Abstract
Background
Scleroderma renal crisis (SRC), the most frequent renal complication of Systemic Sclerosis (SSc), can lead to end-stage renal disease (ESRD), most frequently, but not exclusively, because of scleroderma renal crisis (SRC).
Methods
The main objectives of our study using data extracted from the French renal epidemiology and information network (REIN) registry, were to describe the characteristics and outcomes in an incident French cohort of SSc patients requiring renal replacement therapy (RRT) compared with a matched RRT patient sample.
Results
Between 2002 and 2014, 120 incident SSc patients started RRT in France. SSc was significantly associated with higher mortality (HR 1.95; 95% CI 1.41–2.71; p = 0.001) in comparison with matched controls. Among SSc patients in dialysis, besides age, the only risk factor independently associated with mortality was the inability to walk without help (HR 2.34, CI 95% 1.37–4.02, p = 0.002). Dialysis withdrawal was reported for 22 (18.3%) of the SSc patients compared to 15 (6.3%) for the controls. Patients with SSc have less access to transplantation waiting list (HR 0.21; CI 95% 0.11–0.41, p < 0.001) and to kidney transplantation (KTR) (HR 0.22; 95% CI 0.12–0.43; p < 0.001). During the follow-up, 6 of the 27 patients (22.2%) registered on KTR waiting list died compared to 69 of the 93 (74.2%) patients who were not on the waiting list.
Conclusions
The prognosis for SSc patients requiring RRT is still poor, with a significantly higher mortality and lower registration on kidney transplant waiting-list compared to matched controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic Sclerosis (SSc), also called scleroderma, is a multi-organ autoimmune disease characterized by collagen deposit, inflammation and microvascular disease in several organs including the skin, lung, heart or digestive tract [1]. Among the complications of SSc, renal involvement, and particularly the occurrence of Scleroderma Renal Crisis (SRC) is one of the most serious complications, and a life-threatening condition [2].
The reported incidence of SRC varies across the different studies, from 4 to 12%, more frequent in diffuse SSc than in limited SSc [3,4,5]. Some risk factors are well identified: older age, male gender and anti-RNA polymerase III antibody are independent risk factors for SRC [6], and in addition the use of high-dose corticosteroids can trigger SRC [7].
In more than half of the cases, SRC leads to End-Stage Kidney Disease (ESKD) and requires dialysis [3, 7,8,9,10]: 62% of 110 patients with SRC reported by Penn required dialysis [3]. For some patients, partial renal function recovery is observed, and dialysis can be discontinued: in 2000, Steen [9] reported more than 50% renal recovery for patients with SRC who required renal replacement therapy (RRT).
Despite the quite good efficacy of Angiotensin Converting Enzyme Inhibitors (ACEi) in prevention and treatment of SRC [10, 11], the occurrence of SCR is still associated with a poor prognosis. In a French cohort of 91 patients reported in 2012, 40.7% died within the year after the SRC [7]. Long-term survival in SRC is poor, especially for patients who do not recover renal function [7, 8].
Although the short-term prognosis for scleroderma patients developing kidney disease was reported in these studies, there is limited data available on long term outcomes for patients who required chronic RRT.
Furthermore, other causes of kidney disease in scleroderma can lead to ESKD in SSc: nephroangiosclerosis, drug toxicity or ANCA vasculitis have been reported [1,2,3,4].
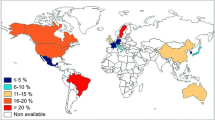
Only two studies in the United States in 2002 [12] and Australia in 2011 [13] analyzed and compared survival of patients with ESKD consecutive to SSc with that of patients with ESKD from other causes: in these two studies, mortality was higher among SSc patients compared to other ESKD patients.
In France, data about patients requiring RRT are collected in a single record, no study has been conducted to assess survival among patients with ESKD with SSc and requiring RRT.
In this context, the main objective of our study, was to determine if SSc appears as factor impacting survival and access to Kidney Transplantation (KTR), in an incident French cohort of patients on dialysis with SSc.
The secondary objectives of this study, using patients' clinical records, were to describe more precisely the clinical manifestations of SSc and the natural history of the disease before the need for dialysis or KTR.
Methods
REIN and patients selection
The Renal Epidemiology and Information Network (REIN) was established in 2001 and has been progressively developed in all French regions up to 2011 and include all patients with ESKD requiring renal replacement therapy [14].
SSc incident patients identified from the initial nephropathy, secondary causes of nephropathy or associated diagnoses recorded in REIN and who started RRT from 1st January 2002 to 31st December 2014 were included in our study. The follow-up lasted until the 31st December 2016.
Data collection
REIN registry
To describe patient characteristics and study any events of interest, three categories of variables were extracted from REIN: (i) demographic data: gender and age; (ii) baseline bio-clinical data: smoking status (current/former smoker, never-smoked); albumin; hemoglobin; Body Mass Index (BMI); malnutrition (serum albumin < 30 g/L or BMI < 20 kg/m2) and comorbidities: diabetes, active malignancy, hepatic disease, chronic respiratory disease, cardiovascular disease (coronary artery disease, peripheral vascular disease, congestive heart failure, arrhythmia, aortic aneurism and cerebrovascular disease), level of walking disability (autonomous, partially dependent and totally dependent); and (iii) information on the medical follow-up: Renal Replacement Therapy (RRT), RRT mode [HemoDialysis (HD), Peritoneal Dialysis (PD), kidney transplantation (KTR)], emergency vs planned first dialysis session, initiation of RRT using a catheter, date of placement on the renal KTR waiting list, date of KTR and date of death. These data are collected by nephrologist or clinical research associate in each center or region.
Medical records
A standardized anonymous questionnaire was completed by authors to collect additional data from patients' clinical records. Items required were: date of diagnosis of SSc, renal function at diagnosis (normal kidney function or kidney disease known before SSc), date of SRC if it occurred, kidney biopsy, renal function recovery and dialysis withdrawal, treatment received (corticosteroids, ACEi, immunosuppressive drugs), clinical manifestations of SSc (malignant hypertension, cardiac, lung, cutaneous, articular, or digestive involvement) and serum antibodies (antinuclear, anti-Scl70, anti RNA polymerase III). All the data collected from patients' clinical records were included in the REIN data base.
Statistical analyses
For the descriptive analyses, categorical variables are presented as numbers and percentages, continuous variables are presented as means and Standard Deviations (SD) or as medians with first- and third-quartiles (InterQuartile Range, IQR).
Each patient on dialysis (HD or PD), with SSc, were matched to 2 patients on dialysis for other cause. Matching characteristics were: gender, age (± 3 years), year of dialysis initiation and several risk factors: diabetes mellitus, cerebrovascular disease (stroke or transient ischemic attack), coronary artery disease (combining coronary insufficiency and myocardial infarction).
Patient follow-up was assessed from the date of first dialysis to the outcome (death, KTR or end of follow-up). Patient survival was assessed from the date of first RRT to death, or to December 31st, 2016. The association between patient-related data and the outcomes of interest was assessed using univariate and multivariate Cox proportional hazard models. Variables with a p value < 0.20 in univariate models were included in the multivariate models. A p value < 0.05 was considered statistically significant. Results were reported as hazard ratios (HR) for Cox analyses with 95% confidence intervals (95% CI). Kaplan Meier failure curves were generated and the log-rank test was used to compare curves.
Descriptive analyses were performed on EXCEL 2016 software (Microsoft®). Survival analyses were performed using the STATA 13.1 software.
Ethics
The National Commission for Information Technology and Privacy (CNIL) approved the data collection conducted by the REIN. The REIN is registered with the CNIL under the number 903188 Version 3. The REIN Scientific Committee approved this study.
Results
Characteristics of 120 SSc patients at the first RRT
Between 2002 and 2014, 120 incident SSc patients started dialysis, amounting to 1.28‰ of the 93,463 incident patients under RRT in France.
The characteristics of patients at initiation of the first RRT are described in Table 1. SSc patients and controls were comparable for the matching characteristics. More SSc patients presented congestive heart failure, arrythmia, chronic lung disease, malnutrition and inability to walk without help.
For the 120 SSc patients, SSc was registered as the primary or secondary cause of nephropathy, but one or several associated diagnoses or causes of nephropathy were also observed. The other diagnoses were: malignant hypertension, for 46 (38.3%) patients, thrombotic microangiopathy for 11 (9.2%) patients, hemolytic and uremic syndrome for 3 (2.5%) patients, nephroangiosclerosis for 6 (5%) patients, and glomerulopathy for 6 (5%) patients.
A renal biopsy was more frequently performed for patients with SSc (57.5%) than for control patients (23.3%).
SSc patients more often started dialysis in emergency compared to controls (55.8% compared to 26.3%) and had less often ArterioVenous Fistula (AVF) created before the start of dialysis (13.2% vs 52.8%). At the end of the follow-up, 68.4% of the SSc patients on HD had no AVF, compared to 33.0% of the control patients.
Survival among the 120 patients with SSc: comparison with 240 controls
The median follow-up for the SSc patients was 34.5 (12.5–60) months, 75 patients (62.5%) had died at the end of follow-up. The global survival of the SSc patients was significantly lower than that of the matched controls (log-rank test: p < 0.001; Fig. 1). Among the patients who died during the follow-up, 85% were died 5 years after dialysis start (median = 20.5 months; IQR: 7–46 months).
In the multivariate survival analysis (Table 2), SSc was significantly associated with a higher mortality rate (HR 1.95; 95% CI 1.41–2.71; p = 0.001) compared to matched controls.
Causes of death and risk factors for mortality among the 120 SSc patients
Cardiovascular events were the most frequent cause of death, more frequent among SSc patients (29.3%) than among control. Death was attributed to SSc for 5 (6.7%) patients. Other causes of death are reported in Table 3.
In the univariate survival analysis, and after multivariate logistic Cox regression analysis and adjustment, besides age, the only risk factor associated with mortality among the 120 SSc patients was the inability to walk without help (HR, 2.34, CI 95% 1.37–4.02, p = 0.002 in multivariate model).
Waiting list and kidney transplantation: comparison of the 120 SSc patients and the 240 controls
Twenty-seven (22.5%) SSc patients were registered on KTR waiting list at the end of follow-up compared to 104 (43.3%) of the matched controls. No SSc patient was listed on the KTR waiting list before the start of dialysis compared to 27 (11.25%) of the control patients. The percentage of patients with SSc waitlisted was 7.5%, 16,7% and 21.7%, and 30%, 38% and 43.3% for the matched controls respectively at 1, 2 and 5 years. Because 95% of waitlisted patients were transplanted, 5 years after being waitlisted, we built 5 years follow-up failure Kaplan–Meier curves. Multivariate model showed indeed that SSc was associated with a lower rate of wait listing (HR 0.21; CI 95% 0.11–0.41, p < 0.001; Table 4. The median duration before inclusion on the KTR waiting list was longer for the SSc patients 18.3 months (10.5–24.3) than for the control patients 6 months (0.1–16.2) after the start of RRT.
Moreover, SSc patients had a lower relative rate of KTR in comparison to the matched controls (HR 0.22; 95% CI 0.12–0.43; p < 0.001; Table 5. No SSc patients had preemptive KTR (compared to 0.8% of controls) and the median duration on dialysis before KTR was longer for the SSc patients: 32 months (25–43) compared to 18.5 months (11–34) for the control patients. KTR was performed for 1.7% of the SSc patients after 2 years on dialysis, 4.2% after 5 years and 9.2% after 10 years compared to 18.3%, 30.4% and 31.6% respectively at 2, 5 and 10 years for the matched controls (Fig. 2).
Comparison of characteristics according to their outcomes of the 120 SSc patients
Table 6 compares the characteristics at the initiation of RRT according to their outcomes of the 120 SSc patients. Dialysis withdrawal was reported for 22 (18.3%) of the SSc patients compared to 15 (6.3%) of the controls. Among the 22 patients for whom dialysis was discontinued, 5 patients died within 1 month after dialysis stop. For the 17 others, we suppose that they had renal recovery.
Patients on KTR waiting list were significantly younger and had higher serum albumin levels. During the follow-up, 6 of the 27 patients (22.2%) registered on KTR waiting list died compared to 69 of the 93 (74.2%) patients who were not on waiting list.
Additional description of 70 patients
For 73 SSc patients (60.8%), complementary data were collected in medical records. The other 47 files were too old or missing. After examination of the medical records, for 3 patients, a diagnosis of SSc reported in REIN appeared as a reporting mistake.
Clinical manifestations among SSc patients are described in Table 7. Concerning renal involvement: 60 (85.7%) patients had ESKD due to SRC. For 37 patients, the SRC occurred in the year of the SSc diagnosis, and for 19 patients, the SSc had been known for at least one year when the SRC occurred. The date of diagnosis of SSc or of SRC was unknown for 4 patients. Two patients had chronic kidney disease attributed to SSc without SRC. Six patients had ESKD not consecutive to SSc: 3 patients had MPO-ANCA-associated vasculitis (MyeloPerOxidase AntiNeutrophil Cytoplasmic Antibody), 1 patient underwent to dialysis for acute tubular necrosis, 1 patient for cardiorenal syndrome, and for 1 patient the cause of ESKD was unknown.
Sixty-two patients (88.6%) received ACEi, in most cases before or just after the diagnosis of renal involvement due to SSc, and 58.6% had steroids to treat SSc without information on the dose received.
The diagnosis of SSc was known more than 1 year before the first RRT for 32 patients (45.7%). For 34 patients (48.6%), RRT was started in the same year as the diagnosis of SSc. Only 1 patient had been on dialysis for 10 years when the diagnosis of SSc was established. For 3 patients, the date of SSc diagnosis was unknown.
For 12 patients (17.1%), renal recovery enabled the discontinuation of dialysis. Ten of the 12 patients (83.3%) having renal recovery had received ACEi, as had 52 of the 58 (89.7%) patients who remained on dialysis. Regarding steroids, 9 of the 12 patients (75%) having renal recovery and 32 of the 58 (55.2%) patients remaining on dialysis received steroids.
Discussion
This study is the first French cohort to evaluate outcomes and survival of SSc patients on dialysis. In comparison to other national cohorts, the mortality is lower in our study: in the ANZDATA registry (Australian and New Zealand Dialysis and Transplant) [13], the survival rate was 72% at 1 year, and only 29% at 5 years compared to 75% and 43.3% respectively in our cohort, and the 2-year survival rate was 49.3% in the USA [12] compared to 64% in our registry. However, both cohorts included patients in an earlier period. This difference in mortality over time can be attributed in part to the improvement of dialysis techniques over the last 15 years and also to the more frequent use of ACEi in SRC [11] as we observed in our cohort: 88.6% of the 70 patients for whom we had access to medical records received ACEi before or immediately after the SRC.
Since SSc has been described as a cardiovascular risk factor [15, 16], we choose cardiovascular comorbidities as matching factor to compare with a control group among patient have the same global cardiovascular risk except SSc.
As expected, patients with SSc had lower survival rates than the matched controls. This lower survival rate among SSc patients could be explained in part by the more frequent comorbidities, in particular malnutrition and inability to walk without help, although malnutrition is not associated with mortality in our multivariate analysis, probably as a result of the small number of patients. Nevertheless, malnutrition and inability to walk are parameters that have been identified as predictors of frailty [17, 18] and that have an impact on vital prognosis in chronic dialysis. In the multivariate analysis, SSc remained associated with mortality (HR 1.95; 95% CI 1.41–2.71; p = 0.001). This result is comparable to that for a sub-group of 68 SSc patients included in the ANZDATA registry in a more recent period (HR 1.88, 95% CI 1.31–2.70) [12].
Despite their poorer prognosis, 27 (22.5%) SSc patients were registered on KTR waiting list. The SSc patients registered for KTR had better survival than non-registered patients. The only significant difference highlighted in these groups was age: patients on waiting list were younger. SSc patients who remained on dialysis and died appeared frailer, with a higher prevalence of malnutrition and walking difficulties, but these differences were not statistically significant. In the adjusted multivariate analysis, SSc is an independent factor for lesser likelihood of registration on KTR waiting list.
Survival after KTR was not analyzed in our study. However, some studies have shown that the prognosis of SSc patients who received KTR was good [19]. Bertrand et al. [20] studied the outcomes of 34 SSc patients who received a KTR between 1987 and 2013. They showed that patient survival was 100%, 90.3% and 82.5% at 1, 3 and 5 years post‐KTR respectively. In their study, the only identified risk factor for death after KTR was pulmonary involvement. In addition, we underlined that the time lapse to registration on waiting list was longer for SSc patients than for other RRT patients. It has been widely accepted that this delay can be explained by the wait for possible renal recovery or patient stabilization after SRC and emergency dialysis or a concern about the prognosis of these patients [21]. However, given the low rate of renal recovery in our series and the potential delay between registration on waiting list and KTR, and considering (i) that patients on chronic dialysis who are not listed on waiting list have higher risk of mortality [22, 23], and (ii) that the prognosis for SSc patients receiving KTR is good [19, 20], we could suggest that registration on KTR waiting list should not be delayed for young SSc patients with fewer comorbidities.
Our results on global survival of SSc patients requiring dialysis are similar to a recent European study [24]. This study, also shows that SSc patient survival after KTR was similar to that other patients requiring RRT: these recent results confirm that registration on transplant KTR waiting list should be considered more often and earlier for scleroderma patients.
In our study, dialysis discontinuation was more often observed among SSc patients than among matched controls patients, that can be explain by a best rate of kidney function recovery. In the case series reported by Penn in 2007 [3], 34% of the 68 patients who required dialysis after SRC, had recovered sufficient renal function to discontinue dialysis. However, in our study, we observed that (i) some patients died shortly after the discontinuation of dialysis, and (ii) more than half the patients for whom dialysis was discontinued were not followed-up in REIN after renal recovery; raising questions on the reasons for dialysis withdrawal: renal recovery or discontinuation for palliative care? In our subgroup analysis, the proportion of patients having renal recovery was 17.1%. In the ANZDATA registry, recovery of renal function was reported for 10% of SSc patients. This difference could also be explained by the more recent period of our study and the use of ACEi since the 1980s.
The analysis of 70 medical records revealed that 85.7% of the SSc patients had ESKD consecutive to SRC. As usually described [3], SRC occurs early after the diagnosis of SSc: for almost half the patients, dialysis was initiated within one year of the diagnosis of SSc. Even if SRC is the main cause of ESKD among SSc patients, because specific lesions, or MAT or maligne HTA, also associated with SSC, other causes of renal impairment have been reported [25, 26]. In our study, 3 patients had MPO-ANCA vasculitis, which has been reported in other studies [27,28,29]. Regarding non-renal involvement, cardiac, pulmonary and digestive involvement seems less frequent in our study than in the series of 50 patients with SRC reported by Texeira et al. [30]. Because of the small number of patients and incomplete data in our series, we cannot highlight the factors impacting prognosis, in particular for renal recovery or anti-RNA pol III, known to be a predictive factor for SRC [31], but only reported for 11.4% in our series.
In conclusion, SSc patients requiring dialysis have poor prognosis compared to matched controls, with a significantly higher mortality and lower registration on kidney transplant waiting-list compared to matched controls. Nevertheless, the younger patients, or patients with fewer comorbidities, registered on KTR waiting list have better global survival after waiting list registration.
References
Denton CP, Khanna D (2017) Systemic sclerosis. Lancet Lond Engl 390(10103):1685–1699
Traub YM, Shapiro AP, Rodnan GP, Medsger TA, McDonald RH, Steen VD et al (1983) Hypertension and renal failure (scleroderma renal crisis) in progressive systemic sclerosis. Review of a 25-year experience with 68 cases. Med (Baltim) 62(6):335–52
Penn H, Howie AJ, Kingdon EJ, Bunn CC, Stratton RJ, Black CM et al (2007) Scleroderma renal crisis: patient characteristics and long-term outcomes. QJM Mon J Assoc Physicians 100(8):485–494
Walker UA, Tyndall A, Czirják L, Denton C, Farge-Bancel D, Kowal-Bielecka O et al (2007) Clinical risk assessment of organ manifestations in systemic sclerosis: a report from the EULAR Scleroderma Trials And Research group database. Ann Rheum Dis 66(6):754–763
Muangchan C, Canadian Scleroderma Research Group, Baron M, Pope J (2013) The 15% rule in scleroderma: the frequency of severe organ complications in systemic sclerosis. A systematic review. J Rheumatol 40(9):1545–1556
Jaeger VK, Wirz EG, Allanore Y, Rossbach P, Riemekasten G, Hachulla E et al (2016) Incidences and risk factors of organ manifestations in the early course of systemic sclerosis: a longitudinal EUSTAR study. PLoS One 11(10):e0163894
Guillevin L, Bérezné A, Seror R, Teixeira L, Pourrat J, Mahr A et al (2012) Scleroderma renal crisis: a retrospective multicentre study on 91 patients and 427 controls. Rheumatol Oxf Engl 51(3):460–467
Walker JG, Ahern MJ, Smith MD, Coleman M, Pile K et al (2003) Scleroderma renal crisis: poor outcome despite aggressive antihypertensive therapy. Intern Med J 33(5–6):216–20
Steen VD, Medsger TA (2000) Long-term outcomes of scleroderma renal crisis. Ann Intern Med 133(8):600–603
Cozzi F, Marson P, Cardarelli S, Favaro M, Tison T, Tonello M et al (2012) Prognosis of scleroderma renal crisis: a long-term observational study. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 27(12):4398–4403
Steen VD, Costantino JP, Shapiro AP, Medsger TA (1990) Outcome of renal crisis in systemic sclerosis: relation to availability of angiotensin converting enzyme (ACE) inhibitors. Ann Intern Med 113(5):352–357
Abbott KC, Trespalacios FC, Welch PG, Agodoa LYC (2002) Scleroderma at end stage renal disease in the United States: patient characteristics and survival. J Nephrol 15(3):236–240
Siva B, McDonald SP, Hawley CM, Rosman JB, Brown FG, Wiggins KJ et al (2011) End-stage kidney disease due to scleroderma–outcomes in 127 consecutive ANZDATA registry cases. Nephrol Dial Trans Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 26(10):3165–3171
Couchoud C, Stengel B, Landais P, Aldigier JC, de Cornelissen F et al (2006) The renal epidemiology and information network (REIN): a new registry for end-stage renal disease in France. Nephrol Dial Transplant 21(2):411–418
Hesselvig JH, Kofoed K, Wu JJ, Dreyer L, Gislason G, Ahlehoff O (2018) Localized scleroderma, systemic sclerosis and cardiovascular risk: a danish nationwide cohort study. Acta Derm Venereol 98(3):361–365. https://doi.org/10.2340/00015555-2842
Chu SY, Chen YJ, Liu CJ, Tseng WC, Lin MW et al (2013) Increased risk of acute myocardial infarction in systemic sclerosis: a nationwide population-based study. Am J Med 126(11):982–988. https://doi.org/10.1016/j.amjmed.2013.06.025
Kim JC, Kalantar-Zadeh K, Kopple JD (2013) Frailty and protein-energy wasting in elderly patients with end stage kidney disease. J Am Soc Nephrol JASN 24(3):337–351
Johansen KL, Chertow GM, Jin C, Kutner NG (2007) Significance of frailty among dialysis patients. J Am Soc Nephrol JASN 18(11):2960–2967
Gibney EM, Parikh CR, Jani A, Fischer MJ, Collier D, Wiseman AC (2004) Kidney transplantation for systemic sclerosis improves survival and may modulate disease activity. Am J Transplant 4(12):2027–2031
Bertrand D, Dehay J, Ott J, Sberro R, Brunelle C, Kamar N et al (2017) Kidney transplantation in patients with systemic sclerosis: a nationwide multicentre study. Transpl Int Off J Eur Soc Organ Transpl 30(3):256–265
Denton CP, Lapadula G, Mouthon L, Müller-Ladner U (2009) Renal complications and scleroderma renal crisis. Rheumatology 48(Suppl 3):iii32–5.
Bouaoun L, Villar E, Ecochard R, Couchoud C (2013) Excess risk of death increases with time from first dialysis for patients on the waiting list: implications for renal allograft allocation policy. Nephron Clin Pract 124(1–2):99–105
Beuscart J-B, Pagniez D, Boulanger E, Duhamel A (2015) Registration on the renal transplantation waiting list and mortality on dialysis: an analysis of the French REIN registry using a multi-state model. J Epidemiol 25(2):133–141
Hruskova Z, Pippias M, Stel VS, Abad-Díez JM, Benítez Sánchez M et al (2019) Characteristics and outcomes of patients with systemic sclerosis (scleroderma) requiring renal replacement therapy in Europe: results from the ERA-EDTA registry. Am J Kidney Dis 73(2):184–193
Shanmugam VK, Steen VD (2010) Renal Manifestations in Scleroderma: evidence for subclinical renal disease as a marker of vasculopathy. Int J Rheumatol. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2933853/
Steen VD, Syzd A, Johnson JP, Greenberg A, Medsger TA (2005) Kidney disease other than renal crisis in patients with diffuse scleroderma. J Rheumatol 32(4):649–655
Anders HJ, Wiebecke B, Haedecke C, Sanden S, Combe C, Schlöndorff D (1999) MPO-ANCA-Positive crescentic glomerulonephritis: a distinct entity of scleroderma renal disease? Am J Kidney Dis Off J Natl Kidney Found 33(4):e3
Endo H, Hosono T, Kondo H (1994) Antineutrophil cytoplasmic autoantibodies in 6 patients with renal failure and systemic sclerosis. J Rheumatol 21(5):864–870
Cheta J, Binder M, Kowalewska J, Magoon S (2018) ANCA-associated vasculitis co-occurrence with systemic sclerosis: a case report of a rare diagnostic dilemma. J Investig Med High Impact Case Rep 6:2324709618785188
Teixeira L, Mouthon L, Mahr A, Berezné A, Agard C, Mehrenberger M et al (2008) Mortality and risk factors of scleroderma renal crisis: a French retrospective study of 50 patients. Ann Rheum Dis 67(1):110–116
Emilie S, Goulvestre C, Bérezné A, Pagnoux C, Guillevin L, Mouthon L (2011) Anti-RNA polymerase III antibodies are associated with scleroderma renal crisis in a French cohort. Scand J Rheumatol 40(5):404–406
Acknowledgements
Authors thank REIN Registry and all its investigators (www.agence-biomedecine.fr) for the data collection and access. We thank Angela Swain-Verdier for revising the English. The authors declare that the results presented in this paper have not been published previously in whole or in part, except in abstract format.
Funding
This research received funding from the Agence de la Biomédecine.
Author information
Authors and Affiliations
Contributions
AL collected the data from medical forms, designed the study, and wrote the paper. AP performed the statistical analysis and contributed to the writing. CC contributed to design the study, and helped to analysis tools and data from REIN registry. ML performed the extraction of included patients and data from REIN database, performed the matching of patients with controls. CV conceived the original idea, contributed to design the study and supervised the work. All authors proofread the paper and approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Nothing to declare.
Ethical approval
The National Commission for Information Technology and Privacy (CNIL) approved the data collection conducted by the REIN. The REIN is registered with the CNIL under the number 903188 Version 3. The REIN Scientific Committee approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lavergne, A., Pladys, A., Couchoud, C. et al. Systemic sclerosis and end-stage renal disease: study of patient characteristics, follow-up and outcomes in France. J Nephrol 34, 617–625 (2021). https://doi.org/10.1007/s40620-020-00746-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00746-9