Abstract
The purpose of this study was to examine whether the National Scientific Council on the Developing Child (NSCDC) resilience framework statistically predicted whether a child with 4 or more adverse childhood experiences (ACEs) ever had a mental health issue. The study also explored which NSCDC modifiable resilience factors had the strongest relationship with mental health issues among children with 4 or more ACEs. Utilizing the 2019 National Survey of Children’s Health, secondary data analysis was conducted using a sample of 1,225 children between 6 and 17 years old that had experienced 4 or more ACEs. Logistic regression examined whether the NSCDC framework was associated with a lower likelihood of mental health issues in school-aged children. Analysis found that the NSCDC framework predicted whether children with 4 or more ACEs ever had a mental health issue. Self-regulation had the strongest relationship with whether a child with 4 or more ACEs ever had a mental health issue. A supportive parent/caregiver relationship was also associated with a lower likelihood of ever having a mental health issue. The results demonstrate the promise of the NSCDC framework and modifiable protective factors to mitigate the impact of ACEs on mental health outcomes. Interventions that teach children skill-based self-regulation and parent/caregiver co-regulation while providing safe and supportive environments can build self-regulation to overcome ACEs. Promoting resilience-building parent–child relationships also have the potential to build resilience to mitigate ACEs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 2016 National Survey of Children’s Health (NSCH) found 46.3% of all children experienced at least one adverse childhood experience (ACE) with 21.7% experiencing multiple ACEs (Bethell et al., 2017). Research has demonstrated that children that have experienced multiple ACEs are at increased risk for various risky health behaviors, mental health issues, behavioral issues, negative health outcomes, and poorer educational outcomes (Bellis et al., 2018; Burke et al., 2011; Choi et al., 2019; Dube et al., 2006; Jimenez et al., 2016; Porche et al., 2016; Song & Qian, 2020; Stempel et al., 2017). One study found that adolescents who experienced four or more ACEs were between 4 and 15 times more likely to have specific mental health issues like anxiety, behavior issues, depression, or substance use disorder (Bomysoad & Francis, 2020). Fortunately, resilience research has identified protective factors that can potentially help children adapt and succeed despite early childhood adversity (Ortiz, 2019). The National Scientific Council on the Developing Child (2015), an interdisciplinary council of researchers in the United States, has identified a framework in which four modifiable factors build resilience to overcome ACEs. These factors include mastery, strong self-regulation/executive functioning, a supportive cultural/faith background, and a stable relationship with at least one caring and supportive adult. While historical resilience research not specific to ACEs has validated these factors (Masten, 2018), no known studies have explored whether the NSCDC framework and factors reduce negative outcomes like mental health issues among children experiencing multiple ACEs. Thus, the present study explored whether the presence of these four NSCDC factors was associated with lower levels of mental health issues ever (depression, anxiety, ADHD, or conduct/behavior issues) among children experiencing four or more ACEs using secondary data from the 2019 NSCH, a national survey administered to households with children across the United States.
Adverse Childhood Experiences (ACEs)
Adverse childhood experiences are traumatic events in childhood that result in poorer educational, health, and quality of life outcomes. ACEs include psychological/emotional abuse, physical abuse, sexual abuse, physical neglect, emotional neglect, household mental illness, household substance abuse, incarceration of a household member, household domestic violence, and parental separation/divorce with some preliminary evidence of economic hardship, bullying, community violence, discrimination, and the death of a close family member potentially being ACEs (Felitti et al., 1998; Finkelhor et al., 2013; Wade et al., 2014). In the seminal ACEs study, Felitti et al. (1998) identified a significant dose-wise relationship between the number of categories of ACEs experienced and risky health behaviors, poor health outcomes, and chronic disease among adults. Since the original ACEs study, multiple studies have found a similar graded relationship with other health outcomes while also further establishing the relationship with poorer mental health outcomes (Hughes et al., 2017; Petruccelli et al., 2019). ACEs have also been associated with a much lower life expectancy, lower income, and increased risk of living in poverty (Brown et al., 2009; Schurer et al., 2019).
ACEs & Childhood Outcomes
Among children, exposure to multiple ACEs has been associated with poorer health outcomes including asthma, headaches, digestive issues, allergies, being overweight/obese, alcohol use, risky sexual behavior, mental health issues, and worse quality of life (Bellis et al., 2018; Burke et al., 2011; Dube et al., 2006; Porche et al., 2016; Song & Qian, 2020). Experiencing multiple ACEs has also been linked to higher rates of absenteeism, learning problems, behavioral issues, and failing a grade along with poorer early literacy skills, school engagement, and academic outcomes (Bellis et al., 2018; Burke et al., 2011; Choi et al., 2019; Jimenez et al., 2016; Porche et al., 2016; Stempel et al., 2017).
ACEs impact short and long-term health and quality of life outcomes by influencing cognitive, social, and emotional impairment which results in risky health behaviors resulting in poorer quality of life, disability, and disease (Felitti et al., 1998). Consequently, a longitudinal study that followed children between 9 to 13 years old to 25 years old found that children with mental health issues were significantly more likely to have negative health and social outcomes in early adulthood (Copeland et al., 2015). Thus, when considering outcomes in childhood, mental health issues may potentially be one of the earlier health outcomes impacted by ACEs. Based upon analysis of the 2016–2017 NCHS, Bomysoad and Francis (2020) found a graded relationship between exposure to one or more ACEs and mental health issues in adolescents. Compared to adolescents with no ACEs, adolescents with four or more ACEs were 4 times more likely to have ADHD, over 5 times more likely to have anxiety, over 7 times more likely to have behavioral issues, 10 times more likely to have depression, and over 15 times more likely to have a substance use disorder. Elmore and Crouch (2020) found that children between 8 and 17 years old with four or more ACEs were 1.7 times more likely to have anxiety and 2.2 times likely to have depression than those not experiencing ACEs. Thus, children experiencing four or more ACEs are at significantly higher risk for mental health issues which likely influence other outcomes. With approximately 46.3% of all children experiencing at least one ACE and 21.7% experiencing two or more ACEs (Bethell et al., 2017), ACEs are a substantial public health issue impacting children’s mental health that poses a threat to their long-term health, educational, and quality of life outcomes. Since ACEs initially impede emotional, social, and cognitive impairment before other outcomes (Felitti et al., 1998) and there is well-documented evidence of poor mental health outcomes among youth experiencing four or more ACEs (Bomysoad & Francis, 2020; Elmore & Crouch, 2020), this study will explore mental health outcomes among school-aged children.
Resilience
While the goal would be to prevent ACEs, resilience research has sought to mitigate the impact of ACEs in children and adults. Resilience is the quality of being able to adapt and succeed despite experiencing adversity (Ortiz, 2019). Historic resilience research not specific to ACEs was grounded in systems theory, attachment theory, and other psychological theories and sought to understand how individuals overcome any type of adversity. Research has expanded to identifying protective factors that have allowed those who have experienced adversity to succeed (Masten, 2018). Protective factors have included predispositions like optimism and temperament, but they also included modifiable protective factors (Hornor, 2017). Thus, one promising approach to address ACEs is to identify modifiable protective factors that mitigate ACEs.
One resilience framework that has been developed to address ACEs is the toxic stress and resilience framework proposed by the National Scientific Council on the Developing Child (2015). In this framework, exposure to ACEs results in negative outcomes through toxic stress. Toxic stress occurs due to intense or ongoing exposure to high levels of stress during childhood that results in physiological changes that impact development, influencing future outcomes. This framework has identified four modifiable factors that build resilience to mitigate ACEs: mastery in some area, strong self-regulation/executive functioning, a supportive cultural/faith background, and a stable relationship with at least one caring and supportive adult. A supportive, stable, caring relationship with at least one adult was identified as the most important of these factors. While no empirical studies were discussed that demonstrated the efficacy of this model in mitigating ACEs, these factors align with factors identified more broadly in resilience research that help individuals overcome adversity (Masten, 2018). Furthermore, factors identified in this framework were similar to those identified by other scholars (Hornor, 2017; Sciaraffa et al., 2017; Soleimanpour et al., 2017). However, before widely implementing interventions to promote these factors, evidence is needed that these factors mitigate ACEs among children.
Other research has sought to identify potential protective factors against ACEs. Bethell et al. (2019) found a dose-wise relationship between positive childhood experiences (PCEs) that included family, community, friend, and school support along with communication factors that could potentially be a protective factor against ACEs. Clements-Nolle and Waddington (2019) found that positive family communication, school connectedness, positive peer role models, and internal resilience moderated the impact of four to five ACEs on psychological distress among female teenagers involved with the juvenile justice system. Bellis et al. (2018) explored the impact of seven resilience factors on multiple childhood health outcomes. The results were mixed with certain resiliency factors being a significant predictor of certain outcomes with no consistent predictors across all outcomes.
While these studies did explore how protective factors could potentially mitigate the impact of ACEs, the factors chosen were not based upon a specific resiliency framework or model. Furthermore, these studies did not provide conclusive evidence of the factors that are most important to mitigate ACEs to inform future interventions. As cited by several researchers, understanding protective factors to mitigate the well-established relationship between ACEs and negative outcomes among children is an important gap that must be better understood (Bomysoad & Francis, 2020; Heard-Garris et al., 2018; Robles et al., 2019). Furthermore, most research on resilience has focused on identifying protective factors for adults (Clements-Nolle & Waddington, 2019). Thus, there remains a substantial gap in the literature regarding a validated resilience framework that can be implemented to build resilience to mitigate the impact of ACEs on childhood outcomes.
Current Study
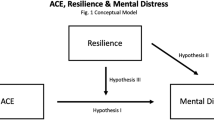
Based upon the previously identified gaps in the literature, this study utilized the 2019 NSCH to examine whether the National Scientific Council on the Developing Child (2015) framework predicts whether school-aged children that experienced four or more ACEs ever had a mental health issue. The study also explored which of the four National Scientific Council on the Developing Child (2015) factors had the strongest relationship with whether school-aged children ever had a mental health issue among the same population. Consistent with the NSCDC framework, this study tested the following hypotheses:
-
1.
Among children that experienced four or more ACEs, the presence of a supportive adult relationship, strong self-regulation, a hopeful family tradition, and/or mastery along with certain demographic characteristics will be associated with a lower likelihood of children ever having had a mental health issue.
-
2.
Of the resilience characteristics, a supportive adult relationship will contribute the most to predicting whether a child with four or more ACEs ever was told they had a mental health issue by a healthcare provider.
Method
Population and Procedures
This cross-sectional study used secondary data from the 2019 National Survey of Children’s Health (NSCH). De-identified data was provided by the U.S. Census Bureau (Maternal and Child Health Bureau, 2019). The NSCH is a national survey administered by the Health Resources and Services Administration’s Maternal and Child Health Bureau to gather information on health, mental health, and overall wellbeing of children between the ages of 0 and 17 years old as reported by parents. In 2019, 184,000 households were sampled with a screener questionnaire to determine eligibility. Of the 68,500 screener questionnaires completed, 35,760 households were eligible. Of those 35,760 households, 29,433 households completed the topical interview used for this study providing data on one child in the home. Households completed different survey versions based upon the child’s age (United States Census Bureau, 2020). Thus, only households with children between 6 and 17 years old completed surveys with all the variables of interest. Therefore, the sample was limited to children between 6 and 17 years old.
Based upon the research questions, the sample only included children that had experienced four or more ACEs. This criterion was chosen because four or more ACEs was the most common threshold for more negative outcomes (Bomysoad & Francis, 2020; Elmore & Crouch, 2020) and other NSCH ACEs studies used this threshold (Crouch et al., 2019a, b; Elmore & Crouch, 2020). The 2019 NCHS included nine ACEs items that asked about whether the child had experienced racism, parental/guardian divorce, parental/guardian death, parental/guardian incarceration, domestic violence in the home, a victim of violence, household mental illness, household drug/alcohol problem, and economic hardship. All variables were dichotomous (yes/no) except for economic hardship, which was categorical (never, rarely, somewhat often, or very often). Consistent with other ACEs studies using the NCHS (Balistreri & Alvira-Hammond, 2016; Crouch et al., 2019a, b; Elmore & Crouch, 2020), economic hardship was dichotomized to yes (“somewhat often” and “very often”) and no (“never” or “rarely”). The total ACEs score was tabulated by adding the number of ACEs experienced in which the child had a “yes” response. This excluded children that had missing ACEs items.
Of the 21,259 households with children between 6 and 17 years old completing the survey, 19,964 (93.4%) completed all nine ACEs items. Of those 19,964 responses, 1,279 (6.4%) experienced four or more ACEs. After excluding children missing data on other variables in the study, the final sample was 1,225 children between the ages of 6 and 17 with no missing data that had experienced four or more ACEs. The sample had an average age of 12.7 years old (SD = 3.36) with 51.3% male and 48.7% female. Approximately 78.6% of the sample was Caucasian, 7.5% black/African American, and 18.9% other. Table 1 includes other sample demographics.
Measures
Demographics
The demographic variables used as predictors in this study were race, sex, gender, age, and socioeconomic status. Race was categorized as “Caucasian”, “black/African American”, and “other”. Gender was categorized as “male” or “female”. Age was a continuous variable between 6 and 17 based upon the child’s age at the time of the survey. Socioeconomic status was defined as the family’s household income as the ratio of the family federal poverty ratio. Consistent with other studies (Stempel et al., 2017), these ratios were recategorized as 0% to 199%, 200%-399%, and 400% or higher.
Resilience Measures
Five predictor variables were used to capture the four constructs from the NSCDC toxic stress and resilience framework (National Scientific Council on the Developing Child, 2015). Consistent with other NSCH studies exploring resilience factors (Foster & Weinstein, 2019; Heard-Garris et al., 2018), ordinal responses for these items were recoded to dichotomous variables to describe whether the child had that characteristic. The first factor, a positive, stable, relationship with at least one caring adult, was based upon two items. First, the parent/caregiver relationship was assessed by the question “How well can you and the child share or talk about things that really matter?” with the responses “very well” and “somewhat well” recoded as “yes” and “not very well” and “not well at all” recoded as “no”. A relationship with another caring adult was based upon the response to the question “other than you or other adults in your home, is there at least one other adult in the child’s school, neighborhood, or community who knows this child well and who he or she can rely on for advice or guidance” with the responses “yes” or “no”. Strong self-regulation was based upon the response to the following item: “How often does this child stay calm and in control when faced with a challenge?”. The responses “always” and “usually” were recoded as “yes” with “sometimes” and “never” coded as “no”. Hopeful family tradition was based upon the response to the item: “When your family faces problems, how often are you likely to stay hopeful even in difficult times?”. The responses “all of the time” and “most of the time” were coded as “yes” while “some of the time” and “none of the time” were coded as “no”. Mastery or control over one area of one’s life was defined based upon whether the child had engaged in at least one extracurricular activity in the form of sports, outside of school clubs/organizations, outside of school organized activities/lessons, or work. If the parents answered “yes” to at least one of those four items, they were coded as having participated in some extracurricular activity.
Mental Health Issues
Child mental health issues were defined by whether the parent or caregiver was ever told by a healthcare provider that their child had depression, anxiety, behavioral issues, or ADHD. Four items that asked “yes” or “no” to whether the parent has been told that their child has one of these mental health issues. If they answered “yes” to any of the items, they were coded as “yes”. If they answer “no” to all four items, they are coded as not ever having a mental health issue. These items have been used in previous studies to explore the relationship between mental health issues and ACEs on the NSCH (Bomysoad & Francis, 2020; Uddin et al., 2020).
Data Analyses
All statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 27.0. First, descriptive statistical analysis was completed for all predictor and outcome variables. Then, logistic regression was completed with validation. The entire sample was analyzed to develop the initial model. The logistic regression model was rerun with a training sample that consisted of 75% of the original sample to determine if the model has the same level of validity. Then, the analysis was completed again with a 25% validation sample to assess the validity in predicting the outcome variable. To determine regression model effectiveness, the model was compared to the improvement of guessing whether a child had a mental issue by chance. By chance, guessing accurately predicted whether a child has at least one mental health issue 51.2% of the time. To have a significant improvement of at least 25%, the model must have accurately predicted whether the child has at least one mental health issue at least 64.0% of the time.
The data set met all assumptions of logistic regression. The dependent variable (mental health issue ever) was dichotomous while each observation was independent. The assumption of no multicollinearity was met since the VIF values for all predictor variables were less than 5.0. There was also a sufficiently large sample size of over 1,000 cases.
Results
Descriptive Results
A total of 1,225 children between the ages of 6 and 17 had experienced at least four ACEs and completed all the variables of interest. Table 1 compares demographic and resilience factors based upon whether they ever had a mental health issue. A total of 708 (57.8%) of children were ever told by a healthcare provider that they had depression, anxiety, behavioral issues, or ADHD. Overall, 89.3% of children had a supportive parent/guardian relationship, 90.6% had another adult from which to seek advice or help, 53.0% had strong self-regulation, 87.4% had a hopeful family tradition, and 80.0% participated in at least one out of school activity. Children that ever had a mental health issue had lower levels of parent/guardian support, other adult support, self-regulation, hopeful family traditions, and extracurricular activity involvement than children that never had a mental health issue. Children that were male (53.8%), Caucasian (77.1%), and in a household less than 200% of the federal poverty limit (54.0%) had the highest percentages of ever having a mental health issue.
Logistic Regression Results
Mental Health Issues
Based upon the logistic regression run on the full sample, the model including all resilience and demographic variables explained a significant amount of variance in whether children had ever had at least one mental health issue (χ2 (11) = 275.82, p < 0.001). Approximately 27.1% of the variance in children with multiple ACEs ever having at least one mental health issue was explained by the predictor variables (Nagelkerke R2 = 0.271). The training sample of 941 was also significant (χ2 (11) = 205.33, p < 0.001) and predicted 26.8% of the variance (Nagelkerke R2 = 0.268) in children ever having a mental health issue.
The model significantly improved on the prediction of whether a child with 4 or more ACEs had at least one mental health issue over chance. As seen in Table 2, the model correctly classified cases approximately 71.3% of the time, exceeding the 64% threshold of at least a 25% improvement over guessing. The model correctly classified 67.4% of those with at least one mental health issue and correctly classified 76.6% of cases without a mental health issue. The training sample and validation sample also demonstrated similar improvements with the training sample correctly classifying 71.2% of children and the validation sample correctly classifying 71.4% of children. Thus, the model with resilience and demographic variables significantly improved the prediction of mental health issues in this sample.
Resilience Factors
Logistic regression results with coefficients are presented in Table 3. After controlling for the other variables, a supportive parent/guardian relationship, strong self-regulation, race, and age were significantly associated with whether a child with multiple ACEs ever had a mental health issue. Strong self-regulation had the strongest association based upon an odds ratio of 0.149. Thus, the odds of a child with four or more ACEs not ever having had a mental health issue in childhood increased by a factor of 6.71 (1.00/0.149) for children with strong self-regulation compared to children without strong self-regulation. The odds of not ever having a mental health issue increased by a factor of 1.77 (1/0.565) for those children that had a supportive parent/caregiver relationship compared to children compared to those without a supportive parent/caregiver relationship. Compared to Caucasian children, the odds of African American children not ever having had a mental health issue increased by a factor of 2.07 (1.00/0.483), and other race increased by a factor of 1.39 (1.00/0.715). In the sample of children between 6 and 17 years old, older children had greater odds of ever having had at least one mental health issue than younger children. For every year of additional age, the odds of having at least one mental health issue increased 5.7%.
In the randomly selected training sample of 75% of the cases, a supportive parent/caregiver relationship and strong self-regulation still significantly contributed to the regression model along with other race compared to Caucasian. Female compared to male was also significant, but African American compared to Caucasian and age no longer significantly contributed to the regression model. While the statistical significance of these variables differed in the training sample, the direction of all the variables was consistent with the full sample, and the overall model was still significant.
Thus, while there was some variability regarding which demographic predictors significantly contributed to the regression model, a supportive relationship with a parent/caregiver and strong self-regulation significantly contributed to the model and decreased the odds that a child would ever have had a mental health issue in both samples. Hopeful family traditions, other adult relationships, and activities outside of school did not significantly contribute to the model after controlling for other variables. Race, gender, and age potentially significantly contributed to the model in a least one sample, but results were inconsistent across the full sample and training sample. However, there was evidence that two of the resilience factors were associated with a lower likelihood of children ever having a mental health issue.
Discussion
This study explored whether the presence of four modifiable protective factors identified by the National Scientific Council on the Developing Child (2015) along with certain demographic factors were associated with lower levels of mental health issues ever (depression, anxiety, behavioral issues, or ADHD) in children between 6 and 17 years old with four or more ACEs. Utilizing the 2019 NSCH, a supportive parent/caregiver relationship, supportive other adult relationship, strong self-regulation, a hopeful family tradition, mastery/engagement in extracurricular activities, age, sex, race, and socioeconomic status accounted for 27.1% of the variance in whether a child with four or more ACEs ever had at least one mental health issue. The regression model also significantly improved the ability to predict whether a child ever had a mental health issue over chance. The study also explored which predictor variables had the strongest relationship with mental health issues in the study population, hypothesizing that supportive adult relationships would have the strongest relationship. Self-regulation had the strongest association with not ever having a negative mental health outcome with a strong parent/guardian relationship being the only other significant resilience variable. Race and age also significantly contributed to the model.
NSCDC Framework
The effectiveness of the regression model that included modifiable resilience factors in predicting whether children with four or more ACEs ever had a mental health issue was consistent with the National Scientific Council on the Developing Child (2015) framework and supported the study’s first hypothesis. This builds upon previous resilience theories and research that has established the importance of adult relationships, self-regulation/executive functioning, mastery, and an affirming and hopeful cultural or faith tradition (Masten, 2018). While not specific to the National Scientific Council on the Developing Child (2015) framework, other researchers have found that protective factors can mitigate the impact of ACEs on mental health issues. Among adults, Bethell et al. (2019) found that having six to seven protective factors decreased the odds of poor mental health or depression by 72% compared to adults with two or fewer protective factors. Another study found adults with four or more ACEs with caregiver protective factors in childhood were significantly less likely to have mental health issues in adulthood (Crouch et al., 2019a, b). Clements-Nolle and Waddington (2019) found that certain protective factors were associated with lower levels of psychological distress among female youth involved in the juvenile justice system. Thus, this study builds upon those studies by demonstrating the ability of protective factors to predict whether a child experiencing four or more ACEs will ever have had a mental illness in childhood using a comprehensive resilience framework and nationwide data set of school-aged children.
Modifiable Resilience Factors
Self-regulation and Parent/Guardian Relationships
The study also explored which modifiable resilience factors had the strongest association with children experiencing four or more ACEs not ever having a mental health issue. Of the resilience factors explored in this study, strong self-regulation contributed the most to the prediction of whether a child with four or more ACEs ever had a mental health issue. A supportive parent/caregiver relationship was the second strongest resilience factor. While both factors decreased the likelihood of a child ever having a mental health issue, the National Scientific Council on the Developing Child (2015) framework indicated that a supportive, stable relationship with at least one caring adult was the most important factor in mitigating ACEs with other studies finding similar outcomes (Robles et al., 2019). Thus, the second hypothesis that a supportive adult relationship was the strongest predictor in the regression model was not supported by this study.
Foster and Weinstein (2019) found a similar outcome in which emotional resilience, which included self-regulation, had the strongest relationship with mitigating the impact of ACEs on obesity. Based upon a significant odds ratio of 0.565 after controlling for the other variables in the study, a supportive parent/caregiver relationship was the second strongest resilience factor in this study. Parental and caregiver relationships have been identified as a protective factor in other studies that mitigates the negative impact of ACEs on children (Crouch et al., 2019a, b; Robles et al., 2019; Uddin et al., 2020). Several factors may have contributed to this discrepancy. First, Woodward et al. (2017) found that children with lower levels of self-regulation were more likely to have mental health issues such as ADHD, anxiety, or behavioral issues. Due to the relationship between self-regulation and these mental health issues, self-regulation may be a stronger protective factor against this particular outcome. Thus, certain protective factors may have a stronger relationship with certain outcomes. Second, while the NSCH self-regulation item was similar to self-regulation described in the National Scientific Council on the Developing Child (2015) framework, other researchers have used the item as a measure of child resilience (Heard-Garris et al., 2018). Thus, this item could potentially be a mediator between other protective factors and mental health issues. Alternatively, the parent/caregiver relationship item only addressed one aspect of parental/caregiver relationships, communication. Items that fully encompassed all aspects of a strong, supportive, caring relationship with one adult based upon the National Scientific Council on the Developing Child (2015) framework may have had a stronger relationship with mental health outcomes.
Other Adult Relationships, Mastery, and Hopeful Family Tradition
In this study, other adult support, involvement in other activities (mastery), and a hopeful family tradition did not significantly contribute to the prediction of mental health issues after controlling for the other variables. The findings are inconsistent with other studies that found mastery or self-efficacy mitigated the negative impact of trauma or ACEs (Cohrdes & Mauz, 2020; Infurna et al., 2015). Hope has also been identified as a protective factor that builds resilience to overcome trauma in other studies (Lenz, 2021; Munoz et al., 2020). The findings were also inconsistent with the National Scientific Council on the Developing Child (2015) framework. Several factors could account for these differences. First, parent/caregiver and other adult relationships are not separated in the National Scientific Council on the Developing Child (2015) framework. Thus, in this sample where 89.3% of children had a supportive parent/caregiver relationship, the addition of other adult support may not have added any unique contribution to the variance or this construct. Second, resilience factors were limited to items on the NSCH. While self-regulation and parent relationship questions more closely aligned with the National Scientific Council on the Developing Child (2015) framework, participation in activities outside of school was a proxy measure for mastery. Participation does not ensure the children had mastery in those areas. Similarly, the National Scientific Council on the Developing Child (2015) considers the fourth factor to be an “affirming faith or cultural tradition” that “responds effectively when challenged”. This includes hope, but the construct goes beyond just hope. In addition, the NSCH item only discussed whether the family stayed hopeful from the caregiver’s perspective. The item was not specific to the child and did not include all aspects of this construct. Thus, the items on the NSCH likely did not include all aspects of the constructs within the NSCDC framework. An instrument that is more closely aligned with the National Scientific Council on the Developing Child (2015) framework could better validate these protective factors.
Limitations & Future Research
The primary limitation of this study was that it was a cross-sectional design that utilized data from the 2019 NSCH based upon parent/caregiver reports. The cross-sectional nature of the study limits the ability to infer temporal or causal relationships between resilience factors and mental health issues. Also, since the items were based upon parental response, the resilience factors did not capture the child’s perception of each of these factors. From a resilience framework, the child’s perspective is more important in determining whether they possess that protective factor. Similarly, when determining the ACEs score, parents or guardians may underreport adverse events that may reflect poorly upon them or may be unaware of some of their child’s experiences. Also, not all the ACEs included in the original ACEs study were included on NSCH. The study excluded ACEs like sexual abuse, physical abuse, and neglect (Felitti et al., 1998). Thus, the number of ACEs was likely underreported for children, meaning some children with four or more ACEs may have been excluded from this study.
Another limitation of this study was that the resilience items on the NSCH did not exactly match the factors in the National Scientific Council on the Developing Child (2015) framework. A supportive adult relationship was composed of two items that were based primarily on communication and support without recognizing other aspects of supportive, stable adult relationships (Centers for Disease Control & Prevention, 2013). While self-regulation appears to align with the National Scientific Council on the Developing Child (2015) framework, executive functioning was not captured by the survey. Proxy measures were also used for the constructs of mastery and a supportive and affirming faith and cultural tradition. While these contained elements of these construct, a survey with items developed using the National Scientific Council on the Developing Child (2015) framework would be needed to validate the model more accurately. Thus, subsequent studies are needed to develop and utilize an instrument that fully captures National Scientific Council on the Developing Child (2015) constructs to further validate this framework.
While this study demonstrated that modifiable resilience factors within the National Scientific Council on the Developing Child (2015) framework predicted whether children with four or more ACES ever had a mental health issue, future research is needed to explore and further validate the framework’s effectiveness with other child and adult outcomes. One important step in further validating the National Scientific Council on the Developing Child (2015) framework is to develop an instrument to measure the four modifiable protective factors as described by the framework. Longitudinal studies are also needed to establish causality, understand pathways of resilience, and determine the relationship between the modifiable protective factors within this model. Finally, the National Scientific Council on the Developing Child (2015) framework is only one approach to understanding how modifiable protective factors mitigate ACEs. The “Health Outcomes from Positive Experiences” framework, positive childhood experiences (PCEs), advantageous childhood experiences, and benevolent childhood experiences (BCEs) are other resilience approaches that seek to understand and explain the relationship between protective factors and ACEs (Bethell et al., 2019; Crandall et al., 2020; Narayan et al., 2018; Sege & Harper Browne, 2017). While some of these approaches have demonstrated some preliminary evidence of a dose-wise relationship between PCEs and more favorable outcomes for those experiencing ACEs (Bethell et al., 2019; Elmore et al., 2020), research is needed to understand if a framework like the National Scientific Council on the Developing Child (2015) framework that emphasizes key factors or a dose-wise relationship better predicts resilience. Thus, future research should explore these and other potential frameworks to identify modifiable protective factors, understand which factors have the strongest relationship, and understand how they relate to inform evidence-based interventions to build resilience to overcome ACEs and other childhood trauma. Furthermore, policymakers should seek to include more robust measures of resilience along with ACEs in national and population-level surveys to further advance resilience research (Centers for Disease Control & Prevention, 2020).
Implications
The identification of modifiable protective factors that potentially mitigate ACEs has strong implications to guide future interventions to improve mental health outcomes among children experiencing multiple ACEs. In this study, self-regulation was the strongest predictor of whether a child ever had a mental health issue. Fortunately, interventions have been effective at increasing self-regulation throughout childhood into early adulthood (Murray et al., 2016). Effective self-regulation interventions should promote “co-regulation” between caregivers and children, instruct children on self-regulation skills, and create predictable and supportive environments. Interventions should also be developmentally appropriate and target multiple ecological levels such as child skill acquisition, parent/caregiver training, educator training, and safe and supportive school environments (Murray et al., 2019). Interventions can target “co-regulation” by teaching parents, teachers, and other caregivers self-regulation to model behaviors, develop supportive relationships, and teach techniques for adults to recognize and be responsive to children’s emotions and needs (Murray et al., 2016, 2019). Self-regulation skills can be targeted through developmentally appropriate interventions that teach children specific skills with increasing complexity across childhood (Murray et al., 2019). While parents can begin early on teaching self-regulation, social-emotional learning is one school-based approach that can be implemented school-wide to develop self-regulation in children (Murray et al., 2016; Zins & Elias, 2007). To create safe and supportive environments, parents, schools, and other caregivers should seek to provide safety, stability, predictability, and regular routines and schedules (Murray et al., 2019; Sciaraffa et al., 2017). Schools can even utilize universal approaches such as trauma-informed schools that create safe environments for students who have experienced trauma by increasing school-wide trauma awareness while preventing re-traumatization (Thomas et al., 2019).
Supportive parent and guardian relationships had the second strongest relationship with whether children experiencing multiple ACEs ever had a mental health issue. Thus, parent education and training interventions should be used to promote positive relationships with children. The Centers for Disease Control and Prevention (2013) has identified several evidence-based parenting education programs that teach parents how to communicate, interact, and play with children in safe, nurturing, and emotionally responsive ways to build supportive relationships. These evidence-based programs often utilized innovative approaches to reach children at higher risk while also delivering developmentally appropriate techniques to connect with children throughout childhood (Centers for Disease Control & Prevention, 2013). In the absence of supportive parent and guardian relationships, interventions should be used that promote other supportive adult relationships such as teacher-student relationships, mentoring relationships, or relationships with other trusted adults such as coaches, counselors, tutors, or naturally occurring mentors (Black et al., 2010; Centers for Disease Control & Prevention, 2013; National Scientific Council on the Developing Child, 2015; Sciaraffa et al., 2017). Thus, this study demonstrates the need for developmentally appropriate interventions that increase self-regulation and supportive adult relationships for children throughout childhood to mitigate ACEs.
Conclusions
Previous research has well documented the negative impact of ACEs on academic, health, and quality of life outcomes. While preventing ACEs would be ideal, a significant proportion of children have experienced ACEs. This study contributed to the literature by demonstrating how modifiable protective factors identified in the toxic stress and resilience framework were associated with lower levels of mental health issues among children with 4 or more ACEs. This current study was the first known study to explore whether the resilience factors identified by the National Scientific Council on the Developing Child (2015) framework were associated with fewer negative mental health outcomes among children experiencing four or more ACEs. Furthermore, the study demonstrated that strong self-regulation and supportive parent/caregiver relationships were associated with a lower likelihood of mental health issues among this population. While future research is needed to further validate the National Scientific Council on the Developing Child (2015) framework, the study outcomes demonstrate the promise for interventions that promote self-regulation and supportive parent/caregiver relationships to build resilience for children to overcome the negative impact of ACEs.
References
Balistreri, K. S., & Alvira-Hammond, M. (2016). Adverse childhood experiences, family functioning and adolescent health and emotional well-being. Public health, 132, 72–78. https://doi.org/10.1016/j.puhe.2015.10.034
Bellis, M. A., Hughes, K., Ford, K., Hardcastle, K. A., Sharp, C. A., Wood, S., & Davies, A. (2018). Adverse childhood experiences and sources of childhood resilience: A retrospective study of their combined relationships with child health and educational attendance. BMC Public health, 18(1), 792. https://doi.org/10.1186/s12889-018-5699-8
Bethell, C., Davis, M. B., Gombojav, N., Stumbo, S., & Powers, K. (2017). A national and across-state profile on adverse childhood experiences among U.S. Children and possibilities to heal and thrive. Retrieved from http://www.cahmi.org/wp-content/uploads/2018/05/aces_brief_final.pdf
Bethell, C., Jones, J., Gombojav, N., Linkenbach, J., & Sege, R. (2019). Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA Pediatr, e193007. https://doi.org/10.1001/jamapediatrics.2019.3007
Black, D. S., Grenard, J. L., Sussman, S., & Rohrbach, L. A. (2010). The influence of school-based natural mentoring relationships on school attachment and subsequent adolescent risk behaviors. Health education research, 25(5), 892–902. https://doi.org/10.1093/her/cyq040
Bomysoad, R. N., & Francis, L. A. (2020). Adverse childhood experiences and mental health conditions among adolescents. Journal of adolescent health, 67(6), 868–870. https://doi.org/10.1016/j.jadohealth.2020.04.013
Brown, D. W., Anda, R. F., Tiemeier, H., Felitti, V. J., Edwards, V. J., Croft, J. B., & Giles, W. H. (2009). Adverse childhood experiences and the risk of premature mortality. American journal of preventive medicine, 37(5), 389–396. https://doi.org/10.1016/j.amepre.2009.06.021
Burke, N. J., Hellman, J. L., Scott, B. G., Weems, C. F., & Carrion, V. G. (2011). The impact of adverse childhood experiences on an urban pediatric population. Child abuse and neglect, 35(6), 408–413. https://doi.org/10.1016/j.chiabu.2011.02.006
Centers for Disease Control and Prevention. (2013). Essentials for childhood: Creating safe, stable, nurturing relationships and environment for all children. Retrieved from https://www.cdc.gov/violenceprevention/pdf/essentials-for-childhood-framework508.pdf
Centers for Disease Control and Prevention. (2020). Adverse childhood experiences prevention strategy. Retrieved from https://stacks.cdc.gov/view/cdc/108183/cdc_108183_DS1.pdf
Choi, J. K., Wang, D., & Jackson, A. P. (2019). Adverse experiences in early childhood and their longitudinal impact on later behavioral problems of children living in poverty. Child abuse and neglect, 98, 104181. https://doi.org/10.1016/j.chiabu.2019.104181
Clements-Nolle, K., & Waddington, R. (2019). Adverse childhood experiences and psychological distress in juvenile offenders: The protective influence of resilience and youth assets. Journal of adolescent health, 64(1), 49–55. https://doi.org/10.1016/j.jadohealth.2018.09.025
Cohrdes, C., & Mauz, E. (2020). Self-efficacy and emotional stability buffer negative effects of adverse childhood experiences on young adult health-related quality of life. Journal of adolescent health, 67(1), 93–100. https://doi.org/10.1016/j.jadohealth.2020.01.005
Copeland, W. E., Wolke, D., Shanahan, L., & Costello, E. J. (2015). Adult functional outcomes of common childhood psychiatric problems: A prospective, longitudinal study. JAMA Psychiatry, 72(9), 892–899. https://doi.org/10.1001/jamapsychiatry.2015.0730
Crandall, A., Broadbent, E., Stanfill, M., Magnusson, B. M., Novilla, M. L. B., Hanson, C. L., & Barnes, M. D. (2020). The influence of adverse and advantageous childhood experiences during adolescence on young adult health. Child abuse and neglect, 108, 104644. https://doi.org/10.1016/j.chiabu.2020.104644
Crouch, E., Radcliff, E., Hung, P., & Bennett, K. (2019a). Challenges to school success and the role of adverse childhood experiences. Academic pediatric, 19(8), 899–907. https://doi.org/10.1016/j.acap.2019.08.006
Crouch, E., Radcliff, E., Strompolis, M., & Srivastav, A. (2019b). Safe, stable, and nurtured: Protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs). Journal of child & adolescent trauma, 12(2), 165–173. https://doi.org/10.1007/s40653-018-0217-9
Dube, S. R., Miller, J. W., Brown, D. W., Giles, W. H., Felitti, V. J., Dong, M., & Anda, R. F. (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of adolescent health, 38(4), 444.e441-444.e410. https://doi.org/10.1016/j.jadohealth.2005.06.006
Elmore, A. L., & Crouch, E. (2020). The association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Academic pediatric, 20(5), 600–608. https://doi.org/10.1016/j.acap.2020.02.012
Elmore, A. L., Crouch, E., & Kabir Chowdhury, M. A. (2020). The interaction of adverse childhood experiences and resiliency on the outcome of depression among children and youth, 8–17 year olds. Child abuse and neglect, 107, 104616. https://doi.org/10.1016/j.chiabu.2020.104616
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American journal of preventive medicine, 14(4), 245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Finkelhor, D., Shattuck, A., Turner, H., & Hamby, S. (2013). Improving the adverse childhood experiences study scale. JAMA Pediatrics, 167(1), 70–75. https://doi.org/10.1001/jamapediatrics.2013.420
Foster, B. A., & Weinstein, K. (2019). Moderating effects of components of resilience on obesity across income strata in the national survey of children’s health. Academic pediatric, 19(1), 58–66. https://doi.org/10.1016/j.acap.2018.08.012
Heard-Garris, N., Davis, M. M., Szilagyi, M., & Kan, K. (2018). Childhood adversity and parent perceptions of child resilience. BMC Pediatrics, 18(1), 204. https://doi.org/10.1186/s12887-018-1170-3
Hornor, G. (2017). Resilience. Journal of pediatric health care, 31(3), 384–390. https://doi.org/10.1016/j.pedhc.2016.09.005
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The lancet public health, 2(8), e356–e366. https://doi.org/10.1016/s2468-2667(17)30118-4
Infurna, F. J., Rivers, C. T., Reich, J., & Zautra, A. J. (2015). Childhood trauma and personal mastery: Their influence on emotional reactivity to everyday events in a community sample of middle-aged adults. PLoS ONE, 10(4), e0121840. https://doi.org/10.1371/journal.pone.0121840
Jimenez, M. E., Wade, R., Jr., Lin, Y., Morrow, L. M., & Reichman, N. E. (2016). Adverse experiences in early childhood and kindergarten outcomes. Pediatrics, 137(2), e20151839. https://doi.org/10.1542/peds.2015-1839
Lenz, A. S. (2021). Evidence for relationships between hope, resilience, and mental health among youth. Journal of counseling & development, 99(1), 96–103. https://doi.org/10.1002/jcad.12357
Masten, A. S. (2018). Resilience theory and research on children and families: Past, present, and promise. Journal of Family Theory & Review, 10(1), 12–31. https://doi.org/10.1111/jftr.12255
Maternal and Child Health Bureau. (2019). National Survey of Children's Health (NSCH). Retrieved from: https://www.census.gov/data/datasets/2019/demo/nsch/nsch2019.html
Munoz, R. T., Hanks, H., & Hellman, C. M. (2020). Hope and resilience as distinct contributors to psychological flourishing among childhood trauma survivors. Traumatology, 26(2), 177. https://doi.org/10.1037/trm0000224
Murray, D. W., Rosanbalm, K., & Christopoulos, C. (2016). Self-regulation and toxic stress report 3: A comprehensive reviewof self-regulation interventions from birth through young adulthood. (OPRE Report #2016–34). Retrieved from Washington, D.C.: https://www.acf.hhs.gov/sites/default/files/documents/acf_report_3_approved_fromword_b508_0.pdf
Murray, D. W., Rosanbalm, K., Christopoulos, C., & Meyer, A. L. (2019). An applied contextual model for promoting self-regulation enactment across development: Implications for prevention, public health and future research. The Journal of Primary Prevention, 40(4), 367–403. https://doi.org/10.1007/s10935-019-00556-1
Narayan, A. J., Rivera, L. M., Bernstein, R. E., Harris, W. W., & Lieberman, A. F. (2018). Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse & Neglect, 78, 19–30. https://doi.org/10.1016/j.chiabu.2017.09.022
National Scientific Council on the Developing Child. (2015). Supportive relationships and active skill-building strengthen the foundations of resilience. Retrieved from https://developingchild.harvard.edu/resources/supportive-relationships-and-active-skill-building-strengthen-the-foundations-of-resilience
Ortiz, R. (2019). Building resilience against the sequelae of adverse childhood experiences: Rise up, change your life, and reform health care. American Journal of Lifestyle Medicine, 13(5), 470–479. https://doi.org/10.1177/1559827619839997
Petruccelli, K., Davis, J., & Berman, T. (2019). Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse and Neglect. https://doi.org/10.1016/j.chiabu.2019.104127
Porche, M. V., Costello, D. M., & Rosen-Reynoso, M. (2016). Adverse family experiences, child mental health, and educational outcomes for a national sample of students. School Ment Health, 8(1), 44–60. https://doi.org/10.1007/s12310-016-9174-3
Robles, A., Gjelsvik, A., Hirway, P., Vivier, P. M., & High, P. (2019). Adverse childhood experiences and protective factors with school engagement. Pediatrics, 144(2). https://doi.org/10.1542/peds.2018-2945
Schurer, S., Trajkovski, K., & Hariharan, T. (2019). Understanding the mechanisms through which adverse childhood experiences affect lifetime economic outcomes. Labour Economics. https://doi.org/10.1016/j.labeco.2019.06.007
Sciaraffa, M. A., Zeanah, P. D., & Zeanah, C. H. (2017). Understanding and promoting resilience in the context of adverse childhood experiences. Early Childhood Education Journal, 46(3), 343–353. https://doi.org/10.1007/s10643-017-0869-3
Sege, R. D., & Harper Browne, C. (2017). Responding to ACEs with hope: Health outcomes from positive experiences. Academic Pediatric, 17(7S), S79–S85. https://doi.org/10.1016/j.acap.2017.03.007
Soleimanpour, S., Geierstanger, S., & Brindis, C. D. (2017). Adverse childhood experiences and resilience: Addressing the unique needs of adolescents. Academic Pediatrics, 17(7S), S108–S114. https://doi.org/10.1016/j.acap.2017.01.008
Song, W., & Qian, X. (2020). Adverse childhood experiences and teen sexual behaviors: The role of self-regulation and school-related factors. Journal of school health, 90(11), 830–841. https://doi.org/10.1111/josh.12947
Stempel, H., Cox-Martin, M., Bronsert, M., Dickinson, L. M., & Allison, M. A. (2017). Chronic school absenteeism and the role of adverse childhood experiences. Academic pediatric, 17(8), 837–843. https://doi.org/10.1016/j.acap.2017.09.013
Thomas, M. S., Crosby, S., & Vanderhaar, J. (2019). Trauma-informed practices in schools across two decades: An interdisciplinary review of research. Review of research in education, 43(1), 422–452. https://doi.org/10.3102/0091732x18821123
Uddin, J., Alharbi, N., Uddin, H., Hossain, M. B., Hatipoglu, S. S., Long, D. L., & Carson, A. P. (2020). Parenting stress and family resilience affect the association of adverse childhood experiences with children’s mental health and attention-deficit/hyperactivity disorder. Journal of affective disorders, 272, 104–109. https://doi.org/10.1016/j.jad.2020.03.132
United States Census Bureau. (2020). 2019 National Survey of Children’s Health: Methodology report. Retrieved from https://www.childhealthdata.org/learn-about-the-nsch/methods
Wade, R., Jr., Shea, J. A., Rubin, D., & Wood, J. (2014). Adverse childhood experiences of low-income urban youth. Pediatrics, 134(1), e13–20. https://doi.org/10.1542/peds.2013-2475
Woodward, L. J., Lu, Z., Morris, A. R., & Healey, D. M. (2017). Preschool self regulation predicts later mental health and educational achievement in very preterm and typically developing children. The clinical neuropsychologist, 31(2), 404–422. https://doi.org/10.1080/13854046.2016.1251614
Zins, J. E., & Elias, M. J. (2007). Social and emotional learning: Promoting the development of all students. Journal of educational and psychological consultation, 17(2–3), 233–255.
Funding
No funding was received in order to conduct this study.
Author information
Authors and Affiliations
Contributions
K. K. formulated the initial study, completed the data analysis, and drafted the manuscript; R. E. contributed to the development of the manuscript, assisted in conceptualizing the study, and assisted in the drafting of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Data utilized in this study was de-identified, secondary data from the 2019 National Survey of Children’s Health that was determined to be not human subjects research based upon review by the University of Alabama at Birmingham Institutional Review Board.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keane, K., Evans, R.R. Exploring the Relationship Between Modifiable Protective Factors and Mental Health Issues Among Children Experiencing Adverse Childhood Experiences Using a Resilience Framework. Journ Child Adol Trauma 15, 987–998 (2022). https://doi.org/10.1007/s40653-022-00471-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40653-022-00471-4