Abstract
Background and objective
Urine output (UO) is routinely measured in the intensive care unit (ICU) but its prognostic value remains debated. The study aimed to investigate the association between day 1 UO and hospital mortality.
Methods
Clinical data were abstracted from the Multiparameter Intelligent Monitoring in Intensive Care II (version 2.6) database. UO was recorded for the first 24 h after ICU entry, and was classified into three categories: UO >0.5, 0.3–0.5 and ≤0.3 ml/kg per hour. The primary endpoint was the hospital mortality. Four models were built to adjust for the hazards ratio of mortality.
Results
A total of 21,207 unselected ICU patients including 2,401 non-survivors and 18,806 survivors were included (mortality rate 11.3 %). Mortality rate increased progressively across UO categories: >0.5 (7.67 %), 0.3–0.5 (11.27 %) and ≤0.3 ml/kg/h (18.29 %), and this relationship remained statistically significant after rigorous control of confounding factors with the Cox proportional hazards regression model. With UO >0.5 as the referent group, the hazards ratios for UO 0.3–0.5 and UO ≤0.3 were 1.41 (95 % CI 1.29–1.54) and 1.52 (95 % CI 1.38–1.67), respectively.
Conclusion
UO obtained on ICU entry is an independent predictor of mortality irrespective of diuretic use. It would be interesting to examine whether strategies to increase UO would improve clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urine output is routinely monitored on at least a daily basis in the intensive care unit (ICU) and it is thought to be a biomarker of acute kidney injury (AKI). According to the Risk, Injury, Failure, Loss, and End-stage kidney disease (RIFLE) and Acute Kidney Injury Network (AKIN) criteria [1, 2] as well as the recently published Kidney Disease Improving Global Outcomes (KDIGO) guidelines [3] both serum creatinine (sCr) and urine output (UO) are recommended for the staging of AKI. sCr has been extensively studied for its association with clinical outcomes, and it is well established that even a small increase in sCr can significantly predict increased risk of death [4–7]. Thus, serial measurements of sCr can help clinicians to target this group of high risk patients. However, UO has not been well established as a biomarker to predict outcome. Most studies employ RIFLE or AKIN criteria without UO (sCr alone) to define and stage AKI because precise UO is often not available [8].
For a biomarker to be of clinical importance, it should be independently associated with clinical outcome. Macedo and coworkers [9] found that UO was an early biomarker of AKI and was associated with adverse clinical outcome. Using OU, more patients would be diagnosed with AKI than by using sCr alone. However, this study was limited by its small sample size, which was subject to selection bias. More recently, Han and coworkers [10] also investigated the prognostic value of AKIN criteria with and without UO, and UO had an additional role in identifying AKI patients. Because UO is readily available even in resource limited countries, we feel that it is of vital importance to determine its role in predicting mortality. In the present study, we used the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) database to examine the association between UO and hospital mortality [11]. We hypothesized that UO on day 1 was independently associated with hospital mortality.
Materials and methods
The database
The MIMIC II (version 2.6) database consisted of more than 30,000 ICU patients admitted to various types of ICU (medical, surgical, coronary care and neonatal) in Beth Israel Deaconess Medical Center (Boston, MA, USA) from 2001 to 2008 [11]. The database categories included: general information (patient demographics, hospital admission and discharge dates), physiological variables [hourly vital signs, Simplified Acute Physiology Score (SAPS) and Sequential Organ Failure Assessment (SOFA) score], medications [intravenous (IV) medication, provider order entry data], laboratory tests (chemistry, hematology and imaging), fluid balance and notes and reports. The establishment of the database was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center and the Massachusetts Institute of Technology (Cambridge, MA, USA). Access to the database was approved after completion of the National Institutes of Health (NIH) web-based training course “Protecting Human Research Participants” by the author Z.Z. (certification number: 1132877).
Data extraction was performed using structure query language (SQL) with pgADmin PostgreSQL tools (version 1.12.3). MIMIC II was a relational database consisting of 38 tables. Data were extracted from the following tables: LABEVENTS, IOEVENTS, POE_MED, TOTALBALEVENTS, COMORBIDITY_SCORES, DEMOGRAPHIC_DETAIL, ICUSTAY_DETAIL.
Study population and definitions
Patients older than 15 years were enrolled in the present analysis. Patients without UO data on their first ICU day were excluded. Data on the following information were extracted: ethnicity, age on ICU admission, sex, body mass index (BMI) on ICU entry, Elixhauser comorbidity score, type of ICU (including coronary care, medical, surgical, and cardiac surgery care units), maximum and day 1 SOFA score and SAPS, day 1 UO, fluid balance, use of diuretics, sCr on ICU admission and before ICU admission, and use of renal replacement therapy (RRT) during ICU stay.
The primary endpoint of our study was the hospital mortality, defined as death observed during hospital stay. Patients discharged alive were considered as censored. Other study endpoints included ICU mortality, hospital length of stay, ICU length of stay, use of RRT, development of AKI, and maximum SOFA and SAPS during ICU stay. An ICU stay was a combination of one or more ICU census events that were separated by less than 24 h. For patients with more than one ICU stay, only the first ICU stay was taken into consideration. ICU length of stay was defined as the difference between date of ICU admission and ICU discharge. AKI was defined according to AKIN criteria without UO [1]. The baseline sCr was defined as the lowest sCr within 6 months before ICU admission. For patients without previous sCr available, baseline sCr was estimated using the following formula [12]: eCr = 0.74 − 0.2 (if female) + 0.08 (if black) + 0.003 × age (in years). The highest sCr during ICU stay was used to define AKI and an increase of more than 1.5 times was considered as indicating AKI. UO was observed for the first 24 h after ICU admission and it was corrected by body weight. In addition, the first 24-h fluid balance was recorded. Because diuretic use is an important confounding factor of UO, use of diuretics was considered only when the order entry time was earlier than the chart time at which the UO was recorded.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) and compared using Student’s t test or Wilcoxon rank-sum test as appropriate. Categorical variables were expressed as percentage and compared using Chi square test or Fisher’s exact test as appropriate. Unadjusted crude outcomes including hospital and ICU mortality, hospital and ICU length of stay, development of AKI, use of RRT, and maximum SOFA and SAPS scores were compared between UO categories of >0.5, 0.3–0.5, and ≤0.3 ml/kg/h. The comparison was performed using Pearson’s Chi squared test.
Hospital mortality was considered as a time-to-event variable. The event was death during hospitalization. A patient was censored when he or she was discharged alive. Patients were followed during their hospital stay. Conventional Cox proportional hazards model was fitted to adjust for the hazards ratio of mortality. Four models were created: model 1 adjusted for demographics and severity of illness; model 2 adjusted for model 1 covariates plus comorbidities, including hypertension, paralysis, chronic pulmonary diseases, diabetes, renal failure, liver disease, metastatic cancer, solid tumor and obesity; model 3 incorporated model 2 plus the use of diuretics; and model 4 included covariates in the previous three models plus AKI based on sCr on ICU entry. A stepwise backward elimination method with a significance level of 0.05 was used to build the final model [13, 14].
All statistical analyses were performed using the software STATA 11.2 (College Station, TX, USA). Two-tailed p < 0.05 was considered to be statistically significant.
Results
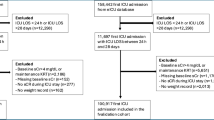
The database contained 32,655 patients, including 8,087 pediatric patients that were excluded from the current analysis. Of the remaining 24,568 adult patients, 3,048 were excluded because of missing UO data and 313 were excluded because of missing data on hospital mortality (Fig. 1). A total of 21,207 patients met our inclusion criteria, including 2,401 non-survivors and 18,806 survivors, giving a mortality rate of 11.3 %. Demographics and baseline characteristics between survivors and non-survivors are presented in Table 1. UO on day 1 was significantly lower in non-survivors than in survivors (0.524 ± 0.724 vs. 0.688 ± 0.652 ml/kg/h; p < 0.001); day 1 sCr was significantly higher in non-survivors than in survivors (1.63 ± 1.41 vs. 1.20 ± 1.31 mg/dl; p < 0.001); non-survivors were more likely to receive diuretics and RRT than survivors (8.04 vs. 1.40 % for RRT use; 11.2 vs. 8.23 % for diuretic use; p < 0.001); and more patients developed AKI among the non-survivors than among the survivors (51.04 vs. 37.06 %; p < 0.001). As expected, non-survivors had significantly greater severity of illness as represented by SOFA score (8 vs. 5; p < 0.001) and SAPS (18 vs. 13; p < 0.001); and higher comorbidity burden (median Elixhauser score: 3 vs. 2, p < 0.001) than survivors. Baseline sCr was not available in 911 patients and their baseline sCr was calculated as described above. A total of 1,027 patients had chronic kidney disease at ICU admission. Actual body weight was available for 18,357 patients, and ideal body weight was estimated for the remaining 2,850 patients. The agreement between AKI based on sCr criteria and AKI based on UO criteria within the first 24 h after ICU admission was 61.5 % (kappa = 0.21).
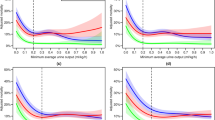
Table 2 shows crude outcomes by UO category. Patients with UO ≤0.3 ml/kg/h per hour had significantly higher hospital and ICU mortality than those with UO of 0.3–0.5 ml/kg/h or >0.5 ml/kg/h. Decreased UO on day 1 had a negative impact on other clinical outcomes including ICU mortality, ICU length of stay, hospital length of stay, development of AKI, use of RRT, maximum SAPS and SOFA score. Table 3 shows the hazards ratio (HR) of hospital mortality in the four proportional hazards models. In all analyses the referent group were patients with UO >0.5 ml/kg/h. The unadjusted HR for hospital mortality was similar in subjects with UO 0.3–0.5 ml/kg/h and UO ≤0.3 ml/kg/h After adjustment for demographics and severity of illness, the HR decreased but remained statistically significant for subjects with both UO categories. The addition of comorbidity covariates and use of diuretics to the model did not significantly alter the HR. The final model was built with the stepwise backward elimination method with a significance level of 0.05. The HRs for mortality in the final model were similar to that in model 3. With respect to patients with UO >0.5 ml/kg/h, there appeared to be a stepwise increase in HR for death going from the category of UO 0.3–0.5 (HR = 1.41) to the category of UO ≤0.3 (HR = 1.52, p < 0.001 for both). Figure 2 displays the Kaplan–Meier survival curves by UO categories, which showed that higher UO on day 1 was associated with a higher probability of survival (log-rank p < 0.001). UO measured within the first 24 h after ICU admission was of limited diagnostic value in predicting subsequent sCr elevation for AKI (area under curve 0.61, 95 % CI 0.60–0.62).
Discussion
In this analysis of a large clinical database, we found a close correlation between day 1 UO and relevant clinical outcomes such as mortality, AKI development and use of RRT. Our study provides empirical evidence that incorporating UO criteria into the definition of AKI is valid. In analogy to sCr, a small increase of which has a negative impact on clinical outcomes, the confirmation that decreased UO is significantly associated to adverse outcome will help to better define AKI. In this regard, UO can be used as an AKI biomarker for risk stratification. In contrast to other biomarkers, UO is an inexpensive and widely available method that can be applied in resource limited countries.
Many studies have focused on the diagnostic performance of UO in predicting subsequent AKI-Cr development [10, 15]. Our study shows that the initial decrease in UO is of limited diagnostic value in predicting subsequent sCr increase, which is in line with Prowle’s study [15]. These findings suggest that most episodes of decrease in UO or oliguria are not followed by renal injury. Probably, such transient oliguria is caused by hypovolemia and can be reversed with adequate resuscitation. Some authors contend that oliguria is actually a sign of renal success, and not of impending renal failure. Although this is not fully confirmed by empirical evidence, a decrease in UO is thought to be the protective mechanism of kidney in response to acute insult [16, 17]. However, we feel that it is not the AKI per se that is clinically relevant, but rather its association with the increase in morbidity and mortality that really counts. Thus, differently from previous studies, we focused specifically on the association of UO and mortality.
Several studies have been performed to validate the UO as a reliable biomarker for the definition and staging of AKI since the publication of the AKI definition by the Acute Dialysis Quality Initiative workgroup. Han et al. [10] examined the association of UO with mortality in 1,625 critically ill patients. Consistently with our finding, they found that the probability of survival was significantly different across UO categories with lower UO predicting adverse outcome. In another study involving 317 surgical ICU (SICU) patients, Macedo et al. [18] also demonstrated a linkage between oliguria and higher mortality. However, in Macedo’s study the UO was recorded hourly and subjects were classified according to the number and duration of oliguria episodes. In clinical practice, UO has to be closely monitored in order to diagnose oliguria as soon as possible and to adapt therapeutics in a reactive manner. In contrast, we classified patients into categories by the mean hourly UO in the first 24 h, and the UO was recorded once daily. Although this classification compromises the timeliness of AKI diagnosis, it is convenient and time-saving for clinical use, and most importantly it does not compromise the power of UO in discriminating non-survivors from survivors (HR 1.52, 95 % CI 1.38–1.67).
The use of diuretics may significantly influence the UO, and thus diuretic use is an important confounding factor that has been addressed in our study. Interestingly, we found that non-survivors were more likely to receive diuretics on day 1, which appears to be contradictory of the finding that lower UO is associated with adverse outcome. The finding was in line with the PICARD study which showed that diuretic use increased the risk of death or non-recovery of renal function (odds ratio OR 1.77, 95 % CI 1.14–2.76) [19]. As a matter of fact, the association between diuretic use and mortality has long been debated. Teixeira and coworkers [20] demonstrated that the use of diuretics was inversely associated with mortality, and this effect persisted after adjustment for fluid balance and UO. In the Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney), researchers failed to identify a significant association between diuretic use and mortality (adjusted OR 1.21, 95 % CI 0.96–1.5) [21]. However, observational studies are subject to allocation bias in that patents with oliguria in the initial hours after ICU admission are more likely to receive diuretics. This issue can be addressed with a more rigorous methodological design, e.g. propensity score matching and randomized controlled trials. It has been noted in many studies that a positive fluid balance is harmful to critically ill patients regarding various outcomes including mortality, oxygenation and renal function [20, 22–24]. Our study confirmed the notion by showing that survivors had significantly less fluid balance than non-survivors. The lower fluid balance in survivors can be partly explained by their higher UO. Actually, the mechanism underlying the association between decreased UO and mortality is largely unknown. One explanation is that decreased UO is associated with a more positive fluid balance, and the latter is a well-established predictor of poor outcome as mentioned previously [25–27]. However, this argument is not supported by a recent multicenter study showing that UO was independently associated with 28-day mortality after adjustment for fluid balance [20]. On the other hand, decreased UO is an indicator of impaired renal function, which in turn results in increased risk of death. Thus, it would be interesting to examine whether the use of diuretics could improve clinical outcome in a randomized controlled trial. However, since the KDIGO guidelines state that diuretics should not be used to treat oliguria or to prevent AKI [28] an alternative means to increase UO is through adequate volume resuscitation. Although the later strategy is practiced widely in most institutions for AKI caused by hypovolemia, its safety and efficacy requires further confirmation.
The strength of the present study is the large sample size that allows for the adjustment of multiple confounding factors. In the analysis, we built four models stepwise to control for potential confounding factors; and the final model was established by a backward elimination procedure. It is of paramount importance to analyze covariates in a retrospective cohort study, as is the case in the present study. Secondly, the subjects of our study came from various types of ICU, making our results applicable to heterogeneous ICU patients. However, there are several limitations that need to be mentioned. Firstly, the study is retrospective in nature and is subject to the inherent limitations of such a study design. For instance, the use of diuretics cannot be controlled because in clinical practice patients with oliguria are more likely to receive diuretics. Secondly, UO was recorded for 24 h and then divided by 24 to obtain hourly UO. Such design excluded the analysis of UO by short intervals (such as the 6-h interval recommended by AKIN). Third, mortality rate was relatively low in the present cohort, making our results less generalizable to other ICU populations. Such a low mortality rate may be attributable to the mild disease severity in our cohort (mean SOFA score: 5). Consistently with Ferreira et al. [29], a SOFA score of 5 corresponds to a mortality rate of around 10 %.
In conclusion, our study confirms previous findings that decreased UO within 24 h after ICU admission is associated with increased risk of death. Decrease in UO is also predictive of subsequent development of AKI. It would be interesting to examine whether strategies aiming to increase UO could benefit these critically ill patients.
References
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11(2):R31
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8(4):R204–R212
Kidney Disease: Improving Global Outcomes (KDIGO)—Acute Kidney Injury Work Group (2012) KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2:1–138
Cruz DN, Bolgan I, Perazella MA, Bonello M, de Cal M, Corradi V, Polanco N, Ocampo C, Nalesso F, Piccinni P, Ronco C, North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI) Investigators (2007) North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI): targeting the problem with the RIFLE Criteria. Clin J Am Soc Nephrol 2(3):418–425
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16(11):3365–3370
Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M (2004) Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 15(6):1597–1605
Praught ML, Shlipak MG (2005) Are small changes in serum creatinine an important risk factor? Curr Opin Nephrol Hypertens 14(3):265–270
Valette X, du Cheyron D (2013) A critical appraisal of the accuracy of the RIFLE and AKIN classifications in defining “acute kidney insufficiency” in critically ill patients. J Crit Care 28(2):116–125
Macedo E, Malhotra R, Bouchard J, Wynn SK, Mehta RL (2011) Oliguria is an early predictor of higher mortality in critically ill patients. Kidney Int 80(7):760–767
Han SS, Kang KJ, Kwon SJ, Wang SJ, Shin SH, Oh SW, Na KY, Chae DW, Kim S, Chin HJ (2012) Additional role of urine output criterion in defining acute kidney injury. Nephrol Dial Transplant 27(1):161–165
Saeed M, Villarroel M, Reisner AT, Clifford G, Lehman LW, Moody G, Heldt T, Kyaw TH, Moody B, Mark RG (2011) Multiparameter Intelligent Monitoring in Intensive Care II: a public-access intensive care unit database. Crit Care Med 39(5):952–960
Závada J, Hoste E, Cartin-Ceba R, Calzavacca P, Gajic O, Clermont G, Bellomo R, Kellum JA, AKI6 Investigators (2010) A comparison of three methods to estimate baseline creatinine for RIFLE classification. Nephrol Dial Transplant 25(12):3911–3918
Peduzzi PN, Hardy RJ, Holford TR (1980) A stepwise variable selection procedure for nonlinear regression models. Biometrics 36(3):511–516
Wiegand RE (2010) Performance of using multiple stepwise algorithms for variable selection. Stat Med 29(15):1647–1659
Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, Haase-Fielitz A, Kellum JA, Cruz D, Ronco C, Tsutsui K, Uchino S, Bellomo R (2011) Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit Care 15(4):R172
Legrand M, Payen D (2011) Understanding urine output in critically ill patients. Ann Intensive Care 1(1):13
Wilson WC, Aronson S (2001) Oliguria. A sign of renal success or impending renal failure? Anesthesiol Clin North America 19(4):841–883
Macedo E, Malhotra R, Claure-Del Granado R, Fedullo P, Mehta RL (2011) Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol Dial Transplant 26(2):509–515
Mehta RL, Pascual MT, Soroko S, Chertow GM, PICARD Study Group (2002) Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA 288(20):2547–2553
Teixeira C, Garzotto F, Piccinni P, Brienza N, Iannuzzi M, Gramaticopolo S, Forfori F, Pelaia P, Rocco M, Ronco C, Anello CB, Bove T, Carlini M, Michetti V, Cruz DN, for the NEFROlogia e Cura INTensiva (NEFROINT) investigators (2013) Fluid balance and urine volume are independent predictors of mortality in acute kidney injury. Crit Care 17(1):R14
Uchino S, Doig GS, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Nacedo E, Gibney N, Tolwani A, Ronco C, Kellum JA, Beginning and Ending Supportive Therapy for the Kidney (B.E.S.T. Kidney) Investigators (2004) Diuretics and mortality in acute renal failure. Crit Care Med 32(8):1669–1677
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354(24):2564–2575
Zhang Z, Zhang Z, Xue Y, Xu X, Ni H (2012) Prognostic value of B-type natriuretic peptide (BNP) and its potential role in guiding fluid therapy in critically ill septic patients. Scand J Trauma Resusc Emerg Med 31(20):86
Arikan AA, Zappitelli M, Goldstein SL, Naipaul A, Jefferson LS, Loftis LL (2012) Fluid overload is associated with impaired oxygenation and morbidity in critically ill children. Pediatr Crit Care Med 13(3):253–258
Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM, Sepsis Occurence in Acutely Ill Patients Investigators (2005) High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 128(5):3098–3108
Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K, Rasmussen MS, Lanng C, Wallin L, Iversen LH, Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen AM, Graungaard B, Pott F, Danish Study Group on Perioperative Fluid Therapy (2003) Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 238(5):641–648
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I (2005) Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology 103(1):25–32
Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV, Tolwani AJ, Waikar SS, Weisbord SD (2013) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for acute kidney injury. Am J Kidney Dis 61(5):649–672
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286(14):1754–1758
Conflict of interest
There is no conflict of interest for all authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Xu, X., Ni, H. et al. Urine output on ICU entry is associated with hospital mortality in unselected critically ill patients. J Nephrol 27, 65–71 (2014). https://doi.org/10.1007/s40620-013-0024-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-013-0024-1