Abstract
Purpose
Metastases to the thyroid gland are uncommon and they represent 1–3% of all thyroid malignancy. The aim of this study is to analyze the diagnostic problems and the role of surgery in metastatic lesions to the thyroid.
Methods
We retrospectively analyzed all patients who had undergone thyroidectomy at our Center. Out of more than 5000 thyroidectomies performed, only 9 cases had metastases to the thyroid gland.
Results
The most common primary tumor arises from kidney and lung. Non-thyroid malignancies diagnosis was obtained with US, FNAC and PET–CT. Surgery was performed in all our series (except for one case) and the expectancy of life after surgery is related to the primary tumor and comorbidities of patients.
Conclusion
The thyroid gland can be a rare site of metastases for many tumors, especially in an abnormal thyroid gland. Surgery is associated with an improved survival and the extension of surgery depends on the extension of the neoplastic lesion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastases to the thyroid gland from non-thyroid sites are uncommon but not rare. In the literature, it has been reported in only 1–3% of all patients who have surgery for thyroid malignancy. However, the rate of incidence in autopsy studies has been variable from 1.9 to 26.4% among patient dying with cancer [1, 2]. In more than 5000 thyroidectomies over a period of 11 years, only 9 cases were found to be metastases to the thyroid gland. Metastases to the thyroid gland has been reported in renal cell carcinoma (RCC), breast cancer, lung cancer, gastrointestinal malignancies, malignant melanoma, sarcoma, hematologic malignancies, and other genitourinary cancers.
The concomitance of thyroid goiter and lack of symptoms can frequently cause problems of diagnosis and treatment, which is why the rate of thyroid metastases at the clinical observation is between 0.006 and 0.3% [3].
Occasionally, symptoms of dysphagia, dyspnea, and hoarseness may be reported [1,2,3].
The aim of this study is to examine the diagnostic problems, the importance of the cytology and the role of the surgery.
Clinical records
From 2007 to 2018, we performed more than 5000 thyroidectomies, and we detected only 9 patients (7 males, 2 female) with non-thyroid metastases (0.18% among all thyroidectomies). The average age of the 9 cases at the time of diagnosis of the thyroid metastases was 68 years (range 48–87 years old).
The thyroid metastases were identified on average 39.5 months (range 2–96 months) after surgery of the primary tumor. This interval was longest in patients with kidney cancer and shortest in patients with lung cancer. In anamnesis, four patients were treated with nephrectomy, two patients with pulmonary lobectomy, one patient with pneumonectomy, one patient with Miles surgery, and the last one with mastectomy.
The clinical presentation in seven cases was a neck indolent node of parenchymatous consistency and mobile with swallowing. In two cases, patients presented clinical symptoms as dysphonia and cough.
The thyroid mobility was preserved towards surface and deep layers: this is an evidence that tumor is limited to the thyroid tissue. All patients were euthyroid: TSH, FT3, and FT4 levels were normal.
The preoperative investigations included ultrasonography (US), fine-needle aspiration cytology (FNAC) and positron emission tomography (PET). These diagnostic studies were performed because patients presented new palpable nodule in the neck or enlargement of the thyroid gland. We did not study serology pre-operative because it was unnecessary for the outcome of the patients. In our series, US findings in seven cases showed a diffuse hypoechoic lesion mimicking a diffuse goiter and in two cases, a hypoechoic nodular lesion with low vascularization. All cases underwent a preoperative FNAC: the cytological diagnosis was correct for metastases in six cases. In three cases, the FNAC suspected a primary thyroid tumor.
Six patients have undergone PET–CT (positron emission tomography–computed tomography) that showed focal area of increased activity in the thyroid gland. Close to the principle area, it was possible to see smaller areas with lower tracer uptake; these areas may probably have a lymphatic origin (Fig. 1). In our series, the pre-operative investigations were led by the result of the FNAC. Therefore, we performed PET–CT to exclude possible metastases in other sites in six patients with cytological diagnosis of non-thyroid malignancies (NTM). If metastases were present in other sites, we would not propose thyroidectomy because the long-term survival would not change. Three patients did not undergo PET–CT because the diagnosis of the FNAC was primary thyroid tumor.
Eight patients were treated with total thyroidectomy. In one case, concomitant latero-cervical lymph node involvement was found and the cytologic findings suggested a primitive thyroid tumor. In this case, we performed neck dissection. Only one patient did not undergo surgery because of comorbidities and short life expectation; this patient had undergone pneumonectomy in the past.
Histological reports showed that four patients had metastases from kidney tumor (RCC), three patients had metastases from lung carcinoma, one patient had metastases from rectum adenocarcinoma, and one patient had metastases from breast carcinoma.
Overall survival was lower among patients with colo-rectal (6 months) and lung cancers (6, 8, and 12 months, respectively). These malignancies often have a more aggressive clinical course than breast (60 months) and renal (10, 36, 48 and 72 months) cancers. One patient with RCC died after 10 months because of other comorbidities and one with RCC is still alive after 72 months (Table 1).
Discussion
The incidence of thyroid cancer has continuously increased over the last decade thanks to new diagnostic tools like US improvement; however, metastases to the thyroid gland are still a rare event. The prevalence of secondary thyroid tumor has been reported to be from 1 to 3% of all malignant tumors to the thyroid [1, 2]. In 2017, Zhang et al. reported that the non-thyroid malignancies (NTM) were present only in 0.3% of all thyroid malignancies and these data are in accordance with our results (0.18%) [3].
In 1931, Willis proposed two hypotheses to explain the low rate of thyroid metastases: fast arterial flow through the thyroid discourages adhesion of malignant cells and the high oxygen saturation and iodine concentration of the thyroid gland inhibit the growth of malignant cells [4]. However, the most important theory is still the proposal of Botson in 1940 and it is based on venous by-pass between paravertebral and neck vein that skips the pulmonary circulation. This event is still rare [5].
A number of studies support that multinodular goiter or a pathological situation of the thyroid can induce the neoplastic cells implant from other organs [6, 7]. If the hypotheses of Willis are correct, pathological thyroid glands with reduced blood flow and lower iodine concentrations should be more susceptible to metastases [4]. In a series by Heffess et al., 42% of patients with thyroid metastases from non-thyroid malignancies were noted in glands with adenomas or thyroiditis [8]. In our series, seven patients had goiter that means an abnormal thyroid gland.
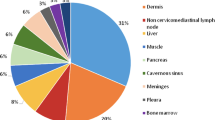
More than half of the patients with distant metastases operated in our study had metastases from kidney and lung (seven patients) and this is in accordance with the literature data [5, 6, 9]. The most common sources of metastases to the thyroid are kidney, followed by lung and breast. Somewhat less frequently, NTM can originate from the gastrointestinal tract, melanomas, and the genitourinary tract. In 2016, Russel et al. performed a literature review including all NTM from 1994 to 2013 and 17 new cases. They reported 818 patients with NTM and the most common primary site of NTM was kidney and then lung cancer. Colorectal cancer represents one of the most common cancers in human pathology; however, metastases to the thyroid are relatively rare, only 10.4% of all NTM originate from the colon [10]. In our series, one patient had NTM that originate from the colon, with relatively short survival time: 6 months following thyroid surgery.
The way of spread for esophagus, larynx, and pharynx tumors is contiguity penetration, for breast and lung tumors is retrograde lymphatic way, and for kidney and gastro-intestinal tumors is hematic spreading. Squamous cell carcinoma from the head and neck region is a rare primary tumor and can be an example of direct extension and metastasis involvement of the thyroid gland. Vatsyayan et al. reported a total of 36 patients with NTM metastases from SCC and presented a treatment algorithm to avoid local recurrence of the tumors [11].
The other share opinion concerns if the NTM could change the functionality of the thyroid. In 2016, Chung et al. considered 170 reports that indicate how the thyroid function was with NTM and most of the patients were euthyroid (87.6%) [7]. Hypothyroidism was related to massive infiltration of the thyroid by a malignant tumor; Shimaoka et al. reported that hypothyroidism required months to be manifest after massive replacement of the thyroid gland [1]. When thyrotoxicosis occurs, it is likely due to the leakage of the hormones into peripheral blood resulting from damage to the thyroid gland by neoplastic embolization. In our series, all the patients were euthyroid.
Diagnosis of thyroid metastasis is sometimes difficult because of lesions that are mostly asymptomatic and can develop in a goiter simulating a primary tumor. In the literature, most of patients presented clinical symptoms such as new or enlarging thyroid nodule, neck swelling, dysphagia, dysphonia, hoarseness, and cough [10].
The best diagnostic tool to study the thyroid gland is ultrasonography although no single mentioned feature is decisive to describe thyroid metastases. Previous reviews in the literature reported that the typical US findings of metastases to the thyroid gland consist of hypoechoic nodules with ill-defined margins and intra-nodular vascularization [12]. Other authors pointed out that the US findings of NTM show a diffuse goiter with heterogeneously hypoechoic or isoechoic echogenicity and internal hypoechoic lines in a “reticular pattern” [13, 14]. Saito et al. classified thyroid metastases into two categories based on the US findings: diffuse type represents diffuse hypoechoic lesions involving the entire thyroid gland and nodular type represents hypoechoic nodular lesions in the thyroid with low vascularization [15]. Our report was in accordance with this division in two possibilities because we found not only diffuse hypoechoic lesions in most of our patients but also, in two cases, nodular lesions as presentation of NTM.
Fine-needle aspiration cytology is an important tool in the diagnosis of thyroid pathology, and it can help to avoid useless thyroidectomy in patients with a poor prognosis [16]. The data collected must be combined with anamnesis to solve diagnostic doubts. However, FNAC may not ensure the definitive diagnosis in all cases. The most common NTM for which FNAC did not make the correct diagnosis were esophagus, cervix, RCC and malignant melanoma. The highest percentage of correct diagnoses in NTM was encountered from breast, lung, and colorectal cancer. FNAC do not yield a definitive diagnosis in all cases, it has been reported as incorrect in 24% of thyroid metastasis cases [7]. In our series, three cases (33%) were misdiagnosed with FNAC: the report suggested a papillary thyroid carcinoma in two cases instead of RCC and, in the last case, a low differentiate thyroid cancer was suspected instead of colo-rectal cancer. As reported in the literature, RCC is associated with most frequently diagnostic errors on FNAC because of the cytological features commonly overlap with primary thyroid neoplasm. Immunocytochemical analysis could help pathologist in differential diagnosis; especially, positive immunostaining for thyroglobulin suggests a primary thyroid malignancy [18].
In our cases, it is difficult to evaluate if thyroidectomy is useful. However, in our opinion, there are some reasons to try a surgical approach like the necessity to have a differential diagnosis between a primitive or a secondary thyroid tumor and the necessity to avoid tracheal stenosis. Moreover, if the thyroid localization is unique and secondary to differentiated tumor consistent with a good life expectancy, we suggest thyroid surgery. Russel et al., in his review, have shown that the survival time is longer in the patients who had undergone thyroid surgery, especially in patients with NTM from RCC [10].
There are different opinions about the correct extension of thyroid metastases surgery. Jesalnieks et al. reported the clinical course in 45 patients undergoing thyroid surgery for NTM from RCC. Although no statistical difference had been observed regarding overall survival between total and subtotal thyroidectomy, this review suggests that total thyroidectomy should always be attempted to avoid thyroid recurrences in patients with multiple, small, and bilateral lesions. The thyroid recurrences developed in all cases of thyroidectomy with positive resection margins [19, 20].
Another review reports that no patients had tumor recurrence when margins were negative and total thyroidectomy was not associated with a better survival compared to thyroid lobectomy [21].
In agreement with our opinion, the extension of surgery must give complete excision of the metastases [7, 22]. We consider surgery useful when the thyroid tumor is the only metastatic lesion and the expectancy of life is good. In our experience, metastasis from kidney tumor has the best outcome, as reported in the literature [6, 10, 23]. We always performed total thyroidectomy because in our series, NTM were bilateral or there were the suspicious of thyroid cancer. It is, therefore, difficult to make definitive conclusions about the correct extension of surgery even if, in our experience, total thyroidectomy is preferable (Table 2).
Conclusions
When a thyroid nodule is detected, in a patient with a prior history of malignancy, before taking any decision, it is important to study this nodule using the necessary diagnostic tools like US, FNAC and PET to exclude if it is a NTM, other possible metastases and verify the possibility to obtain radicality with thyroid surgery.
If there are the findings of other metastases and thyroid is not the only organ involved and the patient has a short expectancy of life, the only reason to perform surgery is to obtain a tracheal decompression and so give a better quality of life to the patient.
References
Shimaoka K, Sokal JE, Pickren JW (1962) Metastatic neoplasms in the thyroid gland. Pathol Clin Find Cancer 15(3):557–565
McCabe DP, Farrar WB, Petkov TM, Finkelmeier W, O'Dwyer P, James A (1985) Clinical and pathologic correlations in disease metastatic to the thyroid gland. Am J Surg 150(4):519–523
Zhang L, Liu Y, Li X, Gao W, Zheng C (2017) Metastases to the thyroid gland: a report of 32 cases in PUMCH. Medicine 96(36):e7927
Willis RA (1931) Metastatic tumours in the thyroid gland. Am J Pathol 7(3):187
Boston OV (1940) The function of the vertebral veins and their role in the spread of metastasis. Ann Surg 122:138–140
Zivaljevic V, Jovanovic M, Perunicic V, Paunovic I (2018) Surgical treatment of metastasis to the thyroid gland: a single centre experience and literature review. Hippokratia 22(3):137
Chung AY, Tran TB, Brumund KT, Weisman RA, Bouvet M (2012) Metastases to the thyroid: a review of the literature from the last decade. Thyroid 22(3):258–268
Heffess CS, Wenig BM, Thompson LD (2002) Metastatic renal cell carcinoma to the thyroid gland: a clinicopathologic study of 36 cases. Cancer Interdiscip Int J Am Cancer Soc 95(9):1869–1878
Wood K, Vini L, Harmer C (2004) Metastases to the thyroid gland: the Royal Marsden experience. Eur J Surg Oncol (EJSO) 30(6):583–588
Russell JO, Yan K, Burkey B, Scharpf J (2016) Non thyroid metastasis to the thyroid gland: case series and review with observations by primary pathology. Otolaryngol Head Neck Surg 155(6):961–968
Vatsyayan A, Mandlik D, Patel P, Sharma N, Joshipura A, Patel M, Sanghvi KJ (2019) Metastasis of squamous cell carcinoma of the head and neck to the thyroid: a single institution’s experience with a review of relevant publications. Br J Oral Maxillofac Surg. 57(7):609–615
Nixon IJ, Coca-Pelaz A, Kaleva AI, Triantafyllou A, Angelos P, Owen RP, Ferlito A (2017) Metastasis to the thyroid gland: a critical review. Ann Surg Oncol 24(6):1533–1539
Papi G, Fadda G, Corsello SM, Corrado S, Rossi ED, Radighieri E, Pontecorvi A (2007) Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol 66(4):565–571
Kim HK, Kim SS, Oak CY, Kim SJ, Yoon JH, Kang HC (2014) Diffuse metastasis to the thyroid: unique ultrasonographic finding and clinical correlation. J Korean Med Sci 29(6):818–824
Saito Y, Sugitani I, Toda K, Yamada K, Fujimoto Y (2014) Metastatic thyroid tumors: ultrasonographic features, prognostic factors, and outcomes in 29 cases. Surg Today 44(1):55–61
Kim TY, Kim WB, Gong G, Hong SJ, Shong YK (2005) Metastasis to the thyroid diagnosed by fine-needle aspiration biopsy. Clin Endocrinol 62(2):236–241
Pastorello RG, Saieg MA (2019) Metastases to the thyroid: potential cytologic mimics of primary thyroid neoplasms. Arch Pathol Lab Med 143(3):394–399
Mirallié E, Rigaud J, Mathonnet M, Gibelin H, Regenet N, Hamy A, Kraimps JL (2005) Management and prognosis of metastases to the thyroid gland. J Am Coll Surg 200(2):203–207
Calzolari F, Sartori PV, Talarico C, Parmeggiani D, Beretta E, Pezzullo L, Misso C (2008) Surgical treatment of intrathyroid metastases: preliminary results of a multicentric study. Anticancer Res 28(5B):2885–2888
Iesalnieks I, Winter H, Bareck E, Sotiropoulos GC, Goretzki PE, Klinkhammer-Schalke M, Raab M (2008) Thyroid metastases of renal cell carcinoma: clinical course in 45 patients undergoing surgery. Assessment of factors affecting patients' survival. Thyroid 18(6):615–624
Beutner U, Leowardi C, Bork U, Lüthi C, Tarantino I, Pahernik S, Müller SA (2015) Survival after renal cell carcinoma metastasis to the thyroid: single center experience and systematic review of the literature. Thyroid 25(3):314–324
De Ridder M, Sermeus AB, Urbain D, Storme GA (2003) Metastases to the thyroid gland—a report of six cases. Eur J Intern Med 14(6):377–379
Chen H, Nicol TL, Udelsman R (1999) Clinically significant, isolated metastatic disease to the thyroid gland. World J Surg 23(2):177–181
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article not contain any studies with human participants or animals.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Battistella, E., Pomba, L., Mattara, G. et al. Metastases to the thyroid gland: review of incidence, clinical presentation, diagnostic problems and surgery, our experience. J Endocrinol Invest 43, 1555–1560 (2020). https://doi.org/10.1007/s40618-020-01282-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01282-w