Abstract
Purpose of Review
This review aims to compile the current knowledge on the impact of climate change on human pathogenic fungi. Ongoing surveillance of the fungal lineages described here will be imperative to predict disease burden and geographic expansion.
Recent Findings
Emerging infectious diseases are increasing in frequency and impact in response to anthropogenic expedited climate change. The simultaneous global emergence of the multidrug-resistant fungus Candida auris has been hypothesized to be intimately related to warming temperatures. Diverse evolutionary pressures, including higher average temperatures caused by climate change and conditioning of pathogens to endothermy, has contributed to antifungal resistance in several fungal lineages. Endemic fungi (e.g., species of Coccidioides, Blastomyces, and Histoplasma) known to be largely constrained by environment and host range are expanding in distribution and increasing disease burden. The COVID-19 pandemic illuminated the vulnerability of human populations to aspergillosis and mucormycosis co-infections. The increasing frequency of extreme weather events presents favorable circumstances for opportunistic fungal infections.
Summary
Long-term shifts in temperatures and weather patterns are anticipated to influence emergence, expansion, and virulence of human pathogenic fungi. This includes warming temperatures and stochastic precipitation that may aid in expanding the distribution of several endemic fungal pathogenic lineages and increase disease burden. Here, we review both long-term climate patterns and short-term environmental disruption events that affect dispersal and incidence of human pathogenic fungi. Population growth, urbanization, intercontinental travel, and increased human longevity coupled with progressively damaging climate change effects generate conditions that make communities increasingly vulnerable to fungal pathogens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
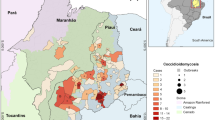
While certain television shows exaggerate doom from a fungal epidemic, there are notes of truth concerning the emergence and expansion of fungal diseases. Massive population die-offs caused by fungal pathogens are increasing in frequency over the last three decades across the kingdom Animalia. These include white-nose syndrome in bats [1], chytridiomycosis in amphibians [2], sea turtle egg fusariosis [3], snake fungal disease [4], cat-transmitted sporotrichosis [5], and sea star wasting disease [6]. Recent recognition by the World Health Organization (WHO) of fungal priority pathogens acknowledges the reality of emerging, expanding, and more virulent human fungal pathogens [7]. Fungal diseases kill more than 1.5 million and affect over a billion people per year [8]. However, infectious fungi receive less attention than viruses and bacteria since they typically do not derive from dramatic spillover events and are generally not transmissible person-to-person. Severe consequences are expected as novel pathogens are introduced to naïve environments. The objective of this review is to compile the current knowledge on the impact of climate change on human pathogenic fungi focusing on emergent fungal pathogens, those with expanding distributions, as well as those with climate change induced virulence (Fig. 1).
Climate change represents a global challenge characterized by long-term shifts in temperatures and weather patterns that is aggravated by anthropogenic carbon emissions. It involves heightened temperatures, irregular weather patterns, retreating of global ice sheets, and elevated sea levels [9, 10]. Temperatures are predicted to rise (2–4 °C in the next 100 years) [11, 12]. Drought, heat waves, longer wildfire seasons, extreme rainfall, and stronger hurricanes are expected to be the results of these changes. Climate change can exacerbate the emergence of fungal pathogens that affect humans directly (i.e., clinical disease) and indirectly (e.g., food security, wildlife extinction, and animal health). It can also alter pathogen evolution and host-pathogen interactions leading to an increased risk of fungal disease outbreaks [13]. This may include adaptation to higher temperatures that can consequently lead to shifts in pathogen geographic distribution [14], changes in wind currents and intensity that affect disease burden and range [15, 16], or community-level phenological shifts that alter both pathogen dispersal and distribution [17, 18].
Pathogenic fungi exist in a broad range of natural habitats. Human pathogenicity has evolved on multiple occasions from non-pathogenic fungi in several major lineages of the fungal tree of life [19••]. Some have well-defined, known geographic ranges (e.g., Blastomyces dermatitidis, Coccidioides spp., and Paracoccidioides spp.), while others are considered ubiquitous (e.g., Aspergillus fumigatus, Fusarium spp.). Their distribution may be defined by that of their animal hosts or vectors [20, 21], while the abundance and distribution of soil- or plant-associated fungi depend directly on climatic factors such as temperature and moisture [22]. For example, coccidioidomycosis incidence in Arizona correlates with hot, dry conditions [23••, 24], blastomycosis clusters associate with rainfall after periods of decreased precipitation [25], incidence of Penicillium marneffei penicilliosis increases during rainy months [26], and aspergillosis correlates with seasonality in some geographic areas [27]. Environmental disruption is a key factor in the dispersal of pathogenic fungi and their potential to cause infection. There is a link between natural disasters and subsequent human fungal infections in these disaster stricken areas [28]. Pathogenic fungi can be displaced from their natural habitats during a disaster, thus increasing their environmental concentration or introducing them to areas where they would not normally be found. An uptick in fungal spores that may come in contact with injured persons greatly increases opportunities for spurious fungal infections [28] caused by natural events such as dust storms [29], earthquakes [30], tsunamis [31,32,33,34,35], hurricanes [36, 37], and tornadoes [38]. Coccidioidomycosis outbreaks were associated with a severe dust storm in the southern San Joaquin Valley of California in December 1977 [29] and with the January 1994 earthquake in Northridge California, when spores were presumably aerosolized and dispersed by dust clouds [30]. Aspergillus has been implicated as an agent of tsunami lung, such as after the 2011 Great East Japan Earthquake and subsequent tsunami where a near-drowning victim, that later died, was found to have disseminated aspergillosis [35]. Persons injured during the 2004 Indian Ocean tsunami showed post-disaster soft tissue mucormycosis [31,32,33]. Clusters of mucormycosis cases have occurred among 13 persons severely injured on the May 22, 2011, tornado in Joplin, Missouri caused by Apophysomyces trapeziformis [38] and 8 patients after the 1985 volcanic eruption in Armero, Colombia, caused by Rhizopus arrhizus [39]. Paracoccidioidomycosis infection rates were strongly correlated to the 1982/1983 El Niño Southern Oscillation in Brazil [40]. Unfortunately, current patterns of population growth, urbanization, and human activity coupled with progressively damaging climate change effects create conditions that render communities increasingly vulnerable to these hazards [41].
Emerging Fungal Diseases
For the purpose of this review, we consider emerging fungal diseases to be those that have been reported to cause human disease in the last 30 years, have arisen in new geographic locations, or have become increasingly problematic with their emergence being attributed to climate change effects, such as candidiasis, fusariosis, mucormycosis, and emergomycosis. Not discussed at length here, but of growing concern, are a number of uncommon disease-causing fungi such as filamentous basidiomycetes [42] and fungi-causing entomophthoromycosis (e.g., conidiobolomycosis and basidiobolomycosis) [43].
Candidiasis
Synergies between temperature (thermal adaptation to warming climates) and fungicide exposure have been invoked to explain the rapid worldwide emergence of multidrug-resistant C. auris in humans, following its discovery in Japan in 2009 [44, 45, 46••]. Pathogenic lineages of this fungus emerged independently on three continents simultaneously (i.e., Asia, Africa, and South America) [45], and it is suggested to have emerged in part as a result of widespread use of antifungal drugs [47]. Candida auris isolates are broadly resistant to antifungals, severely limiting treatment options [45]. This Candida species is also capable of growing at higher temperatures than most of its close relatives while it preferentially colonizes the cooler skin (e.g., ears), facts consistent with a recent acquisition of thermotolerance [46••]. The few C. auris isolates from environmental origin available are significantly different from clinical isolates as they are more susceptible to antifungal agents and grow slowly at 37 and 42 °C [48]. Although human-induced climate changes could be responsible for the continuous narrowing of the thermal restriction zone for C. auris, other factors (e.g., migration, pollution, and high population density) may explain its persistence and acquisition of antifungal resistance [49].
Fusariosis
Various species within Fusarium [50, 51] cause local or invasive fusariosis, generally involving immunosuppressed individuals but occasionally immunocompetent patients [52,53,54]. In healthy individuals, observed fusariosis includes onychomycoses, skin infections, and keratitis. Fusarium keratitis develops from trauma to the eye, contact lens wear, and use of corticosteroids [55,56,57], with trauma being the typical predisposing factor and occurring in 40–60% of patients [56]. Meanwhile, in immunocompromised individuals, deep local and disseminated infections are observed [58]. Fusarium conidia can travel significant distances, making them efficient at dispersal [55]. Some species cause infections worldwide, but endemic regions are tropical and subtropical [54, 59]. Members of the F. solani species complex (FSSC) are the most common (i.e., F. falciforme and F. keratoplasticum) and most virulent human pathogens, followed by the F. oxysporum and F. fujikuroi species complexes (FOSC and FFSC, respectively) [52, 58, 60]. The prevalence of fusaria in the environment has been connected to plumbing systems and soils. FFSC, FOSC, and F. dimerum species complexes are highly represented in sink drain biofilms. The same top six multi-locus sequence types (MLSTs) are found in sink drains and clinical isolates [61], and four FSSC haplotype groups have been particularly associated with human infections [62]. Fusarium spp. can also affect humans indirectly as many of them are mycotoxigenic and can cause devastating diseases, producing trichothecenes and fumonisins [63]. The response of mycotoxigenic fungi to climate change could induce shifts in their geographical distribution and the pattern of mycotoxin occurrence [64•]. Mycotoxin production in Fusarium is highly influenced by climatic conditions; for example, mycotoxin contamination in maize has been connected to extreme levels of precipitation [65]. Mycotoxin contamination is expected to increase as an effect of climate change [66].
Mucormycosis
Fungi in the order Mucorales—including species of Rhizopus, Lichtheimia, and Mucor [67]—are environmentally ubiquitous and can cause life-threatening invasive infections [68]. Associations between weather patterns and mucormycosis have been hypothesized [69,70,71], suggesting that warm and dry conditions contribute to mucormycosis clusters [72]. The sporangiospores of Mucorales are small and can be aerosolized and dispersed under favorable atmospheric conditions which vary from high humidity to xerophytic conditions depending on the taxa [73]. Traumatic skin injury and inhalation or ingestion of spores can lead to invasive mucormycosis [74], usually in patients with diabetes mellitus or who are severely immunocompromised [67]. Mucormycosis cases have been reported after natural disasters, such as causing necrotizing fasciitis in victims of the 2004 Indian Ocean tsunami [31] and the 2011 Missouri tornado [38]. Invasive pulmonary mucormycosis is a recognized secondary complication of COVID-19 [75, 76] and has been reported in combination with pulmonary aspergillosis, especially in COVID-19 critically ill patients in the intensive care unit [77, 78].
Emergomycosis and Emmonsia-Like Pathogens
In 1994, an Italian woman with advanced HIV disease and widespread cutaneous lesions was diagnosed with an atypical disseminated mycosis, caused by the dimorphic fungus Emergomyces africanus [79]. As a result of advancements in molecular identification procedures, E. africanus is now linked to at least 86 patients with disseminated mycoses with advanced HIV in South Africa [80, 81]. The genus Emergomyces includes five species causing emergomycosis systemic fungal infections in immunocompromised persons, and such emergomycoses have been documented on at least four continents [81]. Detections in soil [82] suggest this saprophytic fungus as an opportunistic pathogen taking advantage of the increasing immunocompromised population and human global travel. Characterization of the lung mycobiome in non-human hosts indicates great diversity of close relatives of Emergomyces (e.g., Blastomyces, Emmonsia, and Emmonsiellopsis) [83], many of which have been reported as emerging fungal pathogens causing disease in immunocompromised hosts [84].
Expanding Geographic Distributions
Shifts in global temperature patterns represent an opportunity for environmental fungal pathogens to colonize new geographical areas, expanding their range [85, 86]. Most fungi grow at ambient temperatures; however, only a limited number of species are known to grow well above 37 °C [87]. It is possible that the environment contains large numbers of fungal species with pathogenic potential that are currently non-pathogenic to humans due to their inability to grow at mammalian temperatures [46••]. Higher ambient temperatures, caused by climate change, could lead to selection of fungi with higher thermal tolerance allowing them to breach the mammalian thermal restriction zone [46••] and defeating the protection that was previously granted by endothermy [22].
A selected number of fungi have adapted to shapeshift in multiple environments triggered by changes in temperature (dimorphism). These fungi live as hyphal networks in the environment but shift to a yeast phase for immune evasion upon inhalation of spores by a potential host. Although each fungus possesses its own unique ecology, a number of these are endemic pathogens with defined ranges [88]. In addition to gradual warming and stochastic precipitation that directly affect soil temperature and moisture, geographic expansion of these fungi may be indirectly affected by the distribution of their reservoir hosts or vectors.
Coccidioidomycosis
Coccidioides, causing coccidioidomycosis (Valley fever), is predicted to be intimately influenced by climate change due to its strong correlation with both temperature and precipitation [23••, 89]. A seasonal pattern of wet followed by dry conditions has been linked to increased coccidioidomycosis incidence across the Southwestern United States [90,91,92,93]. Disturbance of dry arid soils caused by high winds or human activities can cause arthrospores to become airborne and inhaled by humans or animals. Spurious natural events can also cause an increase in coccidioidomycosis cases. Unrelenting wildfires in the Western United States have increased significantly in size and frequency over the last 30 years [94]. Smoke contains pollutants harmful to human health as well as viable aerosolized microbes, including fungal conidia that can travel up to hundreds of miles on air currents [95]. Wildfires in California have been broadly correlated to an increase of coccidioidomycosis cases by 20% in the month following smoke exposure [96•]. Additionally, firefighting involves soil-disturbing activities which have been linked to outbreaks of coccidioidomycosis [97]. The distribution of Coccidioides is patchy in the environment and is thought to be dependent on rodent reservoirs that have low-level lung infections [83]. Climate indirectly influences dispersal of Coccidioides as small mammal hosts respond to their habitat, including water and nutrient availability. Upon death, decaying hosts provide keratinaceous materials for the fungus to metabolize and proliferate [21]. Additional thermotolerance to extreme desert temperatures by species of Coccidioides [98] may allow continued proliferation. A pivotal study by Gorris and colleagues estimated that approximately 47.5 M people in 217 counties spanning 12 states live in the coccidioidomycosis endemic region of the United States. This study further estimates that, due to climate warming, by the year 2100, the endemic region of this disease in the USA will more than double in size, affecting 17 states, with the number of cases rising by 50% [85].
Blastomycosis
The environmental niche of Blastomyces, causing blastomycosis, is still largely unknown. However, Blastomyces dermatitidis has been isolated from moist soil and organic matter in the Mississippi and Ohio River Valleys and around the Great Lakes (USA) [99, 100]. Recent transient environmental detections of B. dermatitidis post-flood in Hennepin County Minnesota, a low-endemicity county [101], support the long suspected connection of blastomycosis proliferating after flooding events [102, 103]. Blastomycosis is demanding greater attention due to novel disease-causing species (i.e., B. helicus and B. gilchristii) [104, 105], worsening disease severity [106], and cases expanding beyond the previously defined endemic range [107].
Histoplasmosis
Histoplasma, the causal agent of histoplasmosis, has a global distribution; but the disease is more burdensome in the African and American continents [108]. The radiation of Histoplasma dates to between 3 and 13 million years ago [20]. Nevertheless, climate change arguably has and will continue to influence its rate of expansion. Reports of clinical cases of histoplasmosis in extreme latitudes in Canada [109] and Argentinian Patagonia [110] could be related to new favorable environments for the fungus and/or for its animal vectors. Bats are considered the major reservoir and dispersers. Besides bats, Histoplasma has been detected in a diverse number of wild mammals (e.g., primates, mustelids, and procyonids) [111,112,113], as well as domesticated animals (e.g., equines, canines, and felines) [114, 115]. A tight association with vertebrates suggests that mammals play an important role in the speciation and dispersal mechanisms of Histoplasma. Range, population size, mortality rate, and reproductive success of vertebrate vectors are likely to be affected by climate change [116], which may in turn affect the ecology and evolution of Histoplasma spp.
Cryptococcosis
Cryptococcosis, a fungal infection mainly affecting the lungs or central nervous system, is primarily caused by Cryptococcus neoformans. This fungus has a cosmopolitan distribution and can be found in soil, on decaying wood, in tree hollows, or in bird droppings [117]. While C. neoformans primarily infects immunocompromised individuals, another causative species, C. gattii, can infect healthy individuals [118]. Previously thought to be limited to tropical and subtropical regions of South America, Africa, Asia, and Australia, locally acquired C. gattii outbreaks were first recognized in the late 1990s in the Pacific Northwest (USA) and Europe [119]. Expanding suitable habitat (e.g., eucalyptus trees) and anthropogenic dispersal [120] will only lend to expanding ranges with global warming [121•, 122]. The range expansion of C. gattii may be particularly concerning due to highly virulent clonal lineages [123, 124].
Acquiring Antifungal Resistance and Virulence Factors
Antimicrobial resistance (AMR) is a complex global health challenge, not restricted to particular regions or countries but rather proliferating on every continent. Antifungal resistance usually leads to prolonged treatment and hospital stays, as well as a heightened need for expensive and highly toxic second-line antifungals. The WHO fungal priority pathogens list (FPPL) details antifungal resistance as the highest weighted criterion in determining priority [7]. While AMR in bacteria is propagated by commensal and environmental organisms exchanging extrachromosomal plasmids via horizontal gene transfer, selection for AMR genes and alleles in fungi is generally constrained to within species boundaries; therefore, resistance to antifungals usually evolves de novo for each species [125]. Despite these constraints, evolutionary pressures, including higher average temperatures expected under climate change, conditioning pathogens to endothermy [22], and overuse and dependency on the few available antifungal agents [126, 127], have resulted in antifungal resistance in several fungal lineages. The WHO’s most recent global research agenda for AMR in human health states that Candida auris, Aspergillus fumigatus, and Cryptococcus neoformans are of critical importance [128].
Antifungal drug resistance or tolerance in these fungi is acquired in a variety of ways depending on the antifungal mode of action. For example, azole antifungals inhibit synthesis of the essential membrane component ergosterol. Resistance to azoles can result from mutations in ERG11 homologs, which encode for an enzyme supporting ergosterol production, or from mutations that lead to increased efflux of the drug from the fungal cell [129]. The latter appears to be particularly important in Candida species, while in C. neoformans, overexpression of efflux pumps caused by chromosomal aneuploidy and hypermutation seems to be the main mechanism. Echinocandins, a second class of antifungals, inhibit 1,3-β-d-glucan synthase (FKS1 and FKS2) [130]. Mutations in this gene cause antifungal resistance in Candida and Fusarium, while hypermutation in species of Cryptococcus generates resistance to pyrimidine analogues [125]. However, few studies have explored the extent to which climate changes directly influence the occurrence, directionality, and significance of synergistic interactions between temperature and antifungal resistance.
Climate and environmental pressures have selected for a multitude of additional virulence factors (e.g., thermotolerance, melanin production, and resistance to oxidative stress) that result in successful fungal pathogens. Heat acclimation is thought to be influenced by the availability of new habitats, global climate change, and encountering new hosts [131]. Decreasing human body temperatures [132] make humans even more vulnerable to colonization of thermotolerant pathogens. The capacity for thermotolerance is interspersed among Ascomycetes and Basidiomycetes, suggesting that it may have emerged independently several times in evolutionary history. However, there are certain phylogenetically related taxa, such as cryptococci [133] and aspergilli [134, 135], that have maintained this ability. This phenotype may be due to mutations in heat shock proteins activated in response to changes in temperature that regulate cellular processes associated with morphogenesis, antifungal resistance, and virulence by triggering a wide array of cellular signaling pathways [136]. Fungal thermotolerance is a complex process with diverse manifestations (reviewed in [137]) which requires further study.
Aspergillosis
Aspergillus species are ubiquitous, saprophytic fungi with airborne conidia. Aspergillus fumigatus is the main causative agent of human aspergillosis, which can establish a lung infection when the immune system is compromised [138]. The conidia of A. fumigatus are distinguished by melanin pigmentation which is thought to defend the genetic material from the adverse effects of ionizing radiation in the environment [139]. Oral triazole antifungal drugs (i.e., itraconazole, voriconazole, and posaconazole) are usually effective against A. fumigatus and are used as therapy in management and prophylaxis of invasive aspergillosis [140]. However, azole resistance has emerged in A. fumigatus isolates from Europe, Asia, Middle East, and Africa [141,142,143], likely acquired at least in part from the agricultural use of azoles [144]. High rates of patient mortality are observed when treatment of invasive aspergillosis fails on azole-resistant strains [145,146,147]. The frequency of azole-resistant A. fumigatus is elevated in high-temperature environments such as composts [148,149,150], greenhouses [151], and tropical countries [152]. Heat shock inducing ascospore germination in high-temperature azole-containing habitats can serve as evolutionary accelerators with increased selective pressure on recombination [153] suggesting the occurrence of synergistic interactions between temperature and antifungal resistance [154].
Cryptococcosis
Cryptococcus neoformans is the highest-ranked fungal pathogen in the FPPL [7] and considered a global threat to human health [155]. It regulates caspofungin resistance via posttranscriptional regulation of cell wall biosynthesis genes [156] and flucytosine conversion through transposon mutagenesis [157]. It is also common for C. neoformans to overexpress the drug target and efflux pumps caused by chromosomal aneuploidy and hypermutation [125]. Fluconazole resistance in C. neoformans is attributed to chromosome duplication (aneuploidy) of chromosome 1 which harbors genes ERG11 and AFR1 [158] as well as mutations in the ERG11 gene [159, 160]. A mutation in CDC50 (encodes the β-subunit of membrane lipid flippase) mediates echinocandin resistance by preventing drug uptake [161].
Cryptococcal species maintain several virulence factors that have evolved over long periods of evolutionary time selected by environmental pressures. Melanin production provides protection for multiple species of Cryptococcus from environmental stressors including antifungal compounds, oxidants, UV light, macrophages, and extreme temperature [162]. Cryptococcus gattii preferentially expresses melanin at 30 °C [133] compared with 37 °C for C. neoformans [163]. While C. neoformans is frequently isolated from pigeon guano, the niche of C. gattii remains uncertain; thus, it is unclear what environmental pressures are influencing this phenotype. Although thermotolerance is established in multiple species of Cryptococcus [133], thermotolerant strains of C. laurentii, which normally do not grow at 37 °C, have been associated with disease in extremely immunosuppressed hosts [164]. This may be an indicator that the ability to grow at or above 37 °C may induce pathogenicity in currently benign fungi.
Fusariosis
Fusariosis infections are also challenging to treat due to multidrug resistance [51, 55, 165], further complicated by increased incidence of such infections [166] and the lack of research on developing new therapeutic options for treatment. There is low investment from the pharmaceutical industry for drug development to combat fusariosis [167]. Current treatment and prophylactic agents include amphotericin B, voriconazole, and posaconazole [168]. However, Fusarium spp. have intrinsic resistance to echinocandins [51] and azoles [169]. AMR is a risk factor associated with the use of fungicides in the environment [170]. Azoles are the most commonly used group for pathogen control as well as for treatment of human infections, making it an increasing concern for the potential development of resistance [170]. Additionally, Fusarium has mechanisms that contribute to resistance acquisition to most antifungal agents, like changes in amino acid sequences and overexpression of genes that encode efflux pumps [171].
Candidiasis
The increasing use of azoles for treatment of superficial and systemic infections by C. glabrata has resulted in selection and emergence of resistant isolates and an increase in infections by other non-albicans species [172]. Multiple drug resistance mechanisms have been found in the C. glabrata complex for resistance against azoles, polyenes, and echinocandins. These mechanisms include the overexpression of drug transporters, gene mutations that alter thermotolerance, induction of hypervirulence due to increased adhesion factors, biofilm production, and modifications in vital enzymes that produce cell wall proteins that prevent the activity of drugs designed for its inhibition [173]. Low susceptibility to antifungal therapies available is associated with a higher mortality rate [174].
Candida auris is resistant to fluconazole and has variable susceptibility to other azoles, amphotericin B, and echinocandins [45]. Multidrug resistance and high associated mortality rates make this pathogen an emerging global threat that is difficult to eradicate from hospitals despite intense infection-prevention strategies [45, 47, 175, 176]. The Centers for Disease Control (CDC) has documented that cases of C. auris increased in the USA from 329 in 2018 to 1012 in 2021 [177]. Although accurate data are lacking with respect to antifungal prescription practices, anecdotal evidence suggests an increase in the use of triazoles and other antifungals in recent years. In South Africa, C. auris seems to have emerged more rapidly in private hospitals where echinocandin use is higher than in public hospitals [178]. Increased use of azole antifungals in surgical ICUs is suspected to have caused a shift in the prevalence of Candida species toward the more difficult-to-treat pathogens, particularly C. krusei and C. glabrata [179, 180].
Dermatophytosis
Cutaneous mycoses are among the most common fungal infections worldwide. Dermatophytic fungal species of Microsporum, Epidermophyton, and Trichophyton cause infections of the skin, nails, and hair [181]. Transmission may occur through contact with humans or animals or indirect contact with fomites. During the past decade, an epidemic of severe, antifungal-resistant tinea has emerged in South Asia because of the rapid spread of Trichophyton indotineae, partly owed to the misuse and overuse of topical antifungals and corticosteroids [126]. Severe infections prove to be resistant to conventional antifungals, including allylamines (terbinafine and naftifine) conferred by point mutations in the squalene epoxidase (SQLE) gene and azoles (itraconazole and fluconazole). While the expansion of clinical cases has mainly been attributed to global travel, temperature and humidity are also critical to dermatophyte growth. In rabbit farms, the presence of dermatophytes was significantly higher in animals held under conditions with higher temperatures (> 20 °C) and with humidity ranging from 62 to 65% [182]. The range of Microsporum canis is limited by altitude, suggesting that the fungus may be constrained in the soil by temperature and moisture [183].
Conclusions and Future Directions
Anthropogenic induced climate change may provide fungal pathogens with opportunities to expand their distribution and develop antifungal resistance and other virulence factors. But additional considerations such as the increasing number of immunocompromised hosts, limited antifungal therapies, and an absence of fungal vaccinations compound the emergence, persistence, and expansion of these fungal pathogens. Fungal infections tend to be overlooked, and increased awareness by health care providers, public health professionals, and community members is necessary. The impacts of climate change are predicted to become more severe as global temperatures continue to rise and as climate change contributes to greater frequency and severity of extreme weather events. Very few fungi are obligate to human hosts (i.e., Pneumocystis spp.), while the majority have an environmental phase (e.g., saprobic, endophytic, or aquatic) where they certainly will be impacted by changes in the climate and weather. Despite ongoing research on human fungal pathogens, more work is needed to bridge the gaps between scientists investigating ecology and evolution and physicians diagnosing and treating patients. Advancements in genomics increase opportunities for translational medicine, such as determining resistance profiles and rise of pathogenic strains.
Myriad research questions remain unanswered in this field, from basic biology and ecology of these fungal pathogens to applied clinical research. Further studies are needed to validate hypotheses associated with the emergence of certain fungal pathogens (e.g., Candida auris) and determining the environmental niche of them (e.g., Blastomyces, whose environmental niche is still undetermined). We have summarized the limited current knowledge of how climate change may affect human pathogenic fungi. Yet, a large knowledge gap remains. We encourage studies on (1) the occurrence, directionality, and significance of synergistic interactions between temperature and antifungal resistance [154]; (2) the development of new therapeutic options for treatment, including a higher investment from the pharmaceutical industry for drug development to combat fungal diseases; (3) detailed range expansion of natural reservoirs and surveillance data; and (4) the effects of the interaction between multiple fungal diseases on the same patient (e.g., invasive pulmonary mucormycosis reported in combination with pulmonary aspergillosis in COVID-19 patients in ICU) [77, 78].
Improvements in surveillance and increased education about fungal infections is of paramount importance to alleviate underreporting and delayed diagnosis in order to further accurately understand range expansion and disease burden. For example, although the National Notifiable Diseases Surveillance System (NNDSS) tracks cases of coccidioidomycosis in 26 states (52%), neither histoplasmosis nor blastomycosis is currently a nationally notifiable condition [184]. This detailed incidence and distribution data would be invaluable for its use in disease epidemiology and forecasting. Computational models have been successfully developed for infectious human disease forecasting, such as for dengue viruses [185] and West Nile virus [186], but have rarely been implemented for fungi. Coordination between biologists, mycologists, and epidemiologists along with health officials in each region is needed to further advance in this field and get ahead of the potential challenges climate change effects will have on fungal pathogen distribution expansion and disease incidence.
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance.
Blehert DS, Hicks AC, Behr M, Meteyer CU, Berlowski-Zier BM, Buckles EL, et al. Bat white-nose syndrome: an emerging fungal pathogen? Science. 2009;323:227–227.
Skerratt LF, Berger L, Speare R, Cashins S, McDonald KR, Phillott AD, et al. Spread of chytridiomycosis has caused the rapid global decline and extinction of frogs. EcoHealth. 2007;4:125.
Smyth CW, Sarmiento-Ramírez JM, Short DPG, Diéguez-Uribeondo J, O’Donnell K, Geiser DM. Unraveling the ecology and epidemiology of an emerging fungal disease, sea turtle egg fusariosis (STEF). Hogan DA, editor. PLoS Pathog. 2019;15:e1007682.
Lorch JM, Knowles S, Lankton JS, Michell K, Edwards JL, Kapfer JM, et al. Snake fungal disease: an emerging threat to wild snakes. Phil Trans R Soc B. 2016;371:20150457.
Gremião IDF, Miranda LHM, Reis EG, Rodrigues AM, Pereira SA. Zoonotic epidemic of sporotrichosis: cat to human transmission. Sheppard DC, editor. PLoS Pathog. 2017;13:e1006077.
Hewson I, Button JB, Gudenkauf BM, Miner B, Newton AL, Gaydos JK, et al. Densovirus associated with sea-star wasting disease and mass mortality. Proc Natl Acad Sci USA. 2014;111:17278–83.
WHO. WHO fungal priority pathogens list to guide research, development and public health action. Geneva: World Health Organization; 2022.
Bongomin F, Gago S, Oladele R, Denning D. Global and multi-national prevalence of fungal diseases—estimate precision. JoF. 2017;3:57.
Lipczynska-Kochany E. Effect of climate change on humic substances and associated impacts on the quality of surface water and groundwater: a review. Sci Total Environ. 2018;640–641:1548–65.
Murshed M, Dao NTT. Revisiting the CO2 emission-induced EKC hypothesis in South Asia: the role of export quality improvement. GeoJournal. 2022;87:535–63.
Battisti DavidS, Naylor RL. Historical warnings of future food insecurity with unprecedented seasonal heat. Science. 2009;323:240–4.
Weisheimer A, Palmer TN. Changing frequency of occurrence of extreme seasonal temperatures under global warming. Geophys Res Lett. 2005;32:L20721.
Singh BK, Delgado-Baquerizo M, Egidi E, Guirado E, Leach JE, Liu H, et al. Climate change impacts on plant pathogens, food security and paths forward. Nat Rev Microbiol. 2023
McLean MA, Angilletta MJ, Williams KS. If you can’t stand the heat, stay out of the city: thermal reaction norms of chitinolytic fungi in an urban heat island. J Therm Biol. 2005;30:384–91.
Jasim SA, Mohammadi MJ, Patra I, Jalil AT, Taherian M, Abdulaeva UY, et al. The effect of microorganisms (bacteria and fungi) in dust storm on human health. Rev Environ Health. 2022;39:65–75.
Griffin DW, Kellogg CA, Shinn EA. Dust in the wind: long range transport of dust in the atmosphere and its implications for global public and ecosystem health. Global Chang Human Health. 2001;2:20–33.
Ovaskainen O, Skorokhodova S, Yakovleva M, Sukhov A, Kutenkov A, Kutenkova N, et al. Community-level phenological response to climate change. Proc Natl Acad Sci USA. 2013;110:13434–9.
Vogt-Schilb H, Richard F, Malaval J-C, Rapior S, Fons F, Bourgade V, et al. Climate-induced long-term changes in the phenology of Mediterranean fungi. Fungal Ecology. 2022;60:101166.
•• Rokas A. Evolution of the human pathogenic lifestyle in fungi. Nat Microbiol. 2022;7:607–19. Provides insights into the traits, genetic elements, and genetic and ecological mechanisms that contribute to the evolution of fungal pathogenicity.
Kasuga T, White TJ, Koenig G, Mcewen J, Restrepo A, Castañeda E, et al. Phylogeography of the fungal pathogen Histoplasma capsulatum. Molecular Ecology. 2003;12:3383–401.
Taylor JW, Barker BM. The endozoan, small-mammal reservoir hypothesis and the life cycle of Coccidioides species. Medical Mycology. 2019;57:S16-20.
Garcia-Solache MA, Casadevall A. Global warming will bring new fungal diseases for mammals. mBio. 2010;1:e00061-10.
•• Gorris ME, Cat LA, Zender CS, Treseder KK, Randerson JT. Coccidioidomycosis dynamics in relation to climate in the southwestern United States. GeoHealth. 2018;2:6–24 Forecasters demonstrate the endemic region of Coccidioides will expand in response to climate change.
Tamerius JD, Comrie AC. Coccidioidomycosis incidence in Arizona predicted by seasonal precipitation. Deepe G, editor. PLoS ONE. 2011;6:e21009.
Proctor ME, Klein BS, Jones JM, Davis JP. Cluster of pulmonary blastomycosis in a rural community: evidence for multiple high-risk environmental foci following a sustained period of diminished precipitation. 2001;153:113–20
Le T, Wolbers M, Chi NH, Quang VM, Chinh NT, Huong Lan NP, et al. Epidemiology, seasonality, and predictors of outcome of AIDS-associated Penicillium marneffei infection in Ho Chi Minh City Viet Nam. Clin Infect Diseas. 2011;52:945–52.
Park BJ, Pappas PG, Wannemuehler KA, Alexander BD, Anaissie EJ, Andes DR, et al. Invasive non-Aspergillus mold infections in transplant recipients, United States, 2001–2006. Emerg Infect Dis. 2011;17:1855–64.
Benedict K, Park BJ. Invasive fungal infections after natural disasters. Emerg Infect Dis. 2014;20:349–55.
Flynn NM, Hoeprich PD, Kawachi MM, Lee KK, Lawrence RM, Goldstein E, et al. An unusual outbreak of windborne coccidioidomycosis. N Engl J Med. 1979;301:358–61.
Schneider E, Hajjeh RA, Spiegel RA, Jibson RW, Harp EL, Marshall GA, et al. A coccidioidomycosis outbreak following the Northridge, Calif, earthquake. JAMA. 1997;277:904–8.
Andresen D, Donaldson A, Choo L, Knox A, Klaassen M, Ursic C, et al. Multifocal cutaneous mucormycosis complicating polymicrobial wound infections in a tsunami survivor from Sri Lanka. The Lancet. 2005;365:876–8.
Snell BJ, Tavakoli K. Necrotizing fasciitis caused by Apophysomyces elegans complicating soft-tissue and pelvic injuries in a tsunami survivor from Thailand. Plast Reconstr Surg. 2007;119:448–9.
Maegele M, Gregor S, Yuecel N, Simanski C, Paffrath T, Rixen D, et al. One year ago not business as usual: wound management, infection and psychoemotional control during tertiary medical care following the 2004 Tsunami disaster in southeast Asia. Crit Care. 2006;10:R50.
Garzoni C, Emonet S, Legout L, Benedict R, Hoffmeyer P, Bernard L, et al. Atypical infections in tsunami survivors. Emerg Infect Dis. 2005;11:1591–3.
Kawakami Y, Tagami T, Kusakabe T, Kido N, Kawaguchi T, Omura M, et al. Disseminated aspergillosis associated with tsunami lung. Respir Care. 2012;57:1674–8.
Riddel CE, Surovik JG, Chon SY, Wang W-L, Cho-Vega JH, Cutlan JE, et al. Fungal foes: presentations of chromoblastomycosis post–Hurricane Ike.
Chow NA, Toda M, Pennington AF, Anassi E, Atmar RL, Cox-Ganser JM, et al. Hurricane-associated mold exposures among patients at risk for invasive mold infections after Hurricane Harvey — Houston, Texas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:469–73.
Neblett Fanfair R, Benedict K, Bos J, Bennett SD, Lo Y-C, Adebanjo T, et al. Necrotizing cutaneous mucormycosis after a tornado in Joplin, Missouri, in 2011. N Engl J Med. 2012;367:2214–25.
Patiño JF, Castro D, Valencia A, Morales P. Necrotizing soft tissue lesions after a volcanic cataclysm. World J Surg. 1991;15:240–7.
Barrozo LV, Benard G, Silva MES, Bagagli E, Marques SA, Mendes RP. First description of a cluster of acute/subacute paracoccidioidomycosis cases and its association with a climatic anomaly. Carvalho MS, editor. PLoS Negl Trop Dis. 2010;4:e643.
Huppert HE, Sparks RSJ. Extreme natural hazards: population growth, globalization and environmental change. Philos Trans Royal Soc A: Math Phys Eng Sci. 2006;364:1875–88.
Chowdhary A, Kathuria S, Agarwal K, Meis JF. Recognizing filamentous basidiomycetes as agents of human disease: a review. Med Mycol. 2014;52:782–97.
Shaikh N, Hussain KA, Petraitiene R, Schuetz AN, Walsh TJ. Entomophthoromycosis: a neglected tropical mycosis. Clin Microbiol Infection. 2016;22:688–94.
Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiology and Immunology. 2009;53:41–4.
Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. CLINID. 2017;64:134–40.
•• Casadevall A, Kontoyiannis DP, Robert V. On the emergence of Candida auris: Climate change, azoles, swamps, and birds. Kronstad JW, editor. mBio. 2019;10:e01397-19. Outlines the hypothesis that thermal adaptation of Candida auris is derived from an environmental ancestor induced by warming climate.
Chowdhary A, Sharma C, Meis JF. Candida auris: a rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. Hogan DA, editor. PLoS Pathog. 2017;13:e1006290.
Casadevall A, Kontoyiannis DP, Robert V. Environmental Candida auris and the global warming emergence hypothesis. mBio. 2021;12:e00360-21.
Misseri G, Ippolito M, Cortegiani A. Global warming “heating up” the ICU through Candida auris infections: The climate changes theory. Crit Care. 2019;23:416.
Gomes LB, Ward TJ, Badiale-Furlong E, Del Ponte EM. Species composition, toxigenic potential and pathogenicity of Fusarium graminearum species complex isolates from southern Brazilian rice. Plant Pathol. 2015;64:980–7.
Al-Hatmi AMS, Bonifaz A, Ranque S, Sybren De Hoog G, Verweij PE, Meis JF. Current antifungal treatment of fusariosis. International Journal of Antimicrobial Agents. 2018;51:326–32.
Guarro J. Fusariosis, a complex infection caused by a high diversity of fungal species refractory to treatment. Eur J Clin Microbiol Infect Dis. 2013;32:1491–500.
Dabas Y, Bakhshi S, Xess I. Fatal cases of bloodstream infection by Fusarium solani and review of published literature. Mycopathologia. 2016;181:291–6.
Van Diepeningen AD, Brankovics B, Iltes J, Van Der Lee TAJ, Waalwijk C. Diagnosis of Fusarium infections: approaches to identification by the clinical mycology laboratory. Curr Fungal Infect Rep. 2015;9:135–43.
Taj-Aldeen S. Reduced multidrug susceptibility profile is a common feature of opportunistic Fusarium species: Fusarium multi-drug resistant pattern. JoF. 2017;3:18.
Garnica M, Nucci M. Epidemiology of fusariosis. Curr Fungal Infect Rep. 2013;7:301–5.
Nucci F, Nouér SA, Capone D, Anaissie E, Nucci M. Fusariosis. Semin Respir Crit Care Med. 2015;36:706–14.
Van Diepeningen AD, Al-Hatmi AMS, Brankovics B, De Hoog GS. Taxonomy and clinical spectra of Fusarium species: where do we stand in 2014? Curr Clin Micro Rpt. 2014;1:10–8.
Al-Hatmi AM, Hagen F, Menken SB, Meis JF, De Hoog GS. Global molecular epidemiology and genetic diversity of Fusarium, a significant emerging group of human opportunists from 1958 to 2015. Emerg Microb Infections. 2016;5:1–11.
Van Diepeningen AD, Feng P, Ahmed S, Sudhadham M, Bunyaratavej S, De Hoog GS. Spectrum of Fusarium infections in tropical dermatology evidenced by multilocus sequencing typing diagnostics. Mycoses. 2015;58:48–57.
Short DPG, O’Donnell K, Zhang N, Juba JH, Geiser DM. Widespread occurrence of diverse human pathogenic types of the fungus Fusarium detected in plumbing drains. J Clin Microbiol. 2011;49:4264–72.
Zhang N, O’Donnell K, Sutton DA, Nalim FA, Summerbell RC, Padhye AA, et al. Members of the Fusarium solani species complex that cause infections in both humans and plants are common in the environment. J Clin Microbiol. 2006;44:2186–90.
Woloshuk CP, Shim W-B. Aflatoxins, fumonisins, and trichothecenes: a convergence of knowledge. FEMS Microbiol Rev. 2013;37:94–109.
• Zingales V, Taroncher M, Martino PA, Ruiz M-J, Caloni F. Climate change and effects on molds and mycotoxins. Toxins. 2022;14:445 Summarizes available evidence of the impact of climate change on mycotoxigenic fungi like Aspergillus, Penicillium, and Fusarium.
Janić Hajnal E, Kos J, Radić B, Anić M, Radović R, Kudumija N, et al. Impact of climate changes on the natural prevalence of Fusarium mycotoxins in maize harvested in Serbia and Croatia. Foods. 2023;12:1002.
Ji F, He D, Olaniran AO, Mokoena MP, Xu J, Shi J. Occurrence, toxicity, production and detection of Fusarium mycotoxin: a review. Food Prod Process and Nutr. 2019;1:6.
Kollipara R, Peranteau AJ, Nawas ZY, Tong Y, Woc-Colburn L, Yan AC, et al. Emerging infectious diseases with cutaneous manifestations: fungal, helminthic, protozoan and ectoparasitic infections. Journal of the American Academy of Dermatology. 2016;75:19–30.
Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clinical Infectious Diseases. 2012;54:S23-34.
Al-Ajam MR, Bizri AR, Mokhbat J, Weedon J, Lutwick L. Mucormycosis in the Eastern Mediterranean: a seasonal disease. Epidemiol Infect. 2006;134:341–6.
Shpitzer T, Keller N, Wolf M, Goldschmied-Reouven A, Bahar G, Bahar I, et al. Seasonal variations in rhino-cerebral Mucor infection. Ann Otol Rhinol Laryngol. 2005;114:695–8.
Talmi YP, Goldschmied-Reouven A, Bakon M, Barshack I, Wolf M, Horowitz Z, et al. Rhino-orbital and rhino-orbito-cerebral mucormycosis. Otolaryngol-Head Neck Surg. 2002;127:22–31.
Sivagnanam S, Sengupta DJ, Hoogestraat D, Jain R, Stednick Z, Fredricks DN, et al. Seasonal clustering of sinopulmonary mucormycosis in patients with hematologic malignancies at a large comprehensive cancer center. Antimicrob Resist Infect Control. 2017;6:123.
Richardson M. The ecology of the Zygomycetes and its impact on environmental exposure. Clinical Microbiol Infection. 2009;15:2–9.
Dannaoui E, Lackner M. Special issue: Mucorales and mucormycosis. JoF. 2019;6:6.
Pasero D, Sanna S, Liperi C, Piredda D, Branca GP, Casadio L, et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection. 2021;49:1055–60.
Zurl C, Hoenigl M, Schulz E, Hatzl S, Gorkiewicz G, Krause R, et al. Autopsy proven pulmonary mucormycosis due to Rhizopus microsporus in a critically ill COVID-19 patient with underlying hematological malignancy. JoF. 2021;7:88.
Johnson AK, Ghazarian Z, Cendrowski KD, Persichino JG. Pulmonary aspergillosis and mucormycosis in a patient with COVID-19. Med Mycol Case Reports. 2021;32:64–7.
Mohanty B, Ansari Z, Prasad A, Gupta M, Kumar A. Mucormycosis and aspergillosis: the deadly duo in COVID-19—a case report. J Family Med Prim Care. 2022;11:6529.
Gori S, Drouhet E, Gueho E, Huerre M, Lofaro A, Parenti M, et al. Cutaneous disseminated mycosis in a patient with AIDS due to a new dimorphic fungus. J de mycologie médicale (Paris). 1998;8:57–63.
Kenyon C, Bonorchis K, Corcoran C, Meintjes G, Locketz M, Lehloenya R, et al. A dimorphic fungus causing disseminated infection in South Africa. N Engl J Med. 2013;369:1416–24.
Schwartz IS, Govender NP, Sigler L, Jiang Y, Maphanga TG, Toplis B, et al. Emergomyces: the global rise of new dimorphic fungal pathogens. Hogan DA, editor. PLoS Pathog. 2019;15:e1007977.
Schwartz IS, Lerm B, Hoving JC, Kenyon C, Horsnell WG, Basson WJ, et al. Emergomyces africanus in soil, South Africa. Emerg Infect Dis. 2018;24:377–80.
Salazar-Hamm PS, Montoya KN, Montoya L, Cook K, Liphardt S, Taylor JW, et al. Breathing can be dangerous: opportunistic fungal pathogens and the diverse community of the small mammal lung mycobiome. Front Fungal Biol. 2022;3:996574.
Schwartz IS, Kenyon C, Feng P, Govender NP, Dukik K, Sigler L, et al. 50 years of Emmonsia disease in humans: the dramatic emergence of a cluster of novel fungal pathogens. Heitman J, editor. PLoS Pathog. 2015;11:e1005198.
Gorris ME, Treseder KK, Zender CS, Randerson JT. Expansion of coccidioidomycosis endemic regions in the United States in response to climate change. GeoHealth. 2019;3:308–27.
Rickerts V. Klimawandel und Epidemiologie systemischer Pilzinfektionen. Bundesgesundheitsbl. 2019;62:646–51.
Robert VA, Casadevall A. Vertebrate endothermy restricts most fungi as potential pathogens. J Infect Dis. 2009;200:1623–6.
Van Dyke MCC, Teixeira MM, Barker BM. Fantastic yeasts and where to find them: the hidden diversity of dimorphic fungal pathogens. Curr Opin Microbiol. 2019;52:55–63.
Baptista-Rosas RC, Hinojosa A, Riquelme M. Ecological niche modeling of Coccidioides spp. in western North American deserts. Annals of the New York Academy of Sciences. 2007;1111:35–46.
Comrie AC. Climate factors influencing coccidioidomycosis seasonality and outbreaks. Environ Health Perspect. 2005;113:688–92.
Park BJ, Sigel K, Vaz V, Komatsu K, McRill C, Phelan M, et al. An epidemic of coccidioidomycosis in Arizona associated with climatic changes, 1998–2001. J Infect Dis. 2005;191:1981–7.
Coopersmith EJ, Bell JE, Benedict K, Shriber J, McCotter O, Cosh MH. Relating coccidioidomycosis (Valley fever) incidence to soil moisture conditions: Valley fever and soil moisture. GeoHealth. 2017;1:51–63.
Head JR, Sondermeyer-Cooksey G, Heaney AK, Yu AT, Jones I, Bhattachan A, et al. Effects of precipitation, heat, and drought on incidence and expansion of coccidioidomycosis in western USA: a longitudinal surveillance study. The Lancet Planetary Health. 2022;6:e793-803.
Marlon JR, Bartlein PJ, Gavin DG, Long CJ, Anderson RS, Briles CE, et al. Long-term perspective on wildfires in the Western USA. Proc Natl Acad Sci USA. 2012;109. https://doi.org/10.1073/pnas.1112839109
Kobziar LN, Thompson GR. Wildfire smoke, a potential infectious agent. Science. 2020;370:1408–10.
• Mulliken JS, Hampshire KN, Rappold AG, Fung M, Babik JM, Doernberg SB. Risk of systemic fungal infections after exposure to wildfires: a population-based, retrospective study in California. The Lancet Planetary Health. 2023;7:e381–6 Hospital admission for coccidioidomycosis was found to increase by 20% in the month following smoke exposure from California wildfires.
Laws RL, Jain S, Cooksey GS, Mohle-Boetani J, McNary J, Wilken J, et al. Coccidioidomycosis outbreak among inmate wildland firefighters: California, 2017. Am J Ind Med. 2021;64:266–73.
Mead HL, Hamm PS, Shaffer IN, Teixeira MDM, Wendel CS, Wiederhold NP, et al. Differential thermotolerance adaptation between species of Coccidioides. JoF. 2020;6:366.
Klein BS, Vergeront JM, Weeks RJ, Kumar UN, Mathai G, Varkey B, et al. Isolation of Blastomyces dermatitidis in soil associated with a large outbreak of blastomycosis in Wisconsin. N Engl J Med. 1986;314:529–34.
Reed KD, Meece JK, Archer JR, Peterson AT. Ecologic niche modeling of Blastomyces dermatitidis in Wisconsin. Carter DA, editor. PLoS ONE. 2008;3:e2034.
Jackson KM, Pelletier KC, Scheftel J, Kerkaert JD, Robinson SL, McDonald T, et al. Blastomyces dermatitidis environmental prevalence in Minnesota: analysis and modeling using soil collected at basal and outbreak sites. Elkins CA, editor. Appl Environ Microbiol. 2021;87:e01922-20.
Klein BS, Vergeront JM, Disalvo AF, Kaufman L, Davis JP. Two outbreaks of blastomycosis along rivers in Wisconsin: isolation of Blastomyces dermatitidis from riverbank soil and evidence of its transmission along waterways. Am Rev Respir Dis. 1987;136:1333–8.
Szeder V, Ortega-Gutierrez S, Frank M, Jaradeh SS. CNS blastomycosis in a young man working in fields after Hurricane Katrina. Neurology. 2007;68:1746–7.
Schwartz IS, Wiederhold NP, Hanson KE, Patterson TF, Sigler L. Blastomyces helicus, a new dimorphic fungus causing fatal pulmonary and systemic disease in humans and animals in western Canada and the United States. Clin Infect Dis. 2019;68:188–95.
Brown EM, McTaggart LR, Zhang SX, Low DE, Stevens DA, Richardson SE. Phylogenetic analysis reveals a cryptic species Blastomyces gilchristii, sp. nov. within the human pathogenic fungus Blastomyces dermatitidis. Litvintseva AP, editor. PLoS ONE. 2013;8:e59237.
Carignan A, Boudhrioua C, Moreira S, Pelletier AA, Dufour K, Pépin J, et al. Changing patterns of disease severity in Blastomyces dermatitidis infection, Quebec Canada. Emerg Infect Dis. 2021;27:2810–7.
McDonald R, Dufort E, Jackson BR, Tobin EH, Newman A, Benedict K, et al. Notes from the field: blastomycosis cases occurring outside of regions with known endemicity — New York, 2007–2017. MMWR Morb Mortal Wkly Rep. 2018;67:1077–8.
Bahr NC, Antinori S, Wheat LJ, Sarosi GA. Histoplasmosis infections worldwide: thinking outside of the Ohio River Valley. Curr Trop Med Rep. 2015;2:70–80.
Anderson H, Honish L, Taylor G, Johnson M, Tovstiuk C, Fanning A, et al. Histoplasmosis cluster, Golf Course Canada. Emerg Infect Dis. 2006;12:163–5.
Calanni LM, Pérez RA, Brasili S, Schmidt NG, Iovannitti CA, Zuiani MF, et al. Brote de histoplasmosis en la provincia de Neuquén, Patagonia Argentina. Revista Iberoamericana de Micología. 2013;30:193–9.
Walker J, Spooner ET. Natural infection of the African baboon Papio papio with the large-cell form of Histoplasma. J Pathol Bacteriol. 1960;80:436–8.
Jensen HE, Bloch B, Henriksen P, Dietz HH, Schønheyder H, Kaufman L. Disseminated histoplasmosis in a badger (Meles meles) in Denmark. APMIS. 1992;100:586–92.
Clothier KA, Villanueva M, Torain A, Reinl S, Barr B. Disseminated histoplasmosis in two juvenile raccoons (Procyon lotor) from a nonendemic region of the United States. J Vet Diagn Invest. 2014;26:297–301.
Fischer NM, Favrot C, Monod M, Grest P, Rech K, Wilhelm S. A case in Europe of feline histoplasmosis apparently limited to the skin. Vet Dermatol. 2013;24(635–8):e158.
Brömel C, Sykes JE. Histoplasmosis in dogs and cats. Clin Tech Small Anim Pract. 2005;20:227–32.
Festa F, Ancillotto L, Santini L, Pacifici M, Rocha R, Toshkova N, et al. Bat responses to climate change: a systematic review. Biol Rev. 2023;98:19–33.
Nielsen K, De Obaldia AL, Heitman J. Cryptococcus neoformans mates on pigeon guano: Implications for the realized ecological niche and globalization. Eukaryot Cell. 2007;6:949–59.
Mitchell DH, Sorrell TC, Allworth AM, Heath CH, McGregor AR, Papanaoum K, et al. Cryptococcal disease of the CNS in immunocompetent hosts: influence of cryptococcal variety on clinical manifestations and outcome. Clin Infect Dis. 1995;20:611–6.
Springer DJ, Chaturvedi V. Projecting global occurrence of Cryptococcus gattii. Emerg Infect Dis. 2010;16:14–20.
Kidd SE, Bach PJ, Hingston AO, Mak S, Chow Y, MacDougall L, et al. Cryptococcus gattii dispersal mechanisms, British Columbia Canada. Emerg Infect Dis. 2007;13:51–7.
• Cogliati M. Global warming impact on the expansion of fundamental niche of Cryptococcus gattii VGI in Europe. Environ Microbiol Rep. 2021;13:375–83 Niche modeling by MaxEnt analysis demonstrates the gradual expansion of the fundamental niche of Cryptococcus gattii attributed to climate change.
Mak S, Klinkenberg B, Bartlett K, Fyfe M. Ecological niche modeling of Cryptococcus gattii in British Columbia Canada. Environ Health Perspect. 2010;118:653–8.
Byrnes EJ, Li W, Lewit Y, Ma H, Voelz K, Ren P, et al. Emergence and pathogenicity of highly virulent Cryptococcus gattii genotypes in the northwest United States. Howlett BJ, editor. PLoS Pathog. 2010;6:e1000850.
D’Souza CA, Kronstad JW, Taylor G, Warren R, Yuen M, Hu G, et al. Genome variation in Cryptococcus gattii, an emerging pathogen of immunocompetent hosts. Dromer F, editor. mBio. 2011;2:e00342-10.
Fisher MC, Alastruey-Izquierdo A, Berman J, Bicanic T, Bignell EM, Bowyer P, et al. Tackling the emerging threat of antifungal resistance to human health. Nat Rev Microbiol. 2022;20:557–71.
Gupta AK, Venkataraman M, Hall DC, Cooper EA, Summerbell RC. The emergence of Trichophyton indotineae: Implications for clinical practice. Int J Dermatology. 2023;62:857–61.
Denning DW, Hope WW. Therapy for fungal diseases: opportunities and priorities. Trends in Microbiol. 2010;18:195–204.
WHO Control and Response Strategies, Surveillance, Prevention, and Control Team. Global research agenda for antimicrobial resistance in human health. World Health Organization; 2023 Jun p. 1–12.
Fattouh N, Hdayed D, Geukgeuzian G, Tokajian S, Khalaf RA. Molecular mechanism of fluconazole resistance and pathogenicity attributes of Lebanese Candida albicans hospital isolates. Fungal Gen Biol. 2021;153:103575.
Arendrup MC, Perlin DS. Echinocandin resistance: an emerging clinical problem? Curr Opin Infect Dis. 2014;27:484–92.
Matsushita K, Azuma Y, Kosaka T, Yakushi T, Hoshida H, Akada R, et al. Genomic analyses of thermotolerant microorganisms used for high-temperature fermentations. Biosci Biotechnol Biochem. 2016;80:655–68.
Protsiv M, Ley C, Lankester J, Hastie T, Parsonnet J. Decreasing human body temperature in the United States since the Industrial Revolution. eLife. 2020;9:e49555.
Thompson GR, Albert N, Hodge G, Wilson MD, Sykes JE, Bays DJ, et al. Phenotypic differences of Cryptococcus molecular types and their implications for virulence in a Drosophila model of infection. Infect Immun. 2014;82:3058–65.
Bhabhra R, Askew DS. Thermotolerance and virulence of Aspergillus fumigatus: role of the fungal nucleolus. Med Mycol. 2005;43:87–93.
Barrs VR, Van Doorn TM, Houbraken J, Kidd SE, Martin P, Pinheiro MD, et al. Aspergillus felis sp. nov., an emerging agent of invasive aspergillosis in humans, cats, and dogs. Goldman GH, editor. PLoS ONE. 2013;8:e64871.
Tiwari S, Thakur R, Shankar J. Role of heat-shock proteins in cellular function and in the biology of fungi. Biotechnol Res Int. 2015.
Mattoon ER, Casadevall A, Cordero RJB. Beat the heat: correlates, compounds, and mechanisms involved in fungal thermotolerance. Fungal Biol Rev. 2021;36:60–75.
Segal BH. Aspergillosis. New England J Med. 2009;360:1870–84.
Askew DS. Aspergillus fumigatus: Virulence genes in a street-smart mold. Curr Opin Microbiol. 2008;11:331–7.
Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–60.
Vermeulen E, Lagrou K, Verweij PE. Azole resistance in Aspergillus fumigatus: a growing public health concern. Curr Opin Infect Dis. 2013;26.
Chowdhary A, Sharma C, Van Den Boom M, Yntema JB, Hagen F, Verweij PE, et al. Multi-azole-resistant Aspergillus fumigatus in the environment in Tanzania. J Antimicrob Chemother. 2014;69:2979–83.
Badali H, Vaezi A, Haghani I, Yazdanparast SA, Hedayati MT, Mousavi B, et al. Environmental study of azole-resistant Aspergillus fumigatus with TR34/L98H mutations in the cyp51A gene in Iran. Mycoses. 2013;56:659–63.
Abdolrasouli A, Rhodes J, Beale MA, Hagen F, Rogers TR, Chowdhary A, et al. Genomic context of azole resistance mutations in Aspergillus fumigatus determined using whole-genome sequencing. Taylor JW, editor. mBio. 2015;6:e00536-15.
Howard SJ, Cerar D, Anderson MJ, Albarrag A, Fisher MC, Pasqualotto AC, et al. Frequency and evolution of azole resistance in Aspergillus fumigatus associated with treatment failure. Emerg Infect Dis. 2009;15:1068–76.
Snelders E, Van Der Lee HAL, Kuijpers J, Rijs AJMM, Varga J, Samson RA, et al. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. Chris Kibbler, editor. PLoS Med. 2008;5:e219.
Van Der Linden JWM, Snelders E, Kampinga GA, Rijnders BJA, Mattsson E, Debets-Ossenkopp YJ, et al. Clinical implications of azole resistance in Aspergillus fumigatus, the Netherlands, 2007–2009. Emerg Infect Dis. 2011;17:1846–54.
Millner PD, Marsh PB, Snowden RB, Parr JF. Occurrence of Aspergillus fumigatus during composting of sewage sludge. Appl Environ Microbiol. 1977;34:765–72.
Millner PD, Bassett DA, Marsh PB. Dispersal of Aspergillus fumigatus from sewage sludge compost piles subjected to mechanical agitation in open air. Appl Environ Microbiol. 1980;39:1000–9.
Shouche S, Bhati P, Nema MZ, Jain SK. Mycobiota of decomposing floral waste materials. Asian J Microbiol Biotechnol Environ Sci. 2014;16:417–22.
Zhou D, Korfanty GA, Mo M, Wang R, Li X, Li H, et al. Extensive genetic diversity and widespread azole resistance in greenhouse populations of Aspergillus fumigatus in Yunnan, China. Mitchell AP, editor. mSphere. 2021;6:e00066-21.
Duong T-MN, Le T-V, Tran K-LH, Nguyen P-T, Nguyen B-PT, Nguyen T-A, et al. Azole-resistant Aspergillus fumigatus is highly prevalent in the environment of Vietnam, with marked variability by land use type. Environ Microbiol. 2021;23:7632–42.
Zhang J, Snelders E, Zwaan BJ, Schoustra SE, Meis JF, van Dijk K, et al. A novel environmental azole resistance mutation in Aspergillus fumigatus and a possible role of sexual reproduction in its emergence. mBio. 2017;8(3): 10–1128.
Van Rhijn N, Bromley M. The consequences of our changing environment on life threatening and debilitating fungal diseases in humans. JoF. 2021;7:367.
Zhao Y, Ye L, Zhao F, Zhang L, Lu Z, Chu T, et al. Cryptococcus neoformans, a global threat to human health. Infect Dis Poverty. 2023;12:20.
Kalem MC, Subbiah H, Leipheimer J, Glazier VE, Panepinto JC. Puf4 mediates post-transcriptional regulation of cell wall biosynthesis and caspofungin resistance in Cryptococcus neoformans. Alspaugh JA, editor. mBio. 2021;12:e03225-20.
Gusa A, Williams JD, Cho J-E, Averette AF, Sun S, Shouse EM, et al. Transposon mobilization in the human fungal pathogen Cryptococcus is mutagenic during infection and promotes drug resistance in vitro. Proc Natl Acad Sci USA. 2020;117:9973–80.
Sionov E, Lee H, Chang YC, Kwon-Chung KJ. Cryptococcus neoformans overcomes stress of azole drugs by formation of disomy in specific multiple chromosomes. Filler SG, editor. PLoS Pathog. 2010;6:e1000848.
Gago S, Serrano C, Alastruey-Izquierdo A, Cuesta I, Martín-Mazuelos E, Aller AI, et al. Molecular identification, antifungal resistance and virulence of Cryptococcus neoformans and Cryptococcus deneoformans isolated in Seville Spain. Mycoses. 2017;60:40–50.
Rodero L, Mellado E, Rodriguez AC, Salve A, Guelfand L, Cahn P, et al. G484S amino acid substitution in lanosterol 14-α demethylase ( ERG11) is related to fluconazole resistance in a recurrent Cryptococcus neoformans clinical isolate. Antimicrob Agents Chemother. 2003;47:3653–6.
Huang W, Liao G, Baker GM, Wang Y, Lau R, Paderu P, et al. Lipid flippase subunit Cdc50 mediates drug resistance and virulence in Cryptococcus neoformans. Wright GD, editor. mBio. 2016;7:e00478-16.
Casadevall A, Perfect JR. Cryptococcus neoformans. Washington DC: ASM press; 1998.
Wang Y, Aisen P, Casadevall A. Cryptococcus neoformans melanin and virulence: mechanism of action. Infect Immun. 1995;63:3131–6.
Khawcharoenporn T, Apisarnthanarak A, Mundy LM. Non-neoformans cryptococcal infections: a systematic review. Infection. 2007;35:51.
Espinel-Ingroff A, Colombo AL, Cordoba S, Dufresne PJ, Fuller J, Ghannoum M, et al. International evaluation of MIC distributions and epidemiological cutoff value (ECV) definitions for Fusarium species identified by molecular methods for the CLSI broth microdilution method. Antimicrob Agents Chemother. 2016;60:1079–84.
Batista BG, Lana DFD, Silveira GP, Sá MM, Ferreira M, Russo TVC, et al. Allylic selenocyanates as new agents to combat Fusarium species involved with human infections. ChemistrySelect. 2017;2:11926–32.
Batista BG, Chaves MAD, Reginatto P, Saraiva OJ, Fuentefria AM. Human fusariosis: an emerging infection that is difficult to treat. Rev Soc Bras Med Trop. 2020;53:e20200013.
Herkert PF, Al-Hatmi AMS, De Oliveira Salvador GL, Muro MD, Pinheiro RL, Nucci M, et al. Molecular characterization and antifungal susceptibility of clinical Fusarium species from Brazil. Front Microbiol. 2019;10:737.
Homa M, Galgóczy L, Manikandan P, Narendran V, Sinka R, Csernetics Á, et al. South Indian isolates of the Fusarium solani species complex from clinical and environmental samples: identification, antifungal susceptibilities, and virulence. Front Microbiol. 2018;9:1052.
Dalhoff A. Does the use of antifungal agents in agriculture and food foster polyene resistance development? A reason for concern. J Global Antimicrob Resist. 2018;13:40–8.
Price CL, Parker JE, Warrilow AG, Kelly DE, Kelly SL. Azole fungicides - understanding resistance mechanisms in agricultural fungal pathogens: mode of action and resistance mechanisms to azole fungicides. Pest Manag Sci. 2015;71:1054–8.
Sikora M, Kuthan R, Piskorska-Malolepsza K, Golas-Pradzynska M, Domański D, Augustynowicz-Kopeć E, et al. Prevalence and antifungal susceptibility of the emerging fungal species, Candida nivariensis, isolated in a teaching hospital in Poland. Polish J Microbiol. 2019;68:303–8.
Frías-De-León MG, Hernández-Castro R, Conde-Cuevas E, García-Coronel IH, Vázquez-Aceituno VA, Soriano-Ursúa MA, et al. Candida glabrata antifungal resistance and virulence factors, a perfect pathogenic combination. Pharmaceutics. 2021;13:1529.
Rajendran R, Sherry L, Nile CJ, Sherriff A, Johnson EM, Hanson MF, et al. Biofilm formation is a risk factor for mortality in patients with Candida albicans bloodstream infection—Scotland, 2012–2013. Clin Microbiol Infect. 2016;22:87–93.
Calvo B, Melo ASA, Perozo-Mena A, Hernandez M, Francisco EC, Hagen F, et al. First report of Candida auris in America: clinical and microbiological aspects of 18 episodes of candidemia. J Infection. 2016;73:369–74.
Rudramurthy SM, Chakrabarti A, Paul RA, Sood P, Kaur H, Capoor MR, et al. Candida auris candidaemia in Indian ICUs: analysis of risk factors. J Antimicrob Chemother. 2017;72:1794–801.
Sanyaolu A, Okorie C, Marinkovic A, Abbasi AF, Prakash S, Mangat J, et al. Candida auris : an overview of the emerging drug-resistant fungal infection. Infect Chemother. 2022;54:236.
Govender NP, Patel J, Magobo RE, Naicker S, Wadula J, Whitelaw A, et al. Emergence of azole-resistant Candida parapsilosis causing bloodstream infection: results from laboratory-based sentinel surveillance in South Africa. J Antimicrob Chemother. 2016;71:1994–2004.
Gleason TG. Emerging evidence of selection of fluconazole-tolerant fungi in surgical intensive care units. Arch Surg. 1997;132:1197.
Abi-Said D, Anaissie E, Uzun O, Raad I, Pinzcowski H, Vartivarian S. The epidemiology of hematogenous Candidiasis caused by different Candida species. Clin Infect Dis. 1997;24:1122–8.
Pires CAA, Cruz NFSD, Lobato AM, Sousa POD, Carneiro FRO, Mendes AMD. Clinical, epidemiological, and therapeutic profile of dermatophytosis. An Bras Dermatol. 2014;89:259–64.
Cafarchia C, Camarda A, Coccioli C, Figueredo LA, Circella E, Danesi P, et al. Epidemiology and risk factors for dermatophytoses in rabbit farms. Med Mycol. 2010;48:975–80.
Gallo MG, Lanfranchi P, Poglayen G, Calderola S, Menzano A, Ferroglio E, et al. Seasonal 4-year investigation into the role of the alpine marmot (Marmota marmota) as a carrier of zoophilic dermatophytes. Med Mycol. 2005;43:373–9.
Smith DJ, Williams SL, Endemic Mycoses State Partners Group, Benedict KM, Jackson BR, Toda M, et al. Surveillance for coccidioidomycosis, histoplasmosis, and blastomycosis — United States, 2019. MMWR Surveill Summ. 2022;71:1–14.
Johansson MA, Apfeldorf KM, Dobson S, Devita J, Buczak AL, Baugher B, et al. An open challenge to advance probabilistic forecasting for dengue epidemics. Proc Natl Acad Sci USA. 2019;116:24268–74.
Holcomb KM, Mathis S, Staples JE, Fischer M, Barker CM, Beard CB, et al. Evaluation of an open forecasting challenge to assess skill of West Nile virus neuroinvasive disease prediction. Parasites Vectors. 2023;16:11.
Acknowledgements
The authors would like to thank Drs. Andrea Porras-Alfaro and Donald Natvig for their continuing mentorship and helpful revisions of the manuscript.
Author information
Authors and Affiliations
Contributions
P.S.H. and T.T.C. wrote the manuscript and prepared the figure.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Pathogenesis
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salazar-Hamm, P., Torres-Cruz, T.J. The Impact of Climate Change on Human Fungal Pathogen Distribution and Disease Incidence. Curr Clin Micro Rpt 11, 140–152 (2024). https://doi.org/10.1007/s40588-024-00224-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-024-00224-x