Abstract
Sudden cardiac death (SCD) is a major cause of concern in end stage renal disease (ESRD), contributing to 70 % of cardiovascular mortality and 27 % of all-cause mortality in dialysis patients. Yet its mechanisms and pathogenesis remain largely obscure. This review discusses the potential reasons for an exaggerated risk of SCD in ESRD populations taking into account recent studies and registry data and additionally explores the reasons for the reported recent decline in SCD. The types of arrhythmias typical of the hemodialysis population are yet to be fully characterised and in this paper, we introduce an ongoing implantable loop recorder (ILR) based study in hemodialysis patients—CRASH ILR (Cardio Renal Arrhythmia Study in Haemodialysis patients using Implantable Loop Recorders). The findings of this study will hopefully guide the design and implementation of larger ILR based studies before undertaking larger scale interventional therapeutic trials in this high risk population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD), even in its intermediate stages, has been shown to adversely impact on cardiovascular (CV) outcomes. Mild renal insufficiency in the Heart outcomes and Prevention evaluation (HoPe) study (serum creatinine level 125–200 μmol/l, n = 980 patients with CV disease) was associated with a 40 % increase in the risk of cardiac death when compared with those who had CV disease and normal kidney function [1]. In the presence of end stage renal disease (ESRD), the risk of CV mortality increases exponentially with sudden cardiac death (SCD) contributing to 70 % of CV mortality and 27 % of all-cause mortality in hemodialysis patients [2]. SCD is defined as an unexpected natural death from a cardiac cause within 1 h of onset of symptoms in a person not known to have a potentially fatal condition [3]. The risk of SCD increases as estimated glomerular filtration (eGFR) falls [4, 5]. In their landmark study of 19,440 CKD patients who underwent cardiac catheterisation, Pun et al. [32] demonstrated the impact of declining eGFR on SCD- this relationship was most striking when eGFR fell <60 ml/min/1.72 with a hazard ratio (HR) for each 10 ml/min/1.73 m2 decline in eGFR of 1.11 (95 % confidence interval (CI) 1.06–1.17, p < 0.001) [6].
Following renal transplantation, the general risk of SCD appears to be favourably modified, yet the risk from CV disease remains 3–5 times higher compared to the general population. Although there are no robust SCD mortality data in kidney transplant recipients, a significant number of their deaths are attributed to arrhythmia [7]. It is believed that persistent sympathetic over activity and the use of immunosuppressant drugs may play a role in the CV disease continuum [8].
This review will focus primarily on the cardiac abnormalities linked with SCD in patients with ESRD.
Sudden cardiac death—risk factors and pathogenesis
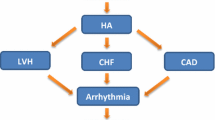
The potential risk factors for SCD in ESRD have been the subject of cardio renal research in recent years. Shared risk factors for CV disease and ESRD undoubtedly play a role in SCD in the hemodialysis population. Diabetes for example is the etiology of ESRD in 20 % of new dialysis cases [9] and is itself associated with a risk of SCD (nocturnal hypoglycaemia can cause ventricular arrhythmias via QT segment prolongation [10]). Similarly, coronary artery disease (CAD), documented in up to 50 % of post mortem studies of SCD in the general population [11] is found in 40 % of dialysis patients [12]. Coronary artery bypass grafting (CABG) or revascularisation in the hemodialysis population does not appear to remove all risk of CV mortality. In one study, all-cause and arrhythmia-related mortality in dialysis patients treated with coronary revascularisation remained high at 290 and 76 deaths per 1,000 patient years respectively [13], suggesting that the link between the two transcends above isolated myocardial ischemia and its effects.
Factors such as inter-dialytic interval (SCD being most common following a long inter-dialytic period, mode of dialysis (hemodialysis carries greater risk compared to peritoneal dialysis), composition of dialysate fluid and dialysis induced rapid fluid and electrolyte shifts (potassium, magnesium, phosphate and calcium [14]) have all been scrutinised, yet the relative importance of the various pathophysiological mechanisms that drive this phenomenon remain largely mysterious. Endothelial dysfunction, interstitial fibrosis and sympathetic over activity are some of the other factors thought to contribute to the increased risk of SCD in ESRD patients [15–18]. ECG findings such as micro T wave alternans, abnormal ventricular repolarization manifesting as QT prolongation and QT dispersion, secondary to the above, have been linked to SCD.
Hemodialysis induces changes in cardiac structure such as left ventricular (LV) hypertrophy and LV dilatation (documented in 75 and 34 % of patients respectively [19]). Independent associations have been demonstrated even between moderate renal impairment and abnormal left ventricular geometry in the absence of clinical heart failure [20]. This may be partly driven by uremic toxins such as indoxylsuplhate and p-cresylsulphate via activation of renal inflammatory and fibrotic processes seen in CV disease related to renal dysfunction [21]. These novel pathways may offer potential early intervention strategies for pre-dialysis patients by targeting the site of toxin production (colon in this case).
A recent study utilising rat models to understand the pathogenesis of ventricular arrhythmias in CKD has suggested that abnormalities in cardiac ion channel and calcium handling can increase vulnerability to early after depolarization, triggered activity and ventricular arrhythmias. In comparison with normal rats, mRNA levels of TGF-β, microRNA-21, and sodium calcium-exchanger type 1 were up regulated in CKD rats whereas the levels of microRNA-29, L-type calcium channel, sarco/endoplasmic reticulum calcium-ATPase type 2a, Kv1.4, and Kv4.3 were down regulated. Cardiac fibrosis in this setting was mild and not different between groups [22], as such this could represent the mechanism of arrhythmias in CKD prior to the onset of left ventricular wall fibrosis.
Incidence of SCD
Registry data are prone to certain inherent limitations, under reporting being one of them. This has been a concern with SCD as well and in their study, Bleyer et al. reviewed death notification forms from 1995 to 2003 in five US dialysis centres using an accepted definition of SCD. Of the 88 of 228 deaths (39 %) that could have been classified as sudden, only 59 (26 % of total deaths) were classified as sudden [14] with the remaining deaths being classified as per their etiologies—e.g. acute myocardial infarction.
Nonetheless it is encouraging to note that the 2013 annual data report from the US Renal data system [2] (the comprehensive national data system that collects, analyzes, and distributes information about ESRD in the United States) demonstrated a decline in the rate of SCD in haemodialysis patients between 2000 and 2011. The rate of SCD in hemodialysis patients fell from 72 to 49 per 1,000 patient years with the largest absolute decline occurring in those at highest risk (elderly, white race, diabetes). The reduction in SCD was most striking in patients on peritoneal dialysis where the rates fell from 62 to 36 per 1,000 patient years. These figures were much more modest in the incident dialysis population (the first 90 days of therapy, known to be a period of heightened SCD risk) with a significant difference in the incidence of SCD in hemodialysis of 7 versus 2 % in peritoneal dialysis patients, at the end of the first year.
In the light of the above, it is useful to analyse the possible explanations for this reduction in SCD. While the increased use of implantable cardioverter defibrillators (ICD) may play a role, overall they remain under utilised. Two-year mortality in dialysis patients following ICD implant still remains high (53 % following implantation for primary prevention and 58 % after implantation for secondary prevention) [2]. Of note beta blocker usage amongst dialysis patients has certainly increased and appears to contribute to the decline in mortality [2].
A further question that arises is whether SCD is as common as suggested by the US data systems. The recent UK Renal Registry annual report [23] revamped the coding system for classification of cause of death, differentiating ‘Uncertain’ and ‘Other’ causes of death and as a result, there was a substantial reduction in the proportion of patients attributed to uncertain causes of death. Subsequently in the 2011 cohort, cardiac disease was responsible for 23 % of deaths in prevalent dialysis patients, with ‘uncertain’ and ‘other’ causes of death contributing to 28 %. It is therefore possible that other catastrophic aetiologies such as intra-cerebral pathology, pulmonary emboli or aneurysms might be contributing to so-called ‘SCD’. If this is the case, the beneficial role of a routine ICD would be questionable.
Arrhythmias and dialysis
Whilst some data are available in relation to numbers of presumed SCD in the dialysis population, there is very limited literature evaluating the actual arrhythmic burden in patients with ESRD. Studies have shown the presence of repolarization abnormalities (QT prolongation, QT dispersion and abnormal T wave axis deviation) in the presence of renal impairment [24, 25] (Table 1). Holter monitoring around dialysis sessions have documented a significant burden of high grade ventricular ectopy and even non sustained ventricular arrhythmias [26, 27]. Ventricular ectopy has been extensively analysed and there appears to be no added risk secondary to the burden of ectopic activity. These studies have generally used the Lown classification for ventricular premature beats which does not take into consideration the duration of arrhythmias or additional risk factors. Thus it is plausible that the predictive value of such non-sustained arrhythmias or other ECG abnormalities recorded in the risk assessment of SCD may not have been explored adequately.
While it has been hypothesized that the process of hemodialysis per se is arrhythmogenic, intradialytic cardiac arrest is a relatively rare phenomenon. Studies have demonstrated intra-dialytic abnormal ventricular repolarization (increased QT dispersion [28] and QT prolongation) yet there has been no evidence of a direct relationship between intradialytic arrhythmias and SCD. Pun et al. in their study of 510 witnessed cardiac arrests in 43,200 hemodialysis patients, failed to show any significant risk association with the use of QT-prolonging medications and in fact demonstrated that increased ultrafiltration volumes and electrolyte abnormalities—low Ca dialysate <2.5 mEq/l [odds ratio (OR) 2.00, 95 % CI 1.40–2.90], higher corrected serum Ca (OR 1.10, 95 % CI 1.00–1.30) and increasing serum dialysate Ca gradient (OR 1.40, 95 % CI 1.10–1.80) were associated with increased risk of sudden cardiac arrest [29]. A separate study showed low potassium dialysate of less than 2 meq/l to be implicated in SCD [30]. More recently Genovesi et al. in their study of 122 hemodialysis patients were also unable to show a significant QTc variation between basal/pre-dialysis, intra dialysis and post dialysis. In their multivariate model, while all three measured QTc intervals appeared to have prognostic values for total mortality, only prolonged basal QTc and intra dialytic QTc intervals were significant predictors of SCD [31].
The risk of SCD appears to be most significant immediately before and immediately after the first weekly haemodialysis session [32, 33]. A bimodal distribution of death occurrences, with a 1.7-fold increased death risk occurring in the 12 h period starting with the dialysis procedure and a threefold increased risk of death in the 12 h before HD at the end of the weekend interval was demonstrated by Bleyer et al. [14]. These daily variations seem to be less in patients on peritoneal dialysis or home hemodialysis or even hemodialysis patients receiving more than three sessions per week [34]. It is thus plausible that the bimodal peak in risk of arrhythmias may be driven by two different types of underlying arrhythmic phenomena, such as tachyarrhythmias and bradyarrhythmias. Bradyarrhythmias secondary to conducting system disease or electrolyte abnormalities may prove detrimental either via profound bradycardia or asystole, or via bradycardia induced tachyarrhythmia.
The burden of supraventricular tachyarrhythmias in dialysis patients also remains largely undefined. Atrial ectopics and atrial fibrillation (AF) have been documented in routine ECGs and 24 h ECG recordings, with a recent meta-analysis suggesting AF prevalence of about 12 % [35] in the hemodialysis population. AF appears to be more common in the intra dialytic period [36]. This is important as AF not only increases the risk of stroke 9.8 fold [37] in the hemodialysis population but has also been identified as an independent risk factor for sudden death [38]. Stroke prevention utilising oral anticoagulants in the dialysis population remains controversial, warranting careful consideration of risks and benefits. All of the above therefore call for a better understanding of the burden of AF and paroxysmal AF in hemodialysis patients.
Therapeutic measures to prevent sudden cardiac death
Survival benefits secondary to risk factor modification remain largely unproven. Statins for example have repeatedly been shown to have no benefits on cardiovascular death, non-fatal myocardial infarction, stroke or all-cause mortality in dialysis patients despite appropriately lowering serum cholesterol [39]. This may be explained by CV disease in this population being mediated by low high density lipoproteins, chylomicrons or small dense low density lipoproteins and thus bypassing disease modifying processes mediated by statins.
Similarly erythropoietin stimulating agents, which cost $1.87 billion annually [2] in US dialysis patients have failed to decrease CV mortality and have in fact been associated with an increased risk of stroke in a large randomized controlled trial in diabetic CKD patients [40]. Active vitamin D supplementation, the second largest medical expenditure in dialysis patients, has also not been shown to reduce left ventricular hypertrophy or improve left ventricular diastolic dysfunction in these patients [41]. The EValuation Of Cinacalcet Hydrochloride Therapy to Lower Cardio Vascular Events (EVOLVE) trial evaluating the use of calcimimetics to treat secondary hyperparathyroidism in dialysis patients has not demonstrated a reduction in cardiovascular deaths either [42].
A large observational study by Foley et al. [43] indicates that beta blocker therapy has a robust association with survival in dialysis patients. Beta blockers exert asympatho-inhibitory effect, can decrease the frequency of ventricular arrhythmias, improve heart rate variability and increase baroreflex sensitivity. Sympathetic over activity is particularly linked with the diseased kidney and although beta blocker specific trials in dialysis patients are limited, data suggests they play a positive and beneficial role in the management of CV disease and reduction of mortality in this population. In a recent placebo-controlled trial of 112 HD patients with dilated cardiomyopathy, Cice et al. [44] showed that carvedilol use was linked with a significant reduction (52 vs. 73 %) in mortality. Beta blocker use at the time of a cardiac arrest in HD patients has also been associated with higher survival [45]. It is therefore encouraging to note that 58 % of current HD patients with no cardiac comorbidities are on beta blockers, as compared to 17 % in 1996–1997 [2, 46].
Implantable cardioverter defibrillators
An ICD offers a well-established interventional treatment in the reduction of SCD in patients with poor LV function or failed SCD. While guidelines do not exclude their use in ESRD patients, they remain significantly under-used. The reasons are multifold. Firstly, the evidence behind ICDs is based on trials that largely excluded those with severe CKD. It is unclear whether ventricular arrhythmias are indeed the primary cause for SCD and if so, whether as a result of concurrent electrolyte imbalances, there is a risk of intractable arrhythmias that will not respond to anti-tachycardia pacing or defibrillation. Guidelines recommend that ICDs are implanted only in those with a life expectancy of >1 year. Prognosis in ESRD is poor and the risks of infection, issues with vascular access or bleeding complications make device implantation even less inviting.
Studies have questioned the efficacy of ICDs in preventing SCD in the presence of CKD [47, 48] with conflicting results on overall mortality reduction in dialysis patients [49]. In one study, one-, two-, and three-year unadjusted survival for dialysis patients receiving an ICD after cardiac arrest were 71, 53, and 36 %, respectively, versus 49, 33, and 23 % for matched dialysis patients who did not receive an ICD [50]. Overall mortality in this study of ESRD patients was significantly higher than that reported for non-ESRD patients in the Anti-Arrhythmics versus Implantable Defibrillators (AVID) trial [51] yet the relative benefit from ICD therapy was similar (42 % reduction in overall death risk for ESRD patients versus 38 % reduction in the AVID trial). The risk of death after primary prevention ICD placement also appears to be proportional to CKD severity [52]. This is despite an increased frequency of appropriate ICD shocks documented in this population. Pun et al.’s meta- analysis of data from the Multicenter Automatic Defibrillator Implantation Trial I (MADIT-I), MADIT-II, and the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) (n = 2,867 patients of whom 36.3 % had eGFR <60 ml/min/1.73 m2) demonstrated that the survival benefit of ICDs in comparison to usual care depends on eGFR and the ICD was associated with survival benefit for patients with eGFR ≥60 ml/min/1.73 m2 (adjusted HR 0.49, 95 % posterior credible interval 0.24–0.95), but not for patients with eGFR <60 ml/min/1.73 m2 (adjusted HR 0.80, 95 % posterior credible interval 0.40–1.53) [53]. A recent meta-analysis of seven studies reporting on patients with ESRD having ICDs concluded that those receiving dialysis had a 2.7 times greater mortality compared with those not on dialysis [54].
ESRD patients have longer stays, higher in-hospital mortality and higher rates of device related complications [55], warranting careful consideration of risks vs benefits of device therapy on an individual basis. In their decision model analysis evaluating risks and benefits of ICD implantation in CKD, Amin et al. [47] demonstrated that with stages 1 and 2 CKD, ICD implantation reduces mortality. In more advanced CKD, the benefit was less significant and age-dependent—ICD implantation was favoured at ages <80 years for stage 3, ages <75 years for stage 4 and ages <65 years for stage CKD.
CRASH-ILR (Cardio Renal Arrhythmia Study in Haemodialysis patients using Implantable Loop Recorders)
Whilst one might argue for a randomised control trial of ICD therapy in dialysis patients, the mixed reports cited above as well as a number of ‘negative’ results from large scale interventional trials in ESRD might make investigators cautious about embarking on further studies in this population. There is one such study (ICD2 trial) underway, designed to evaluate the efficacy and safety of prophylactic ICD therapy in reducing SCD in 200 dialysis patients aged 55–80 years [56]. Engaging dialysis patients in interventional research is particularly challenging and it becomes essential to identify sub-populations of patients with ESRD who are most likely to benefit from an intervention. Prior to designing a trial aimed at reducing SCD, such as with ICD implantation, it is fundamental to gain an understanding of the true burden of arrhythmias (bradycardia and tachyarrhythmia) in the presence of ESRD. A 12 lead ECG only represents a snapshot of cardiac electrical activity and may be recorded when the patient is asymptomatic or between periods of abnormal arrhythmias. Conventional ambulatory ECG recording is more favourable as it provides data for 1–10 days at a time but again this could be an asymptomatic period. Event monitors require patients to have symptoms, have sufficient warning to activate the monitor and to be able to activate the monitor when symptomatic. All of these limitations would appear to be addressed by the use of implantable loop recorders (ILR) and we propose this as the next logical step in the investigation of SCD in the presence of ESRD. We feel that an enhanced understanding is fundamental to embarking on interventional studies.
We therefore designed a unique study called CRASH-ILR (Cardio Renal Arrhythmia Study in Haemodialysis patients using Implantable Loop Recorders) conducted jointly by cardiologists and renal physicians in a regional dialysis unit. In this pilot study of 30 patients we implant a new generation implantable loop recorder (ILR) (Reveal XT, Medtronic, Inc) in patients who have been on hemodialysis for more than 90 days. Demographics, history of co-morbidities, details of dialysis sessions, electrolyte levels and echocardiographic data including precise left ventricular mass measurements are recorded for each patient. Patients download data from the Reveal XT every time they dialyse (thrice weekly) via a secure mobile phone link. In >5,000 days of continuous ECG recording in pts on HD >22 % had significant events (2 patients demonstrated >3 s pauses requiring pacemaker implantation, one died from SCD and ILR interrogation identified ventricular fibrillation, one required ILR explantation due to infection and died from unrelated SCD several weeks later, one had sudden onset of atrial tachycardia requiring anti arrhythmic drugs). Patient activated recordings were all associated with sinus rhythm [57]. We aim to document >30,000 days of monitoring and thus provide insight into developing and powering a definitive study that utilises ILR technology to identify ESRD patients at high risk for SCD). Data from such a study will underpin a targeted interventional study that has a realistic chance of benefit.
Conclusion
Cardiovascular death is common in ESRD, and it has been suggested that SCD accounts for around 27 % of all-cause mortality in this population. Yet data are unclear and this may represent an overestimation. There is uncertainty regarding the arrhythmic mechanism (i.e. brady or tachy arrhythmias) as ESRD with associated neurohormonal activation and cardiac structural abnormalities serves as the perfect substrate for both of these mechanisms. Studies utilizing implantable loop recorder technology will add to our understanding of the pathophysiology and mechanisms involved in SCD and will guide the design and implementation of a larger study aimed at characterising patients at risk of developing arrhythmias.
References
Mann JFE et al (2001) Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med 134:629–636
US Renal Data System (2013) USRDS 2013 Annual Data Report. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda. http://www.usrds.org/2013/pdf/v2_ch4_13.pdf
Zipes DP, Camm AJ, Borggrefe M, Buxton AE (2006) ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation 114:e385–e484
Chonchol M, Goldenberg I, Moss AJ et al (2007) Risk factors for sudden cardiac death in patients with chronic renal insufficiency and left ventricular dysfunction. Am J Nephrol 27:7–14
Goldenberg I, Moss AJ, McNitt S et al (2006) Relations among renal function, risk of sudden cardiac death, and benefit of the implanted cardiac defibrillator in patients with ischemic left ventricular dysfunction. Am J Cardiol 98:485–490
Pun Patrick H, Smarz Thomas R, Honeycutt Emily F, Shaw Linda K, Al-Khatib Sana M, Middleton John P (2009) Chronic kidney disease is associated with increased risk of sudden cardiac death among patients with coronary artery disease. Kidney Int 76(6):652–658. doi:10.1038/ki.2009.219
Jardine AG, Gaston RS, Fellstrom BC, Holdaas H (2011) Prevention of cardiovascular disease in adult recipients of kidney transplants. Lancet 378:1419–1427
Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters K, Dietl KH, Rahn KH (2002) Sympathetic nerve activity in end-stage renal disease. Circulation 106:1974–1979
Farrington K, Rao R, Gilg J, Ansell D, Feest T (2007) New adult patients starting renal replacement therapy in the UK in 2005 (chapter 3). Nephrol Dial Transplant 22 Suppl 7:vii11–vii29
Gill GV, Woodward A, Casson IF, Weston PJ (2009) Cardiac arrhythmia and nocturnal hypoglycaemia in type 1 diabetes—the ‘dead in bed’ syndrome revisited. Diabetologia 52(1):42–45. doi:10.1007/s00125-008-1177-7
Leach IH, Blundell JW, Rowley JM, Turner DR (1995) Acute ischaemic lesions in death due to ischaemic heart disease. An autopsy study of 333 cases of out-of-hospital death. Eur Heart J 16(9):1181–1185
Foley RN, Parfrey PS, Sarnak MJ (1998) Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 32:S112–S119
Herzog CA, Strief JW, Collins AJ, Gilbertson DT (2008) Cause-specific mortality of dialysis patients after coronary revascularization: why don’t dialysis patients have better survival after coronary intervention? Nephrol Dial Transplant 23:2629–2633
Bleyer AJ, Hartman J, Brannon PC, Reeves-Daniel A, Satko SG, Russell G (2006) Characteristics of sudden death in hemodialysis patients. Kidney Int 69:2268–2273
Ritz E, Amann K, Tornig J, Schwarz U, Stein G (1997) Some cardiac abnormalities in renal failure. AdvNephrol Necker Hosp 27:85–103
Amann K, Rychlik I, Miltenberger-Milteny G, Ritz E (1998) Left ventricular hypertrophy in renal failure. Kidney Int Suppl 68:S78–S85
Amann K, Ritz E (1997) Cardiac disease in chronic uremia: pathophysiology. Adv Ren Replace Ther 4:212–224
Nishimura M, Tokoro T, Nishida M, Hashimoto T, Kobayashi H, Yamazaki S, Imai R, Okino K, Iwamoto N, Takahashi H, Ono T (2010) Sympathetic overactivity and sudden cardiac death among hemodialysis patients with left ventricular hypertrophy. Int J Cardiol 142:80–86
Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barré PE (1995) The prognostic importance of left ventricular geometry in uremic cardiomyopathy. J Am Soc Nephrol 5(12):2024–2031
Park M, Hsu CY, Li Y, Mishra RK, Keane M, Rosas SE, Dries D, Xie D, Chen J, He J, Anderson A, Go AS, Shlipak MG, Chronic Renal Insufficiency Cohort (CRIC) Study Group (2012) Associations between kidney function and subclinical cardiac abnormalities in CKD. J Am Soc Nephrol 23:1725–1734
Lekawanvijit S, Kompa AR, Wang BH, Kelly DJ, Krum H (2012) Cardiorenal syndrome: the emerging role of protein-bound uremic toxins. Circ Res 111(11):1470–1483
Hsueh CH, Chen NX, Lin SF, Chen PS, Gattone VH 2nd, Allen MR, Fishbein MC, Moe SM (2014) Pathogenesis of arrhythmias in a model of CKD. J Am Soc Nephrol. pii: ASN.2013121343
UK renal registry 16th annual report accessible from http://www.renalreg.com/Report-Area/Report%202013/08-Chap-08.pdf
Faramawi MF, Caffrey JL, Amanzadeh J, Sharpa LD, Qualls-Hampton R (2011) Cystatin C estimated renal dysfunction predicts T wave axis deviation in US adults: results from NHANES III. Eur J Epidemiol 26:101–107
Kors JA, de Bruyne MC, Hoes AW, van Herpen G, Hofman A, van Bemmel JH, Grobbee DE (1998) T axis as an indicator of risk of cardiac events in elderly people. Lancet 352:601–605
Meier P, Vogt P, Blanc E (2001) Ventricular arrhythmias and sudden cardiac death in end-stage renal disease patients on chronic hemodialysis. Nephron 87:199–214
Burton JO, Korsheed S, Grundy BJ, McIntyre CW (2008) Hemodialysis-induced left ventricular dysfunction is associated with an increase in ventricular arrhythmias. Ren Fail 30(7):701–709. doi:10.1080/08860220802212908
Howse M, Sastry S, Bell GM (2002) Changes in the corrected QT interval and corrected QT dispersion during haemodialysis. Postgrad Med J 78:273–275. doi:10.1136/pmj.78.919.273
Pun PH, Horton JR, Middleton JP (2013) Dialysate calcium concentration and the risk of sudden cardiac arrest in hemodialysis patients. Clin J Am Soc Nephrol 8(5):797–803. doi:10.2215/CJN.10000912
Pun PH, Lehrich RW, Honeycutt EF, Herzog CA, Middleton JP (2011) Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics. Kidney Int 79(2):218–227. doi:10.1038/ki.2010.315
Genovesi S, Rossi E, Nava M, Riva H, De Franceschi S, Fabbrini P, Viganò MR, Pieruzzi F, Stella A, Valsecchi MG, Stramba-Badiale M (2013) A case series of chronic haemodialysis patients: mortality, sudden death, and QT interval. Europace 15(7):1025–1033. doi:10.1093/europace/eus412
Genovesi S, Valsecchi MG, Rossi E, Pogliani D, Acquistapace I, De Cristofaro V, Stella A, Vincenti A (2009) Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol Dial Transplant 24(8):2529–2536. doi:10.1093/ndt/gfp104
Foley RN, Gilbertson DT, Murray T, Collins AJ (2011) Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med 365:1099–1107
Krishnasamy R, Badve SV, Hawley CM, McDonald SP, Boudville N, Brown FG, Polkinghorne KR, Bannister KM, Wiggins KJ, Clayton P, Johnson DW (2013) Daily variation in death in patients treated by long-term dialysis: comparison of in-center hemodialysis to peritoneal and home hemodialysis. Am J Kidney Dis. 61(1):96–103. doi:10.1053/j.ajkd.2012.07.008
Zimmerman D, Sood MM, Rigatto C, Holden RM, Hiremath S, Clase CM (2012) Systematic review and meta analysis of incidence, prevalence and outcomes of atrial fibrillation in patients on dialysis. Nephrol Dial Transplant 27(10):3816–3822. doi:10.1093/ndt/gfs416
Buiten MS, de Bie MK, Rotmans JI, Gabreëls BA, van Dorp W, Wolterbeek R, Trines SA, Schalij MJ, Jukema JW, Rabelink TJ, van Erven L (2014) The dialysis procedure as a trigger for atrial fibrillation: new insights in the development of atrial fibrillation in dialysis patients. Heart 100(9):685–690. doi:10.1136/heartjnl-2013-305417
Vazquez E, Sanchez-Perales C, Garcia-Garcia F, Castellano P, Garcia-Cortes MJ, Liebana A et al (2009) Atrial fibrillation in incident dialysis patients. Kidney Int 76:324–330
Genovesi S, Valsecchi MG, Rossi E, Pogliani D, Acquistapace I, De Cristofaro V, Stella A, Vincenti A (2009) Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol Dial Transplant 24(8):2529–2536. doi:10.1093/ndt/gfp104
Strippoli GF, Navaneethan SD, Johnson DW, Perkovic V, Pellegrini F, Nicolucci A, Craig JC (2008) Effects of statins in patients with chronic kidney disease: meta-analysis and meta-regression of randomised controlled trials. BMJ 336:645–651
Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de Zeeuw D, Eckardt KU, Feyzi JM, Ivanovich P, Kewalramani R, Levey AS, Lewis EF, McGill JB, McMurray JJ, Parfrey P, Parving HH, Remuzzi G, Singh AK, Solomon SD, Toto R, TREAT Investigators (2009) A trial of darbepoetinalfa in type 2 diabetes and chronic kidney disease. N Engl J Med 361:2019–2032
Thadhani R, Appelbaum E, Pritchett Y, Chang Y, Wenger J, Tamez H, Bhan I, Agarwal R, Zoccali C, Wanner C, Lloyd Jones D, Cannata J, Thompson BT, Andress D, Zhang W, Packham D, Singh B, Zehnder D, Shah A, Pachika A, Manning WJ, Solomon SD (2012) Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. J Am Med Assoc 307:674–684
EVOLVE Trial Investigators, Chertow GM, Block GA, Correa-Rotter R, Drueke TB, Floege J, Goodman WG, Herzog CA, Kubo Y, London GM, Mahaffey KW, Mix TC, Moe SM, Trotman ML, Wheeler DC, Parfrey PS (2012) Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med 367:2482–2494
Foley RN, Herzog CA, Collins AJ (2002) Blood pressure and long-term mortality in United States hemodialysis patients: USRDS Waves 3 and 4 Study. Kidney Int 62:1784–1790
Cice G, Ferrara L, D’Andrea A, D’Isa S, Di BA, Cittadini A, Russo PE, Golino P, Calabro R (2003) Carvedilol increases two-year survival in dialysis patients with dilated cardiomyopathy: a prospective, placebo-controlled trial. J Am CollCardiol 41:1438–1444
Pun PH, Lehrich RW, Smith SR, Middleton JP (2007) Predictors of survival after cardiac arrest in outpatient hemodialysis clinics. Clin J Am SocNephrol 2:491–500
Annual Data Report (1998) US Renal Data System: National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda
Amin MS, Fox AD, Kalahasty G, Shepard RK, Wood MA, Ellenbogen KA (2008) Benefit of primary prevention implantable cardioverter-defibrillators in the setting of chronic kidney disease: a decision model analysis. J Cardiovasc Electrophysiol 19:1275–1280
Charytan DM, Patrick AR, Liu J, Setoguchi S, Herzog CA, Brookhart MA, Winkelmayer WC (2011) Trends in the use and outcomes of implantable cardioverter-defibrillators in patients undergoing dialysis in the United States. Am J Kidney Dis 58:409–417
Robin J, Weinberg K, Tiongson J, Carnethon M, Reddy M, Ciaccio C, Quadrini M, Hsu J, Fan J, Choi P, Kadish A, Goldberger J, Passman R (2006) Renal dialysis as a risk factor for appropriate therapies and mortality in implantable cardioverter-defibrillator recipients. Heart Rhythm 3:1196–1201
Hoffmeister JM, Estes NA 3rd, Garlitski AC (2012) Prevention of sudden cardiac death in patients with chronic kidney disease: risk and benefits of the implantable cardioverter defibrillator. J Interv Cardiac Electrophysiol. 35(2):227–234. doi:10.1007/s10840-012-9711-4
Defibrillators The AntiarrhythmicsVersus Implantable, (AVID) Investigators (1997) A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 337:1576–1583
Hess PL, Hellkamp AS, Peterson ED, Sanders GD, Al-Khalidi HR, Curtis LH, Hammill BG, Pun PH, Curtis JP, Anstrom KJ, Hammill SC, Al-Khatib SM (2014) Survival after primary prevention implantable cardioverter-defibrillator placement among patients with chronic kidney disease. Circ Arrhythm Electrophysiol. pii: CIRCEP.114.001455
Pun PH, Al-Khatib SM, Han JY, Edwards R, Bardy GH, Bigger JT, Buxton AE, Moss AJ, Lee KL, Steinman R, Dorian P, Hallstrom A, Cappato R, Kadish AH, Kudenchuk PJ, Mark DB, Hess PL, Inoue LY, Sanders GD (2014) Implantable cardioverter-defibrillators for primary prevention of sudden cardiac death in CKD: a meta-analysis of patient-level data from 3 randomized trials. Am J Kidney Dis. 64(1):32–39. doi:10.1053/j.ajkd.2013.12.009
Sakhuja R, McLaughlin Gavin C, Thakur R, Bhatt DL (2009) Meta-analysis of mortality in dialysis patients with an implantable cardioverter defibrillator. Am J Cardiol 103:735–741
Aggarwal A, Wang Y, Rumsfeld JS, Curtis JP, Heidnereich PA (2009) Clinical characteristics and in-hospital outcome of patients with end-stage renal disease on dialysis referred for implantable cardioverter-defibrillator implantation. Heart Rhythm 6:1565–1571
de Bie MK, Lekkerkerker JC, van Dam B et al (2008) Prevention of sudden cardiac death: rationale and design of the Implantable Cardioverter Defibrillators in Dialysis patients trial—a prospective pilot study. Curr Med Res Opin 24(8):2151–2157
Roberts PR, Zachariah D, Borman N, Morgan JM, Yue AM, Greenwood EF, Phillips PC, Green D, Philip KA, Lewis RJ, Kalra P (2013) Abstract 10581: Cardio Renal Arrhythmia Study in Hemodialysis Patients Using Implantable Loop Recorders (CRASH-ILR). Circulation 128:A10581
Cice G, Di Benedetto A, D’Andrea A, D’Isa S, De Gregorio P, Marcelli D, Gatti E, Calabrò R (2008) Heart rate as independent prognostic factor for mortality in normotensive hemodialysed patients. J Nephrol 21(5):704–712
Suzuki M, Hiroshi T, Aoyama T, Tanaka M, Ishii H, Kisohara M, Iizuka N, Murohara T, Hayano J (2012) Nonlinear measures of heart rate variability and mortality risk in hemodialysis patients. Clin J Am Soc Nephrol 7(9):1454–1460. doi:10.2215/CJN.09430911
Oikawa K, Ishihara R, Maeda T, Yamaguchi K, Koike A, Kawaguchi H, Tabata Y, Murotani N, Itoh H (2009) Prognostic value of heart rate variability in patients with renal failure on hemodialysis. Int J Cardiol 131(3):370–377. doi:10.1016/j.ijcard.2007.10.033
Fukuta H, Hayano J, Ishihara S, Sakata S, Mukai S, Ohte N, Ojika K, Yagi K, Matsumoto H, Sohmiya S, Kimura G (2003) Prognostic value of heart rate variability in patients with end-stage renal disease on chronic haemodialysis. Nephrol Dial Transplant 18(2):318–325
Thomson BK, Momciu B, Huang SH, Chan CT, Urquhart BL, Skanes AC, Krahn AD, Klein GJ, Lindsay RM (2013) Nephron frequent nocturnal hemodialysis associates with improvement of prolonged QTc intervals. Clin Pract 123(1–2):74–82. doi:10.1159/000351382
Oktavia D, Suhardjono, Nasution SA, Setiati S (2013) The clinical factors’ prediction of increased intradialytic QT dispersion on the electrocardiograms of chronic hemodialysis patients. Saudi J Kidney Dis Transpl 24(2):274–280
Covic AC, Buimistriuc LD, Green D, Stefan A, Badarau S, Kalra PA (2013) The prognostic value of electrocardiographic estimation of left ventricular hypertrophy in dialysis patients. Ann Noninvasive Electrocardiol. 18(2):188–198. doi:10.1111/anec.12007
Poulikakos D, Banerjee D, Malik M (2014) Major arrhythmic events and T wave morphology descriptors in hemodialyzed patients. J Electrocardiol. 47(2):240–243. doi:10.1016/j.jelectrocard.2013.11.010
de Bie MK, Koopman MG, Gaasbeek A, Dekker FW, Maan AC, Swenne CA, Scherptong RW, van Dessel PF, Wilde AA, Schalij MJ, Rabelink TJ, Jukema JW (2013) Incremental prognostic value of an abnormal baseline spatial QRS-T angle in chronic dialysis patients. Europace 15(2):290–296. doi:10.1093/europace/eus306
Lee E, Fraser A, Yousef Z (2014) Prompt assessment of cardiac status following preload reduction using 12 lead ECG. Heart. 100 Suppl 3:A33. doi:10.1136/heartjnl-2014-306118.57
Thomson BK, Huang SH, Chan C, Urquhart B, Skanes A, Lindsay RM (2014) Nocturnal home hemodialysis associates with improvement of electrocardiographic features linked to sudden cardiac death. ASAIO J 60(1):99–105
Lin CY, Lin LY, Chen PC (2007) Analysis of T-wave morphology from the 12-lead electrocardiogram for prediction of long-term prognosis in patients initiating haemodialysis. Nephrol Dial Transplant 22(9):2645–2652 Epub 2007 Apr 23
Acknowledgment
CRASH-ILR is an NIHR UK porfolio supported study with an unrestricted grant from Medtronic UK.
Conflict of interest
D. Zachariah has received travel assistance from Medtronic UK. Paul R Kalra has received research grants and travel assistance from Medtronic UK. Paul R Roberts has been paid consultancy fees by Medtronic, Boston scientific and Sorin.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zachariah, D., Kalra, P.R. & Roberts, P.R. Sudden cardiac death in end stage renal disease: unlocking the mystery. J Nephrol 28, 133–141 (2015). https://doi.org/10.1007/s40620-014-0151-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-014-0151-3