Abstract
Introduction
In general, church attendance can be associated with improved health behaviors and fewer related chronic diseases, suggesting a potential opportunity to counteract worsening health behaviors among some immigrants and thereby reduce health disparities. There is a paucity of research, however, on the relationship between religious involvement and immigrants’ health behaviors and whether it varies by host or home country context.
Aim
To examine the relationship between religious involvement, measured by church attendance, with health behaviors among Latino immigrants in the United States (U.S.) and to compare the relationship of home and host country attendance with these behaviors.
Methods
Data from the randomized New Immigrant Survey, including over 1200 immigrants to the U.S. from Mexico and Central America, were analyzed. Health measures included smoking, binge drinking, physical activity, and obesity. Descriptive and multivariate logistic regression analyses were performed using measures of church attendance and ethnic/immigrant characteristics as well as other demographic and health care factors. Separate models were constructed for each behavior.
Results
An association was found between U.S. church attendance and less smoking, less drinking, and greater physical activity but not with obesity. Threshold effects were found. However, almost no associations were found between health behaviors and home country church attendance.
Conclusion
The context in which people live warrants increased attention for successful health promotion initiatives for immigrant populations. The social, psychological, and religious resources in immigrant communities can be leveraged to potentially counteract worsening of chronic disease-related health behaviors of Latino immigrants in the U.S., thereby reducing health disparities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Chronic diseases are responsible for a large majority of deaths and health care costs in the United States (U.S.) [1] and fall disproportionately on lower income populations such as immigrants [2]. Modifiable health behaviors such as smoking, drinking, physical activity, and nutrition can significantly reduce chronic disease risk [2], yet health behaviors in the U.S. are still suboptimal and can vary by population. Although individual responsibility to live a healthy lifestyle and manage chronic disease is often emphasized, this paper suggests that consideration of religious involvement and its context can potentially make initiatives to encourage healthier behaviors among immigrants more successful.
A growing body of research has found a generally protective effect of religion in terms of both mortality and morbidity [3, 4]. Religion influences population health through mediating religious individuals’ lifestyle [5, 6], especially when reinforced by a religious community [7]. Specific religious beliefs can have generally, although not consistently, protective health benefits, in that they can promote wellness and help prevent or manage disease [5, 8,9,10,11]. Religious proscriptions and prescriptions can affect behaviors such as smoking, alcohol abuse, nutrition, and exercise [5, 8, 9, 12, 13]. However, while prior research has generally found a relationship between greater religiosity and better health behaviors, such a relationship has not always been found, especially for the health behavior-related outcome of obesity [4, 9, 14,15,16].
Most studies examine either the relationship of ethnicity and immigration with health [17,18,19] or religion with health [4, 12, 13, 20] without exploring the overlapping associations among these factors and their implications for improving health. Health disparities exist among Latino immigrants especially in terms of chronic diseases, which can be related to health behaviors [21]. If religion is associated with improved health behaviors, it can then potentially play a role in reducing these health disparities. There is at least some evidence supporting such a relationship between religion and health behaviors among Latino immigrants [8, 19, 22, 23]. However, earlier studies have typically focused on a limited number of behaviors or limited populations. In addition, to our knowledge, there are no earlier studies that have compared the impact of both home and host country religiosity on health behaviors despite potentially differing impacts of each, as described below.
Conceptual Framework
While the causal factors for the religion-health connection among immigrants are not fully understood, key mechanisms can include social, psychological, and religious factors. An overall protective effect of religion can be found in terms of both reduced mortality and morbidity, although there can be negative influences of religion on health as well. A range of religious dimensions and measures has been used in research but the strongest evidence of an association between religion and health is through participation in a religious group as measured by congregational attendance [4, 24].
Increased social capital has been associated with improved health outcomes so belonging to a religious community can be expected to have a positive influence on health just as with participation in any group [25,26,27,28]. There is an especially large quantity of social capital in religious communities and Putnam has written that religion is the largest source of social capital in the United States [27]. Not only is there are a large quantity of social capital in religious communities but the quality of this social capital can also be greater as the mechanisms by which social capital can improve health, such as trust and reciprocity, can work especially well in the context of a religious community. For example, friends in a religious community can have a more beneficial impact than friends in other settings [29].
Psychological mechanisms can also play a role in explaining the religion-health connection. Personality characteristics can be related to religious beliefs and at the same time can also affect health. For example, the effects of compassion, often emphasized by religions, are believed to mediate the association between religious involvement and health outcomes [30] and volunteering, often associated with religiosity, can improve preventive health of the volunteers themselves [31, 32]. Religion can also affect health status through religious coping, such as the ability to psychologically deal with an illness [32]. Participation in a religious community can aid coping through a number of mechanisms including providing comfort and emotional support [4, 12, 32]. Religiosity can also help prevent mental health disease [11].
Religion is not merely a set of social activities or psychological constructs, however, but is based on critical underlying ideas from oral and written traditions that affect attitudes and influence behaviors related to health outcomes. There are distinctive aspects of religion, such as theology, rituals, and meaning, that can impact health. For example, the idea of the sacred, belief in a transcendental being, and religious rituals are elements that distinguish religion from other social phenomena and can affect health [5]. Further, many of the links of religiousness with health, well-being, and social behavior may be due to religion’s influences on self-control or self-regulation [32, 33]. Distinctive beliefs and practices of religion itself, such as discouraging smoking or encouraging vegetarianism, can affect health [3,4,5, 11]. These have been given less attention than social or psychological resources or are sometimes even attributed to these other mechanisms [4, 34]. I use the term religious capital to describe these distinctive elements of religion, based on the work of Iannacone [35].
It is important to stress that religious involvement does not always have a positive impact on health. Some religious beliefs and behaviors can harm health. As Portes makes clear, social capital can be negative as well as positive [36]. When group beliefs discourage healthful behaviors or encourage harmful behaviors, pressures to conform can have a negative impact and the social environment can be harmful. Religious struggles can cause stress to health if one feels abandoned by their religion, in contrast to others in the community, leading to negative coping with illness [37]. Religious beliefs may also discourage use of health care services [4, 11].
Religion, Immigrants, and Health
Religious and ethnic identities are often intertwined; compared to other organizations, the communal form of religious practice such as participation in religious institutions can play an especially important role in the lives of Latino and other immigrants [38,39,40,41]. For example, Portes and Rumbaut have written that immigration by Mexicans to the U.S. is permeated at every step by the presence of religion [39]. While religion plays a very important role in Latin America, functions of congregations in each country may vary for immigrants because churches in their host country may serve many integrative and supportive functions that may not have been needed in their home country [28, 39, 41]. Religious institutions often are the initial point of entry for immigrants into U.S. society and serve multiple functions, with potentially important implications [28, 41]. They can be an especially important source of social capital for new immigrants and often provide networks with other congregants or linkages to other communities of similar ethnicity [41].
The role of religion is important for Latino immigrants in the U.S. A Pew survey found that about 60% of them are Catholic, 16% Evangelical Protestant, and 15% unaffiliated, with the remainder primarily belonging to other Christian denominations [42]. In addition to changes in the roles of churches for Latino immigrants, there also may be changes in religious identity and attendance. As with U.S.-born Latinos, there is a trend towards fewer Latino immigrants identifying as Catholic and more identifying as Evangelical Protestant or not affiliating; about a sixth of Latino immigrants change their religion since moving to the U.S. There is also evidence of changes in frequency of attendance at religious services among immigrants [43]. The large majority of Latino immigrants still attend church, with about 40% of Latino immigrants who are Catholics and 71% of those who are evangelical report attending church at least weekly [42].
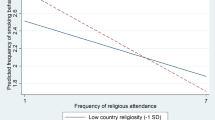
Globalization is not homogenization and the country in which religious involvement takes place is important. While in general, the role of religious involvement for individuals can be expected to vary, depending on whether it occurs in the home or host country, characteristics of the specific country of residence also matter. There is evidence that the relationship between more frequent religious services attendance and better health status varies among countries by contextual as well as individual factors, with it being stronger when the extent of religiosity in a country is greater [44]. There is research that suggests that the migration process is a disruptive event in someone’s life affecting the role of religion in it [43] and contextual factors such as religious pluralism and different concentrations of religion in countries can influence whether someone attends religious services [45]. Further, the contexts of receiving and sending of migrants can differ. Arriving in a new country where one may be a minority and less likely to be integrated into society may change the role that religion plays in one’s life [28, 39,40,41].
There are policy implications to the potentially different roles or religion in home and host countries. Religious institutions often serve multiple functions beyond religious roles for immigrants, including health- and welfare-related ones [28, 39,40,41]. As a result, there may be special opportunities for faith-based interventions for Latinos and other immigrants in their new country. While most of the literature for faith-based interventions has focused on African-American churches [46, 47], there is evidence of successful faith-based health promotion initiatives for Latinos as well [48].
For all these reasons, the contextual factors of religious involvement and where this involvement takes place can potentially affect and have an impact on outcomes such as health behaviors. However, while the existence of a connection between religious involvement and health behaviors in general is well established, its connection for immigrants has been understudied. Further, despite the evidence cited, there has been virtually no research examining how the impact of religious involvement, such as church attendance, on the health of a particular ethnic group may vary depending on whether the context is home or host country, despite concomitant implications for immigrants’ health. This study aims to help fill that gap in knowledge.
Research Objectives
-
1.
To examine the relationship between religious involvement and health behaviors for Latino immigrants in the U.S. I hypothesized that greater religious involvement will be associated with decreased smoking, drinking, and obesity and with increased physical exercise because of the large quantities of faith-based social, psychological, and religious resources.
-
2.
To examine whether any associations found between congregational attendance and current health behaviors for these immigrants vary between attendance in the host country, the U.S., and attendance in their home/prior country. I hypothesized that the relationships between religious involvement and health outcomes will be positive and stronger for host than home country church attendance, particularly because immigrants may have special needs that churches in the U.S. help meet because of their resources and differing roles.
Methods
The study analyzed the New Immigrant Survey (NIS), a random-sample national survey of immigrants to the United States, unique in being a nationally representative survey of new legal immigrants with permanent residence in the U.S. The survey sample drew a randomized sample stratified by immigration type. The survey strata were as follows: spouses of U.S. citizens, employment principals, diversity principals, and other immigrants. The target NIS sampling frame was 12,500 and the response rate was 69% yielding an overall sample of over 8500 from all sample home countries. Data were collected in 2003.
All data used in the study are based on responses to a questionnaire administered to the sample. Face to face interviews with immigrants were conducted in their preferred language, including Spanish and English. The survey administered includes questions on health status, health behaviors, height and weight, religion, immigration, language, income, occupation, education, housing, family, age, and sex, as well as several other demographic categories.
The survey received approval from the Princeton University Institutional Review Board.
The study population was first-generation immigrants from Mexico and Central America 18 and over who self-identify as Christian. Immigrants who had moved to the United States within 6 months of survey administration were excluded, since they were unlikely to have yet established their regular church-going pattern. The sample size was 1232 (weighted = 1525).
The primary outcomes of interest were health behaviors: smoking, binge drinking, physical activity, and obesity, commonly used as indicators of a healthy lifestyle; there is substantial evidence linking these behaviors to health and well-being, especially because of their links to chronic disease and other types of morbidity [2, 49]. Smoking was measured by categorization as current smoker or non-smoker; smoking can affect health in numerous ways, especially as a cause of cancer [50]. Drinking was measured by whether, in the last 3 months, the respondent had four or more alcoholic drinks at least once. Moderate drinking may be protective for some conditions such as cardiovascular disease; as a result, binge drinking, which can lead to stroke and other health problems [51], was chosen as a more useful measure for the sample. Respondents were asked about how often they participated in “light activities such as walking, dancing, bowling, gardening, etc.” and how often the respondent participated in “vigorous physical exercise such as aerobics, running, swimming or bicycling.” Physical activity level was categorized as follows: no exercise, participation in light activity but not vigorous exercise, or participation in vigorous exercise. Physical activity level can affect health status in multiple ways and these categories of physical activity have been used in earlier studies associating exercise and health status [52]. Respondents were categorized as obese if they had a BMI of 30 or more, the World Health Organization criterion. Although obesity is not a health behavior, it is strongly linked with the health behavior of nutrition for which there were no adequate measures in the survey, as well as being associated with increased morbidity [2]; limitations to use of this measure are described below.
Religious involvement was measured through church attendance, both in the U.S. and in the respondents’ home country. Each measure was calculated based on the number of times the respondent attended church and categorized as none if never attended, occasional if attended but less than weekly, and regular if attended weekly or more. Denominational affiliation was also included. Immigrant and ethnicity-related variables included country of birth, number of years in the U.S., level of English proficiency, and visa type.
Control variables include age, gender, marital status, household size, education, occupation, income, education, geographic location, health insurance, number of doctor visits, and whether they had a usual source of care.
Descriptive and multivariate analyses using logistic regression were performed for all health outcomes. Variables were included in the final model for each measure if they had a p value less than .05. Some variables were included on a prespecified theoretical basis, including U.S. church attendance, prior country church attendance, religious denomination, country of birth, age, and gender.
A statistical tolerance analysis was performed to examine covariability between variables. No tolerance was below the threshold of 20%, which would have indicated a covariability issue. Most variables had less than 1% of the data missing, and the only variable for which more than 10% of the data was missing was income, with 29%. In this case, missing data was imputed for the variable, prior to being added to the model, using multiple imputations to improve variance and standard error estimates.
Data Availability
The dataset used is publicly available through nis.princeton.edu. Further details about the survey as well as a partial list of publications using the dataset are available on the website.
Results
Descriptive statistics for health and demographic variables for the sample are in Table 1. The sample population was largely under 50 years of age and a small majority was female. Respondents had low socioeconomic status with roughly two thirds having less than 12 years of education and a similar percentage having average income below $20,000. Over three quarters of the sample was married or lived with a partner. There was substantial variation in health outcomes measures. The sample had suboptimal health behaviors as measured by smoking, binge drinking, physical activity level, and obesity. Almost half of respondents were in less than very good health.
Descriptive statistics for religion and immigration variables are listed in Table 2. Almost 20% of the sample attended church regularly in the U.S., at least once a week or more, while 27% never attended church. The remainder went to church occasionally. In terms of home country church attendance, the majority attended at least weekly but only 6% never attended church in their prior country. The sample was predominantly Catholic, 83%, while 5% listed themselves as Orthodox, 5% as Evangelical-Pentecostal Protestants, and the rest as other Protestant denominations.
As indicated in Table 2, the study population was predominantly Mexican, 65% of the sample, with 25% Salvadoran and 10% Guatemalan, so that there was a diversity of ethnicities in the sample. The majority of the sample had been in the U.S. between 5 and 14 years and had limited English proficiency.
Next, multivariate models were built for each outcome measure. Based on the criteria described above, all final models included the following: age, gender, U.S. church attendance, prior country church attendance, denomination, and country of birth for all four models. The smoking model (whether the respondent is a current smoker) also included doctor visits. The drinking model (whether the respondent drank four or more alcoholic drinks at least once in the last 3 months) also included English proficiency, region of residence, and health insurance status. The physical activity model (whether the respondent has performed no, light, or vigorous activity) also included English proficiency, region of residence, and education. The obesity model (whether the respondent has a BMI of 30 or more) also included education.
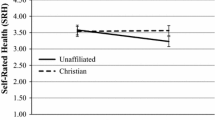
Adjusted odds ratios for all comparisons were calculated from the final model estimates. Standard errors and confidence intervals were produced for all variables. Table 3 provides a summary of the study’s findings about the relationship between church attendance and health behaviors when controlling for other religious, immigrant, and demographic variables. U.S. church attendance was associated with a positive outcome for three of the four behaviors: current levels of smoking, physical activity, and binge drinking (only marginally significant at p < .06).
The results were consistent with hypotheses about the relationship of religious involvement with positive health behaviors. Effect sizes found were typically modest, with the exception of smoking. Despite the low incidence and small cell sizes, smoking was the only measure with double digit odds of non-church attenders being more likely to smoke than regular church attenders. The directions of the effects were as predicted, with regular churchgoers always having better outcomes than those who never attended church. There was a threshold effect in that the occasional attenders always had similar results to the non-attenders or the regular attenders, never in between as would be the case if there was a dose-response relationship. However, the specific threshold varied by health behavior (Table 2).
For binge drinking, there was no difference between those who never attended church and those who attended occasionally; a connection between attendance and binge drinking was found only among those who attended regularly. In the case of physical activity and smoking, however, the threshold for a relationship between church attendance and positive outcomes was occasional attendance as both occasional and regular church attendance were associated with lowered odds of smoking and increased odds of physical activity, relative to non-attendance. No statistically significant association was found between church attendance and obesity, although the effect was in the predicted direction.
In contrast to U.S./host country church attendance results, however, only physical activity, among the four outcomes studied, was associated with home/prior country church attendance at a statistically significant level (Table 4). Even in that case, the strength of the association was weaker than that for U.S. attendance and there was not the same threshold effect.
It is possible that home country church attendance had a weaker association with health behaviors because of extensive time elapsing since immigration, so that any impact had worn off or been crowded out by more recent U.S. church attendance. To address this concern, several sensitivity analyses were run for the models, including only more recent immigrants who had arrived within the last year, within the last 2 years, and within the last 3 years. The models were also rerun excluding U.S. church attendance from the model. In all of these additional analyses, similar results were still found, with little association between home country religious involvement and current health behaviors.
Discussion
The findings of an association between current host country church attendance and positive outcomes for three of the four health-related outcomes tested are consistent with and lend further support to the principal literature summarized at this paper’s outset of a generally but not consistently positive relationship between religious involvement and health behaviors. The findings of lower smoking and binge drinking rates among the religiously involved support the conceptual framework that guided the study, as well as previous studies linking religiosity with lower rates of risky behaviors [4, 14]. In addition, the findings are consistent with mechanisms such as social group or leadership influences in a religious community limiting deviance from denominational teachings and proscriptions against smoking and drinking [8, 53].
Church attendance was also associated with physical activity, a protective behavior in that it typically improves health. The reasons for this association are less obvious than those for smoking and drinking. Different mechanisms may come into play in influencing such protective behaviors as exercise compared to risky behaviors which can harm health. In addition, certain physical activities may be part of church life, such as walking to mass, and results are consistent with some, although not all, literature about physical activity among religious Latinos in the U.S. [54, 55].
Obesity was the only outcome measure analyzed for which U.S. church attendance was not associated with a positive outcome. This is generally consistent with prior literature, which did not show positive associations between religiosity and obesity, sometimes even finding negative ones [4, 15, 16]. While reasons for this study’s finding are unclear, unmeasured variables may confound the relationship between obesity and church attendance, such as genetics, social networks, family influences, or especially nutrition, for which there was no good NIS survey measure.
There was a much weaker relationship found between home country church attendance and current health behaviors, however, with an association found only with physical activity. Results differed between home and host country attendance even for this health behavior, with differences in strength of results and in threshold effects. The weak relationship between religious involvement and health behaviors in the sample was true even when only focusing on more recent immigrants.
These findings help deepen our knowledge of the relationship between religiosity and health behaviors. While prior studies provide evidence of a generally positive connection between them [4], understanding how the relationship may vary depending on whether one is attending church in one’s home country or the country one has migrated to is a contribution of this study to the body of literature.
Differences in the impact of attending church between home and host country may account for the differences found in the relationships between religious involvement and home or host country. The context of reception in one’s new country and related need for assistance with integration and resources may interact with the social and psychological benefits and the religious capital that church attendance can provide. Differences in degree of country religiosity, alternative forms of social capital, or government actions among countries may also affect health. In addition, the impact of church attendance on health after migration may vary because of other contextual factors in specific countries. As noted, there is evidence that the relationship between subjective health and religious services attendance varies among countries because of contextual factors, including those related to religion [44].
There are important public policy implications to the findings as faith-based programs can help reduce health disparities among immigrant and other minority populations [23, 46]. A leading hypothesis for the association found between poorer health and longer residence in the U.S. among many Latino immigrants is worsening health behaviors related to chronic diseases because of acculturation [17, 19, 56]. Conversely, this study found that church attendance was associated with improved health behaviors. While not recommending that people start attending church to improve their health, many Latinos already attend church and not all of them refrain from smoking and drinking or are physically active [19, 28]. As a result, there is an opportunity to counteract the phenomenon of worsening health behaviors through faith-based initiatives targeting churchgoers with suboptimal heath behaviors, potentially reducing chronic-disease related inequalities.
The study’s findings can be of great value in creating or enhancing health promotion initiatives for Latino churchgoing populations in the U.S. on a more systematic basis. Although many churches sponsor health-related programs, the majority do not. Furthermore, it is those churches serving the poor and vulnerable, groups in which immigrants are disproportionately represented, that are least likely to offer such programs [57]. Faith-based health behavior interventions have potential among Latinos [48] and a focus on religious traditions as part of the intervention has the potential to improve prevention not just care [58]. Interventions can be developed and implemented to take advantage of faith-based opportunities in potentially addressing the problem of worsening health among immigrants as they reside longer in the U.S. and thereby reduce health disparities of Latinos [48, 54, 59]. In addition, Latino religious leaders should be encouraged to take a more active role in improving the health of their congregants, thereby increasing their adoption of successful initiatives found among other vulnerable populations [46, 60]. A church’s lay leadership and other congregants should also be involved in any initiative as encouragement from fellow church members can have a major impact on a healthy lifestyle [61].
Key Limitations/Additional Research
The data are based on the sample’s answers to survey questions asked, with the usual potential limitations to the validity or reliability of subjective responses. Further, because the data are cross-sectional, we cannot reject the hypothesis that people with healthier behaviors are likelier to want to attend church. However, there is no evidence of this. In addition, if this were the reason for findings, it is unclear why only churches in the U.S., but not in Latin America, would be likely to attract regularly attending congregants with healthier behaviors.
It is possible that results could vary using more recent surveys of immigrants but to our knowledge none exist with all the relevant data and with a similarly high level of validity. Further, the study’s primary objective was to understand the intersection of key contextual factors such as religion, ethnicity, and migration on health behaviors, rather than to measure the exact prevalence of specific behaviors. The topic of this research has been greatly understudied and there is no theoretical reason to expect that the nature of these relationships would have changed substantially since the data was collected so the results from this study can still make an important contribution despite any limitations.
There was no adequate measure of overall nutrition in the survey. Although not a heath behavior itself, obesity was used both because of its connection to chronic diseases and because it is strongly influenced by nutrition. However, this measure was limited in its use as a proxy for nutrition because there are other factors which may also be determinants of obesity, including genetics.
The hypothesis that only those with adequate functional status attend church cannot be ruled out. However, over 85% of the study sample is under age 50; therefore, physical capability is unlikely to be an important explanatory factor for variations in attendance.
Whereas the survey was very extensive and many factors were included in the analyses, some potential confounding variables were omitted from the survey. In particular, it would have been helpful to include social measures outside of those for family and religious community. Further, there was only a limited number of religion-related questions asked in the survey. Questions about congregational characteristics, reasons why people attended services, home religious practice, and whether the congregation offered any health-related programs would have been useful.
This study could not fully answer questions related to underlying reasons for findings of relationships between church attendance and specific behaviors. Additional research is needed to better understand the mechanisms by which church attendance can affect health, such as through intensive interviews with church leaders and congregants. Analyses using congregational information together with the individual-level data in the survey would also be of value. Whereas this study only examined health behaviors, it would also be useful to examine the relationship of religious involvement with other health outcomes such as individual chronic diseases that may be linked to these health behaviors.
Conclusion
Religious involvement has an important place among factors related to Latino immigrant health and an opportunity exists to reduce health disparities for Latino immigrants through church-based interventions to improve health behaviors. Regular church attendance was associated with positive outcomes for three of the four health-related outcomes studied. However, these associations were primarily found for host but not home country church attendance, consistent with the idea that host country churches, such as in the U.S., play a special role in immigrants’ lives, that can impact health. These findings are important not only for the study’s aims but because of their implications for policy and interventions as well as to guide future research.
References
Center for Communicable Diseases. Chronic disease and health promotion. 2017. http://www.cdc.gov/chronicdisease. Accessed 4 December 2017.
World Health Organization. Noncommunicable diseases factsheet. 2017. http://www.who.int/mediacentre/factsheets/fs355/en/. Accessed 4 December 2017.
Ellison C, Levin J. The religion-health connection: evidence, theory and future directions. Health Educ Behav. 1998;25:700–20. https://doi.org/10.1177/109019819802500603.
Koenig H, Kind D, Carson V. Handbook of religion and health. Second ed. New York: Oxford University Press; 2012.
Krause N, Hill P, Emmons R, Pargament K, Ironson G. Assessing the relationship between religious involvement and health behaviors. Health Educ Behav. 2017;44:278–84. https://doi.org/10.1177/1090198116655314.
Headey B, Hoehne G, Wagner GG. Does religion make you healthier and longer lived? Evidence for Germany. Soc Indic Res. 2014;119(3):1335–61.
Stark R. Religion and conformity. In: Day J, Laufer W, editors. Crimes, values, and religion. Norwood: Ablex; 1987. p. 111–20.
Ford J. Some implications of denominational heterogeneity and church attendance for alcohol consumption among Hispanics. J Sci Study Relig. 2006;45(20):253–67. https://doi.org/10.1111/j.1468-5906.2006.00304.x.
Hill T, Ellison CG, Burdette A, Musick M. Religious involvement and healthy lifestyles. Ann Behav Med. 2007;34(2):217–22. https://doi.org/10.1080/08836610701566993.
Benjamins MR, Ellison CG, Krause NM, Marcum JP. Religion and preventive service use: do congregational support and religious beliefs explain the relationship between attendance and utilization? J Behav Med. 2011;34(6):462–76.
Idler E. Religion as a social determinant of public health. New York: Oxford University Press; 2014.
Chatters L. Religion and health: public health research and practice. Ann Rev Public Health. 2000;21:355–67.
Levin J. God, faith, and health: exploring the spirituality-healing connection. New York: Wiley; 2001.
Garrusi B, Nakhaee N. Religion and smoking: a review of recent literature. Int J Psychiatry Med. 2012;43(3):279–92.
Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Incident obesity and cardiovascular risk factors between young adulthood and middle age by religious involvement. Prev Med. 2012;54(2):117–21.
Godbolt D, Vaghela P, Burdette, et al. Religious attendance and body mass: an examination of variations by race and gender. J Relig Health. 2017. https://doi.org/10.1007/s10943-017-0490-1.
Lara M, Gamboa C, Kahramanian I, Morales L, Bautista D. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Ann Rev Public Health. 2005;26:367–97. https://doi.org/10.1146/annurev.publhealth.26.021304.144615.
Markides K, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60(spec 2):68–75.
Rumbaut RG. Assimilation and its discontents: between rhetoric and reality. Int Migr Rev. 1997;31(4):923–60.
Pargament KI. APA handbook of psychology, religion, and spirituality. Washington, DC: American Psychological Association; 2013.
Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31(1):99–112. https://doi.org/10.1093/epirev/mxp008.
Garcia G, Ellison CG, Sunil T. Religion and selected health behaviors among Latinos in Texas. J Relig Health. 2013;52(1):18–31.
Kegler M, Hall S, Kiser M. Facilitators, challenges, and collaborative activities in faith and health partnerships to address health disparities. Health Educ Behav. 2010;37(5):665–79. https://doi.org/10.1177/1090198110363882.
Powell L, Shahabi L, Thoresen C. Religion and spirituality: linkages to physical health. Am Psychol. 2003;58(1):43–52.
Berkman L, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2014.
Eriksson M. Social capital and health—implications for health promotion. Glob Health Action. 2011;4:5611.
Putnam R. Bowling alone. New York: Simon and Schuster; 2000.
Avalos H. Introduction to the U.S. Latina and Latino religious experience. Boston: Brill Academic Publishers; 2004.
Putnam R, Campbell D. American grace: how religion divides and unites us. New York: Simon and Schuster; 2011.
Steffen PR, Masters KS. Does compassion mediate the intrinsic religion-health relationship? Ann Behav Med. 2005;30(3):217–24.
Park JZ, Smith C. ‘To whom much has been given…’: religious capital and community voluntarism among churchgoing Protestants. J Sci Study Relig. 2000;39(3):272–86.
Kim ES, Konrath SH. Volunteering is prospectively associated health care use among older adults. Soc Sci Med. 2016;149(c):122–9.
Krause N. Church-based social support and change in health over time. Rev Relig Res. 2006;48(2):125–40.
Sloan R. Blind faith. New York: St. Martin’s Press; 2006.
Iannacone L. Religious practice: a human capital approach. J Sci Study Relig. 1990;29(3):297–314.
Portes A. Social capital: its origins and applications in modern sociology. Annu Rev Sociol. 1998;24:1–24.
Stauner N, Exline JJ, Pargament KI. Religious and spiritual struggles as concerns for health and well-being. Horizonte. 2016;14(41):48–75.
Solano J. The Central American religious experience in the U.S: Salvadorans and Guatemalans as case studies. In: Avalos H, editor. Introduction to the U.S. Latina and Latino religious experience. Boston: Brill Academic Publishers; 2004. p. 116–142.
Portes A, Rumbaut R. Immigrant America: a portrait. Fourth ed. Oakland: University of California Press; 2014.
Warner R, Warner G. Gatherings in diaspora: religious communities and the new immigration. Philadelphia: Temple University Press; 1998.
Foley M, Hoge T. Religion and the new immigrants: how faith communities form our newest citizens. New York: Oxford University Press; 2007.
Pew Research Center. The shifting religious identity of Latinos in the United States. 2014. http://www.pewforum.org/2014/05/07/theshifting-religious-identity-of-latinos-in-the-united-states. Accessed 23 Feb 2018.
Massey DS, Higgins ME. The effect of immigration on religious belief and practice: a theologizing or alienating experience. Soc Sci Res. 2011;40(5):1371–89.
Nicholson A, Rose R, Bobek M. Association between attendance at religious services and self-reported health in 22 European countries. Soc Sci Med. 2009;69(4):519–28. https://doi.org/10.1016/j.socscimed.2009.06.024.
Connor P. International migration and religious participation: the mediating impact of individual and contextual effects. Sociol Forum. 2009;24(4):779–803.
Newlin K, Dyess SM, Allard E, Chase S, Melkus GD. A methodological review of faith-based health promotion literature: advancing the science to expand delivery of diabetes education to Black Americans. J Relig Health. 2012;51(4):1075–97.
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Schwingel A, Glavez P. Divine interventions: faith-based approaches to health promotion programs for Latinos. J Relig Health. 2015;56(3):1052–63.
Department of Health, United Kingdom. Health and well-being. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/278140/Health_Behaviours_and_Wellbeing.pdf. Accessed 23 Feb 2018.
American Cancer Society. How smoking tobacco affects your cancer risk. Available at https://www.cancer.org/cancer/cancer-causes/tobacco-and-cancer/health-risks-of-smoking-tobacco.html. Accessed 23 Feb 2018.
Naimi TS, Brewer RD, Mokdad A, Clark D, et al. Binge drinking among US adults. JAMA. 2013;289(1):70–5.
He X, Baker D. Body mass index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am J Public Health. 2004;94:1567–73.
Kaplan S, Caiman N, Golub M, Ruddock C, Billings J. The role of faith based institutions in addressing health disparities. J Health Care Poor Underserved. 2006;7(2 suppl):9–19. https://doi.org/10.1353/hpu.2006.0088.
Arredondo E, Elder J, Ayala G, Campbell N. Fe en Acción: Promoting physical activity among churchgoing Latinas. Am J Public Health. 2017;107(7):1109–15.
Silfee V, Haughton C, Lemon S, Lora V, Rosal M. Spirituality and physical activity and sedentary behavior among Latino men and women in Massachusetts. Ethn Dis. 2017;27(1):3–10.
Abraído-Lanza A, Chao M, Florez K. Do healthy behaviors decline with greater acculturation? Soc Sci Med. 2005;61(6):1243–55. https://doi.org/10.1016/j.socscimed.2005.01.016.
Trinitapoli J, Ellison CG, Boardman JD. U.S. religious congregations and the sponsorship of health-related programs. Soc Sci Med. 2009;68(2):2231–9. https://doi.org/10.1016/j.socscimed.2009.03.036.
Rozier M. Religion and public health: moral tradition as both problem and solution. J Relig Health. 2015;55(6):1891–906.
Baig AA, Benitez A, Locklin CA, et al. Picture good health; a church-based self-management intervention among Latino adults with diabetes. J Gen Intern Med. 2015;30(10):1481–90. https://doi.org/10.1007/s11606-015-3339-x.
Gross T, Story C, Harvey I, Whitt-Glover M. Pastors’ perceptions on the health status of the Black church and African-American communities. J Racial Ethn Health Disparities. 2017; https://doi.org/10.1007/s40615-017-0401-x.
Krause N, Shaw B, Liang J. Social relationships in religious institutions and healthy lifestyles. Health Educ Behav. 2011;38(1):25–38.
Acknowledgments
The author would like to acknowledge the assistance of the following during the course of the research and writing of this paper: Ana Abraído-Lanza, PhD; Angela Aidala, PhD; Nancy Foner, PhD; Joyce Moon-Howard, DrPH; Courtney Bender, PhD; and Victor Rodwin, PhD.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The survey used in the study was reviewed and approved by the Institutional Review Board of Princeton University.
Conflict of Interest
The author declares that he has no conflict of interest.
Ethical Approval (Animals)
This article does not contain any studies with animals performed by any of the authors.
Ethical Approval (Human Subjects)
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable.
Rights and permissions
About this article
Cite this article
Shapiro, E. Places of Habits and Hearts: Church Attendance and Latino Immigrant Health Behaviors in the United States. J. Racial and Ethnic Health Disparities 5, 1328–1336 (2018). https://doi.org/10.1007/s40615-018-0481-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-018-0481-2