Abstract
Background and objectives
End stage renal disease (ESRD) patients are exposed to the risk of ionizing radiation during repeated imaging studies. The variability in diagnostic imaging policies and the accompanying radiation doses across various renal units is still unknown. We studied this variability at the centre level and quantified the associated radiation doses at the patient level.
Methods
Fourteen Italian nephrology departments enrolled 739 patients on haemodialysis and 486 kidney transplant patients. The details of the radiological procedures performed over one year were recorded. The effective doses and organ doses of radiation were estimated for each patient using standardized methods to convert exposure parameters into effective and organ doses
Results
Computed tomography (CT) was the major contributor (> 77%) to ionizing radiation exposure. Among the haemodialysis and kidney transplant patients, 15% and 6% were in the high (≥ 20 mSv per year) radiation dose groups, respectively. In haemodialysis patients, the most exposed organs were the liver (16 mSv), the kidney (15 mSv) and the stomach (14 mSv), while the uterus (6.2 mSv), the lung (5.7 mSv) and the liver (5.5 mSv) were the most exposed in kidney transplant patients. The average cumulative effective dose (CED) of ionizing radiation among centres in this study was highly variable both in haemodialysis (from 6.4 to 18.8 mSv per patient-year; p = 0.018) and even more so in kidney transplant (from 0.6 to 13.7 mSv per patient-year; p = 0.002) patients.
Conclusions
Radiation exposure attributable to medical imaging is high in distinct subgroups of haemodialysis and transplant patients. Furthermore, there is high inter-centre variability in radiation exposure, suggesting that nephrology units have substantially different clinical policies for the application of diagnostic imaging studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
End stage renal disease (ESRD) patients make up a population (of the almost) unique risk profile for adverse clinical outcomes spanning from cardiovascular disease to infectious disease and cancer. The death rate for cardiovascular and non-cardiovascular complications in this population is about ten times higher than in the coeval general population [1]. The risk for various types of cancers in ESRD patients younger than 35 years of age is at least three times higher than in age- and sex-matched individuals in the general population [2]. According to the United States Renal Data System (USRDS), ESRD patients on average are hospitalized twice a year and stay in the hospital for 13 days. Due to their high burden of co-morbidities, these patients are repeatedly exposed to imaging studies and ionizing radiation both for diagnostic and therapeutic purposes. In the same vein, ESRD patients who receive a kidney transplant frequently undergo diagnostic studies to evaluate early and late graft complications, acute rejection, drug toxicity, ischaemic damage and other renal and extra-renal complications. Because of the cumulative, long-term effects of radiation exposure, this scenario is of concern, particularly for the risk of cancer. The radiation burden of medical imaging in these patients can be high, with an estimated effective dose of more than 100 mSv in just a few years [3,4,5,6]. Some ESRD patients, e.g. haemodialysis patients on waiting lists for transplantation, might have sufficiently high exposure to ionizing radiation which may materially contribute to their increased risk of cancer. However, to date, only relatively small single-centre studies have been carried out. These studies are inherently limited because the use of radiation-related procedures is highly variable depending on the (local) availability of technologies, hospital size and output, and local clinical policies. Furthermore, in all these studies radiation exposures were measured by the estimated effective dose (ED), which is a sex- and age- averaged metric and as such is an inherently imperfect estimator of the risk of radiation at the individual level. Studies focusing on patient-specific assessment of cumulated equivalent organ doses (HT) [7] are (held as) a necessary step to improve the estimate of the risk of ionizing radiation exposure in the ESRD population.
In this survey involving fourteen Italian nephrology units, representative of the diagnostic and monitoring practices in ESRD and transplant patients in Italy, we aimed at quantifying exposure to ionizing radiation on an individual basis by estimating both the cumulated ED and HT.
The secondary aim was to investigate the presence of differences in average patient radiation exposure among centres.
Materials and methods
Data collection
The Institutional Review Board approved the study of each participating centre.
Given the fact that our study deals with data extracted from electronic medical records for which patients already provided informed consent, no further “informed consent” was requested.
We selected Italian Nephrology and Transplantation units with sizeable dialysis units (i.e. with at least 50 patients) and with follow up clinics dedicated to renal transplant patients. These units had to be located in Hospitals with a well-established Radiological Information System and a Picture Archiving and Management System. A complete list of participating centres can be found in the legend of Tables 2 and 3.
We collected complete demographic and clinical data for each patient and detailed information about examinations involving ionizing radiation exposure, including dosimetric parameters, from all participating units. Physicians at these units were asked to fill in pre-established forms for clinical and dosimetric data and to upload them to an online database. Data were analysed centrally by the coordinating centres of Reggio Calabria and Novara.
Data collection was carried out between 1st January and 31st December, 2011 in 11 Units, and from 1st January to 31st December, 2012 in three Units. We excluded patients who had been diagnosed with cancer within 5 years from the start of the follow-up or during the study period. The exclusion of these patients rested under the assumption that these cancers were unlikely to be related to the exposures being measured for the present analysis. Only patients with a follow-up duration ≥ 1 year were included in the study. Patients who died in the 6 months after the completion of data collection were excluded from the study because their exposure to ionizing radiation risk could be inflated by their poor health status thus ? demanding intensive investigations. Co-morbidities were abstracted by reviewing medical notes, clinical summaries and patient interviews.
Radiology examinations performed during the study period were directly obtained from the Radiology Information System of the participating centres. For conventional radiology examinations, only the number of each specific procedure was recorded. With regard to computed tomography (CT), the number of series, the length of coverage per series, the kV, pitch, average mAs, volumetric CT dose index (mGy), and dose-length product (mGy cm) were registered, while for nuclear medicine procedures, the individual administered activity of a specific radiopharmaceutical was recorded. For interventional radiology procedures, the dose area product (Gy cm2) was registered.
Data validation
The data set was verified for completeness and consistency by cross-checks of the records in the database. First, missing values and outliers were sought in order to identify potential mistakes. Suspected outliers generated by errors in unit conversion or transcription errors were identified and corrected. Further possible inconsistencies in the data were identified by cross-checking with redundancies in the collected information. All data defined by this process were then analysed in detail. Whenever it was deemed necessary, the participating centres were contacted and asked to integrate incomplete data or correct inconsistent data.
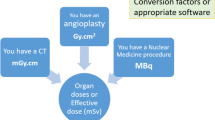
Estimates of radiation doses
Along with current recommendations for conventional diagnostic radiology procedures [8], ED and HT estimates were derived for each specific examination using the PCXMC 1.5 software (STUK, Radiation and Nuclear Safety Authority, Helsinki, Finland) assuming a fixed set of exposure parameters summarized in Table 1.
For cardiac interventional radiology procedures, radiation doses were measured by the dose area product in Gy cm2 using inbuilt ionization chambers. The ED and the HT were derived using conversion factors described elsewhere [9].
The ED and the HT for CT were estimated using the individual dose reports and the computational software ImPACT CT patient dose calculator v1.03 (ImPACT, London, UK) which uses tissue weighing coefficients, as specified by the International Commission on Radiological Protection publication 103 [10]. Average mAs were used in computations to account for the use of tube current modulation in modern scanners [11].
The ED and the HT from nuclear medicine procedures were estimated by considering the individual administered activity of specific radiopharmaceuticals. Conversion coefficients relating ED and HT to administered activity were obtained from the addenda to ICRP Publication 53 [12]. In positron emission tomography/CT studies, the contribution of the CT used for attenuation correction was attributed to nuclear medicine procedures.
Cumulative effective dose (CED) and cumulated HT were expressed for each patient in mSv per patient-year.
Statistical analysis
Data were described using the mean and standard deviation or median and intra-quartile ranges. One way Analysis of Variance (ANOVA) was used to assess the presence of significant differences among participating centres in terms of CED. The correlation between continuous anagraphic and clinical variables with CED was assessed using Spearman’s rank correlation coefficient. The impact of comorbidities on CED was assessed using the Mann–Whitney U test.
CED and cumulated HT were expressed as least squares means, which are the best linear estimates in the population for the marginal means in the ANOVA design. The standard errors of the means (and thus the 95% confidence intervals) were estimated using the whole data set starting from the error variance [13].
Box and whisker plots were used to provide a graphical representation of the distribution of individual dosimetric indexes among centres.
Statistical analyses were performed using the software STATISTICA 6.0 (StatSoft Inc, Tulsa, OK) using a two-sided type I error rate of 0.05.
Results
Overall, 739 haemodialysis and 486 kidney transplant patients entered this study over the (fixed) 1-year time window. The demographic and clinical characteristics of these patients listed by centre are reported in Tables 2 and 3, respectively. On average, age was 67 ± 15 years (63% males) for haemodialysis patients and 55 ± 13 years (63% males) for kidney transplant patients. Among haemodialysis patients, 11% were on the renal transplant waiting list, 27% had diabetes, 22% had a history of coronary heart disease, and 14% had had a neoplasia. The corresponding figures for these co-morbidities among kidney transplant patients were 13% (both for diabetes and coronary heart disease) and 8% (neoplasia).
Statistically significant correlations between continuous anagraphic and clinical variables with CED and the impact of comorbidities on CED are reported in Table 4.
The total number of radiology procedures carried out during the 1-year follow-up was 3093 in haemodialysis and 836 in transplant patients. The median number of procedures was 2 (interquartile range 1–6) in the former group and 1 (0–3) in the latter. The frequency distribution of radiological procedures among participating centres is reported in Fig. 1.
The proportion of total radiation exposure attributable to different types of investigations is shown in Table 5, together with mean CED and Total CED. The median CED in haemodialysis patients was 2.4 mSv (interquartile range 0.2–11.7 mSv), which was six times higher than the corresponding value of 0.4 mSv (IQR = 0.0–2.0) in kidney transplant patients. The distribution of CED among centres is reported in Fig. 2.
We calculated population-based rates of CED for the overall study population according to the categories proposed by Fazel et al. [14]. Among haemodialysis patients, 40% were in the negligible (< 1 mSv per year), 45% were in the low-moderate (< 20 mSv per year), 10% were in the high (20 to < 50 mSv per year) and 5% in the very high (≥ 50 mSv per year) radiation dose levels. Among the kidney transplant subjects, 40% were in the negligible, 54% were in the low-moderate, 4% were in the high and 2% in the very high radiation dose levels.
The averages of the estimated CED are reported in Fig. 3 in increasing order of magnitude across different centres. Average CED among participating centres ranged from 6.4 to 18.8 mSv per patient-year among haemodialysis patients and from 0.6 to 13.7 mSv per patient-year among kidney transplant patients. Of note, the variation of average CED among participating centres was highly significant both in haemodialysis (F = 2.10; p = 0.018) and in kidney transplant (F = 2.69; p = 0.002) patients.
The average cumulated HT are reported in ascending order in Fig. 4. In haemodialysis patients, the most exposed organs were the liver (16 mSv), the kidney (15 mSv) and the stomach (14 mSv), while the uterus (6.2 mSv), the lung (5.7 mSv) and the liver (5.5 mSv) were the most exposed in kidney transplant patients. On average, exposure to CT contributed 77% to HT with a maximum of 89% for the ovaries and a minimum of 62% for the lungs. Conventional radiology provided on average 10% of HT with a maximum of 25% for the lungs. Nuclear Medicine contributed on average 6.6% to HT,, and the bladder (15%) and the colon (12%) were the most exposed organs. Interventional Radiology contributed on average 6.6% to HT, and peak exposures were in the liver (15%) and the lungs (11%).
Discussion
This study involving 14 nephrology units in Italy shows that radiation exposure attributable to medical imaging in haemodialysis and transplant patients is on average low. However, about 15% of haemodialysis patients and 6% of transplant patients have high or very high exposures to ionizing radiation. Radiation exposure was highly variable among centres suggesting substantially different clinical policies for the application of imaging studies in the haemodialysis and transplant populations.
Radiation is one of the most extensively studied carcinogens. Estimates of potential cancer risk from radiation are currently based on a linear no-threshold model, which is the model best supported by available epidemiological data [15]. According to the BEIR VII report [16], a radiation dose of the magnitude of 100 mSv can cause various types of neoplasias. As remarked, patients with end-stage renal disease have an excess risk for cancer as compared to the general population [2].
Doses of radiation from medical imaging procedures can be substantial in selected groups of patients who undergo repetitive imaging studies. A recent systematic review documented that ESRD is the condition entailing the highest risk of exposure to ionizing radiation, after cancer [17].
The median cumulative effective dose of ionizing radiation exposure in haemodialysis and transplant patients included in this study is within the limits of the natural background exposure. The cumulative dose was higher in haemodialysis (2.4 mSv per patient-year) than in transplant (0.4 mSv per patient-year) patients, possibly because of concerns about the nephrotoxic potential of iodinated contrast agents in transplanted patients.
The long-term risk due to the use of medical radiation should always be incorporated into the risk–benefit assessment of diagnostic and therapeutic imaging. However, profiling the risk–benefit is complex in ESRD patients, a selected group of patients with multiple co-morbidities and severe competing and confounding risks for death and cancer. While radiation exposure in this survey is reasonably low when considering the whole population, it is not negligible when considering the most exposed subgroups. For instance, when selecting only patients in the upper fourth quartile, the average CED (37.7 and 16.5 mSv patient-year for haemodialysis and kidney transplant, respectively) is equal to or higher than the median CED in patients with gastric cancer (52.3 mSv for 47 months) [18], or lung cancer (84 mSv for 36 months) [19].
Haemodialysis patients with previous myocardial infarction, diabetes and without previous cancer were subjected on average to lower CED. Although statistically significant, the very weak negative correlations between CED and age and haemodialysis vintage could hardly be interpreted as being clinically relevant. In kidney transplant patients the only demographical variable associated with a lower CED was male sex, whilst the presence of comorbidities was not associated with different CEDs.
The substantial between-centre variability in patient’ exposure to ionizing radiation is a relevant finding of the present study. The variability was striking for transplant patients, for whom we observed a 20-fold variation between the minimum and maximum average radiation exposure among different centres.
A meta regression with the average CED per centre as the dependent variable and anagraphic, clinical and comorbidities as the independent variables failed to identify any statistically significant predictor of the average CED in either haemodialysis or kidney transplant centres.
Awareness of the risk of exposure to ionizing radiation remains unsatisfactory among clinical nephrologists. Patients are followed up based on local protocols by applying radiological examinations at disparate time-intervals which results in a highly variable intensity of exposure depending on the local clinical policies. Protocol harmonization and education of nephrologists on the risks of radiation exposure are of obvious importance to limit such risk in these populations.
The source of ionizing radiation exposure was variable across organs or tissues. Nuclear medicine contributed to more than 12% of the exposure of the bladder and the colon. This observation goes along with the fact that the excretion of most radionuclides is via the urinary and gastrointestinal systems. Interventional radiology was responsible for 18% of the exposure of the liver and the lungs, which are the most exposed organs during cardiac procedures such as coronary angiography or percutaneous angioplasty. On the other hand, conventional radiology provided the maximum contribution in the lung (25%), while CT was responsible in 89% of the exposures of the ovaries and uterus.
Some limitations in our survey should be acknowledged. First, there are uncertainties about the assumptions concerning the shape and the geometry of exposed organs and the estimation of effective doses and measured dosimetric indexes. However, the methods we applied are the standard ones used worldwide to estimate the risk of exposure to ionizing radiation [20]. The fact that our observations are limited to a single country is another limitation. Therefore, findings in the present study cannot be generalized to other countries. International surveys are needed to confirm whether the risk of excessive exposure to ionizing radiations in some subgroups of haemodialysis and transplant patients also applies to countries other than Italy. Shared, evidence-based protocols limiting the application of imaging studies implying exposure to ionizing radiation is of obvious importance for reducing the risk of such exposures among these populations.
References
de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomedas LM, Ansell D et al (2009) Cardiovascular and non-cardiovascular mortality among patients starting dialysis. JAMA 302:1782–1789
Maisonneuve P, Agodoa L, Gellert R, Stewart JH, Buccianti G, Lowenfels AB et al (1999) Cancer in patients on dialysis for end-stage renal disease: an international collaborative study. Lancet 354:93–99
Kinsella SM, Coyle JP, Long EB, McWilliams SR, Maher MM, Clarkson MR et al (2010) Maintenance hemodialysis patients have high cumulative radiation exposure. Kidney Int 78:789–793
De Mauri A, Brambilla M, Chiarinotti D, Matheoud R, Carriero A, De Leo M (2011) Estimated Radiation exposure from medical imaging in hemodialysis patients. J Am Soc Nephrol 22:571–578
Nguyen KN, Patel AM, Weng FL (2013) Ionizing radiation exposure among kidney transplant recipients due to medical imaging during the pretransplant evaluation. Clin J Am Soc Nephrol 8:833–839
De Mauri A, Brambilla M, Izzo C, Matheoud R, Chiarinotti D, Carriero A et al (2012) Cumulative radiation dose from medical imaging in kidney transplant patients. Nephrol Dial Transplant 27:3645–4365
Brambilla M, De Mauri A, Lizio D, Matheoud R, De Leo M, Carriero A (2014) Estimated radiation risk of cancer from medical imaging in haemodialysis patients. Nephrol Dial Transplant 29:1680–1686
Mettler FA, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248:254–263
Compagnone G, Ortolani P, Domenichelli S, Ovi V, Califano G, Dall’Ara G et al (2011) Effective and equivalent organ doses in patients undergoing coronary angiography and percutaneous coronary intervention. Med Phys 38:2168–2175
The 2007 recommendations of the International Commission on Radiological Protection: ICRP publication 103. Ann ICRP 2007
Miglioretti ADL (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169:2078–2086
ICRP publication 80 (1998) Radiation dose to patients from radiopharmaceuticals. Addendum 2 to ICRP 53. Also, includes addendum 1 to ICRP publication 72. Ann ICRP 28:1–130
Milliken GA, Johnson DE (2009) Analysis of messy data, volume I: designed experiments. Chapman and Hall/CRC, New York
Fazel R, Krumholtz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361:849–857
Little MP, Wakeford R, Tawn EJ, Bouffler SD, de Gonzalez BA (2009) Risks associated with low doses and low dose rates of ionizing radiation: why linearity may be (almost) the best we can do. Radiology 251:6–12
Board of Radiation Effects Research Division on Earth and Life Sciences National Research Council of the National Academies (2006) Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. National Academies Press, Washington, DC
Brambilla M, De Mauri A, Leva L, Carriero A, Picano E (2013) Cumulative radiation dose from medical imaging in chronic adult patients. Am J Med 126:480–486
Lee YJ, Chung YE, Lim JS, Kim JH, Kim YJ, Lee HJ et al (2012) Cumulative radiation exposure during follow-up after curative surgery for gastric cancer. Korean J Radiol 13:144–151
Stiles BM, Mirza F, Towe CW, Ho VP, Port JL, Lee PC et al (2011) Cumulative radiation dose from medical imaging procedures in patients undergoing resection for lung cancer. Ann Thorac Surg 92:1170–1178
Martin CJ (2007) Effective dose: how should it be applied to medical exposures. Br J Radiol 80:639–647
Acknowledgements
This work was presented in abstract form at the ERA-EDTA Congress–Wien 2016 and the ECMP Congress–Athens 2016.
MIRA-ESRD study Investigators and participating centres: Emilio Balestra (Ancona), Diego Bellino (Genova), Roberta Benevento (Bologna), Cristina Bregant (Trieste), Paola Bregant (Trieste), Barbara Cannillo (Novara), Giuseppe Casto (Pisa), Doriana Chiarinotti (Novara), Sara Cimolai (Mestre), Giacomo Colussi (Milano), Antonio De Agostini (Brescia), Fausto Declich (Lecco), Maria Grazia Facchini (Bologna), Maria Alessandra Galione (Lecco), Cesare Gavotti (Genova), Ugo Gerini (Trieste), Paola Isoardi (Torino), Cristina Izzo (Novara), Fabrizio Levrero (Genova), Eric Lorenzon (Trieste), Stefano Maffei (Torino), Stefania Maggi (Ancona), Alberto Mari (Ancona), Federico Mattana (Genova), Alberto Menegotto (Milano), Ophelia Meniconi (Pisa), Nicoletta Paruccini (Monza), Luisa Pierotti (Bologna), Federico Pieruzzi (Monza), Giuseppe Pontoriero (Lecco), Adele Postorino (Reggio Calabria), Marco Quaglia (Novara), Osvaldo Rampado (Torino), Andrea Ranghino (Torino), Sonia Reccanello (Mestre), Stefania Sabatino (Udine), Giulia Sangalli (Lecco), Chiara Sottocornola (Pisa), Marina Sutto (Milano), Salvatore Tata (Mestre), Alberto Torresin (Milano), Antonio Traino (Pisa), Annalisa Trianni (Udine), Letizia Zeni (Brescia).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest and funding statement
The authors have no conflicts of interest and no funding to declare.
Ethical approval
The Institutional Review Board approved the study of each participating centre.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the MIRA-ESRD Study Investigators are mentioned "Acknowledgements" section.
Rights and permissions
About this article
Cite this article
Postorino, M., Lizio, D., De Mauri, A. et al. Radiation dose from medical imaging in end stage renal disease patients: a Nationwide Italian Survey. J Nephrol 34, 791–799 (2021). https://doi.org/10.1007/s40620-020-00911-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00911-0