Harrap S. (2012). The requirement for bioscience knowledge in medical education. Med Journ of Aust. 2012;196(6):409.
Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med. 2013;88(10):1407–10.
Custers EJ, ten Cate OJ. Medical students’ attitudes towards and perception of the basic sciences: a comparison between students in the old and the new curriculum at the University Medical Center Utrecht. The Netherlands Med Educ. 2002;36:1142–50.
Harris DE, Hannum L, Gupta S. Contributing factors to student success in anatomy & physiology: lower outside workload and better preparation. Amer Bio Teach. 2004;66:168–75.
Woods NN, Brooks LR, Norman GR. The value of basic science in clinical diagnosis: creating coherence among signs and symptoms. Med Educ. 2005;39:107–12.
Norman G. How basic is basic science? Adv Health Sci Educ Theory Pract. 2007;12:401–3.
Boshuizen HP, Schmidt HG. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci. 1992;16(2):153–84.
Custers EJ, ten Cate OT. Very long-term retention of basic science knowledge in doctors after graduation. Med Educ. 2011;45(4):422–30.
Nouns Z, Schauber S, Witt C, Kingreen H, Schüttpelz-Brauns K. Development of knowledge in basic sciences: a comparison of two medical curricula. Med Educ. 2012;46(12):1206–14.
Woods NN, Brooks LR, Norman GR. The role of biomedical knowledge in diagnosis of difficult clinical cases. Adv in Health Sci Educ. 2007;12:417–26.
Spencer AL, Brosenitsch T, Levine AS, Kanter SL. Back to the basic sciences: an innovative approach to teaching senior medical students how best to integrate basic science and clinical medicine. Acad Med. 2008;83(7):662–9.
Smith K. The case for basic sciences in the undergraduate curriculum. Clin Teach. 2010;7(3):211–4.
Pawlina W. Basic sciences in medical education: why? How? When? Where? Med Teach. 2009;31(9):787–9.
Malau-Aduli BS, Lee AY, Cooling N, Catchpole M, Jose M, Turner R. Retention of knowledge and perceived relevance of basic sciences in an integrated case-based learning (CBL) curriculum. BMC Med Educ. 2013;13(1):139.
Kulasegaram KM, Chaudhary Z, Woods N, Dore K, Neville A, Norman G. Contexts, concepts and cognition: principles for the transfer of basic science knowledge. Med Educ. 2017;51(2):184–95.
Sivapragasam M. Basic science in integrated curricula. Persp on Med Educ. 2016;5(4):257–8.
Mylopoulos M, Woods N. Preparing medical students for future learning using basic science instruction. Med Educ. 2014;48:667–73.
Cutrer WB, Miller B, Pusic MV, Mejicano G, Mangrulkar RS, Gruppen LD, et al. Fostering the development of master adaptive learners: a conceptual model to guide skill acquisition in medical education. Acad Med. 2017;92:70–5.
Norman G. Teaching basic science to optimize transfer. Med Teach. 2009;31(9):807–11.
Hopkins R, Pratt D, Bowen JL, Regehr G. Integrating basic science without integrating basic scientists: reconsidering the place of individual teachers in curriculum reform. Acad Med. 2015;90(2):149–53.
D’Eon MF. Knowledge loss of medical students on first year basic science courses at the University of Saskatchewan. BMC Med Educ. 2006;6(1):5.
Weggemans MM, Custers EJ, ten Cate OT. Unprepared retesting of first year knowledge: how much do second year medical students remember? Med Sci Educ. 2017;27(4):597–605.
Ling YU, Swanson DB, Holtzman K, Bucak SD. Retention of basic science information by senior medical students. Acad Med. 2008;83(10):82–5.
Schneid SD, Pashler H, Armour C. How much basic science content do second-year medical students remember from their first year? Med Teach. 2019;41:231–3.
Custers EJ. Long-term retention of basic science knowledge: a review study. Adv in Health Sci Educ. 2010;15(1):109–28.
Swanson DB, Case SM, Luecht RM, Dillon GF. Retention of basic science information by fourth-year medical students. Acad Med. 1996;71:80–2.
Sanson-Fisher RW, Rolfe IE, Williams N. Competency based teaching: the need for a new approach to teaching clinical skills in the undergraduate medical education course. Med Teach. 2005;27:29–36.
Weston WW. Do we pay enough attention to science in medical education? Can Med Educ J. 2018;9(3):109–14.
Tokuda Y, Goto E, Otaki J, Jacobs J, Omata F, Obara H, et al. Undergraduate educational environment, perceived preparedness for postgraduate clinical training, and pass rate on the National Medical Licensure Examination in Japan. BMC Med Educ. 2010;10(1):35.
Prince KJ, Boshuizen HP, Van Der Vleuten CP, Scherpbier AJ. Students’ opinions about their preparation for clinical practice. Med Educ. 2005;39(7):704–12.
Chen CA, Kotliar D. Drolet, BC. (2015). Medical education in the United States: do residents feel prepared? Persp on Med Educ. 2015;4(4):181–5.
Windish DM, Paulman PM, Goroll AH, Bass EB. Do clerkship directors think medical students are prepared for the clerkship years? Acad Med. 2004;79(1):56–61.
Wenrich M, Jackson MB, Scherpbier AJ, Wolfhagen IH, Ramsey PG, Goldstein EA. Ready or not? Expectations of faculty and medical students for clinical skills preparation for clerkships. Med Educ Online. 2010;15(1):56–61.
Pascual TN, Chhem R, Wang SC, Vujnovic S. Undergraduate radiology education in the era of dynamism in medical curriculum: an educational perspective. Euro J of Rad. 2011;78(3):319–25.
Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Amer J of Clin Nutr. 2014;99(5):1153–66.
Fleiss JL. Levin B. MC. Statistical methods for rates and proportions. John Wiley & Sons: Paik; 2013.
Kwan CY. Learning of medical pharmacology via innovation: a personal experience at McMaster and in Asia. Acta Pharmacol Sin. 2004;25:1186–94.
Wiernik PH. A dangerous lack of pharmacology education in medical and nursing schools: a policy statement from the American College of Clinical Pharmacology. The J of Clin Pharmacol. 2015;55(9):953–4.
Aronson JK. A manifesto for clinical pharmacology from principles to practice. Br J of Clin Pharm. 2010;70:3–13.
Ross S, Loke YK. Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. British J of Clin Pharm. 2009;67:662–70.
Harding S, Britten N, Bristow D. The performance of junior doctors in applying clinical pharmacology knowledge and prescribing skills to standardized clinical cases. Br Jour of Clin Pharm. 2010;69:598–606.
Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2:253–9.
Ghosh S. Combination of didactic lectures and case-oriented problem-solving tutorials toward better learning: perceptions of students from a conventional medical curriculum. Adv in Phys Educ. 2007;31:193–7.
Harris DE, Hannum L, Gupta S. Contributing factors to student success in anatomy & physiology: lower outside workload and better preparation. Amer Bio Teach. 2004;66:168–75.
Costa ML, Van Rensburg L, Rushton N. Does teaching style matter? A randomised trial of group discussion versus lectures in orthopaedic undergraduate teaching. Med Educ. 2007;41:214–7.
Wai J, Lubinski D, Benbow CP, Steiger JH. 2010. Accomplishment in science, technology, engineering, and mathematics (STEM) and its relation to STEM educational dose: a 25-year longitudinal study. J of Educ Psych. 2010;102:860-871.
Maley MA, Harvey JR, Boer WBD, Scott NW, Arena GE. Addressing current problems in teaching pathology to medical students: blended learning. Med Teach. 2008;30(1):1–9.
Mattick K, Marshall R, Bligh J. Tissue pathology in undergraduate medical education: atrophy or evolution? J of Path. 2004;203:871–6.
Wood A, Struthers K, Whiten S, Jackson D, Herrington CS. Introducing gross pathology to undergraduate medical students in the dissecting room. Anat Sci Educ. 2010;3:97–100.
Mann CM, Wood A. How much do medical students know about infection control? J of Hospital Infection. 2006;64:366–70.
Chamberlain NR, Stuart MK, Singh VK, Sargentini NJ. Utilization of case presentations in medical microbiology to enhance relevance of basic science for medical students. Med Educ. 2012;17(1):15943.
de Vries TP. Presenting clinical pharmacology and therapeutics: a problem based approach for choosing and prescribing drugs. Br J of Clin Pharm. 1993;35:581–6.
Vollebregt JA, van Oldenrijk J, Kox D, van Galen SR, Sturm B, Metz JCM, et al. Evaluation of a pharmacotherapy context-learning programme for preclinical medical students. Brit J of Clin Pharm. 2006;62:666–72.
Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine: nutrition education for medical students and residents. Nutr in Clin Pract. 2010;25:471–80.
Devries S, Dalen JE, Eisenberg DM, Maizes V, Ornish D, Prasad A, et al. A deficiency of nutrition education in medical training. Amer J of Med. 2014;127(9):804–6.
Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in US medical schools: latest update of a national survey. Acad Med. 2010;85:1537–42.
Mogre V, Stevens FC, Aryee PA, Amalba A, Scherpbier AJ. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students’ perspectives on barriers and strategies. BMC Med Educ. 2018;18(1):26.
Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff. 2008;27:491–1502.
Weingart SN, Wilson RM, Gibberd RW, Harrison B. Epidemiology of medical error. West J of Med. 2000;172:390–3.
Dahle LO, Brynhildsen J, Fallsberg MB, Rundquist I, Hammar M. Pros and cons of vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum: examples and experiences from Linköping. Sweden Med Teach. 2002;24(3):280–5.
Grande JP. Training of physicians for the twenty-first century: role of the basic sciences. Med Teach. 2009;31:802–6.
Ito TA, Larsen JT, Smith NK, Cacioppo JT. Negative information weighs more heavily on the brain: the negativity bias in evaluative categorizations. J of Personal and Social Psych. 1998;75:887–900.
Acknowledgments
The authors would like to thank Ken Meadows (Western University) for carefully reviewing the interview questionnaires to ensure our questions were impartial and targeted and providing critical feedback, and the UME clerkship directors at the Schulich School of Medicine & Dentistry for taking part in the interviews for this research project and providing invaluable information regarding the basic science pre-clerkship curriculum.
Funding
This research was funded by the Government of Ontario (Ontario Graduate Scholarship), and the American Association of Anatomists (Education Research Scholarship).
Author information
Authors and Affiliations
Contributions
All authors made contributions to the study design, and/or data analysis, and/or data interpretation. Additionally, all authors were involved in drafting and/or editing this manuscript and provided final approval.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Norris, M.E., Cachia, M.A., Johnson, M.I. et al. Expectations and Perceptions of Students’ Basic Science Knowledge: Through the Lens of Clerkship Directors. Med.Sci.Educ. 30, 355–365 (2020). https://doi.org/10.1007/s40670-019-00913-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-019-00913-z