Abstract
Background
Approximately 10% of non-communicable diseases (NCDs) can be attributed to hypertension. The prevalence of hypertension is steadily increasing among urban, rural, and tribal populations alike. There has been a growing incidence of hypertension within underprivileged groups; however, there is a scarcity of research focusing on the risks of hypertension within Indian tribes. The current study aimed to estimate the pooled prevalence of hypertension among tribes and the risk factors of hypertension.
Methods
This study uses data from the fifth phase of the National Family Health Survey (NFHS-5) in India, covering 2,843,917 individuals in 636,699 households. A total of 69,176 individuals belonging to tribal communities aged between 15 and 49, encompassing both males and females, have been incorporated into our study. The study utilized bivariate and multivariable binary logistic regression analyses, which were conducted using the R statistical software.
Results
Among 69,176 tribal populations between 15 and 49 years, the overall prevalence of hypertension was 12.54% (8676/69176; 95% CI, 12.29%, 12.79%). The prevalence of hypertension among males was 16.4% and 12.07% among females. Age, gender, education, marital status, smoking, and alcohol consumption were found to be the significant predictors of hypertension among tribes.
Conclusion
The rising prevalence and potential dangers of hypertension within Indian tribes highlight their epidemiological transition burdened by significant cardiometabolic health concerns, necessitating prompt and ongoing monitoring and surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is a prominent public health concern that is increasingly prevalent within diverse ethnic groups and traditional communities residing in middle-income countries [1, 2]. An estimated 71% of the global mortality rate is attributed to non-communicable diseases (NCDs), which claim the lives of over 40 million individuals annually [3]. According to the Global Burden of Disease (GBD) study, cardiovascular diseases (CVD) have been identified as the primary cause of mortality and morbidity [4]; also, as estimated, hypertension was responsible for approximately 1.63 million deaths in 2016, which is significantly higher than the 0.78 million deaths that had been reported in 1990 [5].
Non-communicable diseases (NCDs) in both developed and developing nations have reached epidemic proportions. Non-communicable diseases (NCDs) account for more than 70% of mortality and contribute to more than 50% of the global disease burden. A combination of cardiovascular diseases (CVDs), carcinomas, respiratory illnesses, and stroke accounts for approximately 44% of premature non-communicable disease (NCD) deaths and nearly 80% of cardiovascular disease (CVD)–related deaths. Globally, hypertension impacts more than 25% of the populace. Worldwide, hypertension is acknowledged as the third leading cause of death across all age groups. In India, stroke is responsible for 57% of mortality cases related to stroke and 24% of mortality cases pertaining to coronary heart disease [6].
There are more than 370 million indigenous individuals living in 90 distinct nations, accounting for roughly 5% of the worldwide population [7]. India is home to the largest indigenous population globally, with an estimated count of 104 million individuals, constituting approximately 8.6% of the nation’s overall population [8]. The indigenous population in India is officially referred to as tribal people and categorized as scheduled tribes.
Diabetes and hypertension are the most prevalent non-communicable diseases (NCDs), and their shared association with several comorbidities negatively impacts adherence to treatment, contributing to poorer health outcomes, lowered quality of life, and premature mortality [9].
Hypertension can be diagnosed and treated with proper medication. Early detection, treatment, and management can reduce hypertension-related health problems [10]. Inadequate treatment of diabetes and hypertension has major implications on the health outcomes of individuals and its financial burden on communities [11]. The majority of hypertensives, especially in tribal communities, are undiagnosed and, therefore, never receive treatment. Therefore, it is imperative to evaluate and emphasize the increasing prevalence of hypertension within indigenous communities in India. The primary objective of our study was to estimate the prevalence of hypertension within the Indian tribal population by utilizing nationally representative data obtained from the National Family Health Survey-5(2019).
Materials and Methods
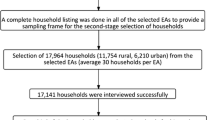
The data employed in this analysis was acquired from the fifth iteration of the National Family Health Survey (NFHS-5), a survey conducted at the household level in India between 2019 and 2021. The survey is designed to be nationally representative. The National Family Health Survey-5 (NFHS-5) implemented a sampling strategy involving two stratification stages. The sampling methodology employed in the initial stage varied between rural and urban regions within each district. In rural settings, villages were designated as the primary sampling units (PSUs) and were selected by applying probability proportional to size (PPS) methodology. Conversely, census enumeration blocks (CEBs) were employed as the PSUs in urban areas and were chosen using probability proportional to size systematic sampling. Following the completion of the mapping and household listing process for the specified primary sampling units (PSUs), a total of 22 households were chosen through the utilization of systematic random sampling in both rural and urban PSUs. The survey encompassed a total of 707 districts spanning 28 states and eight union territories in India. The successful interviews encompassed a population of 2,843,917 individuals residing in 636,699 households. Among the total population of 2,843,917 individuals, a count of 2,078,315 adults aged 15 years and older was recorded. The survey encompassed a sample size of 135,239 women and 17,729 men belonging to tribal communities who were interviewed. An extensive exposition of the sampling methodology and instruments employed in the survey has been provided elsewhere [12].
Inclusion criteria were as follows: tribal men and women aged 15 to 49 with three systolic and diastolic measurement and/or medication details.
Exclusion criteria were as follows: Those who refused to participate in blood pressure measurement and had missing data in covariates were excluded from the study. Following our inclusion criteria, a total of 69,176 tribes were included in the study (Fig. 1).
Outcome Variables
The current investigation operationalized hypertension as having a systolic blood pressure equal to or exceeding 140 mm Hg and/or a diastolic blood pressure equal to or exceeding 90 mm Hg. In addition, an individual is classified as having hypertension if he/she responded yes to “currently taking medications for hypertension.”
Predictor Variables
To study the factors influencing hypertension, the baseline variables used in the bivariate and multivariable regression analysis included sociodemographic and behavioral characteristics. The sociodemographic variables included a wealth index calculated from a standard set of interviewer-observed assets divided into five categories (quintiles), namely, poorest, poorer, middle, richer, and richest. We included age in years (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49), gender (male/female), place of residence (urban/rural), occupation (employed/unemployed), and marital status (unmarried/living with partner/separated). Level of education was categorized into four groups: no education (no formal education), primary (1–5 years of schooling), secondary (6–12 years of schooling), and higher (> 12 years of schooling). Behavioral characteristics include smoking (yes/no), alcohol (yes/no), and how often they consume alcohol, and it was classified into almost every day, about once a week, less than once a week, and none.
Results
Table 1 shows the characteristics of the tribal population. Majority of the participants were females (89%), living in rural (86%) and employed (62%). Seventy-one percent were living with partners, 43% were from the poorest wealth index, and the majority were non-smokers and non-drinkers, with 98% and 93%.
Among 69,176 tribal populations between 15 and 49 years, the overall prevalence of hypertension was 12.54% (8676/69176; 95% CI, 12.29%, 12.79%). The prevalence of hypertension among males was 16.4% and 12.07% among females. The mean (standard deviation) and median (interquartile range) age among males are 30.62 (9.85) and 30 (22–39), and among females are 30.46 (9.79) and 30 (22–38) respectively.
Our results revealed, the state-wise percentage of hypertension among the tribal population was noted in Andaman and Nicobar with 29.41% (5/17; 95% CI, 7.75%-51.07%), followed by Sikkim with 27.12% (32/118; 95% CI, 19.09–35.14%), and the lowest was noted in Puducherry and Chandigarh with 0% followed by Rajasthan with 7.56% (433/5730; 95% CI, 6.87–8.24%) and DNH and DD with 8.57% (9/105; 95% CI, 3.22–13.93%) respectively (Fig. 2).
The prevalence of hypertension among males at 15 and 49 years of age was 4.13% (9/218; 95% CI 1.49%, 6.77%) and 27.34% (38/139; 95% CI, 19.93%, 34.75%). Similarly, the prevalence of hypertension among females at 15 and 49 years of age was 2.81% (61/2169; 95% CI, 2.12%, 3.51%) and 30.09% (340/1130; 95% CI, 27.41, 32.76), respectively (Fig. 3).
Risk Factors Associated with Hypertension
Table 2 shows the logistic regression analysis performed for not hypertensive and hypertensive between 15 and 49 years with sociodemographic and behavioral characteristics. Individuals with 20–24 years (cOR 1.55; 95% CI 1.35, 1.78), 25–29 years (cOR 2.27; 95% CI 1.99, 2.60), 30–34 years (cOR 3.61; 95% CI 3.17, 4.11), 35–39 years (cOR 5.02; 95% CI 4.43, 5.68), 40–44 years (cOR 7.42; 95% CI 6.53, 8.43), and 45–49 years (cOR 9.71; 95% CI 8.58, 11.00) are having higher odds of being hypertensive compared to 15–19 years of age. Males (cOR1.43; 95% CI 1.28, 1.59) are having higher odds of being hypertensive compared to females. Those who live in urban settings (aOR 1.28; 95% CI 1.16, 1.42) have higher odds of being hypertensive compared to those who live in rural settings. Individuals with no education (aOR 1.82; 95% CI 1.58, 2.09) and primary education (aOR 1.43; 95% CI 1.22, 1.67) have higher odds of being hypertensive compared to those with higher education.
In adjusted analysis, increasing age has a strong association with hypertension. Males (aOR 1.26; 95% CI 1.05, 1.51) are having higher odds of being hypertensive compared to females. Individuals who smoke cigarettes (aOR 1.29; 95% CI 1.01, 1.65) have higher odds of being hypertensive than non-smokers. Compared to those who do not consume alcohol, those consuming alcohol (aOR 1.23; 95% CI 1.04, 1.44) have higher odds of being hypertensive.
Compared to the unemployed, those employed have higher odds of being hypertensive (cOR 1.77; 95% CI 1.57, 2.00). Compared to those who are unmarried, living with a partner (cOR 2.65; 95% CI 2.41, 2.91), and separated (cOR 4.57; 95% CI 4.00, 5.22) have higher odds of being hypertensive. Individuals with richer (cOR 1.19; 95% CI 1.08, 1.32) and the richest (cOR 1.45; 95% CI 1.23, 1.70) wealth index have higher odds of being hypertensive compared to the poorest.
Compared to non-smokers and non-alcohol drinkers, smokers (cOR 1.92; 95% CI 1.58, 2.34) and alcohol drinkers (cOR 1.98; 95% CI 1.80, 2.16) have higher odds of being hypertensive. Individuals who consume alcohol almost daily (cOR 1.95; 95% CI 1.55, 2.45) have higher odds of being hypertensive than to those who do not consume alcohol.
Discussion
In terms of global mortality, high blood pressure is a major contributor, killing some 9.4 million people yearly due to its association with cardiovascular disease [13]. The prevailing belief was that indigenous populations had lower susceptibility to lifestyle diseases such as hypertension, attributed to their unique cultural practices and customs. This elucidates the rationale behind the disparate findings observed in studies examining the prevalence of hypertension among indigenous populations across different states in India. Obtaining a precise prevalence estimate for the Indian tribal population poses difficulties due to the population’s extensive diversity and heterogeneity.
The current study aimed to determine the prevalence of hypertension among the scheduled tribes of India. The results of the investigation revealed a prevalence rate of 12.54%. According to the findings of a recent systematic review and meta-analysis, the prevalence of hypertension among the tribal population in India is estimated to be 16.7% [14]. In 2014, Rizwan et al. [15] conducted a meta-analysis that yielded a pooled estimate of hypertension prevalence at 16.1%. The data indicates a consistent upward trend in the prevalence of hypertension within the tribal population in recent years.
The global distribution of hypertension exhibits variations among different ethnic groups. According to a research study conducted on various ethnic groups in Sudan, it was found that the prevalence of undiagnosed hypertension was 49.4%. Additionally, approximately 41% of the population exhibited prehypertension [16]. The findings of a research investigation carried out on indigenous tribes in Malaysia revealed that the incidence of hypertension was 25.5% [17]. The prevalence of hypertension in Thasongyang, Thailand, was found to exceed 27%. Among this group, 15% were identified as hypertensive, while 12% were classified as prehypertensive [18].
Andaman and Nicobar exhibited the highest prevalence of hypertension, at 29.41%, according to the findings. Sikkim, in close proximity, exhibited a prevalence rate of 27.12%. In contrast, the regions of Puducherry and Chandigarh exhibited the lowest reported rates of hypertension, with no documented cases of the condition. Rajasthan demonstrated a comparatively diminished prevalence rate of 7.56%. Numerous studies undertaken in Kerala have reported a prevalence of hypertension spanning from 40 to 48% [19, 20], thereby signifying a substantial incidence of this pathological state among the populace. Kandpal et al. [21] documented a prevalence rate of 43.4% in Himachal Pradesh, whereas Raina et al. [22]. documented a prevalence rate of 12.9% in Uttarakhand.
Among indigenous communities, there exists a notable resemblance to both urban and rural settings. The results of our study suggest that the prevalence of hypertension is 15% among urban tribes and 12% in rural tribes. Several studies reported that the prevalence of hypertension among tribes in rural areas varies from 5.75 to 50.76% [23, 24], and the prevalence of hypertension among tribes in urban areas ranges from 16.40 to 30.81% [25]. The study reveals that modernization and acculturation increase hypertension incidence, with lower prevalence in rural India due to geographical diversity. Migration and urbanization contribute to increased blood pressure due to lifestyle changes. Rural-to-urban migration increases demand for housing, clean water, sanitation, healthcare, and public amenities, resulting in a higher demand for essential services and infrastructure.
Our study revealed that hypertension increases with age. The prevalence of hypertension among males at age 15 was 4.13%, and age 49 was 27.34%. The study found a positive correlation between age and hypertension prevalence, with females having a prevalence of 2.81% at 15 and 30.09% at 49 and males having a prevalence of 4.13 at 15 and 27.34% at 49. Several studies confirm that hypertension increases with age [26,27,28]. It may be due to arterial stiffening, increased vascular resistance, lifestyle factors, and hormonal changes.
In our study, compared to non-smokers and non-alcohol drinkers, smokers (cOR 1.92; 95% CI 1.58, 2.34) and alcohol drinkers (cOR 1.98; 95% CI 1.80, 2.16) have higher odds of being hypertensive. Individuals who consume alcohol almost daily (cOR 1.95; 95% CI 1.55, 2.45) have higher odds of being hypertensive compared to those who do not consume alcohol. The Global Adult Tobacco Survey (GATS) shows a tobacco prevalence of 10.38% in India, with smokeless tobacco usage at 21.38%. Tobacco use is present in 28.6% of adults, with 14.2% of women and 42.4% of men being current users, contrasting the overall prevalence [29].
Murmu et al. [30] emphasize the significant social determinants and burden of tobacco use among India’s tribal population. Several studies have confirmed smoking has been significantly associated with hypertension [23, 31, 32].
Alcohol consumption was reported by an estimated 7% of the participants in the current study. A statistically significant correlation was observed between alcohol consumption and an elevated risk of hypertension, as determined by a study by Meshram et al. [19]. The relative risk was 1.4 (95% CI 1.17–1.73). Furthermore, our research findings indicate that alcohol consumption plays a substantial role in the onset of hypertension among the tribal populations of India. This discovery is supported by previous studies that have established the detrimental effects of alcohol intake on hypertension [32,33,34].
Limitations
Nevertheless, this study had several limitations. The dataset’s cross-sectional nature precludes any possibility of drawing causal inferences. Additionally, the analysis included only participants within particular age ranges, namely, individuals aged 15 to 49 years, encompassing both men and women. Hence, the conclusions drawn from the study lack generalizability to the broader tribal population in India. The investigation was limited to a sample size of 69,176 individuals from tribal communities due to insufficient data on systolic and diastolic measures, as well as incomplete medication information. Therefore, hypertension might be either overestimated or underestimated. Approximately half of the tribal participants in the study exhibited a missing value for the outcome variable. It is possible that this subgroup may possess distinct probabilities of experiencing hypertension, as well as other factors influencing hypertension, compared to the individuals included in the analysis. Unfortunately, the analysis conducted in this study was unable to examine the impact of behavioral risk factors, such as nutrition and physical inactivity, due to the unavailability of relevant data in the dataset.
Conclusion
The prevalence of hypertension is on the rise among tribal populations. There was a positive correlation observed between advancing age and the occurrence of hypertension. There was a statistically significant association seen between hypertension and various demographic factors, including education level, literacy status, marital status, gender, employment status, residence, and wealth index. The phenomenon of urbanization, together with the resulting lifestyle changes within the broader socioeconomic framework, acculturation, and marginalization, is a significantly interconnected and indicative variable contributing to the prevalence of lifestyle diseases among Indian tribes. The condition is predominantly asymptomatic and necessitates early intervention to mitigate its potential long-term consequences. Our investigation has revealed that hypertension is becoming a noteworthy health issue within the tribal population. It is imperative to enhance the capacity of health services to prioritize the evolving health requirements, particularly pertaining to hypertension and its correlated risk factors.
Data availability
Data sharing is not applicable to this article as no datasets were generated during the current study. The National Family Health Survey-5 datasets are available on the DHS platform: https://dhsprogram.com/data/.
References
Giri PP, Mohapatra B, Kar K. Prevalence of hypertension and the associated factors among Sabar and Munda tribes of Eastern India. J Family Med Prim Care. 2022;11(9):5065–71.
Chakma T, Kavishwar A, Sharma RK, Rao PV. High prevalence of hypertension and its selected risk factors among adult tribal population in Central India. Pathog Glob Health. 2017;111(7):343–50. https://doi.org/10.1080/20477724.2017.1396411.
Non-communicable diseases. https://www.who.int/newsroom/factsheets/detail/noncommunicable-diseases. Accessed 21 Dec 2023.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cCardiovascular dDiseases and Rrisk Ffactors, 1990–2019: Uupdate Ffrom the GBD 2019 sStudy. J Am Coll Cardiol. 2020;76(25):2982–3021.
Gupta R, Gaur K, S. Ram CV,. Emerging trends in hypertension epidemiology in India. J Hum Hypertens. 2019;33(8):575–87. https://doi.org/10.1038/s41371-018-0117-3.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
United Nations. State of the world’s indigenous peoples: education. 2017. https://www.un.org/development/desa/indigenouspeoples/news/2017/12/state-of-the-worlds-indigenous-peoples-iiieducation. Accessed 21 Dec 2023
Office of Registrar General & Census Commissioner India. Census info. ministry of home affairs G of India. 2011. Available from http://www.censusindia.gov.in/2011census/HLO/HH14.html.
Patil M, Hedaoo RP, Shah RP, Tauseef SM, Marzo RR, Ching SM, Lambert G. Assessment of health-related quality of life among male patients with controlled and uncontrolled hypertension in semi urban India. Inquiry: J Health Care Organization, Provision, and Financing, 2023;60:00469580231167010
Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Ccontrol of Hhypertension: JACC health promotion series. J Am Coll Cardiol. 2018;72(11):1278–93.
Biswas A, Singh RK, Singh SK. Medical and non-medical cost of hypertension and heart diseases in India. Cogent Soc Sci 2016;2(1):1250616. Available from https://doi.org/10.1080/23311886.2016.1250616.
International Institute for Population Sciences (IIPS) and ICF. National family health survey (NFHS-5), 2019–21. India: 2021; Volume 1. Mumbai: IIPS.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223 /pmc/articles/PMC7998524/.
Babu B V., Hazarika CR, Raina SK, Masoodi SR, Basappa YC, Thomas N, et al. Hypertension prevalence, awareness, treatment, control and risk factors in tribal population of India: a multi-centric cross-sectional study. J Racial Ethn Health Disparities. 2023; https://doi.org/10.1007/s40615-023-01817-w
Rizwan SA, Kumar R, Singh AK, Kusuma YS, Yadav K, Pandav CS. Prevalence of hypertension in Indian tribes: a systematic review and meta-analysis of observational studies. PLoS one. 2014;9(5):e95896.
Noor SK, Elsugud NA, Bushara SO, Elmadhoun WM, Ahmed MH. High prevalence of hypertension among an ethnic group in Sudan: implications for prevention. Ren Fail. 2016;38(3):352–6. https://doi.org/10.3109/0886022X.2015.1128839.
Chua EY, Zalilah MS, Haemamalar K, Norhasmah S, Geeta A. Obesity indices predict hypertension among indigenous adults in Krau Wildlife Reserve, Peninsular Malaysia. J Health Popul Nutr. 2017;36(1):24. https://doi.org/10.1186/s41043-017-0102-4.
Aung MN, Lorga T, Srikrajang J, Kreuangchai S, Tonpanya W, Jaiin P, et al. Assessing awareness and knowledge of hypertension in an at-risk population in the Karen Assessing awareness and knowledge of hypertension in an at-risk population in the Karen ethnic rural community , Thasongyang , Thailand. 2022; https://doi.org/10.2147/IJGM.S29406
Meshram I, Arlappa N, Balkrishna N, Rao K, Laxmaiah A, Brahmam G. Prevalence of hypertension, its correlates and awareness among adult tribal population of Kerala state, India. J Postgrad Med. 2012;58(4):255 https://www.jpgmonline.com/article.asp?issn=0022-3859;year=2012;volume=58;issue=4;spage=255;epage=261;aulast=Meshram.
Sajeev P, Soman B. Prevalence of noncommunicable disease risk factors among the Kani tribe in Thiruvananthapuram district. Kerala Indian Heart J. 2018;70(5):598–603.
Kandpal V, Sachdeva MP, Saraswathy KN. An assessment study of CVD related risk factors in a tribal population of India. BMC Public Health. 2016;16(1):1–8. https://doi.org/10.1186/s12889-016-3106-x.
Raina SK, Chander V, Prasher CL, Raina S. Prevalence of hypertension in a tribal land locked population at high altitude. Scientifica (Cairo). 2016;2016(4000 m):1–9.
Ganie MA, Parvez T, Viswanath SA, Sreenivas V, Ramakrishnan L, Nisar S, Sahar T, Robbani I, Ali SA, Rashid A, Wani IA. Prevalence, pattern & correlates of hypertension among tribal population of Kashmir, India: a cross-sectional study. Indian J Med Res. 2024;154(3):467–75.
Manimunda SP, Sugunan AP, Benegal V, Balakrishna N, Rao MV, Pesala KS. Association of hypertension with risk factors & hypertension related behaviour among the aboriginal Nicobarese tribe living in Car Nicobar Island, India. Indian J Med Res. 2011;133(3):287 (/pmc/articles/PMC3103153/).
Borah PK, Devi U, Biswas D, Kalita HC, Sharma M, Mahanta J. Distribution of blood pressure & correlates of hypertension in school children aged 5–14 years from North east India. Indian J Med Res. 2015;142(3):293 (/pmc/articles/PMC4669864/).
Id IVK, Id NS, Bandawe C, Kohler H peter. PLOS GLOBAL PUBLIC HEALTH Aging and hypertension among the global poor — panel data evidence from Malawi. 2022;1–19. https://doi.org/10.1371/journal.pgph.0000600
Ramakrishnan S, Zachariah G, Gupta K, Shivkumar Rao J, Mohanan PP, Venugopal K, et al. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309–13 https://www.scopus.com/inward/record.uri?eid=2-s2.0-85074098839&doi=10.1016%2Fj.ihj.2019.09.012&partnerID=40&md5=6bbb6088fd0eaf64d4e61724e18f11d1.
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170 (/pmc/articles/PMC4011565/).
Rai B, Bramhankar M. Tobacco use among Indian states: key findings from the latest demographic health survey 2019–2020. Tob Prev Cessat. 2021;7.
Murmu J, Agrawal R, Manna S, Pattnaik S, Ghosal S, Sinha A, Acharya AS, Kanungo S, Pati S. Social determinants of tobacco use among tribal communities in India: evidence from the first wave of longitudinal ageing study in India. Plos One. 2023;18(3):e0282487.
Priyadarsini S, Kumari S, Chandra P, Lakra K, Charan S, Dhawan P, et al. Association of tobacco with hypertension in adult females : evidence from National Family Health Survey-IV for an aspirational Indian state. Clin Epidemiol Glob Health. 2022;15:101061. https://doi.org/10.1016/j.cegh.2022.101061.
Anand N, Hussain S. Prevalence of hypertension & associated risk factors among tribal population in a rural community of Katihar. J Evol Med Dent Sci. 2020;9(23):1725–30.
Ray J, Som K, Paul R, Bandyopadhyay D. Prevalence of alcohol use among tribal population based on self-reported data: a hospital-based pilot study from West Bengal. J Indian Acad Clin Med, 2018;19:269–73.
Singh PK, Dubey R, Singh L, Singh N, Kumar C, Kashyap S, Subramanian SV, Singh S. Mixed effect of alcohol, smoking, and smokeless tobacco use on hypertension among adult population in India: a nationally representative cross-sectional study. International Journal of Environmental Research and Public Health, 2022;19(6):3239.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chinnaiyan, S., Dharmaraj, A. & Palanisamy, B. Prevalence and Associated Risk Factors of Hypertension Among Tribal Population Aged 15–49 in India: Evidence from National Family Health Survey, 2019–2021. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02005-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02005-0